Introduction
Bladder cancer is a major health problem,
particularly among males. It is estimated that in the year 2008,
150,000 patients succumbed to bladder cancer and 386,300 new
patients were diagnosed throughout the world (1). In the USA, bladder cancer is the fifth
most common malignancy (2).
According to a critical systematic review, bladder cancer is the
most expensive malignancy to treat on a per-patient basis due to
the requirement for lifelong routine monitoring and treatment from
diagnosis to mortality (3,4).
Over the past 10 years, great progress has been made
in our understanding of bladder cancer (5,6), and
radical cystectomy with orthotopic ileal neobladder is frequently
performed for muscle-invasive bladder cancer and high-risk
superficial tumors that are unresponsive to intravesical therapy
(7,8). With the development of laparoscopic
surgery in urology, laparoscopic radical cystectomy with different
urinary diversions has been reported as a step by step procedure
(9,10). Another study has indicated that
laparoscopic radical cystectomy with orthotopic ileal neobladder is
feasible and provides a number of intraoperative and post-operative
advantages over a traditional open approach (11), including decreasing the amount of
intraoperative bleeding, reducing post-operative pain and
complications, shortening the time required for recovery, and
allowing low morbidity and oncological safety.
Although the surgical techniques of laparoscopic
radical cystectomy with orthotopic ileal neobladder have been
studied extensively, no previous study has examined the long-term
urodynamic changes of this surgical procedure. Urodynamic testing
or urodynamics assesses the ability of the bladder and urethra to
store and release urine (12). The
purpose of the present study was to determine the long-term
urodynamics of laparoscopic radical cystectomy with orthotopic
ileal neobladder for patients with bladder cancer. This long-term
evaluation of urodynamics would also aid in promoting the
recognition of this procedure as an effective standard treatment
for bladder cancer.
Patients and methods
Patients and study design
This prospective observational study was conducted
between January 2010 and December 2012. Bladder cancer patients who
received laparoscopic radical cystectomy with orthotopic ileal
neobladder in the Department of Urology, Sichuan Academy of Medical
Sciences and Sichuan Provincial People’s Hospital (Chengdu,
Sichuan, China), were included, while bladder cancer patients who
showed evidence of distant metastases at diagnosis, complications
with serious internal diseases or any other malignancies were all
excluded.
This study was approved by the Institutional Review
Board of the Sichuan Academy of Medical Sciences and Sichuan
Provincial People’s Hospital and was conducted in accordance with
the 1975 Declaration of Helsinki. All patients signed informed
consent forms prior to participating in this study.
Surgical procedures and urodynamic
assessment
Prior to surgery, a complete physical examination
and routine other examinations, including urodynamic testing and
pre-operative examinations, such as cystoscopy, ultrasonography,
abdominal and pelvic CT or MRI, were all performed. The
laparoscopic radical cystectomy and orthotopic ileal neobladder
procedures were performed by surgical specialists, and detailed
information on the surgical procedures can be obtained from a
previously published study (10).
When discharged from hospital following surgery, all patients were
prospectively followed up at a clinic in the Sichuan Academy of
Medical Sciences and Sichuan Provincial People’s Hospital for
>12 months, and excretory urography and urodynamics were
examined every 6 months.
In this study, urodynamic evaluations were performed
using a Nidoc 970 A Urodynamic System (Yongxin Medical Equipment
Co., Ltd., Chengdu, Sichuan, China), and the following urodynamic
parameters were assessed: Maximum flow rate, residual urine,
maximum bladder capacity, maximum bladder pressures during filling
and voiding, and bladder compliance.
Statistical analysis
The storage and statistical analyses were performed
using SPSS version 17.0 (SPSS, Inc., Chicago, IL, USA). Continuous
data are presented as the mean ± standard deviation, while
categorical data are presented as n (%). Comparisons of continuous
data employed an independent two-sided paired t-test. P<0.05 was
considered to indicate a statistically significant difference.
Results
General information
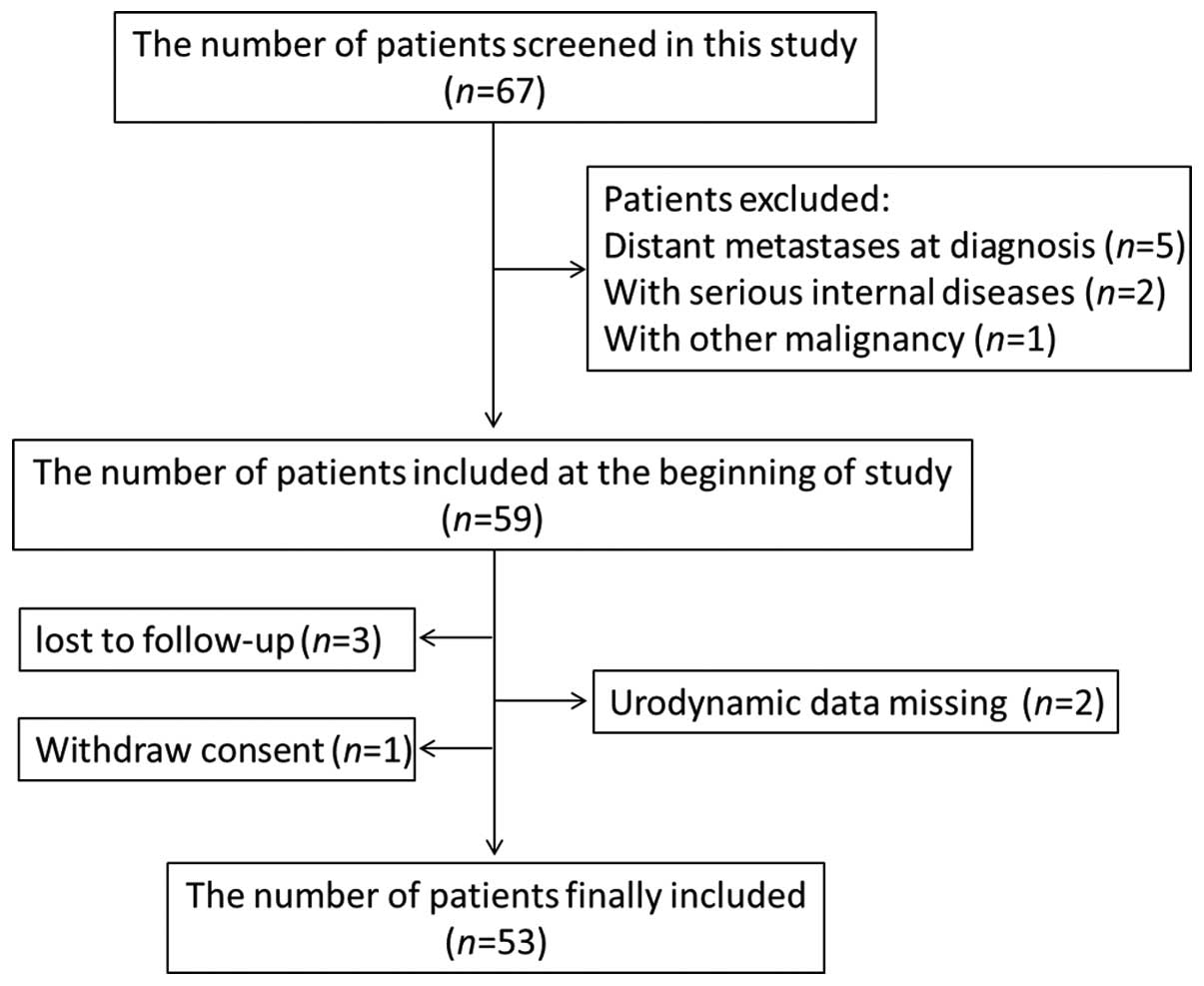
As shown in Fig. 1,
a total of 67 bladder cancer patients were screened in the present
study, and only 53 patients were finally included; the other 14
patients were excluded from the statistical analysis for various
reasons.
The detailed demographics, pre-operative surgical
history and pre-operative stage parameters of the 53 included
patients are all listed in Table I.
The intraoperative events and short-term postoperative data of the
patients are summarized in Table II, and indicated that
laparoscopic radical cystectomy with extracorporeal formation of a
neobladder are feasible and safe procedures for bladder cancer
patients.
 | Table IDemographics and pre-operative
clinical parameters. |
Table I
Demographics and pre-operative
clinical parameters.
| Parameters | Value |
|---|
| Demographics |
| Age, years | 58.7±7.3 |
| Male/female, n
(%) | 51 (96.2)/2
(3.8) |
| Body mass index,
kg/m2 | 20.9±2.7 |
| History of open or
abdominal/pelvic surgery, n (%) |
| Partial
cystectomy | 6 (11.3) |
| Cholecystectomy | 3 (5.7) |
| Repair of gastric
perforation | 2 (3.8) |
| Partial
gastrectomy | 2 (3.8) |
| Appendectomy | 1 (1.9) |
| Pre-operative
clinical T-staging, n (%) |
| T1 | 6 (11.3) |
| T2a | 28 (52.8) |
| T2b | 10 (18.9) |
| T3b | 8 (15.1) |
| T4a | 1 (1.9) |
| Pre-operative
clinical N-staging, n (%) |
| N0 | 49 (92.5) |
| N1 | 4 (7.5) |
| Pre-operative
histological characteristics, n (%) |
| Grade I/II/III | 7 (13.2) |
| Grade II | 42 (79.2) |
| Grade III | 4 (7.5) |
Changes in urodynamics
In order to investigate the long-term efficacy of
laparoscopic radical cystectomy with orthotopic ileal neobladder
for bladder cancer, all patients were followed up for at least 12
months and the urodynamic improvement of the patients was
evaluated. During the follow-up period, no patients reported
difficulty in urinating (Table
II), and the daily frequency of urination and the urine output
gradually improved with time.
 | Table IIIntraoperative events and
post-operative data. |
Table II
Intraoperative events and
post-operative data.
| Parameters | Value |
|---|
| Duration of surgical
procedures, min | 308.5±62.7 |
| Estimated blood loss,
ml | 210.5±106.8 |
| Blood transfusion, n
(%) | 8 (15.1) |
| Duration of
intra-abdominal drainage, days | 3.2±1.4 |
| Duration of foley
catheter, days | 12.4±2.9 |
| Duration of bilateral
ureteral stent, days | 11.8±2.2 |
| Bowel activity
recovery time post-surgery, days | 3.1±1.8 |
| Time until food
intake post-surgery, days | 4.2±0.7 |
| Hospitalization time
post-surgery, days | 13.5±2.6 |
| Follow-up time
post-discharge, months | 17.6±5.3 |
| Difficulty urinating
during follow-up, n (%) | 0 (0.0) |
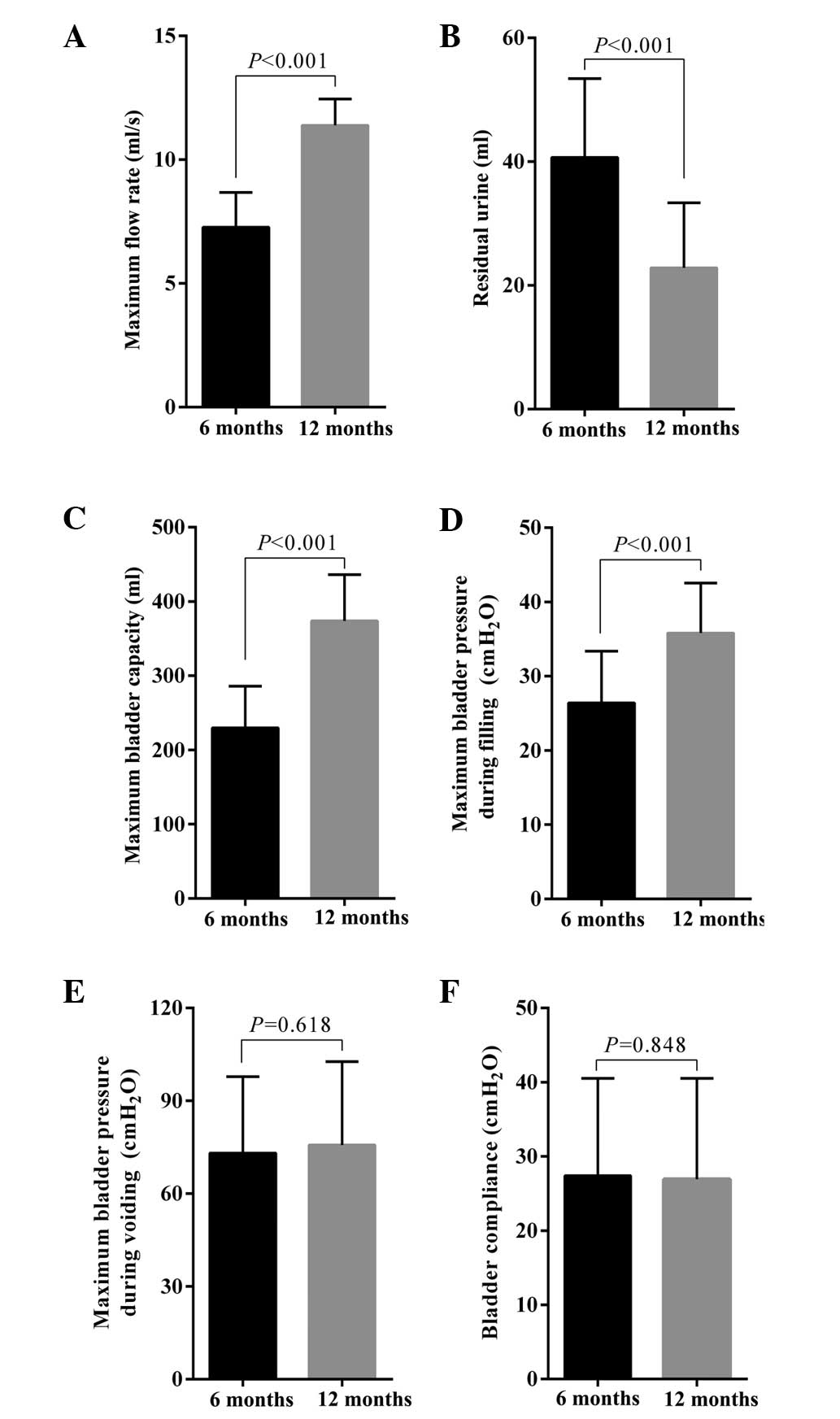
As shown in Fig. 2,
there was a time-related continuous improvement in urodynamics.
Compared with 6 months after the initial surgical treatment, the
maximum flow rate (11.4±1.1 vs. 7.3±1.4 ml/sec; P<0.001),
residual urine (22.8±10.5 vs. 40.7±12.7 ml; P<0.001), maximum
bladder capacity (373.8±62.2 vs. 229.7±56.3 ml; P<0.001) and
maximum bladder pressure during filling (35.8±6.7 vs. 26.4±7.0 cm
H2O; P<0.001) at 12 months had all improved
significantly. However, there was no significant difference in
either the maximum bladder pressures during voiding (75.7±24.7 vs.
73.1±24.7 cm H2O; P=0.618) or bladder compliance
(26.9±13.6 vs. 27.4±13.1 cm H2O; P=0.848) at 12 and 6
months after initial surgical treatment. These long-term dynamic
improvements in urodynamics showed that the constructed neobladder
had good storage and voiding functions.
Discussion
Bladder cancer is one of the most common
malignancies, and has become the most expensive to treat on a
per-patient basis (13). Due to the
extreme severity and metastasis-prone nature, bladder cancer
patients have a poor prognosis and high mortality rate. Although
the treatment of bladder cancer is complex, surgery remains
generally acknowledged as the most effective treatment (14). Currently, radical cystectomy is
widely used for muscle-invasive bladder cancer treatment,
particularly for bladder cancer with T-staging >2. With the
continuous improvement of surgical techniques and the wide
application of advanced auxiliary equipment, there have been a
number of studies documenting novel surgical approaches for bladder
cancer (15–17), including laparoscopic radical
cystectomy with orthotopic ileal neobladder, and due to the
successful reconstruction of the neobladder, the post-operative
quality of life of these patients has been greatly improved in
recent years.
Although urinary diversion following radical
cystectomy can be carried out in several ways, orthotopic
neobladder has been recognized as a relatively effective surgery
(19). Besides avoiding the
occurrences of urine and stool mixing and urine extravasation, the
physiological function of the orthotopic bladder is also extremely
close to the original bladder compared with other traditional
urinary diversion surgeries (20).
Considering the functional association between the bladder and
bowel, the potent clinical application values of orthotopic ileal
neobladder following radical cystectomy have been widely assessed
(21–23). Currently, a program of strictly
timed voiding has been carried out in all post-operative patients,
which aids patients in establishing the storage and voiding
functions of new bladders as soon as possible. However, significant
differences remain in the biological characteristics and neural
induction between the ileum and bladder. Long-term dynamic
monitoring of neobladder function following surgery is important,
and thus provides a basis for timely clinical intervention if
abnormalities of the neobladder observed.
A normal lower urinary tract should be able to
achieve efficient and low-pressure bladder filling, low-pressure
urine storage with perfect continence and periodic complete
voluntary urine expulsion, again at low pressure (24). In the present study, the orthotopic
ileal bladder that was constructed exhibited a high capacity,
improved compliance and low pressure at 6 months post-surgery. The
residual urine content was also gradually reduced with the
extension of the post-operative recovery time, which significantly
contributed to the prevention of urinary tract infections.
Moreover, the aforementioned functional parameters of the
orthotopic ileal bladder were further improved at 12 months
post-surgery. Thus, these findings further indicate the technical
feasibility and improved long-term prognosis of the orthotopic
ileal bladder, which is consistent with a previous study (25).
Studies have reported that the occurrence of night
continence is ~20%, which is higher than that of day continence.
Although the mechanism of night continence is not fully clarified,
pelvic muscle relaxation, contraction of external sphincter and
reservoir allantoic, and the lack of sensing urine expansion may be
possible causes (26). In the
present cohort, the ideal improvement in urodynamics during
long-term follow-up may also be explained by the adequate level of
health education and early bladder voiding function training,
including timed voiding during the day and night, a balanced intake
of water throughout the day and increased abdominal pressure using
the hands (or a squatting posture) to maximize emptying of the
bladder when urinating.
The limitation of the present study is the
relatively small sample size, and consequently, large sample,
multi-center studies are required. However, the dynamic monitoring
data for the urodynamics reported in this study provide novel
valuable evidence for the comprehensive evaluation of laparoscopic
radical cystectomy with orthotopic ileal neobladder for bladder
cancer in real life clinical practice.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011.
|
|
2
|
Kaplan AL, Litwin MS and Chamie K: The
future of bladder cancer care in the USA. Nat Rev Urol. 11:59–62.
2014.
|
|
3
|
Botteman MF, Pashos CL, Redaelli A, Laskin
B and Hauser R: The health economics of bladder cancer: a
comprehensive review of the published literature.
Pharmacoeconomics. 21:1315–1330. 2003.
|
|
4
|
Christoforidou EP, Riza E, Kales SN, et
al: Bladder cancer and arsenic through drinking water: a systematic
review of epidemiologic evidence. J Environ Sci Health A Tox Hazard
Subst Environ Eng. 48:1764–1775. 2013.
|
|
5
|
Rodriguez Faba O, Gaya JM, López JM, et
al: Current management of non-muscle-invasive bladder cancer.
Minerva Med. 104:273–286. 2013.
|
|
6
|
Cheung G, Sahai A, Billia M, Dasgupta P
and Khan MS: Recent advances in the diagnosis and treatment of
bladder cancer. BMC Med. 11:132013.
|
|
7
|
Clifton MM and Tollefson MK: Anatomic
basis of radical cystectomy and orthotopic urinary diversion in
female patients. Clin Anat. 26:105–109. 2013.
|
|
8
|
Kübler H and Gschwend JE: Ileal neobladder
in women with bladder cancer: cancer control and functional
aspects. Curr Opin Urol. 21:478–482. 2011.
|
|
9
|
Aboumarzouk OM, Drewa T, Olejniczak P and
Chlosta PL: Laparoscopic radical cystectomy: a 5-year review of a
single institute’s operative data and complications and a
systematic review of the literature. Int Braz J Urol. 38:330–340.
2012.
|
|
10
|
Huang J, Lin T, Xu K, et al: Laparoscopic
radical cystectomy with orthotopic ileal neobladder: a report of 85
cases. J Endourol. 22:939–946. 2008.
|
|
11
|
Challacombe BJ, Bochner BH, Dasgupta P, et
al: The role of laparoscopic and robotic cystectomy in the
management of muscle-invasive bladder cancer with special emphasis
on cancer control and complications. Eur Urol. 60:767–775.
2011.
|
|
12
|
Theofrastous JP, Whiteside J and Paraiso
MF: The utility of urodynamic testing. J Am Assoc Gynecol Laparosc.
10:548–552. 2003.
|
|
13
|
Mossanen M and Gore JL: The burden of
bladder cancer care: direct and indirect costs. Curr Opin Urol. May
30–2014.(Epub ahead of print).
|
|
14
|
Mueller J, Schrader AJ, Schrader M,
Schnoeller T and Jentzmik F: Management of muscle-invasive bladder
cancer. Minerva Urol Nefrol. 65:235–248. 2013.
|
|
15
|
Azzouni F: Current status of minimally
invasive radical cystectomy: an outcome-based comparison. Exp Rev
Anticancer Ther. 13:681–695. 2013.
|
|
16
|
Nix J, Smith A, Kurpad R, Nielsen ME,
Wallen EM and Pruthi RS: Prospective randomized controlled trial of
robotic versus open radical cystectomy for bladder cancer:
perioperative and pathologic results. Eur Urol. 57:196–201.
2010.
|
|
17
|
Izquierdo L, Bolton DM and Lawrentschuk N:
Radical cystectomy and orthotopic bladder substitution: surgical
tricks and management of complications. Minerva Urol Nefrol.
65:225–234. 2013.
|
|
18
|
Berger A and Aron M: Laparoscopic radical
cystectomy: long-term outcomes. Curr Opin Urol. 18:167–172.
2008.
|
|
19
|
Roghmann F, Becker A, Trinh QD, et al:
Updated assessment of neobladder utilization and morbidity
according to urinary diversion after radical cystectomy: A
contemporary US-population-based cohort. Can Urol Assoc J.
7:E552–E560. 2013.
|
|
20
|
Herdiman O, Ong K, Johnson L and
Lawrentschuk N: Orthotopic bladder substitution (Neobladder): part
II: postoperative complications, management, and long-term
follow-up. J Wound Ostomy Continence Nurs. 40:171–180. 2013.
|
|
21
|
Hart S, Skinner EC, Meyerowitz BE, Boyd S,
Lieskovsky G and Skinner DG: Quality of life after radical
cystectomy for bladder cancer in patients with an ileal conduit,
cutaneous or urethral kock pouch. J Urol. 162:77–81. 1999.
|
|
22
|
Guan Z, Li J and Yang R: Impacts of
different grafts for bladder reconstruction on postoperative
recovery of the patients. Nan Fang Yi Ke Da Xue Xue Bao.
33:1250–1252. 2013.(In Chinese).
|
|
23
|
Marim G, Bal K, Balci U, Girgin C and
Dinçel C: Long-term urodynamic and functional analysis of
orthotopic ‘W’ ileal neobladder following radical cystectomy. Int
Urol Nephrol. 40:629–636. 2008.
|
|
24
|
Chapple C: Overview on the lower urinary
tract. Handb Exp Pharmacol. 202:1–14. 2011.
|
|
25
|
Chen Z, Lu G, Li X, et al: Better
compliance contributes to better nocturnal continence with
orthotopic ileal neobladder than ileocolonic neobladder after
radical cystectomy for bladder cancer. Urology. 73:838–844.
2009.
|
|
26
|
Schrier BP, Laguna MP, van der Pal F,
Isorna S and Witjes JA: Comparison of orthotopic sigmoid and ileal
neobladders: continence and urodynamic parameters. Europ Urol.
47:679–685. 2005.
|