Introduction
Hepatic epithelioid hemangioendothelioma (HEH) is a
rare vascular tumor of the liver with low- to intermediate-grade
malignancy. Due to the rare tumor incidence and non-specific
clinical presentation, HEH is difficult to differentiate from focal
liver lesions including hepatocellular carcinoma, angiosarcoma and
metastatic carcinoma (1–3). Although modern cross-sectional imaging
techniques display the typical radiographic features of HEH, such
as coalescence of nodules, capsular retraction and intralesional
calcifications, the final definitive diagnosis of HEH is entirely
dependent on histopathological verification (1–3).
In general, fine needle biopsy is able to provide a
valuable diagnosis of HEH, but this can be confused with other
conditions, particularly sclerosing hemangioma and sclerosing
adenocarcinoma (1). In patients
with HEH, parenchymal abnormalities are irregularly distributed and
sampling variability is almost inevitable. Therefore, the
specificity of the diagnosis mainly depends on precise tumor
localization and a biopsy specimen of sufficient size (4). In the present study, we report the
case of a patient whose underwent two, percutaneous liver biopsies,
both of which failed to reveal a diagnosis of HEH. The patient was
ultimately diagnosed by laparoscopic liver biopsy, as this
technique allowed adequate tissue sampling under direct vision. The
patient provided written informed consent.
Case report
A 42-year-old female was admitted to West China
Hospital, Sichuan University (Chengdu, China) in February, 2013
with mild right upper quadrant discomfort. The patient had no
history of drug and alcohol abuse, or hepatitis. An abdominal
ultrasound and the initial laboratory tests were scheduled.
Ultrasonography showed multiple hypoechoic masses in the liver,
whereas the liver function tests were in the normal range. Tumor
markers, including α-fetoprotein (AFP), cancer embryonic antigen
(CEA), carbohydrate antigen 199 (CA199), and CA125 were all within
normal limits.
In view of such findings, liver metastases were
suspected and, thus, whole body magnetic resonance imaging (MRI)
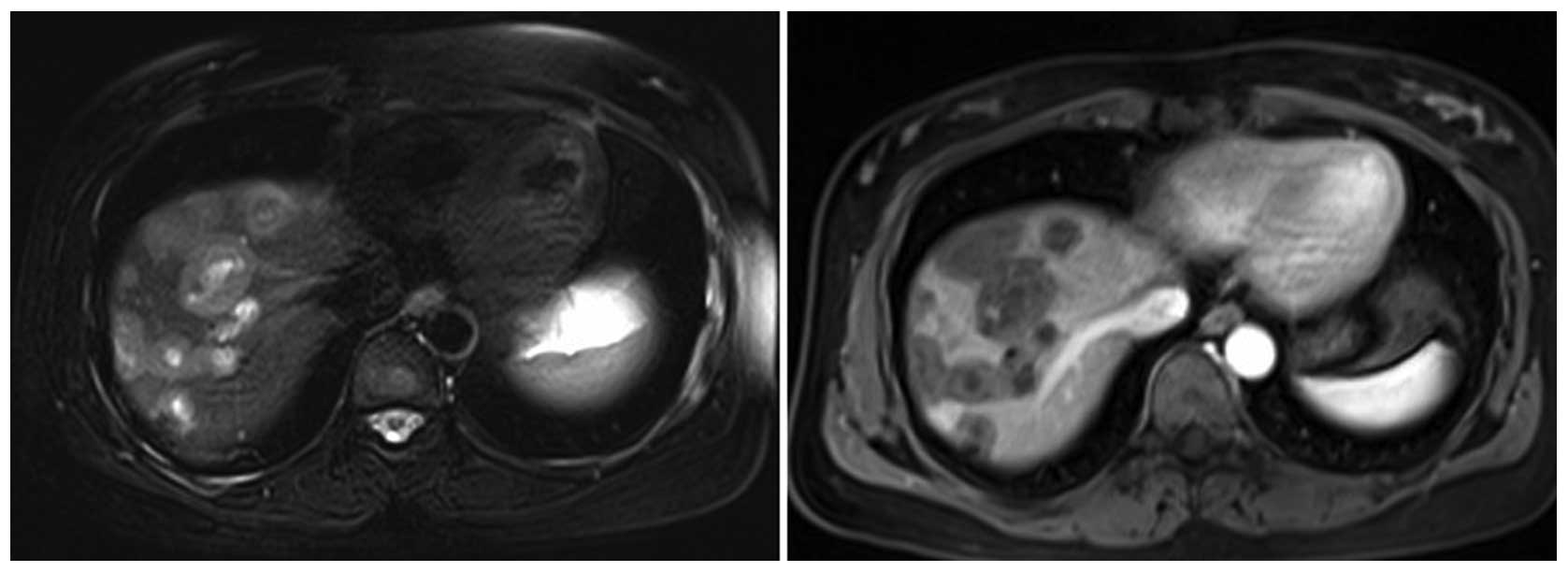
was performed to find the primary tumor. MRI showed multiple mass
lesions scattered throughout the liver with low-signal intensity on
T1-weighted imaging (T1WI) and high-signal intensity on T2-weighted
imaging (T2WI) (Fig. 1). There was
no evidence of extrahepatic disease. Subsequently, ultrasound
(US)-guided liver biopsy from the largest liver lesion was
performed using an 18-gauge needle. This showed massive
hepatocellular necrosis mixed with some epithelial cells. As the
first biopsy was considered to have sampling error, a repeat biopsy
was performed from the second largest liver lesion and the specimen
was analyzed by the senior pathologists. However, the results still
showed massive hepatocellular necrosis and no obvious atypical
epithelial proliferation. Following consultation with the
pathologists, inadequate specimen (1 mm in diameter and <2 cm in
length) was considered to be the main reason for diagnosis failure.
Therefore, laparoscopic liver biopsy was performed to obtain
adequate tissue samples for histological examination.
Under general anesthesia, carbon dioxide
pneumoperitoneum was achieved with the patient in supine position.
Three laparoscopic ports were inserted: A 10-mm camera port was
placed immediately below the umbilicus, a 12-mm trocar was placed
below the xiphoid process and a 5-mm trocar was placed below the
rib cage at the level of the right midclavicular line. Several
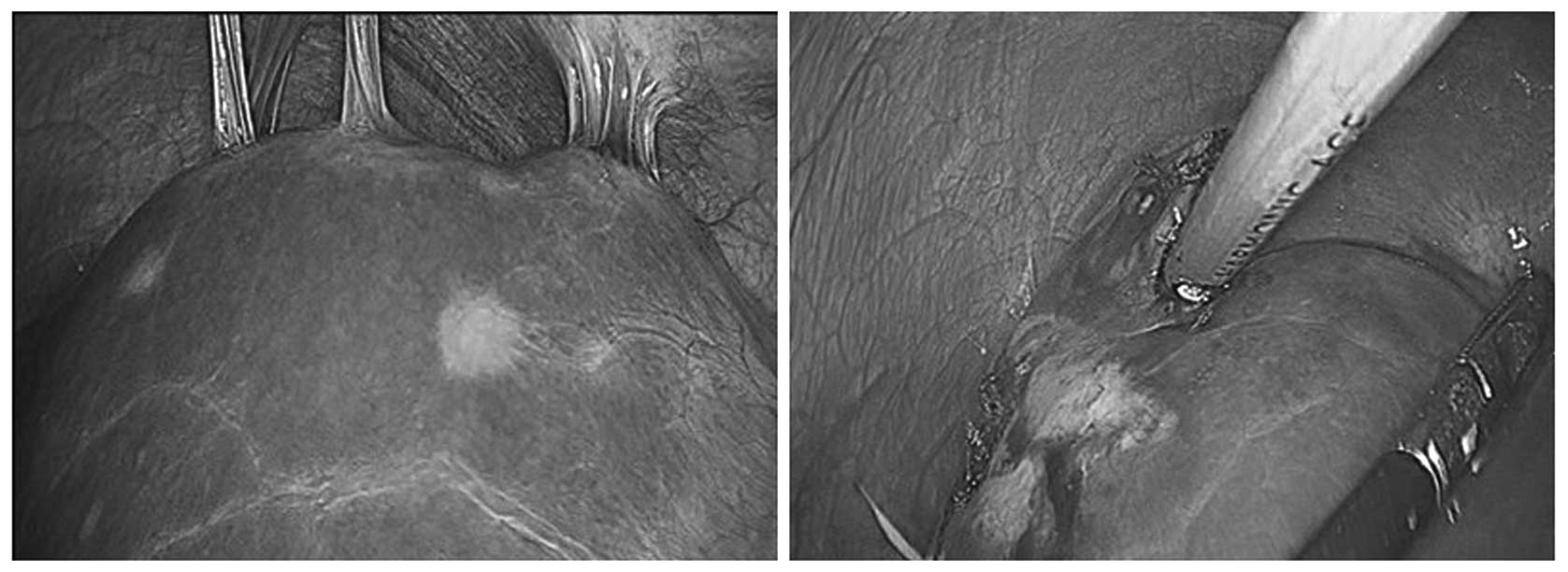
masses of varying size and with a gray appearance were seen
protruding from the surface of the right liver lobe (Fig. 2). A wedge resection liver mass
biopsy of ~1.5×1.5×1.0 cm in size was obtained using an ultrasonic
scalpel (Harmonic Scalpel; Ethicon Endo-Surgery Inc., Cincinnati,
OH, USA) (Fig. 2). The patient was
discharged on the first postoperative day with no complications.
After one week, the histopathology report revealed medium -to
large-sized pleiomorphic cells spread within the sinusoids and
small veins. These cells stained positive for CD31, CD34 and factor
VIII-related antigen, as well as CK7, CK19 and phosphoenolpyruvate
carboxykinase. Thus, the overall immunohistochemical findings
supported the diagnosis of HEH. Therefore, we recommended that the
patient undergo liver transplantation, but the patient refused.
During the past eight months of follow-up after discharge, the
patient has been asymptomatic and liver ultrasonography at
two-month intervals has shown no significant change with respect to
lesion size.
Discussion
HEH is a rare tumor with an incidence of <0.1 per
100,000 individuals worldwide (5).
The clinical manifestation of HEH varies from asymptomatic to
non-specific symptoms, such as right upper quadrant discomfort,
weight loss and abnormal liver function (3). In addition, routine laboratory tests
are usually inconclusive and normal serum tumor markers, including
AFP, CEA, CA199 and CA125, do not exclude other primary and
secondary liver tumors. In the majority of patients, the tumor is
first discovered incidentally during imaging studies. Although
typical imaging features of HEH, such as coalescence of nodules,
capsular retraction and intralesional calcifications, have been
proposed to be useful in improving the diagnosis of this rare
hepatic tumor, great imaging heterogeneity still persists (2). Additionally, definitive diagnosis of
HEH requires histopathological examination. Diagnosis of HEH is
mostly confirmed by immunohistochemical evidence of endothelial
differentiation, which mainly depends on the detection of the
expression of certain key endothelial cell markers, such as CD31,
CD34 and factor VIII-related antigen (1). In the present case, a diagnosis of HEH
was missed in the two core biopsies, which may have been due to
poor biopsy specimens that were insufficient in size and with
central necrosis in the liver mass.
In hepatic tumors such as HEH, parenchymal
abnormalities are irregularly distributed and sampling variability
is almost inevitable (4). Thus, in
order to improve the accuracy of diagnosis and further grading and
tumor staging, the most practical solution appears to be obtaining
a biopsy specimen of sufficient size. Laparoscopic liver biopsy not
only allows for the systematic visualization of lesions, but also
obtains adequate tissue samples under direct vision (4,5).
However, according to the various related literature, despite a
high sensitivity and specificity of laparoscopic liver biopsy for
the diagnosis of liver lesions, the diagnostic accuracy varies for
different disease process: 98% for chronic liver disease, 91% for
abnormal liver function and only 85% for cancer (6). In addition, complications of
laparoscopic liver biopsy include general anesthesia, bowel
perforation, bleeding from the biopsy site and local abdominal wall
trauma (5,7). Additionally, high expenses and the
requirement for special expertise in performing the procedure have
limited its use. However, biopsies performed with narrower gauge
needles (smaller than 18 gauge) have occasionally been found to be
adequate to establish the diagnosis (4). To the best of our knowledge, there are
no direct comparisons of the complications and outcomes between
percutaneous and laparoscopic biopsy to date. However, it should be
noted that use of a thin biopsy needle may increase the sampling
error and lead to an incorrect diagnosis, due to an insufficient
sample size (8).
In summary, in the present case, when US-guided
percutaneous liver biopsy failed to diagnose HEH, laparoscopic
liver biopsy was safely performed, obtaining adequate specimens for
analysis. Although this method was not the preferred technique and
has certain drawbacks, it is considered to be a useful and
minimally invasive approach for liver lesions when other
less-invasive diagnostic modalities fail or are difficult to be
performed.
References
|
1
|
Makhlouf HR, Ishak KG and Goodman ZD:
Epithelioid hemangioendothelioma of the liver: a clinicopathologic
study of 137 cases. Cancer. 85:562–582. 1999.
|
|
2
|
Lyburn ID, Torreggiani WC, Harris AC, et
al: Hepatic epithelioid hemangioendothelioma: sonographic, CT, and
MR imaging appearances. AJR Am J Roentgenol. 180:1359–1364.
2003.
|
|
3
|
Mehrabi A, Kashfi A, Fonouni H, et al:
Primary malignant hepatic epithelioid hemangioendothelioma: a
comprehensive review of the literature with emphasis on the
surgical therapy. Cancer. 107:2108–2121. 2006.
|
|
4
|
Rockey DC, Caldwell SH, Goodman ZD, et al:
Liver biopsy. Hepatology. 49:1017–1044. 2009.
|
|
5
|
Richardson WS, Stefanidis D, Chang L,
Earle DB and Fanelli RD: The role of diagnostic laparoscopy for
chronic abdominal conditions: an evidence-based review. Surg
Endosc. 23:2073–2077. 2009.
|
|
6
|
Jalan R, Harrison DJ, Dillon JF, Elton RA,
Finlayson ND and Hayes PC: Laparoscopy and histology in the
diagnosis of chronic liver disease. QJM. 88:559–564. 1995.
|
|
7
|
Vargas C, Jeffers LJ, Bernstein D, et al:
Diagnostic laparoscopy: a 5-year experience in a hepatology
training program. Am J Gastroenterol. 90:1258–1262. 1995.
|
|
8
|
Brunetti E, Silini E, Pistorio A, et al:
Coarse vs. fine needle aspiration biopsy for the assessment of
diffuse liver disease from hepatitis C virus-related chronic
hepatitis. J Hepatol. 40:501–506. 2004.
|