Introduction
Basal cell adenoma (BCA) was first described in the
salivary gland in a study by Kleinsasser and Klein in 1967
(1). This tumor represents 1–2% of
all salivary gland tumors, and the majority of these are found in
the parotid gland. In 1991, BCA was recognized as an independent
entity in the second edition of the Salivary Gland Tumors
Classification by the World Health Organization (2). Histologically, this tumor is composed
of basaloid cells delineated from the stroma by the basement
membrane. There are four characteristic patterns of BCA; solid,
trabecular, tubular and membranous. The membranous subtype
exhibiting high recurrence rates. Histological and
immunohistochemical staining are used for diagnosis, while surgical
resection with a cuff of normal salivary tissue is the main
treatment. The current study reports a rare case of synchronous BCA
of the left parotid gland in a 68-year-old male. In addition, the
clinical features of the condition are described and a review of
the literature is presented. This study was approved by the Ethics
Committee of Wuhan Central Hospital (Wuhan, China) and was
performed according to the Declaration of Helsinki. Patient
provided written informed consent.
Case report
In November 2012, a 68-year-old male presented to
the Wuhan Union Hospital (Wuhan, China) with a mass in the left
infra-auricular area was referred to the Department of Oral and
Maxillofacial Surgery at Wuhan Central Hospital (Wuhan, China) in
March 2013. Four months prior to admittance, an ultrasound
examination at Wuhan Union Hospital identified a homogeneous tumor
in the left parotid region. A fine-needle aspiration biopsy
extracted brown liquid indicative of a cyst of the parotid
gland.
Upon physical examination, a round, 1.5×1.5-cm,
movable, tender and painless mass was palpable on the superior
portion of the parotid gland of the left side. The tumor was not
attached to the skin, and no facial palsy or regional
lymphadenopathy was observed.
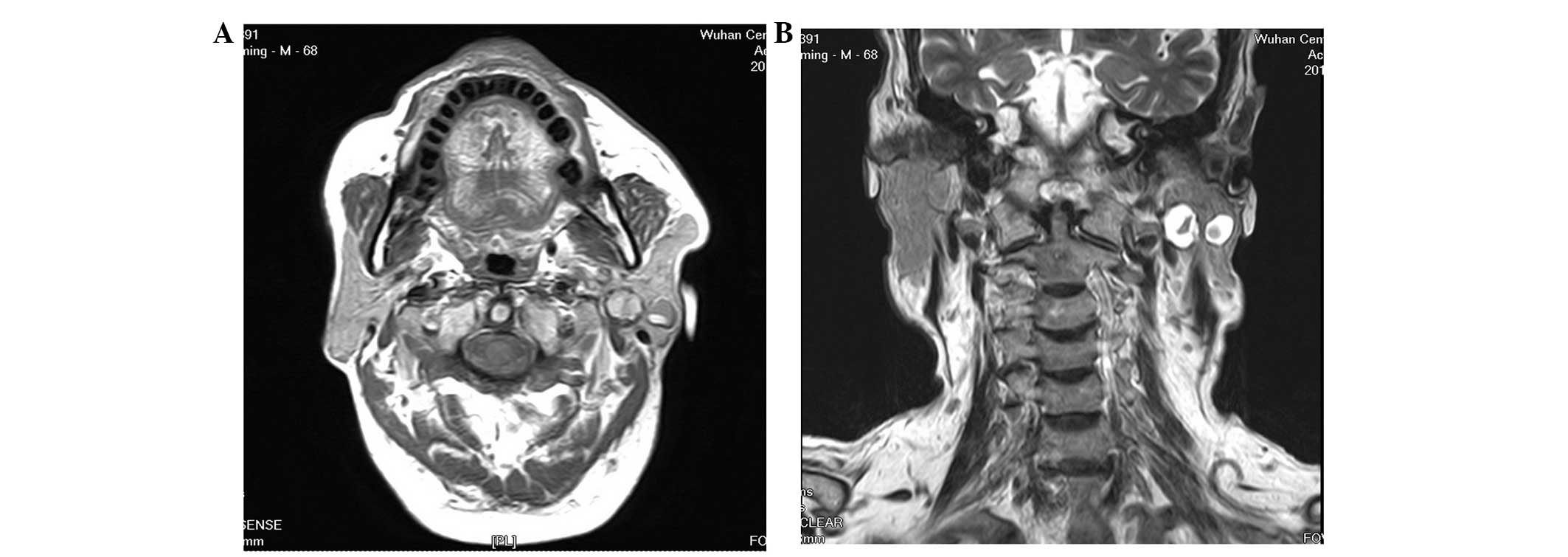
Magnetic resonance imaging (MRI) was performed and
showed two independent masses in the superficial and deep lobes of
the parotid gland on the left side, respectively (Figs. 1 and 2). The tumors were well-marginated, with
peripheral solid and central cystic components. The superficial
tumor measured 12 mm in diameter, whereas the deeper tumor measured
15 mm in diameter. From these results, the initial diagnosis was of
synchronous unilateral tumors, similar to Warthin’s tumors.
The MRI features on the T1-weighted images revealed
differences in the composition of the tumors. The solid component
of the superior tumor returned a hypointense signal, higher than
that of muscle, but lower than the surrounding parotid tissue. For
the deep mass, however, the solid component exhibited slight
hyperintensity compared with the superior tumor, and isointensity
compared with the surrounding parotid tissue. Compared with the
central component of the two masses, the superior tumor exhibited
moderate enhancement and the deep tumor was slightly hypointense.
On T2-weighted images, moderate enhancement was observed in the
peripheral component and hypointensity in the central
component.
A total parotidectomy was performed, which included
resection of the two tumors and preservation of the facial nerve.
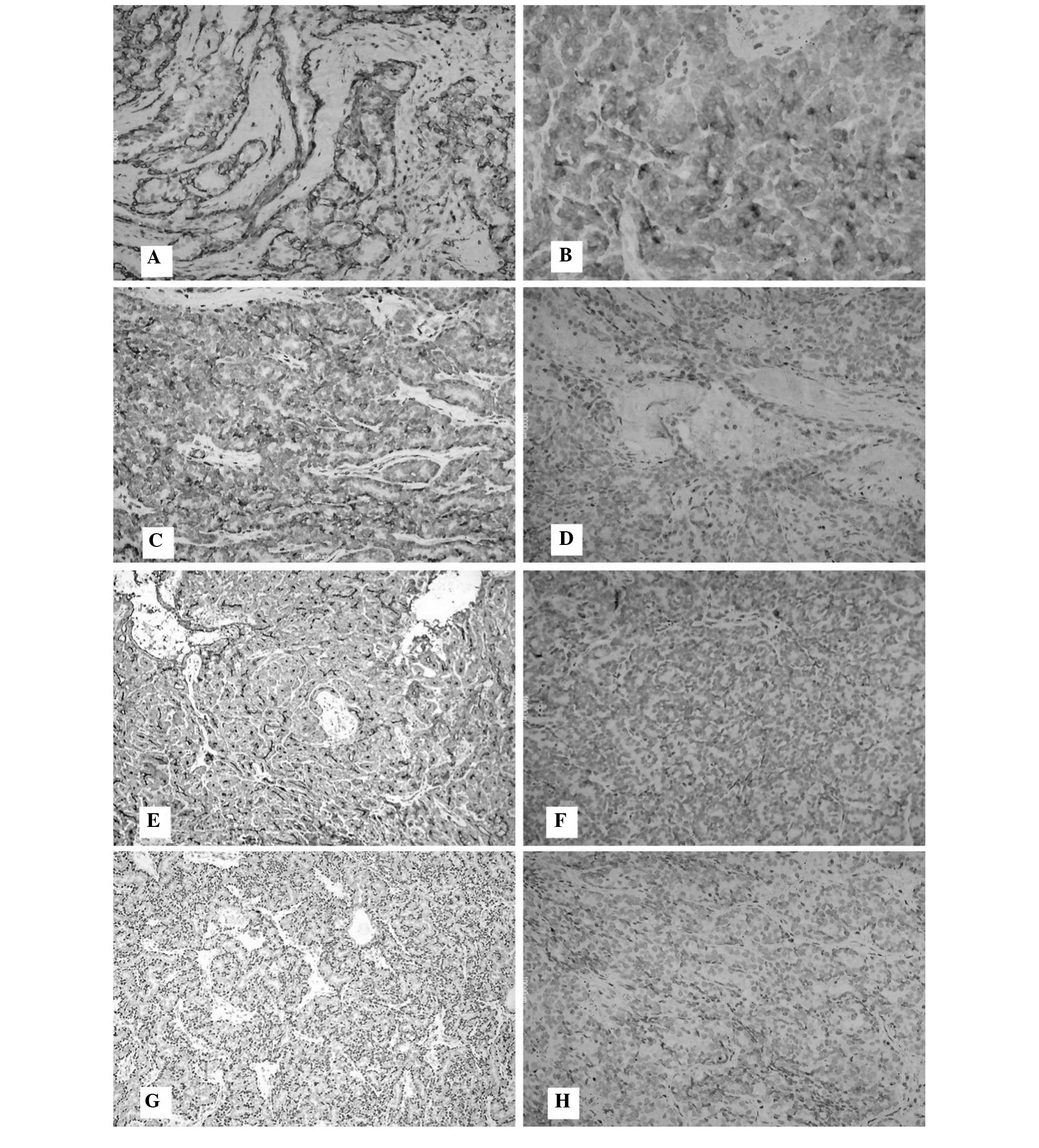
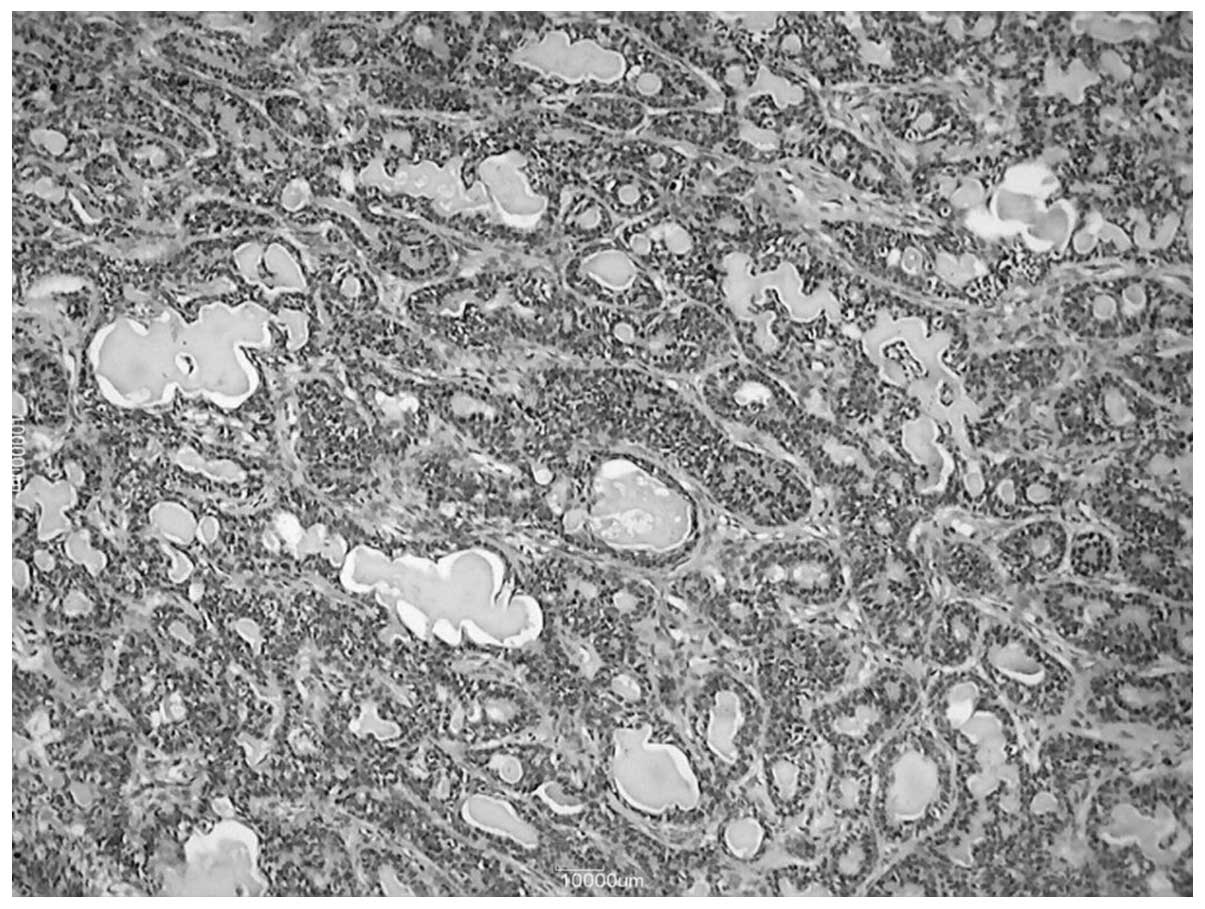
Hispathological examination and immunohistochemical study
demonstrated that the tumors were BCAs (Figs. 3 and 4). After 6 months of
follow-up, no sign of recurrence was found and the facial nerve
function had recovered well.
Discussion
Synchronous unilateral or bilateral multifocal
tumors of the salivary glands rarely occur, representing <1% of
major salivary gland tumors (3).
Adenolymphoma is the most common type of multifocal tumor (4,5). BCA
is an uncommon benign neoplasm, accounting for ~2% of tumors in the
salivary glands, and with the majority found in the parotid
gland.
The occurrence of synchronous bilateral BCAs of the
parotid gland is also rare, with only four previously reported
cases (6–9). Synchronous unilateral BCA in the
parotid gland is extremely rare, and has only been reported once by
Kuratomi et al (10) in
2006. This study described the case of an elderly female with two
simultaneous BCAs as recurrent tumors of pleomorphic adenoma (PA)
of the left parotid gland.
Clinical palpation is poor at detecting multifocal
ipsilateral tumors, particularly for those tumors that occur in the
deep portion. The use of imaging techniques is necessary
pre-operatively. Studies on MRI and computed tomography (CT) for
the assessment of BCA are few in number. Kiyosue et al
(11) first reported the MRI
findings of BCA of the parotid gland. In the study, BCA was well
circumscribed with a rounded shape. The solid section of the tumor
exhibited a lower intensity signal than that of the surrounding
parotid tissue on T1- and T2-weighted images. Ethunandan et
al (12), however, found that
imaging investigations were able to diagnose only 23% of
ipsilateral multiple tumors, while another 56% of tumors were noted
by palpation during the surgery, and therefore suggested the use of
intra-operative palpation to evaluate the presence and location of
multiple tumors.
Differential diagnoses for BCA of the parotid gland
include PA and Warthin’s tumors. A mass with lobulated contours
favors the diagnosis of a PA, while cyst formation is more common
in Warthin’s tumors (13,14). Kuratomi et al (10) found that epithelial tumor cells of
PA may form BCA through certain differentiation mechanisms. This
was a result of the authors identifying that basal cells of the
epithelium of PA possess reserve cell functions, through
epithelial-mesenchymal transdifferentiation, forming the
predominant basaloid cell population of BCA. Chawla et al
(15) described the CT appearance
of 14 cases of BCA of the parotid gland and found the presence of
linear bands or stellate-shaped non-enhanced areas may be a
specific imaging feature of the tumor.
Histologically, BCA is composed of basaloid cells
that are sharply delineated from the stroma by the basement
membrane. The absence of a chondromyxoid stroma may be used to
distinguish the tumors from PA (16). There are four characteristic
patterns of BCA: Solid, trabecular, tubular and membranous. The
membranous subtype forms 10% of BCAs, and is often
non-encapsulated, multicentric and multilobular, with a
post-resection recurrence rate of up to 25% (16). The other subtypes, however, have low
recurrence rates due to the absence of pseudopodia (17).
The present study encountered a rare case of
synchronous BCA of the left parotid gland. Local excision or
extracapsular dissection is not suitable for multifocal ipsilateral
or non-encapsulated tumors, therefore, the present case underwent a
total parotidectomy.
References
|
1
|
Kleinsasser O and Klein HJ: Basal cell
adenoma of the salivary glands. Arch Klin Exp Ohr Nas
Kehlkopsheilkd. 189:302–316. 1967.(In German).
|
|
2
|
Seifert G and Sobin LH; World Health
Organization International Histological Classification of Tumours.
Histological Typing of Salivary Gland Tumors. Springer-verlag;
Berlin: 1991
|
|
3
|
Foote FW Jr and Frazell EL: Tumors of the
major salivary glands. Cancer. 6:1065–1133. 1953.
|
|
4
|
Lam KH, Ho HC, Ho CM and Wei WI:
Multifocal nature of adenolymphoma of the parotid. Br J Surg.
81:1612–1614. 1994.
|
|
5
|
Maiorano E, Lo Muzio L, Favia G and
Piattelli A: Warthin’s tumour: a study of 78 cases with emphasis on
bilaterality, multifocality and association with other
malignancies. Oral Oncol. 38:35–40. 2002.
|
|
6
|
Zarbo RJ, Ricci A Jr, Kowalczyk PD, et al:
Intranasal dermal analogue tumor (membranous basal cell adenoma).
Ultrastructure and immunohistochemistry. Arch Otolaryngol.
111:333–337. 1985.
|
|
7
|
Katsuno S, Ishii K, Otsuka A, et al:
Bilateral basal-cell adenomas in the parotid glands. J Laryngol
Otol. 114:83–85. 2000.
|
|
8
|
Suzuki S, Okamura H and Ohtani I:
Bilateral parotid gland basal cell adenomas. Case report. ORL J
Otorhinolaryngol Relat Spec. 62:278–281. 2000.
|
|
9
|
Reddy KA, Trimurthy Rao A, Krishna R, et
al: A rare case of bilateral basal cell adenomas in the parotid
glands. Indian J Surg. 70:32–34. 2008.
|
|
10
|
Kuratomi Y, Satoh S, Hayashida S and
Inokuchi A: Basal cell adenoma and lymphoepithelial cyst as
recurrent tumors of pleomorphic adenoma of the parotid gland. Auris
Nasus Larynx. 33:97–100. 2006.
|
|
11
|
Kiyosue H, Mori H, Okahara M, et al: Head
and neck imaging. Diagnostic imaging of parotid gland tumors. Jpn J
Diagn Imaging. 20:38–54. 2000.
|
|
12
|
Ethunandan M, Pratt CA, Morrison A, et al:
Multiple synchronous and metachronous neoplasms of the parotid
gland: the Chichester experience. Br J Oral Maxillofac Surg.
44:397–401. 2006.
|
|
13
|
Silvers AR and Som PM: Salivary glands.
Radiol Clin North Am. 36:941–966. 1998.
|
|
14
|
Choi DS, Na DG, Byun HS, et al: Salivary
gland tumors: evaluation with two-phase helical CT. Radiology.
214:231–236. 2000.
|
|
15
|
Chawla AJ, Tan TY and Tan GJ: Basal cell
adenomas of the parotid gland: CT scan features. Eur J Radiol.
58:260–265. 2006.
|
|
16
|
Luna MA: Salivary gland. Head and Neck
Surgical Pathology. Pilch PZ: Lippincott, Williams and Wilkins;
Philadelphia: pp. 312–315. 2001
|
|
17
|
Phillips PP and Olsen KD: Recurrent
pleomorphic adenoma of the parotid gland: report of 126 cases and a
review of the literature. Ann Otol Rhinol Laryngol. 104:100–104.
1995.
|