Introduction
Endometrial cancer is the most common gynecological
malignancy in western countries (1). The majority of endometrial carcinomas
(ECs) are diagnosed at an early stage (FIGO I–II), exhibit a
favorable prognosis and may be cured predominantly by primary
surgery and adjuvant radiotherapy. However, 10–15% of tumors recur
and the majority (80–90%) of recurrences take place within three
years (2). Treatment of recurrences
is a challenge. Local vaginal recurrences are curable if diagnosed
early, however, pelvic and distant recurrences exhibit a poor
prognosis. A number of predictive and prognostic factors have been
studied previously, for example, age of the patient, time between
treatment and recurrence (3), prior
radiotherapy (4), histological
type, FIGO grade, size of the tumor (5), type of therapy for the recurrent
disease (6) and radiation dose to
the target (7). However, the
importance of these factors remains controversial. Notably, in
randomized phase III trials, postoperative adjuvant radiotherapy
significantly improved locoregional (vaginal and pelvic) tumor
control, but did not improve survival rate (4,8). An
explanation for this paradox may be found by investigating the
natural history of the recurrences and the association between
local, regional and distant sites of recurrences versus adjuvant
therapy.
In the present retrospective study of 100
endometrial cancer recurrences, a number of predictive and
prognostic factors were analyzed. The natural history of the
recurrences was the predominant focus of the study and the
importance of local, regional and distant recurrences for tumor
control and survival were also analyzed and considered with regard
to the various types of therapy administered and the outcome for
these patients.
Patients and methods
Patients
Between January 1990 and December 1999 100 patients
with recurrent EC were consecutively registered and treated at
University Hospital (Örebro, Sweden). A total of 82 patients were
treated primarily with abdominal hysterectomy and bilateral
salpingo-oophorectomy, five patients with external radiotherapy and
brachytherapy, 13 with brachytherapy alone, and two patients with
chemotherapy. In 15 patients, lymph node sampling was performed and
in four patients lymphadenectomy was performed.
A total of 30 patients exhibited vaginal recurrences
and, in 21 patients, the first was a solitary vaginal recurrence.
In nine cases the vaginal recurrence was combined with a pelvic
recurrence or distant metastases. Furthermore, in 70 patients, the
recurrence had extra-vaginal or multiple locations. Radiotherapy
was the treatment selected for 35 patients predominantly using a
combination of external beam therapy and vaginal brachytherapy. A
total of 49 patients received chemotherapy (five in combination
with radiotherapy). In 12 patients, local surgery in combination
with chemotherapy or hormonal therapy was administered, three
patients received surgery alone and 13 patients did not receive any
treatment.
The study was approved by the Ethics Committee of
Uppsala, Sweden (Dnr 2013/136).
External radiotherapy
External beam pelvic irradiation was administered to
41 patients and vaginal brachytherapy to 91 patients. The total
external dose varied between 40.0 and 46.0 Gy (mean dose, 44.4 Gy).
The dose per fraction was 2.0 Gy with five fractions administered
per week, whereby a four-field box-technique was used. The external
treatment equipment used was 18-MV linear accelerators (Clinac IX,
Varian Medical Systems, Inc., Palo Alto, CA, USA).
Brachytherapy
A total of 13 patients were treated with
intrauterine irradiation as the definitive primary therapy, and
five patients with brachytherapy and external beam pelvic
irradiation. The total brachytherapy dose varied between 5.0 and
48.0 Gy (mean dose, 23.8 Gy). The dose per fraction varied between
2.5 and 6.0 Gy. Brachytherapy was administered using the high
dose-rate technique (MicroSelectron, Ir-192; Elekta Instrument AB,
Stockholm, Sweden). The intrauterine treatment was administered
using twin-applicators, and the vaginal treatment was administered
using plastic cylinders (20, 25 or 30 mm in diameter) whereby the
dose was specified 5 mm from the surface of the applicator. The
upper two-thirds of the vaginal walls were defined as the target
for adjuvant treatment and the whole vagina for the treatment of
recurrent disease.
Chemotherapy
A total of 49 patients received chemotherapy as the
only treatment (n=35) or in combination with radiotherapy (n=5),
hormonal therapy (n=4) or surgery (n=5). The most common
chemotherapy regimen used (n=29) was a combination of teniposide,
vincristine and cisplatin (VOP-regimen) (9). The second most common regimen (n=10)
used was carboplatin and paclitaxel. Cisplatin-cyclophosphamide and
cisplatin-doxorubicin were administered to two patients each,
single drug carboplatin was administered to two patients and single
drug cyclophosphamide was administered to four patients. The median
number of courses administered first-line was seven (range, 1–13
courses). The number of regimens used varied between one and four.
The median duration of chemotherapy treatment was 9 months (range,
1–49 months).
Follow-up
All patients were treated and followed-up at
University Hospital (Örebro, Sweden). During the first year
following treatment the patients attended regular hospital visits
every three months, then every four months during the second and
third years, every six months up to five years and, following that,
annually for up to ten years. The median follow-up time for
surviving patients was 140 months (range, 51–185 months).
Statistical analysis
For comparison of proportions, Pearson’s
χ2 test was used and, for continuous variables,
Student’s t-test was used for comparing independent groups. For
variables with dichotomous outcomes the logistic regression
analysis was used with univariate and multivariate techniques. The
Kaplan-Meier method was used for the survival analyses. Cox
proportional regression analysis was used to analyze prognostic
factors with overall or cancer-specific survival rate as the
endpoint. P<0.05 was considered to indicate a statistically
significant difference. Statistica software, version 10 (StatSoft,
Inc., Tulsa, OK, USA) was used for statistical analyses.
Results
Original stage distribution and histology
of the tumors
The median age of the 100 patients with recurrent
ECs was 70 years (range, 38–92 years). The original FIGO stage
distribution is shown in Table I. A
total of 85 tumors (85.0%) were stage I, eight tumors were stage
II, six tumors were stage III and one tumor was stage IVB.
Histological tumor type was identified as endometrioid in 90 cases
(90.0%), serous carcinoma in eight cases, with one clear cell
carcinoma and one undifferentiated carcinoma. Overall, 24
carcinomas were well differentiated, 54 moderately
well-differentiated and 22 poorly differentiated. In 36 cases, the
tumor infiltrated <50% of the myometrial thickness and, in 29
cases, the tumor infiltrated >50% (deep infiltration). In 58
tumors, the DNA ploidy was analyzed and 11 tumors (19.0%) were
identified to be aneuploid. Lymphovascular space invasion was not
regularly reported in this study of ECs. Overall, 29 carcinomas
(29.0%) were classified as low-risk, 51 carcinomas (51.0%) as
intermediate-risk and 20 carcinomas (20.0%) as high-risk.
 | Table IOriginal FIGO stage distribution and
histopathological characteristics of the tumors. |
Table I
Original FIGO stage distribution and
histopathological characteristics of the tumors.
| Parameter | n | % |
|---|
| FIGO stage |
| IA | 42 | 42.0 |
| IB | 39 | 39.0 |
| IC | 4 | 4.0 |
| IIA | 3 | 3.0 |
| IIB | 5 | 5.0 |
| IIIA | 4 | 4.0 |
| IIIC | 2 | 2.0 |
| IVB | 1 | 1.0 |
| Histology |
| Endometrioid | 90 | 90.0 |
| UPSC (serous) | 8 | 8.0 |
| Clear cell | 1 | 1.0 |
|
Undifferentiated | 1 | 1.0 |
| FIGO grade |
| Well
differentiated | 24 | 24.0 |
| Moderately
well-differentiated | 54 | 54.0 |
| Poorly
differentiated | 22 | 22.0 |
| DNA ploidy |
| Diploid | 47 | 47.0 |
| Aneuploid | 11 | 11.0 |
| Unknown | 42 | 42.0 |
| S-phase fraction
(%) | 7.3 (mean) | 1.0–20.0 (range) |
| Myometrial
invasion |
| Superficial
(<50%) | 52 | 52.0 |
| Deep (≥50%) | 48 | 48.0 |
| Risk groups |
| Low | 29 | 29.0 |
| Medium | 51 | 51.0 |
| High | 20 | 20.0 |
Primary therapy of the tumors
A total of 82 patients (82.0%) underwent primary
surgery with total abdominal hysterectomy and bilateral
salpingo-oophorectomy. Lymph node sampling was performed in 15
patients and pelvic lymphadenectomy in four patients. In 81
patients, no surgery was performed on the lymph nodes. A total of
41 patients (41.0%) received radiotherapy as primary radiotherapy
or adjuvant postoperative pelvic irradiation, and 91 patients
(91.0%) received vaginal brachytherapy as a primary therapy or
postoperative adjuvant therapy. Furthermore, 11 patients received
adjuvant chemotherapy due to high-risk factors. With the exception
of three, all patients achieved primary cure (97.0%) of their
ECs.
Pattern of recurrences
A single vaginal recurrence was diagnosed as the
first recurrence in 21 cases (21.0%). A vaginal and pelvic
recurrence was diagnosed in two cases; in one case a combined
vaginal and abdominal recurrence occurred, and in one case the
sites of relapse included the vagina, pelvis and lungs. In an
additional five cases, the vaginal recurrences were combined with
multiple distant recurrences to the lymph nodes, liver and lungs.
Overall, 30 vaginal recurrences were identified and, of these, 21
recurrences were solitary vaginal relapses. Pelvic recurrences were
recorded in 16 cases, abdominal recurrences in 24 cases and distant
recurrences in 59 cases. The median time period from diagnosis to
the first recurrence was 32 months (range, 5–217 months).
In 45 patients (45.0%), a second recurrence was
diagnosed, whereby six cases were identified as a novel vaginal
recurrence and, in 39 cases, recurrence occurred at regional or
distant sites, including the pelvis, abdomen, lymph nodes, liver,
lungs, bone and central nervous system. The median time period
between the first and second recurrence was 12 months (range, 1–146
months). In 12 patients (12.0%), a third relapse was recorded, four
at the vaginal site and eight at various distant sites. The median
time period between the second and third recurrence was 13 months
(range, 3–70 months). Four cases experienced a forth relapse (all
distant) and one patient exhibited a fifth relapse with metastasis
to the pelvis and liver.
Response rates
The overall response rate of the patients was 28.6%
(22/77 patients). In the group treated with radiotherapy, the
response rate was 87.5% (21/24 patients) and, in the chemotherapy
group, the response rate was 33.3% (12/36 patients). In the group
receiving other types of therapy, such as surgery or hormonal
treatment, the response rate was 5.9%.
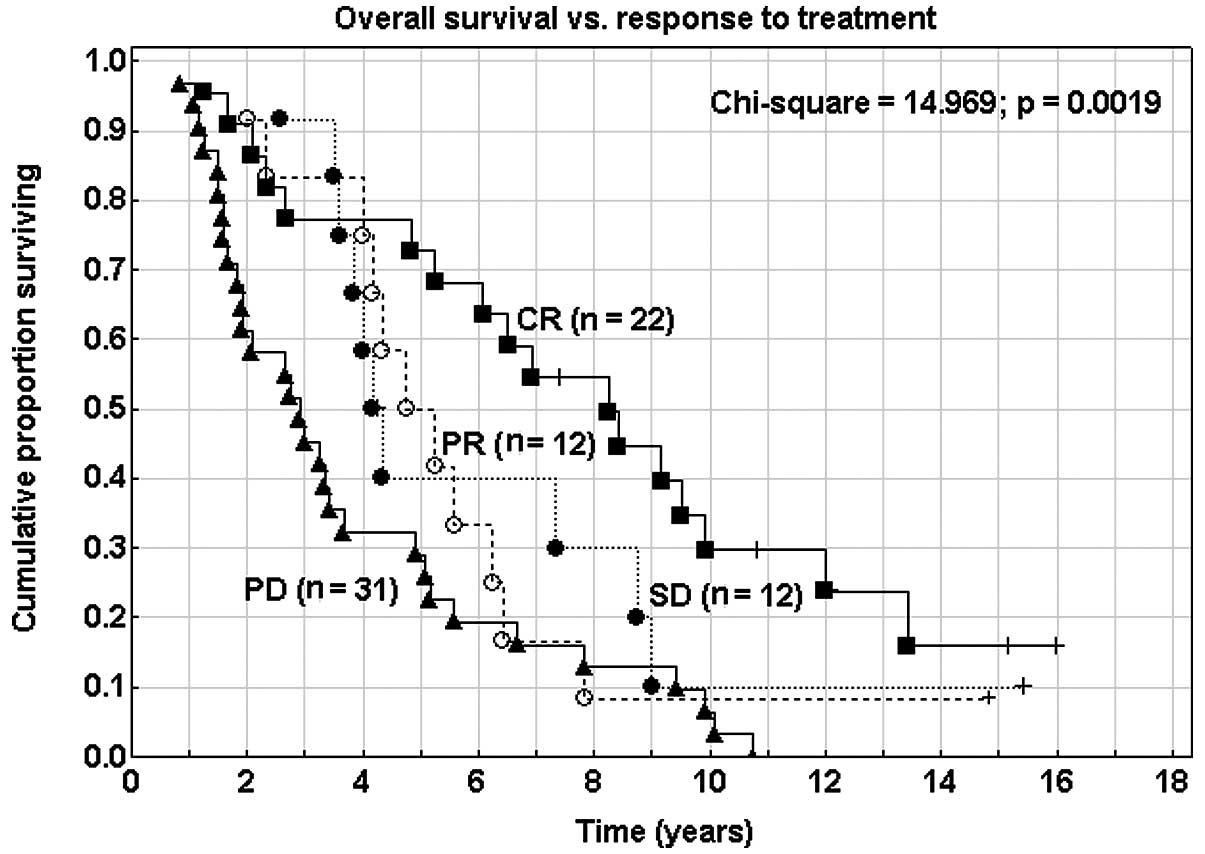
Response to administered therapy was significantly
associated with the overall survival rate (P=0.002; Fig. 1). Patients achieving complete
remission (CR) exhibited a 72.7% five-year survival rate whereas
patients who did not achieve CR exhibited a survival rate of
35.7%.
Local tumor control
The five-year local (vaginal) control rate was
88.3%. A total of 12 novel vaginal recurrences occurred during the
follow-up period. Thus, 40.0% (12/30) vaginal recurrences recurred
once. For the treatment of the first vaginal recurrence, 15 out of
21 patients received radiotherapy, external beam irradiation and
vaginal brachytherapy in combination, and 14 of these patients
(93.3%) achieved local control of the vaginal tumor. In six
patients with vaginal recurrences, additional treatment types, such
as surgery and chemotherapy, were administered; however only two of
these patients (33.3%) achieved complete local control
(P<0.001).
In the group of 15 patients achieving complete
remission, 10 novel recurrences were identified as a second
recurrence and, in three cases (20.0%), a novel vaginal recurrence
was diagnosed. In seven cases, distant recurrences to the liver,
lungs, lymph nodes and bone were identified. During the follow-up,
an additional three recurrences were identified as a third
recurrence (vagina plus pelvis and lung) and as a forth recurrence
(vagina plus abdomen).
Survival data of the patients
At the time of follow-up 10 patients (10.0%) had
survived, 77 patients had succumbed to the disease, and 13 patients
had succumbed to intercurrent diseases. The median follow-up time
for surviving patients was 140 months (range, 51–185 months).
The overall five-year survival rate of the patients
was 43.9% [95% confidence interval (CI), 34.1–53.7%] and the
cancer-specific survival rate was 47.0% (95% CI, 37.0–57.0%).
Females exhibiting vaginal recurrences alone exhibited an increased
overall survival rate (61.9%) when compared with females with
recurrences at other sites (39.0% at five years); however, no
significant differences were identified (P=0.286). Patients with
FIGO stage III tumors exhibited a five-year overall survival rate
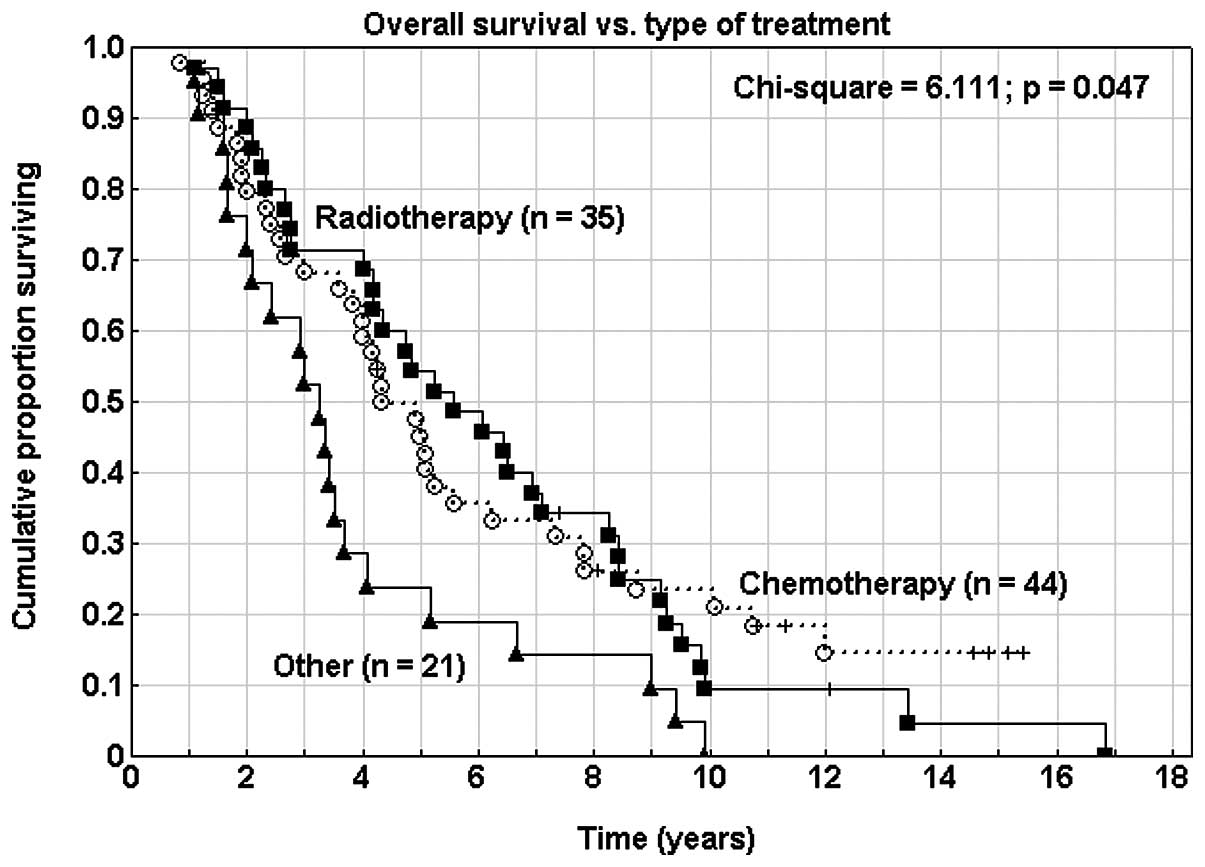
of 35.3%. Overall survival rate was significantly associated with
treatment type of the recurrent disease (P=0.047). Patients who did
not receive radiotherapy or chemotherapy (n=21) exhibited a
decreased overall survival rate (Fig.
2). Furthermore, no significant difference was identified
between overall survival of patients treated with surgery alone
(n=3), hormonal therapy alone (n=5) or with no active therapy
(n=13) (P=0.425). The overall five-year survival rate of patients
following the first recurrence was 19.2% (95% CI, 11.3–26.1%) and
the median survival time was 14.8 months. In the group that did not
receive radiotherapy or chemotherapy, the survival rate was 5.4%
(P<0.001). No significant difference in survival rate was
identified between patients treated with radiotherapy, chemotherapy
or a combination of the two.
Cox proportional regression analyses
In univariate Cox proportional regression analysis,
patient age, time to recurrence (TTR), FIGO- and nuclear grade of
the tumor, the risk group and response to therapy were
significantly associated with overall survival rate. However, the
original tumor stage, DNA ploidy, myometrial infiltration and lymph
node surgery (sampling or lymphadenectomy) were not associated with
the survival rate in this study (Table
II). Patient age (P<0.001), time interval to recurrence
(P<0.001), FIGO grade (P=0.048), nuclear grade of the tumor
(P=0.001) and response to therapy (P<0.001) were also identified
as significant prognostic factors in multivariate Cox analysis with
regard to overall survival rate (Table III). The site of recurrence was
not found to be significant with regard to overall survival
rate.
 | Table IIUnivariate Cox proportional regression
analyses. Prognostic factors of the primary tumor and the
recurrence for overall survival rate. |
Table II
Univariate Cox proportional regression
analyses. Prognostic factors of the primary tumor and the
recurrence for overall survival rate.
| Prognostic
factor | β | Standard error | Risk ratio | 95% confidence
interval | P-value |
|---|
| Age (per year) | 0.033 | 0.013 | 1.034 | 1.009–1.060 | 0.008 |
| Primary tumor |
| FIGO-stage (per
stage) | 0.021 | 0.163 | 1.021 | 0.742–1.406 | 0.898 |
| FIGO-grade (3 vs.
1–2) | 0.633 | 0.265 | 1.883 | 1.119–3.168 | 0.017 |
| Nuclear grade (3 vs.
1–2) | 1.088 | 0.353 | 2.968 | 1.487–5.925 | 0.002 |
| DNA ploidya | 0.155 | 0.343 | 1.168 | 0.597–2.285 | 0.651 |
| Infiltrationb | 0.218 | 0.247 | 1.244 | 0.767–2.018 | 0.376 |
| Risk groups (3 vs.
1–2) | 0.898 | 0.263 | 2.454 | 1.465–4.112 | <0.001 |
| Lymph node
surgeryc | 0.311 | 0.258 | 1.364 | 0.823–2.261 | 0.229 |
| External beam
RTc | 0.214 | 0.215 | 1.238 | 0.812–1.888 | 0.321 |
| Vaginal RTc | −0.031 | 0.354 | 0.970 | 0.485–1.940 | 0.930 |
| Adjuvant
chemotherapyc | 0.498 | 0.324 | 1.645 | 0.872–3.103 | 0.124 |
| Recurrence |
| Time to recurrence
(months) | −0.013 | 0.004 | 0.988 | 0.980–0.995 | 0.002 |
| Treatment (CT vs.
RT) | −0.048 | 0.232 | 0.953 | 0.605–1.503 | 0.837 |
| Treatment
responsed | 1.595 | 0.323 | 4.927 | 2.618–9.273 | <0.001 |
| Site of
recurrencee | 0.208 | 0.247 | 1.232 | 0.760–1.996 | 0.398 |
| Number of
recurrences | −0.110 | 0.128 | 0.896 | 0.697–1.151 | 0.389 |
 | Table IIIMultivariate Cox proportional
regression analysis. Prognostic factors of the primary tumor and
the recurrence for overall survival rate. |
Table III
Multivariate Cox proportional
regression analysis. Prognostic factors of the primary tumor and
the recurrence for overall survival rate.
| Prognostic
factor | β | Standard error | Risk ratio | 95% confidence
interval | P-value |
|---|
| Patient |
| Age (per
year) | 0.046 | 0.013 | 1.047 | 1.021–1.074 | <0.001 |
| Primary tumor |
| FIGO-gradea | 0.544 | 0.275 | 1.723 | 1.004–2.956 | 0.048 |
| Nuclear
gradea | 1.272 | 0.391 | 3.569 | 1.660–7.674 | 0.001 |
| Recurrence |
| Time to
recurrencec | −0.022 | 0.005 | 0.978 | 0.969–0.988 | <0.001 |
| Treatment
responseb | 1.595 | 0.323 | 4.927 | 2.618–9.273 | <0.001 |
No significant difference in overall survival rate
was identified between patients that received external beam therapy
as part of their primary treatment and patients that received
surgery alone or surgery in addition to vaginal brachytherapy
(P=0.322). Adjuvant vaginal brachytherapy was not associated with
overall survival rate (P=0.927). In addition, the probability of
achieving complete vaginal remission was higher (100.0 vs. 67.3%)
in the group receiving no adjuvant brachytherapy as part of the
first-line treatment; however, no significant differences were
identified (P=0.269). Type of treatment for the recurrences in the
complete series is presented in Table
IV.
 | Table IVTreatment of the recurrences of the
complete series (n=100). |
Table IV
Treatment of the recurrences of the
complete series (n=100).
| Treatment | n | % |
|---|
| Surgery | 12 | 12.0 |
| ± Radiotherapy or
chemotherapy | | |
| Radiotherapy | 35 | 35.0 |
| External beam
therapy + vaginal brachytherapy | | |
| Chemotherapy | 49 | 49.0 |
| ± Surgery,
radiotherapy or hormonal therapy | | |
| Hormonal
therapy | 10 | 10.0 |
| ± Radiotherapy or
chemotherapy | | |
| No active
treatment | 13 | 13.0 |
Predictive and prognostic factors for
treatment outcome
The primary risk group of the tumor was also
significantly associated with the outcome of the treatment of the
vaginal recurrence. A total of 73.4% of patients with tumors
belonging to a low-risk group achieved complete remission, 42.1% in
the medium risk group and 0.0% in the high-risk group.
In addition, TTR was significantly associated with
overall survival rate (P=0.002). The risk of mortality decreased
2.1% per month with increasing TTR. This was also observed for
cancer-specific survival rate (P=0.001) and local (vaginal) and
locoregional (vaginal or pelvic) recurrences in separate analyses
(P<0.001).
Discussion
EC has a favorable prognosis, however, 10–15%
patients relapse (10) and the
five-year overall survival rate is 80% (11). It has become common to identify
three risk groups (high, medium and low) among EC patients with
different survival and recurrence rates, as well as different
patterns of recurrence. Vaginal recurrences are the most frequent
type of recurrences in all risk groups and also the type of relapse
that is possible to cure if diagnosed early (8,12). The
risk group distribution for high-, medium- and low-risk groups was
20, 51 and 29%, respectively. The endometrioid type constituted 90%
of the cases and 22% were poorly differentiated. A total of 91
patients (91%) received postoperative adjuvant brachytherapy and 41
patients (41%) received external beam irradiation to the pelvic
region.
In 21 patients, single vaginal recurrences were
diagnosed and, in nine patients, vaginal relapse in combination
with pelvic, abdominal, liver, lung or lymph node metastases was
identified. The median time between diagnosis and recurrence was 32
months, which is consistent with previous studies (3). A second recurrence was recorded in 45
patients (45%), whereby six were vaginal and 39 were regional or
distant. In 17 patients, ≥3 recurrences were recorded. The median
time between the first and the second recurrence was 12 months.
In the present study, 76% (16/21 patients) vaginal
recurrences achieved primary cure. Following a combination of
brachytherapy and external beam therapy a cure rate of 93% was
achieved. However, in the group receiving other therapies, only 33%
achieved local control and this was significantly lower than that
in the radiotherapy group. Hasbini et al reported the same
local control rate in a study of 23 patients (13). Among 10 patients with a second,
third or fourth vaginal recurrence, seven patients succumbed to the
disease. The five-year cumulative local control rate was 67%. This
was comparable to the results of Pai et al (14), whereby a 90% complete response rate
and a 74% 10-year cumulative local control rate was reported in a
series of 20 patients. Furthermore, Jhingran et al (6) reported a five-year local control rate
of 69% in a study of 91 patients. In the PORTEC-1 trial, 35
isolated vaginal recurrences were treated with curative intent
(external radiotherapy and brachytherapy, and in some cases
surgery), and 89% achieved complete remission and 77% achieved
long-term remission (4). In a study
of 22 patients with isolated vaginal recurrences, Petignat et
al (15) reported an 100%
complete response rate whereby no patients exhibited locoregional
recurrences. However, Hart et al (16) reported a 54% failure rate following
radiotherapy in 26 tumor recurrences. Brachytherapy was not used as
a routine treatment in these patients. External beam therapy with
or without adjuvants is not sufficient to replace vaginal
brachytherapy in the treatment of vaginal relapses. In the present
study, nine cases of distant metastasis (30%) were identified with
the vaginal recurrence as the first recurrence and during follow-up
and, following treatment, an additional 15 regional or distant
recurrences (50%) were identified. Therefore, 52% (11/21) isolated
vaginal recurrences recurred distantly following locoregional
treatment with radiotherapy (17).
The overall five-year survival rate of the patients
was 44% and the cancer-specific survival was 47%. In a study by
Wylie et al (18), of 58
recurrences, an overall survival rate of 53% and a local control
rate of 65% were identified. Lin et al (5) also reported a rate of 53% in a study
of 50 patients. Colombo et al (19) reported a 57% survival rate without
evidence of disease between three and 11 years following treatment.
By contrast, Blecharz et al (20) reported a five-year overall survival
rate of only 42% in 47 patients that received treatment for vaginal
recurrences and the corresponding rate for pelvic recurrences was
13%. A similar survival rate was reported by Jhingran et al
(6), with 43% overall survival at
five years. Creutzberg et al (4) identified a difference in survival
following the treatment of vaginal relapses between two groups with
or without prior external radiotherapy (PORTEC-1 study); the
five-year survival rates were 43 and 65%, respectively. However, in
the present study, such a difference in survival rate was not
identified. TTR for all recurrences was a significant prognostic
factor for cancer-specific and overall survival rate but not for
patients with locoregional relapses. In addition, Robbins et
al (3) reported that a TTR of
<18 months was associated with shorter overall and
cancer-specific survival, but only in patients with extra-pelvic
recurrence.
In univariate Cox analyses, FIGO grade, nuclear
grade, the original risk group of the tumor (low-, medium- or
high-risk), TTR and response type, as well as patient age were
statistically significant prognostic factors for overall survival
rate. However, in multivariate analysis only age, FIGO grade,
nuclear grade, TTR and type of response (complete remission) were
found to be independent and significant prognostic factors for
overall survival rate. This was also identified for cancer-specific
survival rate. Furthermore, previous studies have identified
additional predictive and prognostic factors. Lin et al
(5) reported that age, FIGO grade
and size of the recurrence were significant predictors of overall
survival. In addition, Blecharz et al (20) found that recurrence site (vaginal
versus pelvic recurrences) was the only independent prognostic
factor for five-year overall survival. Hasbini et al
(13) revealed that extra-vaginal
extension, tumor size and stage of initial disease had a
significant impact on the prognosis. Smaniotto et al
(21) presented a scoring system
(time between surgery and recurrence, pelvic wall site, positive
lymph nodes, hemoglobin levels <11 g/dl) to identify patients
benefiting from treatment. Patients with a low score (<2)
exhibited a significantly improved outcome, local control of the
disease and overall survival when compared with patients with a
score of ≥2. Jhingran et al (6) found that external beam irradiation in
addition to brachytherapy versus single modality therapy was
significant in univariate analysis with regard to overall survival
rate. In a multivariate study of 73 endometrial cancer recurrences,
Jereczek et al (7) reported
that only the stage of recurrent disease and a high total
irradiation dose were found to correlate with improved
survival.
Toxicity was not evaluated in this study. However,
from previous studies using similar treatment techniques of vaginal
recurrences 14% grade 3 toxicity of the vagina and 11% grade 3–4
gastrointestinal toxicity was recorded (22). Pai et al (14) reported a late complication rate of
15% and no grade 3 or 4 late complications. Petignat et al
(15) reported 18% late grade 3–4
gastrointestinal toxicity and 50% grade 3 vaginal toxicity. Nag
et al (23) reported 13
patients with interstitial brachytherapy for salvage of vaginal
recurrence, whereby all tumors were locally controlled; however,
long-term morbidity was 15%, including vaginal ulceration,
colorectal fistula and grade 2 proctitis.
An important conclusion from the present study was
that radiotherapy (high-dose rate vaginal brachytherapy and
external beam irradiation) is an important part of the therapy to
achieve local tumor control. However, survival is dependent on
extra-vaginal tumor localization and, in this study, 79% of
patients exhibited regional or distant metastases at diagnosis and
50% of local recurrences showed novel recurrences at distant sites
during the follow-up period. With regard to locoregional
recurrences, 63% were part of a generalized, extra-pelvic tumor
spread at diagnosis or during follow-up. This may provide an
explanation for the failure of locoregional adjuvant therapy for
prolonging survival despite improved locoregional tumor control.
This failure was also evident in the treatment of recurrent
disease, as shown in the present study. Radiotherapy exhibited the
highest locoregional control rate (71%); however, survival was
similar to chemotherapy-treated patients with 11% complete clinical
remission.
In conclusion, in the current study, 21% of patients
exhibited single vaginal recurrences and 93% of cases were cured
using combined radiotherapy (external beam irradiation in
combination with vaginal brachytherapy). Thus, 79% of patients
exhibited regional or distant metastases at the diagnosis of the
first recurrence and 52% of the primary isolated vaginal
recurrences recurred as distant metastases. Age, tumor grade, TTR
and therapy responses were significant prognostic factors.
Locoregional control was achieved by radiotherapy; however,
survival was similar to that with chemotherapy alone and was
significantly improved when compared with other types of therapy or
no active treatment.
Acknowledgments
The authors would like to thank Mr. Peter Jansson
for working on the database and retrieving the patient data, and
Mrs. Elisabeth Peippo for secretarial support and data management,
University Hospital (Örebro Sweden).
References
|
1
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2012. CA Cancer J Clin. 62:10–29. 2012.
|
|
2
|
Sohaib SA, Houghton SL, Meroni R, Rockall
AG, Blake P and Reznek RH: Recurrent endometrial cancer: patterns
of recurrent disease and assessment of prognosis. Clin Radiol.
62:28–34; discussion 35–36. 2007.
|
|
3
|
Robbins JR, Yechieli R, Laser B, Mahan M,
Rasool N and Elshaikh MA: Is time to recurrence after hysterectomy
predictive of survival in patients with early stage endometrial
carcinoma? Gynecol Oncol. 127:38–42. 2012.
|
|
4
|
Creutzberg CL, van Putten WL, Koper PC,
Lybeert ML, Jobsen JJ, Wárlám-Rodenhuis CC, De Winter KA, Lutgens
LC, van den Bergh AC, van der Steen-Banasik E, et al: PORTEC Study
Group: Survival after relapse in patients with endometrial cancer:
results from a randomized trial. Gynecol Oncol. 89:201–209.
2003.
|
|
5
|
Lin LL, Grigsby PW, Powell MA and Mutch
DG: Definitive radiotherapy in the management of isolated vaginal
recurrences of endometrial cancer. Int J Radiat Oncol Biol Phys.
63:500–504. 2005.
|
|
6
|
Jhingran A, Burke TW and Eifel PJ:
Definitive radiotherapy for patients with isolated vaginal
recurrence of endometrial carcinoma after hysterectomy. Int J
Radiat Oncol Biol Phys. 56:1366–1372. 2003.
|
|
7
|
Jereczek-Fossa B, Badizo A and Jassem J:
Recurrent endometrial cancer after surgery alone: results of
salvage radiotherapy. Int J Radiat Oncol Biol Phys. 48:405–413.
2000.
|
|
8
|
Sorbe B, Horvath G, Andersson H, Boman K,
Lundgren C and Pettersson B: External pelvic and vaginal
irradiation versus vaginal irradiation alone as postoperative
therapy in medium-risk endometrial carcinoma - a prospective
randomized study. Int J Radiat Oncol Biol Phys. 82:1249–1255.
2012.
|
|
9
|
Sorbe B, Wolmesjö E and Frankendal B:
VM-26-vincristine-cisplatin combination chemotherapy in the
treatment of primary advanced and recurrent endometrial carcinoma.
Obstet Gynecol. 73:343–348. 1989.
|
|
10
|
Morrow CP, Bundy BN, Kurman RJ, Creasman
WT, Heller P, Homesley HD and Graham JE: Relationship between
surgical-pathological risk factors and outcome in clinical stage I
and II carcinoma of the endometrium: a Gynecologic Oncology Group
Study. Gynecol Oncol. 40:55–65. 1991.
|
|
11
|
Creasman WT, Odicino F, Maisonneuve P,
Quinn MA, Beller U, Benedet JL, et al: Carcinoma of the corpus
uteri, FIGO 26th Annual Report on the Results of Treatment in
Gynecological Cancer. Int J Gynaecol Obstet. 95(Suppl 1):
S105–S143. 2006.
|
|
12
|
Ng TY, Perrin LC, Nicklin JL, Cheuk R and
Crandon AJ: Local recurrence in high-risk node-negative stage I
endometrial carcinoma treated with postoperative vaginal vault
brachytherapy. Gynecol Oncol. 79:490–494. 2000.
|
|
13
|
Hasbini A, Haie-Meder C, Morice P, Chirat
E, Duvillard P, Lhommé C, Delapierre M and Gerbaulet A: Outcome
after salvage radiotherapy (brachytherapy +/− external) in patients
with a vaginal recurrence from endometrial carcinomas. Radiother
Oncol. 65:23–28. 2002.
|
|
14
|
Pai HH, Souhami L, Clark BG and Roman T:
Isolated vaginal recurrences in endometrial carcinoma: treatment
results using high-dose-rate intracavitary brachytherapy and
external beam radiotherapy. Gynecol Oncol. 66:300–307. 1997.
|
|
15
|
Petignat P, Jolicoeur M, Alobaid A, Drouin
P, Gauthier P, Provencher D, Donath D and Van Nguyen T: Salvage
treatment with high-dose-rate brachytherapy for isolated vaginal
endometrial cancer recurrence. Gynecol Oncol. 101:445–449.
2006.
|
|
16
|
Hart KB, Han I, Shamsa F, Court WS, Chuba
P, Deppe G, Malone J, Christensen C and Porter AT: Radiation
therapy for endometrial cancer in patients treated for
postoperative recurrence. Int J Radiat Oncol Biol Phys. 41:7–11.
1998.
|
|
17
|
Corn BW, Lanciano RM, D’agostino R,
Kiggundu E, Dunton CJ, Purser P and Greven KM: The relationship of
local and distant failure from endometrial cancer: defining a
clinical paradigm. Gynecol Oncol. 66:411–416. 1997.
|
|
18
|
Wylie J, Irwin C, Pintilie M, Levin W,
Manchul L, Milosevic M and Fyles A: Results of radical radiotherapy
for recurrent endometrial cancer. Gynecol Oncol. 77:66–72.
2000.
|
|
19
|
Colombo A, Cormio G, Placa F, Landoni F,
Ardizzoia A, Gabriele A and Lissoni A: Brachytherapy for isolated
vaginal recurrences from endometrial carcinoma. Tumori. 84:649–651.
1998.
|
|
20
|
Blecharz P, Brandys P, Urbański K,
Reinfuss M and Patla A: Vaginal and pelvic recurrences in stage I
and II endometrial carcinoma - survival and prognostic factors. Eur
J Gynaecol Oncol. 32:403–407. 2011.
|
|
21
|
Smaniotto D, D’Agostino G, Luzi S,
Valentini V, Macchia G, Mangiacotti MG, Margariti PA, Ferrandina G
and Scambia G: Concurrent 5-fluorouracil, mitomycin C and
radiation, with or without brachytherapy, in recurrent endometrial
cancer: a scoring system to predict clinical response and outcome.
Tumori. 91:215–220. 2005.
|
|
22
|
Sorbe B and Söderström K: Treatment of
vaginal recurrences in endometrial carcinoma by high-dose-rate
brachytherapy. Anticancer Res. 33:241–247. 2013.
|
|
23
|
Nag S, Yacoub S, Copeland LJ and Fowler
JM: Interstitial brachytherapy for salvage treatment of vaginal
recurrences in previously unirradiated endometrial cancer patients.
Int J Radiat Oncol Biol Phys. 54:1153–1159. 2002.
|