Introduction
Diagnosis and treatment of superior vena cava (SVC)
syndrome, resulting from clear cell renal cell carcinoma, is a
challenge in clinical practice. SVC syndrome is a complication
caused by obstruction of the SVC (either compressed or internally
obstructed) and/or compression of the heart. Management of the SVC
syndrome induced by malignant conditions is based on anticancer
therapy and the relief of symptoms (1). Renal carcinoma has a high frequency of
renal vein and inferior vena cava extension. The efficacy and
safety of treatments for renal carcinoma with SVC involvement
requires clarification in future studies. The present case study
describes the case of a patient who presented with a large,
malignant thrombosis of the SVC and received intensity-modulated
radiation therapy following an intra-atrial tumor thrombus
resection, which resulted in stable local control.
Case report
On 16th March 2012, a 49-year-old female who
experienced symptoms of exertional dyspnea and increased fatigue
for 15 months presented at the Department of Cardiac Surgery,
Xinqiao Hospital (Chongqing, China). The patient reported dyspnea,
which developed following activity and sleeping in the supine
position, which gradually worsened, without chest pain, heavy
sweating and palpitations. The patient additionally reported poor
sleep and a loss of appetite, although no marked weight loss. Two
days prior to the the patient presenting at the hospital, the
described symptoms worsened and the patient experienced bilateral
edema in the lower limbs. Physical examination revealed cyanosis,
an enlarged heart and a weakened cardiac sound. A transesophageal
echocardiography demonstrated a right atrial mass originating in
the inferior vena cava (IVC; size, 14×8 cm) that caused a tricuspid
inflow obstruction and the abdomen ultrasonic examination
demonstrated a mass in the lower right kidney. An emergency
resection of the intra-atrial tumor thrombus was performed. Frozen
sections obtained from the intra-atrial surgery revealed abundant
necrosis with heterotypic cells. The intra-atrial tumor thrombus
was tightly attached to the abdominal aorta, therefore, only a
partial resection could be performed to relieve the tricuspid
obstruction. Histological examination confirmed the diagnosis of a
clear cell renal cell carcinoma, however, the patient’s symptoms
had partially subsided following a month of recovery. The patient
refused a right nephrectomy, and interleukin-2 and interferon-α
therapy, as well as additional types of targeted therapy. The
patient underwent intensity-modulated radiation therapy (56 Gy/24
fractions of one fraction per day, five days a week; from the IVC,
where the mass initiated, to the iliac vein, which included the
mass on the upper kidney). Following this, the patient refused
further therapy. Six months following the radiation therapy, the
symptoms had markedly improved, thus enhancing the patient’s
quality of life; furthermore, the edema in the lower limbs had
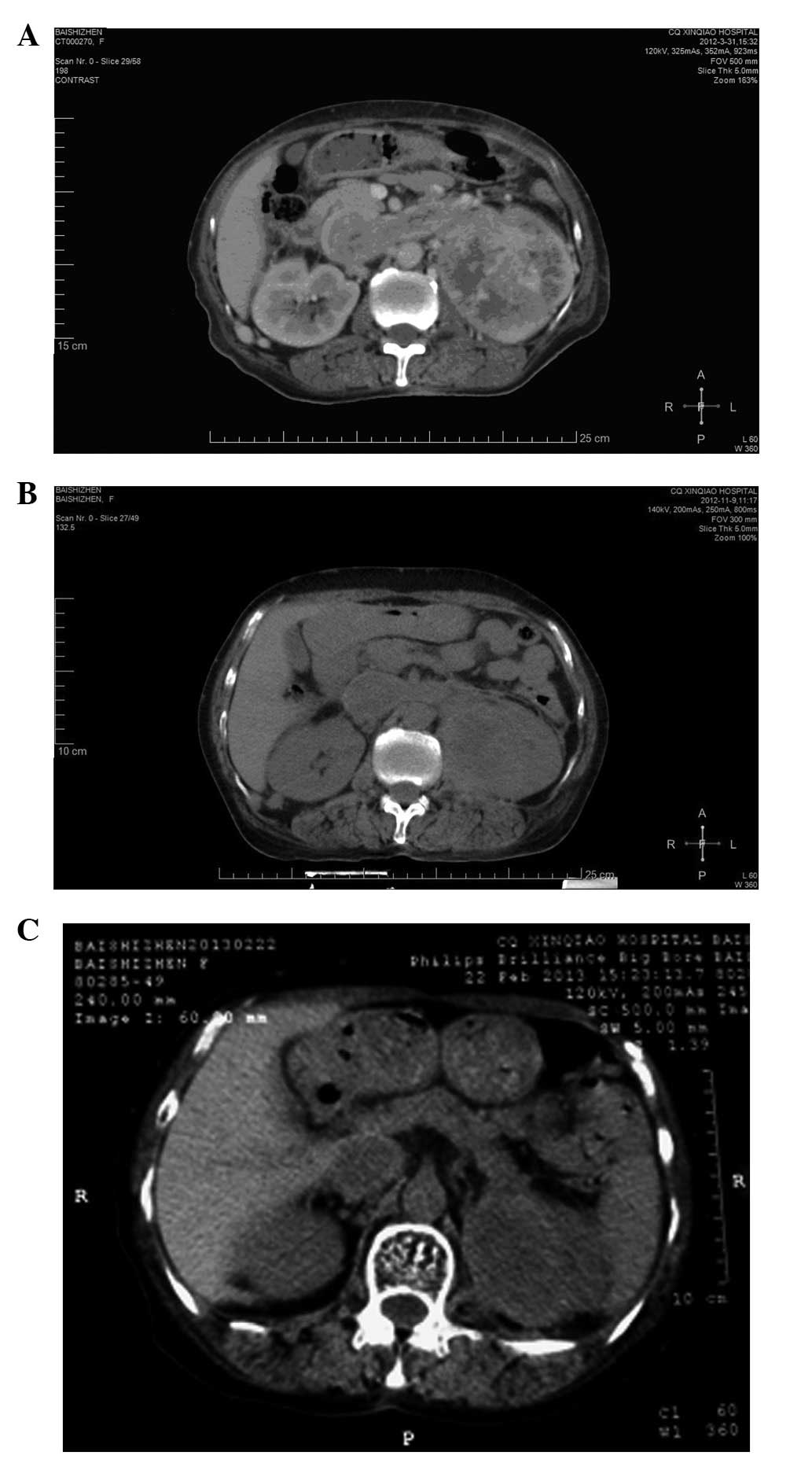
disappeared. On the 9th November 2012 and the
22nd February 2013, computed tomography (CT) indicated
that the tumors on the kidney and IVC were stable (Fig. 1), however, additional metastatic
lesions were identified in both lungs. Patient provided written
informed consent.
Discussion
SVC syndrome is difficult to treat, due to the
complications associated with the pathology and the limited data
that is available. The majority of reports for SVC are case studies
and randomized trials are rare. In addition to treatment strategies
to relieve symptoms, chemotherapy, surgical intervention and
radiation therapy are commonly adopted methods of treatment;
however, the control rate of the disease remains poor (2). According to previous reports,
percutaneous placement of an intravascular stent, which offers
rapid relief of the symptoms, is the most common intervention, due
to its low level of complexity and low mortality rate (3). Surgical bypass grafting is an
alternative approach that is more suitable in patients with no
original malignancies or with malignancies that are not sensitive
to treatment (4). A sternotomy or
thoracotomy with extensive resection and reconstruction of the SVC
are additional common therapeutic strategies (5).
More than 90% of SVC syndromes are attributable to a
malignancy. Carcinoma of the bronchus is the most common cause, as
well as lymphoma, germ-cell cancer, metastatic disease, thymoma and
mesothelioma. The majority of SVC syndrome cases are caused by
radiation-sensitive tumors (1),
therefore, these particular patients may benefit from radiotherapy.
It is generally considered that the treatment of clear cell renal
cell carcinoma by radiation therapy is ineffective, however,
metastatic lesions have been reported to be sensitive to and safe
to treat using radiation therapy. Svedman et al (6) conducted a prospective phase II trial
using extracranial stereotactic radiotherapy in primary and
metastatic clear cell renal cell carcinomas. This treatment method
was shown to achieve local control in 98% of treated lesions
(6). Furthermore, a retrospective
analysis demonstrated the feasibility of stereotactic radiosurgery
(SRS)-based treatment of brain metastases originating from clear
cell renal cell carcinoma in obtaining central nervous system
control (7). These data indicated
that radiotherapy may be a potential therapeutic strategy for clear
cell renal cell carcinoma.
Sunitinib is a small molecule inhibitor that has
been shown as an effective first-line therapeutic agent for
metastatic clear cell renal cell carcinoma. Chiba et al
(8) and Harshman et al
(9) administered sunitinib (dose,
50 mg) as a neoadjuvant therapy in patients with clear cell renal
cell carcinoma and a thrombus of the vena cava. The vena cava
thrombus noticeably shrank following treatment (8). However, Cost et al (10) reported that targeted molecular
therapy produced a minimal clinical effect on clear cell renal cell
carcinoma thrombi. Consistently, a retrospective analysis of 14
patients by Bigot et al (11) showed that neoadjuvant targeted
management therapy yielded a limited response on clear cell renal
cell carcinoma patients with an IVC thrombus.
In conclusion, additional data are required to
determine the efficacy of radiation therapy for the treatment of
clear cell renal cell carcinoma-induced vena cava thrombi.
References
|
1
|
Wilson LD, Detterbeck FC and Yahalom J:
Clinical practice. Superior vena cava syndrome with malignant
causes. N Engl J Med. 356:1862–1869. 2007.
|
|
2
|
Rowell NP and Gleeson FV: Steroids,
radiotherapy, chemotherapy and stents for superior vena caval
obstruction in carcinoma of the bronchus. Cochrane Database Syst
Rev. 4:CD0013162001.
|
|
3
|
Urruticoechea A, Mesía R, Domínguez J, et
al: Treatment of malignant superior vena cava syndrome by
endovascular stent insertion. Experience on 52 patients with lung
cancer. Lung Cancer. 43:209–214. 2004.
|
|
4
|
Kennedy DP and Palit TK: Reconstruction of
superior vena cava syndrome due to benign disease using superficial
femoral vein. Ann Vasc Surg. 24:555.e7–555.e12. 2010.
|
|
5
|
Lequaglie C, Conti B, Brega-Massone PP and
Giudice G: The difficultapproach to neoplastic superior vena cava
syndrome: surgical option. J Cardiovasc Surg (Torino). 44:667–671.
2003.
|
|
6
|
Svedman C, Sandström P, Pisa P, et al: A
prospective Phase II trial of using extracranial stereotactic
radiotherapy in primary and metastatic renal cell carcinoma. Acta
Oncol. 45:870–875. 2006.
|
|
7
|
Samlowski WE, Majer M, Boucher KM, et al:
Multidisciplinary treatment of brain metastases derived from clear
cell renal cancer incorporating stereotactic radiosurgery. Cancer.
113:2539–2548. 2008.
|
|
8
|
Chiba H, Hirose T, Shimoda N and Kanagawa
K: A case of advanced renal cell carcinoma with inferior vena cava
thrombus treated with sunitinib as neoadjuvant therapy. Nihon
Hinyokika Gakkai Zasshi. 103:623–626. 2012.(In Japanese).
|
|
9
|
Harshman LC, Srinivas S, Kamaya A and
Chung BI: Laparoscopicradical nephrectomy after shrinkage of a
caval tumor thrombus with sunitinib. Nat Rev Urol. 6:338–343.
2009.
|
|
10
|
Cost NG, Delacroix SE Jr, Sleeper JP, et
al: The impact of targeted molecular therapies on the level of
renal cell carcinoma vena caval tumor thrombus. Eur Urol.
59:912–918. 2011.
|
|
11
|
Bigot P, Fardoun T, Bernhard JC, et al:
Neoadjuvant targeted molecular therapies in patients undergoing
nephrectomy and inferior vena cava thrombectomy: is it useful?
World J Urol. 32:109–114. 2014.
|