Introduction
Malignant melanoma (MM), a common neoplasm of the
skin and mucous membranes, constitutes 1% of all cancer cases
(1). In total, 5% of melanocytic
malignancies in females occur in the vulva, with rare cases
detected in the ovary, uterus or uterine cervix (2). MM commonly clinically presents at an
advanced stage, and the diagnosis is confirmed by histological
examination using certain staining techniques and by
immunohistochemical analysis (3).
The majority of patients respond poorly to therapy (4). Certain therapeutic regimens are
recommended for cervical melanoma, including radical hysterectomy
with pelvic lymph node dissection, and partial vaginectomy followed
by radiation therapy with either intracavitary or external beam
radiation, or the two treatments combined. However, the majority of
patients exhibit poor long-term survival (5). Written informed consent was obtained
from the patient.
Case report
In June 2011, a female who presented with a one-week
history of bleeding from the vagina was admitted to the Shanghai
Tenth People’s Hospital (Shanghai, China). A gynecological
examination revealed a ulcero-proliferative lesion that measured
1×2.5 cm2 on the anterior lip of the cervix. The
parametrium was not involved and the growth was primarily
restricted to the cervix. An incisional biopsy was performed and
the sample sent for histopathological examination. The lesion
histopathology revealed a malignant neoplasm, which indicated the
possibility of a primary uterine cervical melanoma. The chest X-ray
and abdominopelvic computed tomography results were normal. The
patient was administered chemotherapy consisting of 20
mg/m2 intravenous cisplatin, 250 mg/m2
dacarbazine and 1 mg/m2 vincristine in each cycle, and
received two such cycles at four week intervals.
The patient then underwent radical hysterectomy with
bilateral salpingo-oophorectomy and pelvic lymphadenectomy. A
specimen of the uterus, cervix and vaginal cuff with bilateral
attached adnexae, and a pelvic lymph node dissection specimen were
received for analysis. Gross examination revealed a
4×2.5-cm2 ulcero-proliferative lesion in the cervix. The
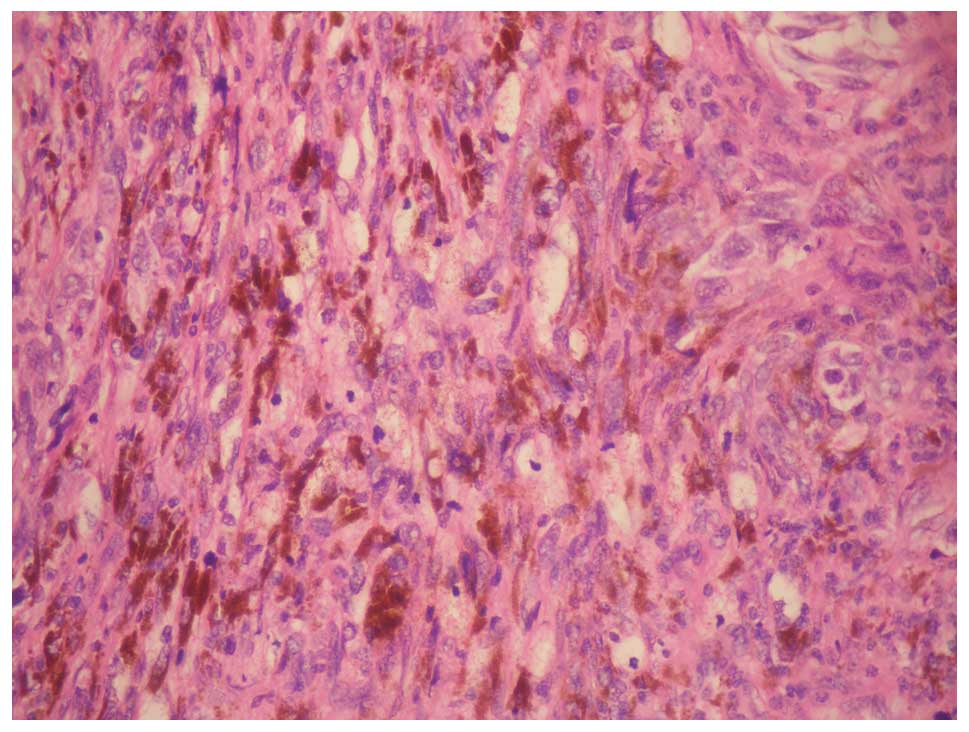
microscopic features of the specimen were comparable with those
observed in the pre-operative biopsy (Fig. 1). The final diagnosis for the
patient was International Federation of Gynecology and Obstetrics
stage IB1 melanoma of the cervix with no lymph node metastasis.
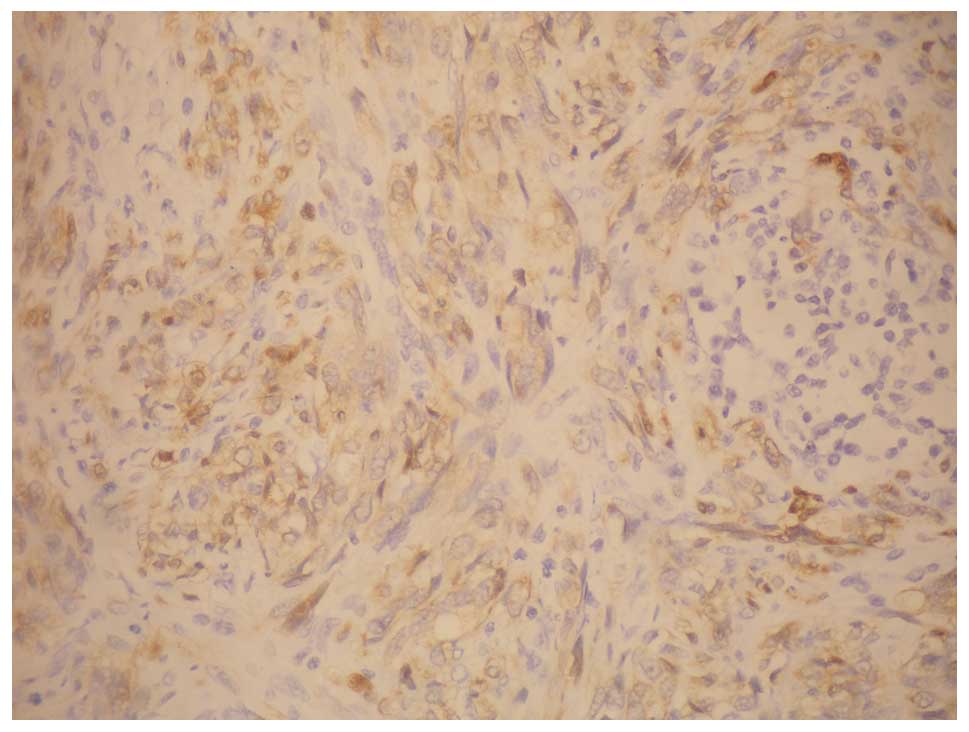
Immunohistochemistry revealed diffuse positive reactions for S-100
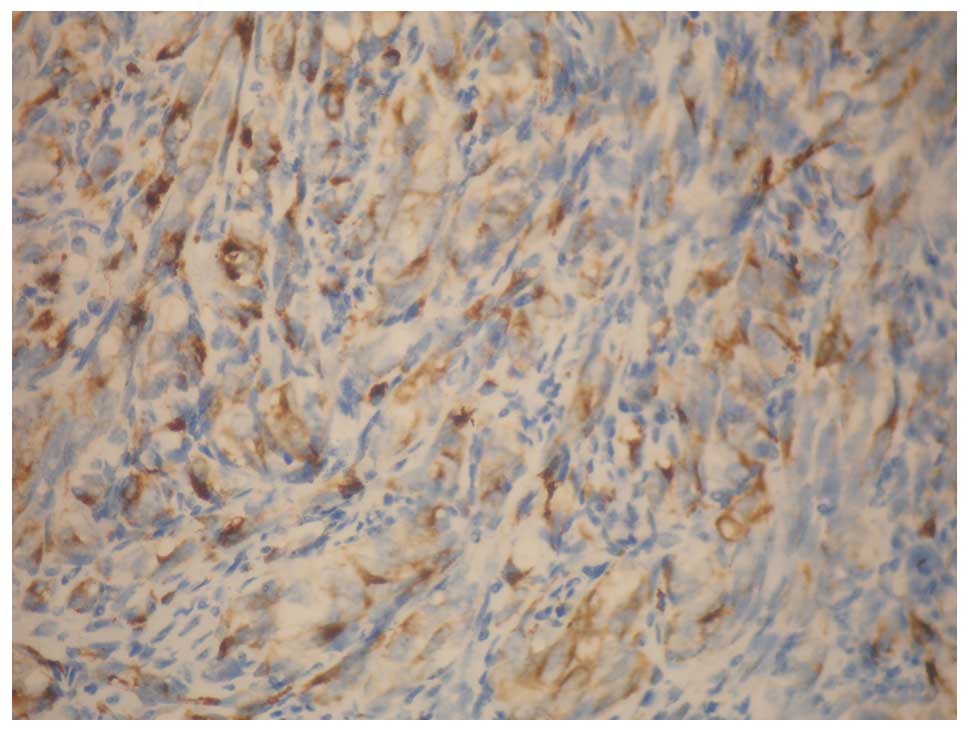
protein (Fig. 2), human melanoma
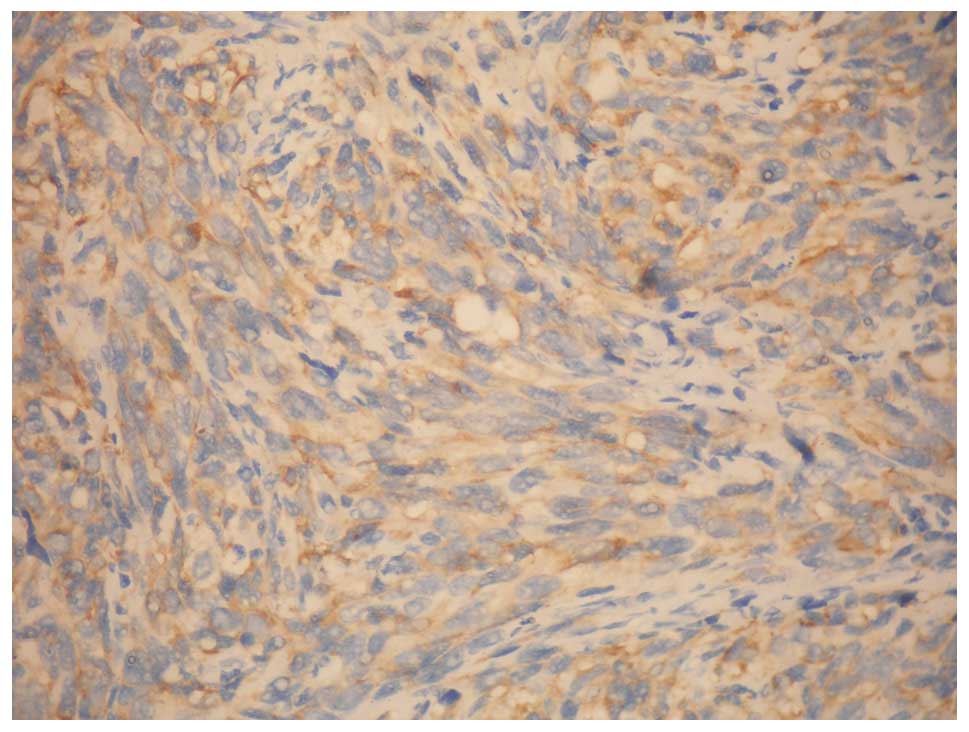
black 45 (HMB-45; Fig. 3) and
melanoma antigen recognized by T-cells (Fig. 4), which confirmed the diagnosis of
MM, with no reaction for epithelial markers, namely high molecular
weight-cytokeratin and epithelial membrane antigen.
A comprehensive assessment for melanotic lesions in
the uveal tract (opthalmoscopy), skin and other mucosal
sites was negative. A pre-operative abdominal ultrasound
examination revealed that the structures of the spleen, liver,
bowel, kidneys and retroperitoneum were normal. Since a primary
melanoma and epitheliotropism of the melanoma cells was not
present, a diagnosis of primary cervical melanoma was reached.
Subsequently, the patient received one cycle of combination
chemotherapy with dacarbazine, cisplatin and vincristine. This
regimen was followed by chemotherapy using 20 mg/m2
intravenous cisplatin and 250 mg/m2 dacarbazine between
days 1 and 3 in each cycle, for four such cycles at four week
intervals. The final chemotherapy cycle was administered in January
2012. The patient was kept under close observation and has been
well for 30 months without recurrence subsequent to surgery. The
most recent imaging results, including chest X-ray and
abdominopelvic computed tomography results, were normal. The
patient has subsequently had regular follow-up assessments.
Discussion
Primary melanoma of the cervix is a rare condition.
A total of 5% melanocytic malignancies in females occur in the
vulva, with rare malignancies also detected in the ovary, uterus
and uterine cervix (2). Cervical
melanoma is hypothesized to arise from the cervical melanocytic
cells. The entire spectrum of melanocytic lesions, including blue
nevi, benign lentigines and melanomas, are known to occur in the
cervix (4). As the peak incidence
of primary carcinoma of the uterine cervix occurs between 40 and 50
years of age, this places the patient in the present case study,
aged 65 years, in an older age group, although whether prognosis
depends on the age of the patient is not known.
Diagnosis of cervical MM is usually determined by
gynecological examination, histopathology and electron microscopy,
and is confirmed by immunohistochemical staining with S-100 and
HMB-45. As the cervix was not previously considered to contain
melanocytes, the possibility of cervical melanoma was controversial
for a long period of time. Therefore, ruling out the diagnosis of
melanoma elsewhere in the body prior to the diagnosis of primary
cervical melanoma is important. Furthermore, the cervix is not a
common site for metastatic malignancies, due to a limited blood
supply and the poor nature of the cervical fibrous stroma site for
tumor growth. Morris and Taylor (6)
suggested the following diagnostic criteria: (i) The presence of
melanin in the normal cervical epithelium; (ii) the absence of
melanoma anywhere else in the body; (iii) the demonstration of
junctional change in the cervix; and (iv) metastases according to
the pattern of cervical carcinoma.
Little consensus has been achieved with regard to
what is the most effective approach in terms of the clinical
management of MM of the uterine cervix. Radical hysterectomy is the
most common procedure (5,7–9). The
recommended treatment is usually surgery, including radical
hysterectomy, pelvic lymphadenectomy and partial vaginectomy
(10). Although the benefit of
lymphadenectomy is controversial, this treatment should be
advocated in cases with large growth of the tumor and the presence
of pigmented lymph nodes, which signifies a higher risk of
secondary metastases. Post-operative chemotherapy is a further
viable treatment option in these cases, as numerous patients
develop metastatic disease (11).
Dacarbazine, a drug that has been demonstrated to reduce tumor size
in patients with cutaneous MM, may have potential in cervical MM
treatment (11). In the present
case study, a combination of dacarbazine, cisplatin and vincristine
was advocated, with which the patient remained disease-free for a
minimum of 29 months following surgery.
The prognosis of primary cervical MM is usually
poor. Survival times are variable, but usually range between 0.1
month and 14 years. Studies have indicated that 87.5% patients
succumb to the disease within three years of diagnosis (10). In one study of 78 patients, although
the majority of patients were diagnosed at an early stage, only two
survived >5 years (10).
In conclusion, cytopathologists should be aware of
this type of lesion upon evaluation of cervical smear cytology in
order to provide an early diagnosis of cervical MM. Radical
hysterectomy with bilateral salpingo-oophorectomy and pelvic
lymphadenectomy is advisable for surgical treatment. Chemotherapy
may be also considered in patients following surgery.
References
|
1
|
Morrow CP and DiSaia PJ: Malignant
melanoma of the female genitalia: a clinical analysis. Obstet
Gynecol Surv. 31:233–271. 1976.
|
|
2
|
Kedzia W, Sajdak S, Kedzia H and
Spaczynski M: Primary melanoma of the uterine cervix in a 19 year
old woman-case report. Ginekol Pol. 68:386–389. 1997.(In
Polish).
|
|
3
|
Ariel IM: Malignant melanoma of the female
genital system: a report of 48 patients and review of literature. J
Surg Oncol. 16:371–383. 1981.
|
|
4
|
Dematos P, Tyler D and Seigler HF: Mucosal
melanoma of the female genitalia: a clinicopathologic study of
forty-three cases at Duke University Medical Center. Surgery.
124:38–48. 1998.
|
|
5
|
Cantuaria G, Angioli R, Nahmias J, Estape
R and Penalver M: Primary malignant melanoma of the uterine cervix:
case report and review of the literature. Gynecol Oncol.
75:170–174. 1999.
|
|
6
|
Morris HJ and Taylor HB: Melanomas of the
vagina. Am J Clin Pathol. 46:420–426. 1966.
|
|
7
|
Santoso JT, Kucera PR and Ray J: Primary
malignant melanoma of the uterine cervix: two case reports and a
century’s review. Obstet Gynecol Surv. 45:733–740. 1990.
|
|
8
|
Jones HW III, Droegmueller W and Makowski
EL: A primary melanocarcinoma of the cervix. Am J Obstet Gynecol.
111:959–963. 1971.
|
|
9
|
Genton CY, Kunz J and Schreiner WE:
Primary malignant melanoma of the vagina and cervix uteri. Report
of a case with ultrastructural study. Virchows Arch A Pathol Anat
Histol. 393:245–250. 1981.
|
|
10
|
Pusceddu S, Bajetta E, Carcangiu ML,
Formisano B, Ducceschi M and Buzzoni R: A literature overview of
primary cervical malignant melanoma: An exceedingly rare cancer.
Crit Rev Oncol Hematol. 81:185–195. 2012.
|
|
11
|
Kristiansen SB, Anderson R and Cohen DM:
Primary malignant melanoma of the cervix and review of the
literature. Gynecol Oncol. 47:398–403. 1992.
|