Introduction
There are two peaks of osteosarcoma incidence, as
determined by population-based surveillance (1). The first is during adolescence, and
the later peak is in the eighth decade. Neoadjuvant and adjuvant
chemotherapy protocols have improved long-term survival,
particularly in young patients with osteosarcoma. In
population-based data, the relative five-year survival rates are
61.6, 58.7, and 24.2% in osteosarcoma patients aged 0–24, 25–59 and
60–85 years, respectively (1), with
older patients having a poorer prognosis. Malignant fibrous
histiocytoma (MFH) and dedifferentiated chondrosarcoma are known to
occur in elderly patients (2,3).
Phase II studies of single agents and combinations
of drugs have documented the efficacy of methotrexate (MTX),
doxorubicin (DXR) and cisplatin (CDDP) in advanced osteosarcoma
(4–6), leading to randomized studies
confirming the efficacy of adjuvant chemotherapy (7,8). This
three-drug combination represents the standard care for
osteosarcoma. Ifosfamide (IFM), in studies with other agents, has
been shown to exhibit significant activity in recurrent or
metastatic osteosarcoma (9,10). However, IFM did not improve the
degree of tumor necrosis in a study of patients with osteosarcoma
who were treated with a neoadjuvant MTX, DXR, and CDDP regimen,
with or without IFM (11).
Neoadjuvant and adjuvant chemotherapy protocols have
not been established specifically for adult and older patients with
bone sarcomas. Furthermore, the completion rate of regimens that
have included CDDP and/or MTX has been reported to be low in this
population (12,13). High completion rates of neoadjuvant
and adjuvant chemotherapy with DXR and IFM have been reported in
older patients with soft-tissue sarcoma (14,15).
The present study was undertaken to determine the safety and
efficacy of neoadjuvant and adjuvant chemotherapy with DXR and IFM
for bone sarcoma in adult and older patients.
Patients and methods
Patients
Patients with bone sarcoma treated with neoadjuvant
and adjuvant chemotherapy in four Nagoya Musculoskeletal Oncology
Group Hospitals (Nagoya University Hospital, Aichi Cancer Center
Hospital, Aichi Cancer Center Aichi Hospital and Nagoya Memorial
Hospital) in Japan between January 2004 and February 2011 were
reviewed. Patients aged >40 years with osteosarcoma and MFH of
the bone were prospectively treated with IFM+DXR in these
institutions. Other bone sarcomas in patients of all ages were
treated with IFM+DXR according to the attending physician’s
decision. After obtaining a waiver of patient informed consent
requirements from the institutional review board, 18 consecutive
patients with bone sarcoma were retrospectively reviewed. This
study was approved by the ethics committee of Nagoya University
Graduate School and School of Medicine (Nagoya, Japan).
Patient characteristics and treatment
regimens
Baseline demographic and clinical characteristics
are listed in Table I. The study
group consisted of 12 males and six females, with a median age of
63 years (range, 28–76 years). Histological subtypes were
osteosarcoma (n=10), MFH of the bone (n=4), dedifferentiated
chondrosarcoma (n=3) and angiosarcoma of the bone (n=1). According
to the staging system of the American Joint Committee on Cancer
(16), there were four patients of
stage IIA, ten of stage IIB, one of stage IVA and three of stage
IVB. The timing of chemotherapy was neoadjuvant and adjuvant in
seven patients, neoadjuvant only in seven and adjuvant only in
four. The median number of cycles of chemotherapy was 4 (range,
1–7). Patients were treated with neoadjuvant and/or adjuvant
chemotherapy with 50–60 mg/m2 DXR and 6–10
g/m2 IFM every 3–4 weeks.
 | Table IBaseline demographics and clinical
characteristics. |
Table I
Baseline demographics and clinical
characteristics.
| Characteristic | Value |
|---|
| Gender, n (%) |
| Male | 12 (66) |
| Female | 6 (34) |
| Histological subtype,
n (%) |
| Osteosarcoma | 10 (56) |
| MFH of the bone | 4 (22) |
| Dedifferentiated
chondrosarcoma | 3 (17) |
| Angiosarcoma of the
bone | 1 (6) |
| AJCC stage, n
(%) |
| IIA | 4 (22) |
| IIB | 10 (56) |
| IVA | 1 (6) |
| IVB | 3 (17) |
| Definitive treatment,
n (%) |
| Surgery | 15 (83) |
| Heavy ion
radiation | 1 (6) |
| Surgery and heavy
ion radiation | 1 (6) |
| Inoperable with
PD | 1 (6) |
| Site of definitive
treatment (n=17), n (%) |
| Primary,
extremity | 9 (53) |
| Primary, trunk | 5 (29) |
| Primary and
metastasis | 2 (12) |
| Solitary distant
recurrence | 1 (6) |
| Timing of
chemotherapy, n (%) |
| Neoadjuvant
only | 7 (39) |
| Adjuvant only | 4 (22) |
| Neoadjuvant and
adjuvant | 7 (39) |
| Median age, years
(range) | 63 (28–76) |
| Median number of
chemotherapy cycles (range) | 4 (1–7) |
| Median follow up,
months (range) | 18.0 (4.6–73.7) |
Treatment analysis
Side-effects were graded according to the Common
Terminology Criteria for Adverse Events v4.0 (17). The treatment efficacies were
evaluated according to Response Evaluation Criteria In Solid Tumors
(RECIST) v1.1 analysis of magnetic resonance imaging (18), necrosis rate of resected tumor and
patient outcome.
Statistical analysis
The overall survival (OS) rate from definitive
treatment was calculated using Kaplan-Meier product limit methods.
A log-rank test was used to identify differences in survival rates
between groups. P<0.05 was used to indicate a statistically
significant difference.
Results
Definitive treatments
One patient with metastasis could not undergo
definitive surgery due to disease progression during neoadjuvant
chemotherapy. The sites of definitive treatment for the primary
tumors were the femur (n=4), tibia (n=3), humerus (n=2), pelvis
(n=2), sternum (n=2) and spine (n=1) in patients without
metastasis. The metastatic sites of definitive treatment for
patients with metastatic tumors were the lung only (n=1), the lymph
nodes only (n=1), and the bone and soft tissues (n=1). Definitive
treatments were surgery in 15 cases, heavy ion radiation in one
case and surgery and heavy ion radiation in one case each. Sites of
definitive treatment were primary of the extremity in nine cases,
primary of the trunk in five, primary and metastasis in two, and
solitary distant recurrence in one.
Treatment response
Evaluation with RECIST for the treatment site showed
that the responses following neoadjuvant chemotherapy, with a
median number cycles of 3.5 (range, 1–5), were stable disease (SD)
in 11 cases (79%) and progressive disease (PD) in three (21%)
(Table II). Of the 12 patients
with SD and PD, there were five (42%) with tumor necrosis of ≥90%
(Table II). The final status was
no evidence of disease in nine cases (50%), alive without disease
in two (11%) and dead of disease in seven (39%), at a median
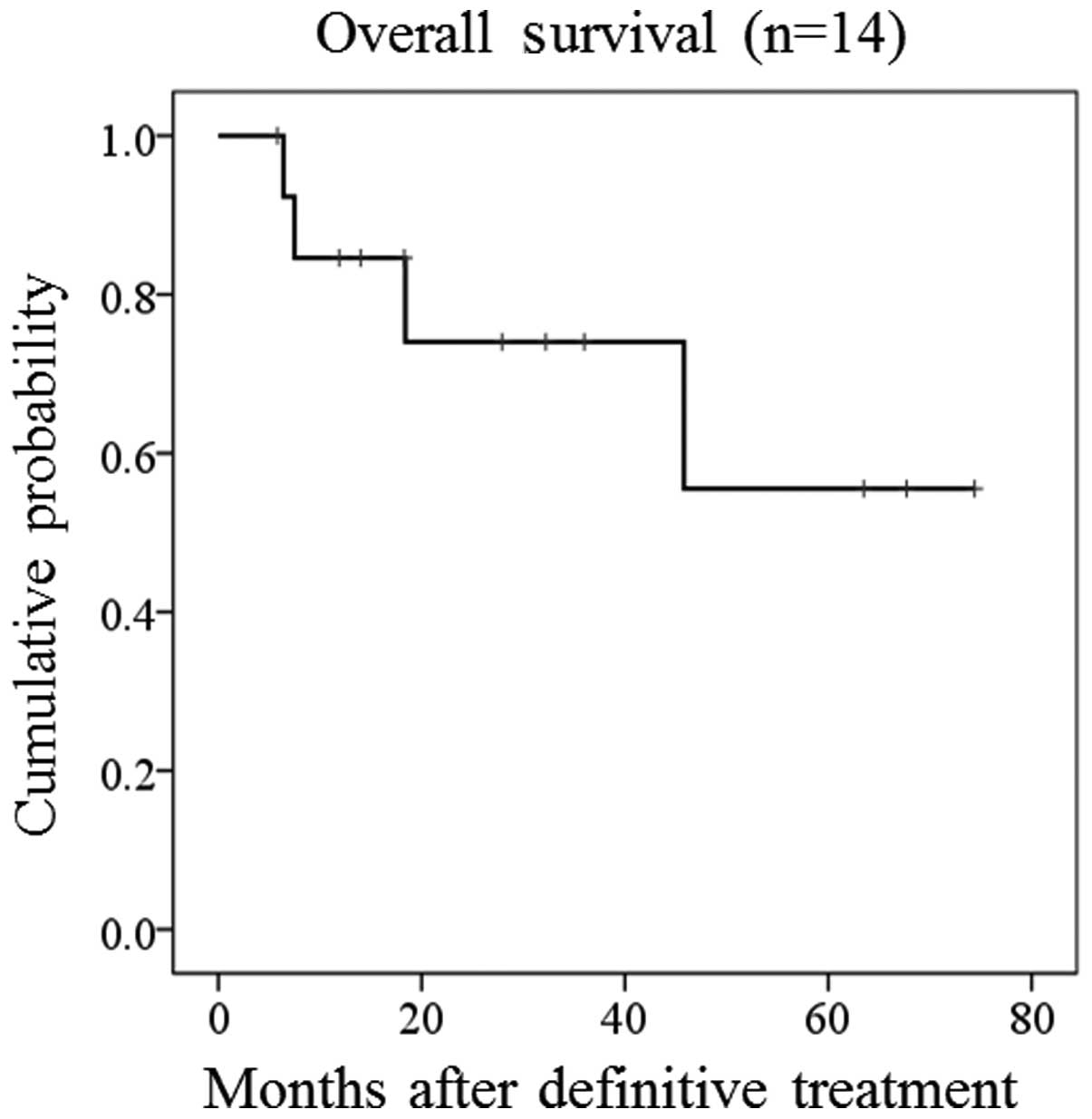
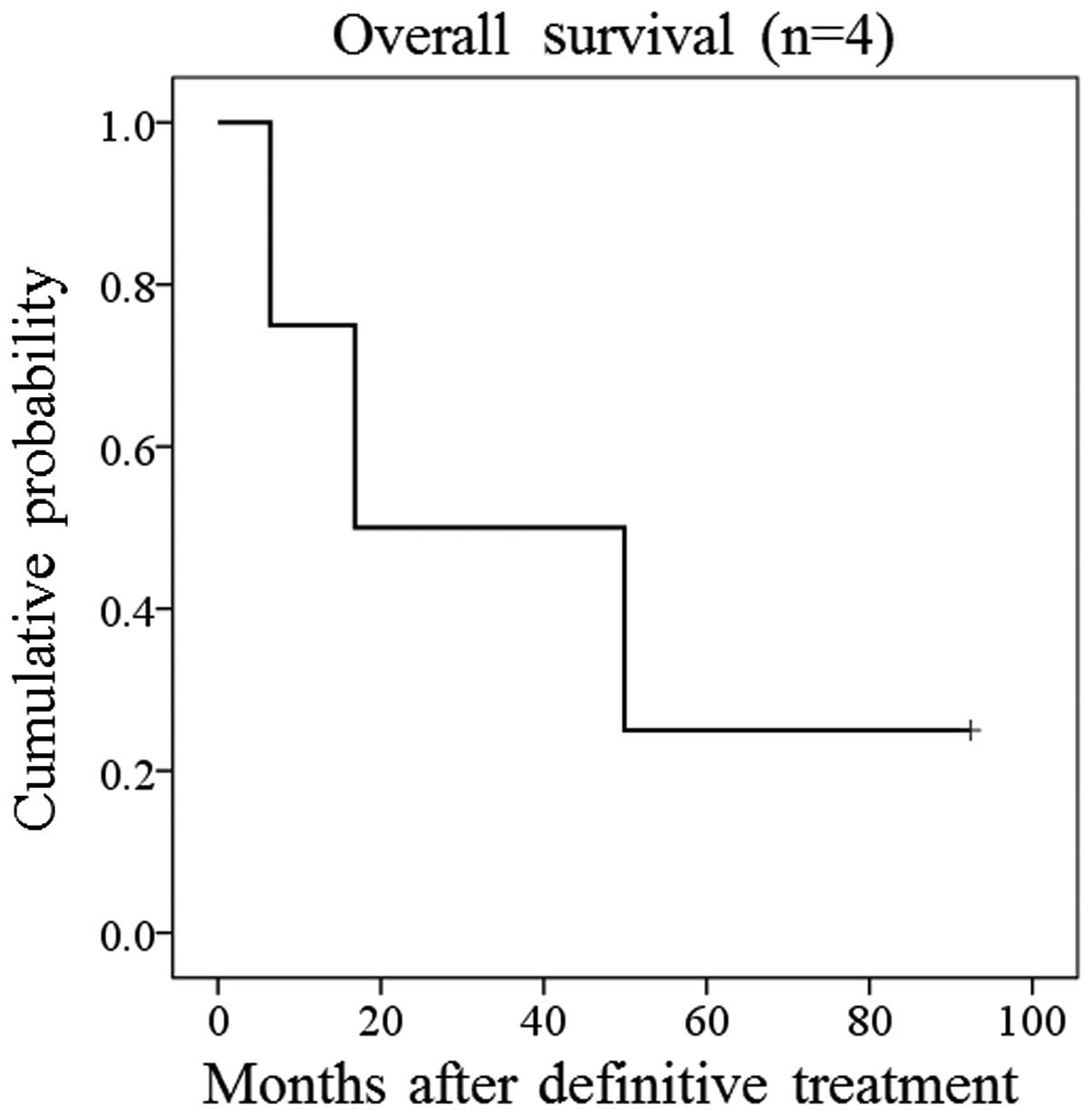
follow-up time of 18.0 months (range, 4.6–73.7 months) (Table II). Estimated five-year OS rates
for patients without and with metastasis prior to treatment were
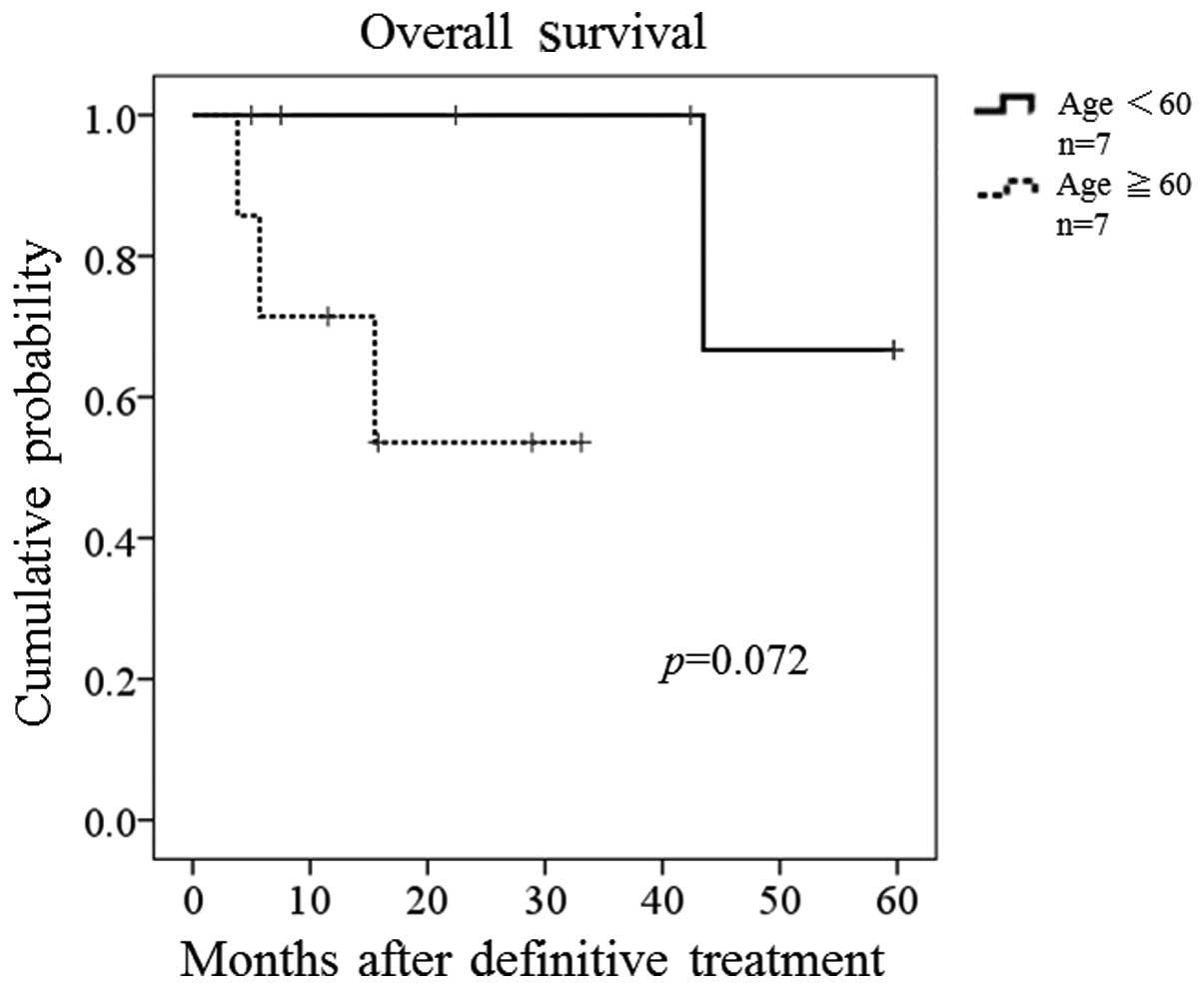
56% (Fig. 1) and 25% (Fig. 2), respectively (Table II). Estimated two-year OS rates for
patients without metastasis were 100% in patients aged <60
years, and 54% in patients >60 years (P=0.072 between the two
groups) (Fig. 3).
 | Table IIEfficacy data. |
Table II
Efficacy data.
| Response
category | Value |
|---|
| RECIST response
(n=14), n (%) |
| SD | 11 (79) |
| PD | 3 (21) |
| Tissue response in SD
and PD (n=12), n (%) |
| Necrosis ≥90% | 5 (42) |
| Necrosis
<90% | 7 (58) |
| Final status (n=18),
n (%) |
| NED | 9 (50) |
| AWD | 2 (11) |
| DOD | 7 (39) |
| Estimated five-year
OS rate, % |
| AJCC stage II | 56 |
| AJCC stage IV | 25 |
One patient discontinued chemotherapy due to a
temporarily depressed level of consciousness with arrhythmia (grade
2). Major grade 3 or 4 side-effects included leukopenia in 14 cases
(78%), anemia in seven (39%), thrombocytopenia in three (17%),
nausea in two (11%), and febrile neutropenia in two (11%).
Cardiotoxicity was not observed in the follow-up periods.
Discussion
The number of aged osteosarcoma patients is
increasing (19,20). Chemotherapy with DXR, CDDP and
high-dose MTX has become a standard neoadjuvant and adjuvant
treatment for osteosarcoma of young patients. However, older
patients have been reported to receive less chemotherapy and have a
poorer outcome (19). Since the
completion rate of regimens, including CDDP and/or MTX, has been
reported to be low in middle-aged and older bone sarcoma patients
(12,13), a chemotherapeutic regimen with DXR
and IFM was prospectively applied to adult and older patients with
bone sarcomas in the present study. This regimen has already been
widely used for adult patients with soft-tissue sarcoma (15,21).
In the present study, only one patient discontinued chemotherapy
due to a temporarily depressed level of consciousness with
arrhythmia, suggesting that the combination of DXR and IFM is well
tolerated, even in patients >60 years (22).
High-dose IFM treatment was reported to be
associated with a higher incidence of azoospermia (23). However, this is less of a
disadvantage with respect to infertility in the case of older
patients. DXR-induced cardiotoxicity has been reported in the
long-term follow-up of osteosarcoma (24); however no cardiotoxicity was noted
in the present study, albeit within only a short median follow-up
period of 18.0 months (range, 4.6–73.7 months).
Bramwell et al reported that adjuvant and/or
neoadjuvant chemotherapy is beneficial in patients with MFH of the
bone (13). The merit of adjuvant
and/or neoadjuvant chemotherapy for dedifferentiated chondrosarcoma
has not been proven (3). However,
the present study performed adjuvant chemotherapy with IFM and DXR
due to the poor outcome in patients with the sarcoma.
Previous studies have demonstrated ≥90% tumor
necrosis in 21–48% of cases following neoadjuvant chemotherapy in
osteosarcoma patients aged >40 years (12,19,25,26).
In a study on MFH of the bone, ≥90% tumor necrosis was observed in
42% of patients subsequent to chemotherapy (13). In the present study, the responses
following neoadjuvant chemotherapy were SD in 11 cases and PD in
three. Five of 12 patients (42%) with bone sarcoma had ≥90%
necrosis, and the efficacy of this treatment was acceptable.
In studies on neoadjuvant and/or adjuvant
chemotherapy for non-metastatic osteosarcoma of an extremity, the
estimated five-year OS rate was reported as 55–70% in patients aged
40–60 years (12,25) and 51% in patients >40 years
(19). In MFH of the bone, the
five-year OS rate following neoadjuvant and/or adjuvant
chemotherapy was 59% in non-metastatic patients with a median age
of 42 years (range, 14–62 years) (13). In non-metastatic patients aged
<60 years who underwent limb salvage for dedifferentiated
chondrosarcoma, the five-year OS rates were reported as 25% in
those who did not have chemotherapy compared with 45% in those who
did. However, no significant difference was noted between these
groups on univariate analysis (3).
In the present study, even though there were five tumors located in
the axial skeleton and nine in the extremities, and the median age
of the patients was 63 years (range, 28–76 years), the five-year OS
rate of 56% was comparable to that of previous reports regarding
bone sarcoma in patients without metastasis (3,12,13,19,25).
There were certain limitations to the present study.
The first was the diversity of the chemotherapy dose and cycles
based on the attending physician’s decision. A combination regimen
with DXR (60 mg/m2) and IFM (10 g/m2) was
typically selected, used in four cycles prior to surgery and two
cycles subsequent to surgery, but certain cases were treated with
different doses and cycles according to the attending physician’s
decision. The second limitation was the short follow-up periods in
this study. In particular, the follow-up periods in the older
patients were short, and did not allow calculation of the estimated
OS rate at five years in this population. Furthermore, the study
was unable to evaluate cardiotoxicity over a long follow-up period.
Finally, the study included various bone sarcomas, including
osteosarcoma, cases of adult and older patients, and extremity and
trunk sites. However, the results may be useful in demonstrating
the clinical features of bone sarcoma of various subtypes, sites
and age in actual practice.
In conclusion, the estimated five-year OS rate and
necrosis rate following neoadjuvant and adjuvant chemotherapy with
DXR and IFM for bone sarcomas in this study were acceptable in
patients without metastasis prior to treatment. A better
coordinated prospective study of this combination regimen for aged
patients with bone sarcoma will be required to clarify its efficacy
and tolerability.
Acknowledgements
Funding was granted from the Ministry of Education,
Culture, Sports, Science and Technology of Japan (Grant-in-Aid for
Scientific Research, no. 24791533). The authors would like to thank
Miss. Eri Ishihara for providing secretarial assistance.
References
|
1
|
Mirabello L, Troisi RJ and Savage SA:
Osteosarcoma incidence and survival rates from 1973 to 2004: data
from the Surveillance, Epidemiology, and End Results Program.
Cancer. 115:1531–1543. 2009.
|
|
2
|
Weiss SW and Enzinger FM: Malignant
fibrous histiocytoma: an analysis of 200 cases. Cancer.
41:2250–2266. 1978.
|
|
3
|
Grimer RJ, Gosheger G, Taminiau A, et al:
Dedifferentiated chondrosarcoma: prognostic factors and outcome
from a European group. Eur J Cancer. 43:2060–2065. 2007.
|
|
4
|
Cores EP, Holland JF, Wang JJ and Sinks
LF: Doxorubicin in disseminated osteosarcoma. JAMA. 221:1132–1138.
1972.
|
|
5
|
Jaffe N, Paed D, Farber S, et al:
Favorable response of metastatic osteogenic sarcoma to pulse
high-dose methotrexate with citrovorum rescue and radiation
therapy. Cancer. 31:1367–1373. 1973.
|
|
6
|
Ochs JJ, Freeman AI, Douglass HO Jr, Higby
DS, Mindell ER and Sinks LF: cis-Dichlorodiammineplatinum (II) in
advanced osteogenic sarcoma. Cancer Treat Rep. 62:239–245.
1978.
|
|
7
|
Link MP, Goorin AM, Miser AW, et al: The
effect of adjuvant chemotherapy on relapse-free survival in
patients with osteosarcoma of the extremity. N Eng J Med.
314:1600–1606. 1986.
|
|
8
|
Eilber F, Giuliano A, Eckardt J, Patterson
K, Moseley S and Goodnight J: Adjuvant chemotherapy for
osteosarcoma: a randomized prospective trial. J Clin Oncol.
5:21–26. 1987.
|
|
9
|
Miser JS, Kinsella TJ, Triche TJ, et al:
Ifosfamide with mesna uroprotection and etoposide: an effective
regimen in the treatment of recurrent sarcomas and other tumors of
children and young adults. J Clin Oncol. 5:1191–1198. 1987.
|
|
10
|
Goorin AM, Harris MB, Bernstein M, et al:
Phase II/III trial of etoposide and high-dose ifosfamide in newly
diagnosed metastatic osteosarcoma: a pediatric oncology group
trial. J Clin Oncol. 20:426–433. 2002.
|
|
11
|
Ferrari S, Ruggieri P, Cefalo G, et al:
Neoadjuvant chemotherapy with methotrexate, cisplatin, and
doxorubicin with or without ifosfamide in nonmetastatic
osteosarcoma of the extremity: an Italian sarcoma group trial
ISG/OS-1. J Clin Oncol. 30:2112–2118. 2012.
|
|
12
|
Song WS, Kong CB, Jeon DG, et al:
Prognosis of extremity osteosarcoma in patients aged 40–60 years: a
cohort/case controlled study at a single institute. Eur J Surg
Oncol. 36:483–488. 2010.
|
|
13
|
Bramwell VH, Steward WP, Nooij M, et al:
Neoadjuvant chemotherapy with doxorubicin and cisplatin in
malignant fibrous histiocytoma of bone: A European Osteosarcoma
Intergroup study. J Clin Oncol. 17:3260–3269. 1999.
|
|
14
|
Woll PJ, Reichardt P, Le Cesne A, et al:
EORTC Soft Tissue and Bone Sarcoma Group and the NCIC Clinical
Trials Group Sarcoma Disease Site Committee: Adjuvant chemotherapy
with doxorubicin, ifosfamide, and lenograstim for resected
soft-tissue sarcoma (EORTC 62931): a multicentre randomised
controlled trial. Lancet Oncol. 13:1045–1054. 2012.
|
|
15
|
Frustaci S, Gherlinzoni F, De Paoli A, et
al: Adjuvant chemotherapy for adult soft tissue sarcomas of the
extremities and girdles: results of the Italian randomized
cooperative trial. J Clin Oncol. 19:1238–1247. 2001.
|
|
16
|
Edge SB, Byrd DR, Compton CC, et al: Bone.
AJCC Cancer Staging Manual. 7th edition. New York, Springer; New
York, NY: pp. 281–290. 2010
|
|
17
|
National Cancer Institute. National Cancer
Institute Common Toxicity Criteria version 4.0. http://evs.nci.nih.gov/ftp1/CTCAE/.
Accessed September 10, 2013
|
|
18
|
Eisenhauer EA, Therasse P, Bogaerts J, et
al: New response evaluation criteria in solid tumours: revised
RECIST guideline (version 1.1). Eur J Cancer. 45:228–247. 2009.
|
|
19
|
Grimer RJ, Cannon SR, Taminiau AM, et al:
Osteosarcoma over the age of forty. Eur J Cancer. 39:157–163.
2003.
|
|
20
|
Nishida Y, Isu K, Ueda T, et al:
Osteosarcoma in the elderly over 60 years: a multicenter study by
the Japanese Musculoskeletal Oncology Group. J Sur Oncol.
100:48–54. 2009.
|
|
21
|
Comandone A, Bretti S, Bertetto O, Oliva
C, Bergnolo P and Bumma C: Low dose adriamycin and ifosfamide in
the treatment of advanced adult soft tissue sarcomas. Anticancer
Res. 20:2077–2080. 2000.
|
|
22
|
Urakawa H, Tsukushi S, Tsurudome I, et al:
Metastasis of osteosarcoma to stomach made clinically evident by
hematemesis: a case report. World J Surg Oncol. 11:482013.
|
|
23
|
Longhi A, Macchiagodena M, Vitali G and
Bacci G: Fertility in male patients treated with neoadjuvant
chemotherapy for osteosarcoma. J Pediatr Hematol/Oncol. 25:292–296.
2003.
|
|
24
|
Bacci G, Ferrari S, Bertoni F, et al:
Long-term outcome for patients with nonmetastatic osteosarcoma of
the extremity treated at the istituto ortopedico rizzoli according
to the istituto ortopedico rizzoli/osteosarcoma-2 protocol: an
updated report. J Clin Oncol. 18:4016–4027. 2000.
|
|
25
|
Bacci G, Ferrari S, Mercuri M, et al:
Neoadjuvant chemotherapy for osteosarcoma of the extremities in
patients aged 41–60 years: outcome in 34 cases treated with
adriamycin, cisplatinum and ifosfamide between 1984 and 1999. Acta
Orthop. 78:377–384. 2007.
|
|
26
|
Manoso MW, Healey JH, Boland PJ, et al: De
novo osteogenic sarcoma in patients older than forty: benefit of
multimodality therapy. Clin Orthop Relat Res. 438:110–115.
2005.
|