Introduction
Primary malignant lymphoma of the breast (PLB) is a
rare disease, which accounts for only 0.4–0.5% of all breast
malignancies, 0.38–0.7% of all non-Hodgkin’s lymphomas (NHLs) and
1.7–2.2% of extranodal NHLs in the caucasian population (1–4). A
painless mass is the most common presentation, which occurs in ~61%
of cases (5). Other symptoms
include palpable lymph nodes, local pain and local inflamation
(5). The majority of cases of PLB
are diagnosed by biopsy or postoperative pathological observations.
The specific criteria for the diagnosis of PLB includes, the breast
as the tumor site, a history of previous lymphoma and no evidence
of widespread disease at diagnosis, lymphoma has been demonstrated
to exhibit a close association with breast tissue in pathological
specimens, and ipsilateral lymph node involvement (6). Current treatments for PLB include
radiotherapy and/or chemotherapy (5). The use of combined therapy is
considered to be the most effective for PLB patients, even at the
early stages of the disease (1).
The overall prognosis of patient with PLB is relatively good, with
an overall five-year survival rate of 50–82% (7–9). The
present study reports the rare case of 39-year-old female with PLB.
Due to the rarity of the disease, the relevant literature was also
reviewed. Written informed consent was obtained from the
patient.
Case report
In April 2013, a 39-year-old female presented to the
Department of Surgery, Suining Central Hospital (Suining, China)
with a six month history of a painless mass in the left breast. The
mass had rapidly increased in size over six months. No history of
other diseases was identified. On physical examination, a
nontender, demarcated firm 5.0×5.0 cm elastic mass with an
irregular surface, was palpable in the upper inner quadrant of the
left breast. The right breast was normal. Enlargement of the
axillary lymph nodes was not identified. On ultrasonography, the
mass was observed to be solid, almost entirely hyperechoic, and
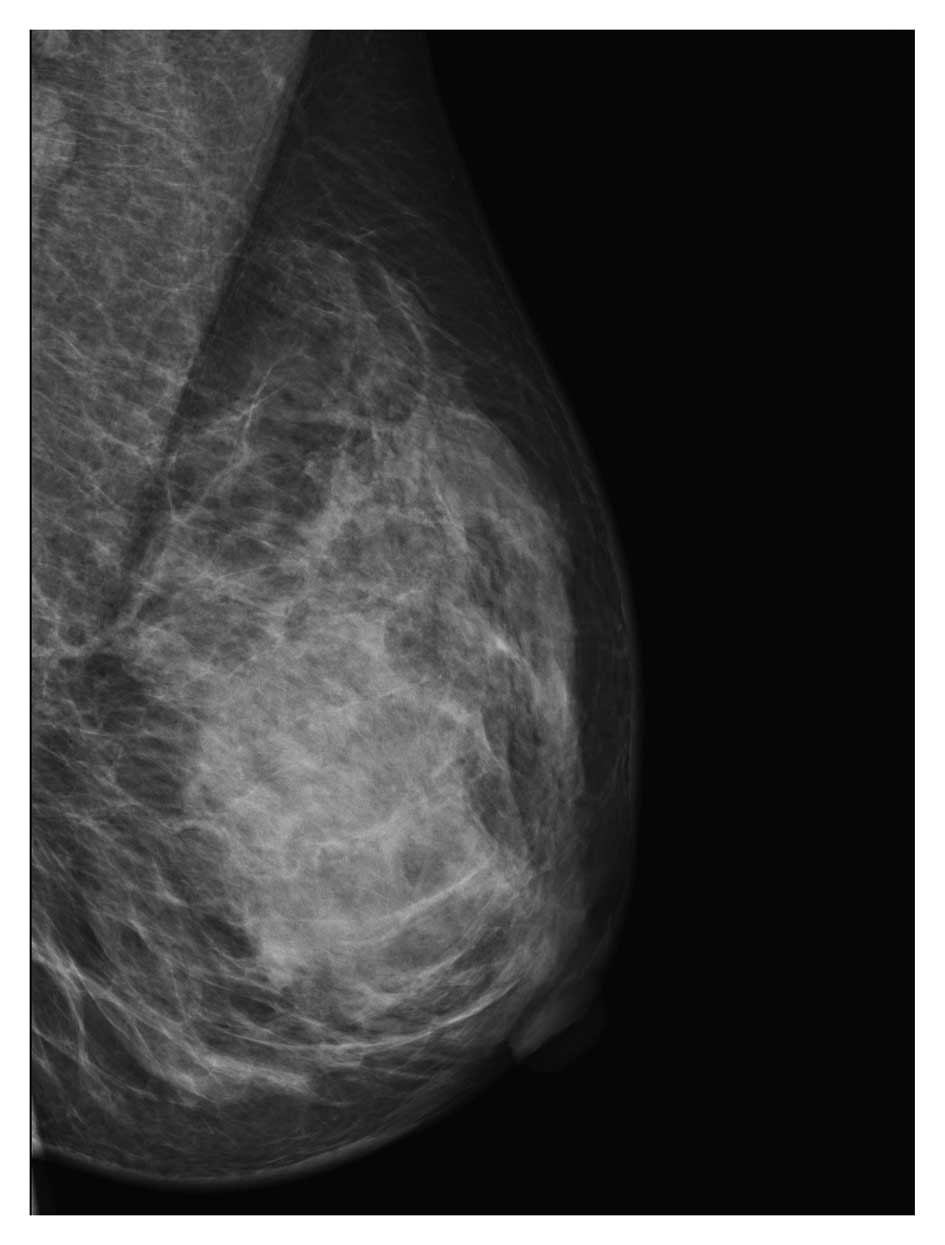
exhibited a circumscribed margin in the palpable area. Digital
radiographic examination revealed a mass of 5.0×4.0×4.0 cm with an
increased density shadow (Fig. 1).
The radiological results were assessed prospectively according to
the American College of Radiology Breast Imaging-Reporting and Data
System (10,11) as category 3 or 4 (suspicion for
malignancy). An ultrasound guided core needle biopsy of the left
breast was performed. The histological results revealed the
infiltration of a large number of lymphocytes into the breast
lobular and duct and lymphocyte hyperplastic lesions were
suspected. Thus, mass excision was performed and a definitive
diagnosis was established. Grossly, the 5.0×5.0×4.0 cm tumor was
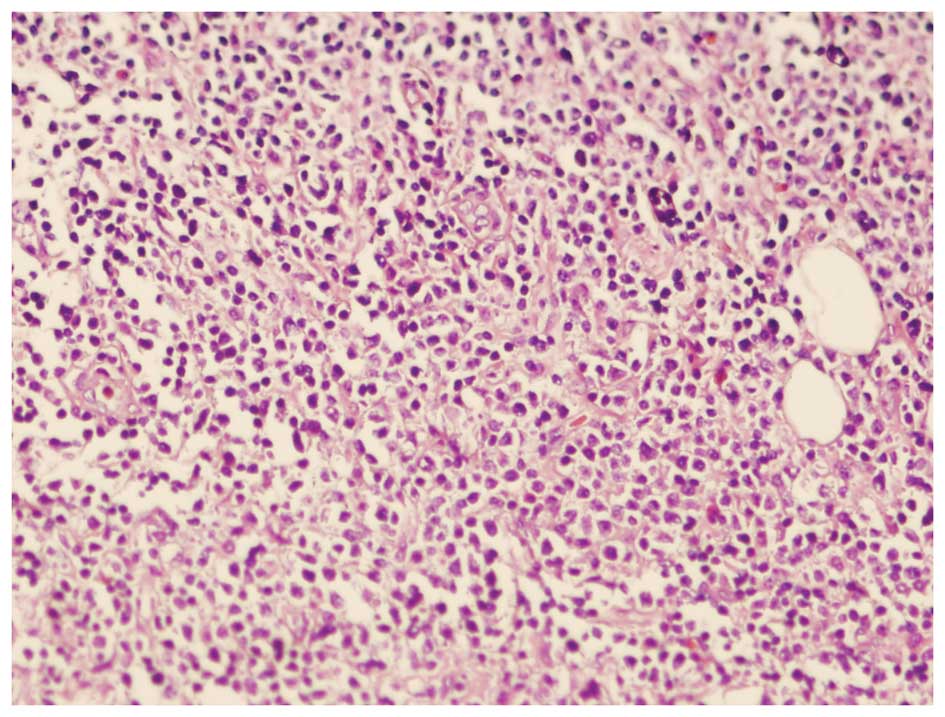
gray-white and poorly circumscribed. Microscopically, the tumor
cells demonstrated invasive growth and a tendency to surround and
invade the wall and lumina of the epithelial structures, resulting
in a lymphoepithelial lesion. In addition, the mammary gland
structure was destroyed. Numerous neoplastic lymphocytes revealed a
diffuse growth pattern (Fig. 2).
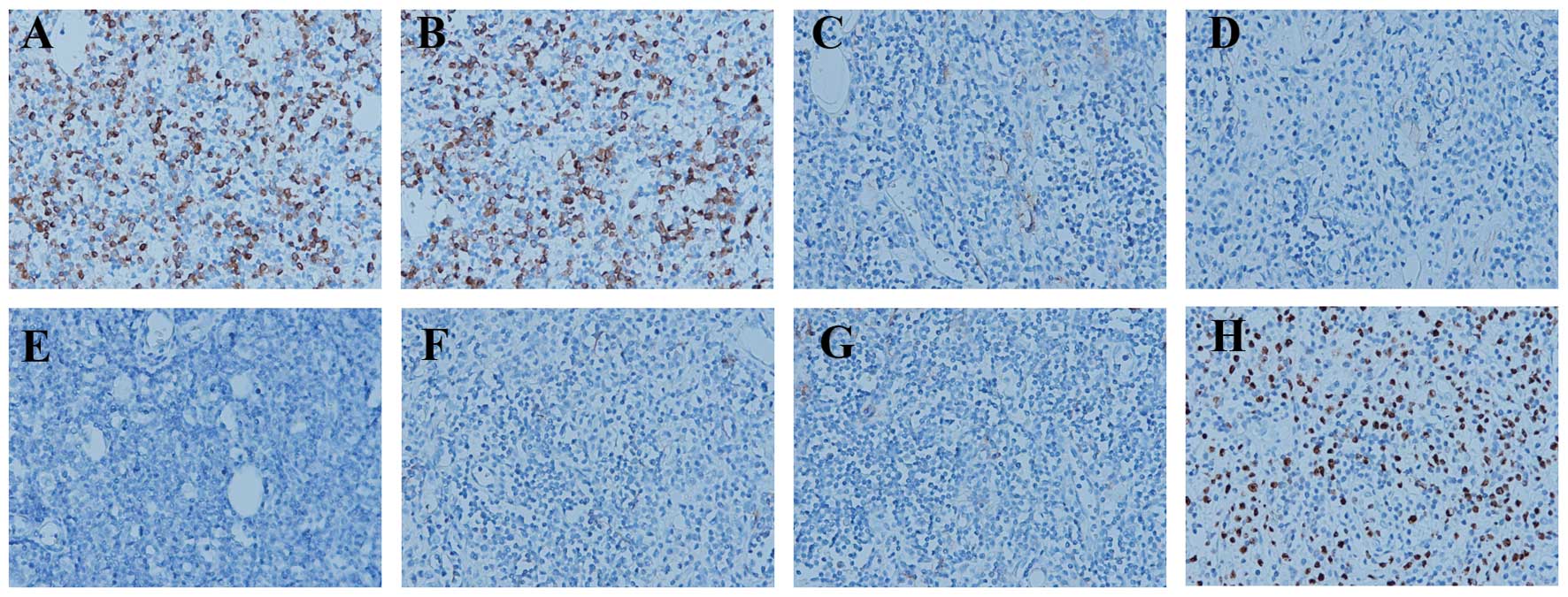
The examination results revealed malignant lymphoma and thus,
further immunophenotype analysis was required to determine the type
of lymphoma. The immunohistochemical profile was positive for
cluster of differentiation (CD)20 and CD79a and negative for CD3,
myeloperoxidase, terminal deoxynucleotidyl transferase, CD99 and
CD138 (Fig. 3). In addition, the
Ki67 positive rate was 60% (Fig.
3). The results confirmed the diagnosis of a diffuse large
B-cell lymphoma. Additionally, the patient underwent further
examination to exclude metastatic disease using positron emission
tomography/computed tomography, which revealed no evidence of
further disease. Thus, primary NHL of the breast (diffuse large
B-cell lymphoma type) was diagnosed. The patient was treated with
six cycles of combination chemotherapy [intravenous
cyclophosphamide (750 mg/m2, day 1), intravenous
doxorubicin (50 mg/m2, day 1), intravenous vincristine
(1.4 mg/m2, day 1 and 8) and prednisone (80 mg, daus
1–5)] for six months. Following three cycles of chemotherapy,
radiation was adminstered to the local site (40 Gy), in combination
with chemotherapy for an additional three cycles. The patient
exhibited a positive response with no evidence of disease. During
the follow-up period of 10 months, no symptoms or signs of disease
recurrence were observed. At present, the patient is receiving
regular follow-up.
Discussion
PLB remains a rare disease, however, the occurrence
is increasing due to improvements to diagnostic techniques and
increasing awareness of the disease. The criteria for PLB diagnosis
have been defined by Wiseman and Liao (12), and include an adequate pathological
specimen, presence of mammary tissue and lymphomatous infiltrate in
close association and exclusion of previous extramammarian lymphoma
or systemic lymphoma. The presence of ipsilateral axillary lymph
node involvement has also been considered acceptable criteria
(13). Histologically, PLB may be
grouped as a large cell B-cell lymphoma, monocytoid B-cell
lymphoma, and undifferentiated, some of which may be T-cell
(14). The histological examination
and immunohistochemical profile may aid with differentiating
between breast diseases, including medullary carcinoma and invasive
lobular carcinoma. According to the aforementioned criteria, in the
present study, the patient was diagnosed with PLB. The
immunohistochemical analysis revealed large B-cell lymphoma.
To date, no standard treatment for PLB has been
identified. Mastectomy is not indicated and wide local excision is
not required as these tumors are highly sensitive to radiotherapy
and systemic chemotherapy (15). In
a previous study, combined therapy using chemotherapy and
radiotherapy, was been found to be the most successful treatment
(16). For small localized tumors,
adequate surgical resection may be effective, followed by
chemotherapy or radiotherapy (12).
With regards to prognosis, it appears that patients with PBL
exhibit a better prognosis than patients with breast cancer or/and
other extranodal lymphomas (17).
Furthermore, previous studies have indicated that the size of PBL,
bilaterality and axillary lymph node involvement did not affect
prognosis, however, the histological type appeared to be the most
significant prognostic factor, with low-grade PBL exhibiting the
best prognosis and high-grade exhibiting the poorest prognosis
(14,18).
However, the majority of studies have been
descriptive studies and thus, detailed studies exploring the
molecular mechanisms of PLB are urgently required. A number of
hypotheses have been proposed to explain the pathogenesis of PLB.
Hormonal stimulation may be an important factor as PLB was observed
frequently in women during pregnancy or postpartum (1). In male patients, the administration of
steroid hormones was associated with the manifestation of PLB. In
addition, certain studies have revealed a clear association between
PBL and mucosa-associated lymphoid tissue (19). The detailed etiology and mechanism
of PLB origination and progression requires further
clarification.
In conclusion, this study reports a rare case of a
female with PLB presenting as a painless mass in the left breast.
As the clinical symptoms of PLB are diverse and nonspecific,
misdiagnosis as other breast diseases may occur. Overall, PLB is
rare, however, the prevalence is increasing. Therefore, this
disease requires attention. The early diagnosis and timely
treatment are important factors when treating PLB. Furthermore,
additional studies focusing on the etiology and mechanism of PLB
are required.
References
|
1
|
Joks M, Mysliwiec K and Lewandowski K:
Primary breast lymphoma - a review of the literature and report of
three cases. Arch Med Sci. 7:27–33. 2011.
|
|
2
|
Bobrow LG, Richards MA, Happerfield LC,
Diss TC, Isaacson PG, Lammie GA and Millis RR: Breast lymphomas: a
clinicopathologic review. Hum Pathol. 24:274–278. 1993.
|
|
3
|
Arber DA, Simpson JF, Weiss LM and
Rappaport H: Non-Hodgkin’s lymphoma involving the breast. Am J Surg
Pathol. 18:288–295. 1994.
|
|
4
|
Topalovski M, Crisan D and Mattson JC:
Lymphoma of the breast. A clinicopathologic study of primary and
secondary cases. Arch Pathol Lab Med. 123:1208–1218. 1999.
|
|
5
|
Jeanneret-Sozzi W, Taghian A, Epelbaum R,
Poortmans P, Zwahlen D, Amsler B, Villette S, Belkacémi Y, Nguyen
T, Scalliet P, et al: Primary breast lymphoma: patient profile,
outcome and prognostic factors. A multicentre Rare Cancer Network
study. BMC Cancer. 8:862008.
|
|
6
|
Jennings WC, Baker RS, Murray SS, Howard
CA, Parker DE, Peabody LF, Vice HM, Sheehan WW and Broughan TA:
Primary breast lymphoma: the role of mastectomy and the importance
of lymph node status. Ann Surg. 245:784–789. 2007.
|
|
7
|
Avilés A, Delgado S, Nambo MJ, Neri N,
Murillo E and Cleto S: Primary breast lymphoma: results of a
controlled clinical trial. Oncology. 69:256–260. 2005.
|
|
8
|
Ryan G, Martinelli G, Kuper-Hommel M,
Tsang R, Pruneri G, Yuen K, Roos D, Lennard A, Devizzi L, Crabb S,
et al; International Extranodal Lymphoma Study Group. Primary
diffuse large B-cell lymphoma of the breast: prognostic factors and
outcomes of a study by the International Extranodal Lymphoma Study
Group. Ann Oncol. 19:233–241. 2008.
|
|
9
|
Ganjoo K, Advani R, Mariappan MR, McMillan
A and Horning S: Non-Hodgkin lymphoma of the breast. Cancer.
110:25–30. 2007.
|
|
10
|
Obenauer S, Hermann KP and Grabbe E:
Applications and literature review of the BI-RADS classification.
Eur Radiol. 15:1027–1036. 2005.
|
|
11
|
Liberman L and Menell JH: Breast imaging
reporting and data system (BI-RADS). Radiol Clin North Am.
40:409–430. 2002.
|
|
12
|
Wiseman C and Liao KT: Primary lymphoma of
the breast. Cancer. 29:1705–1712. 1972.
|
|
13
|
Duman BB, Sahin B, Guvenc B and Ergin M:
Lymphoma of the breast in a male patient. Med Oncol. 28(Suppl 1):
S490–S493. 2011.
|
|
14
|
Hugh JC, Jackson FI, Hanson J and Poppema
S: Primary breast lymphoma. An immunohistologic study of 20 new
cases. Cancer. 66:2602–2611. 1990.
|
|
15
|
Brogi E and Harris NL: Lymphomas of the
breast: pathology and clinical behavior. Semin Oncol. 26:357–364.
1999.
|
|
16
|
Mouna B, Saber B, Tijani EH, Hind M, Amina
T and Hassan E: Primary malignant non-Hodgkin’s lymphoma of the
breast: a study of seven cases and literature review. World J Surg
Oncol. 10:1512012.
|
|
17
|
Freeman C, Berg JW and Cutler SJ:
Occurrence and prognosis of extranodal lymphomas. Cancer.
29:252–260. 1972.
|
|
18
|
Abbondanzo SL, Seidman JD, Lefkowitz M,
Tavassoli FA and Krishnan J: Primary diffuse large B-cell lymphoma
of the breast. A clinicopathologic study of 31 cases. Pathol Res
Pract. 192:37–43. 1996.
|
|
19
|
Mpallas G, Simatos G, Tasidou A, Patra E,
Galateros G, Lakiotis G, Papanicolaou S, Mpallas E and Anagnostou
D: Primary breast lymphoma in a male patient. Breast. 13:436–438.
2004.
|