Introduction
Blastic plasmacytoid dendritic cell neoplasm (BPDCN)
is an extremely rare haematological malignancy that was recently
considered as a distinct disease entity originating from the
precursors of plasmacytoid dendritic cells (PDCs) (1). Patients with BPDCN are usually in
their 50s and 60s (2,3), but children can also be affected
(4–6). Skin lesions typically appear as the
first clinical manifestation, with frequent evolution towards overt
leukemia (7). Histologically, BPDCN
presents as a diffuse monomorphic infiltrate of medium-sized
lymphoid cells in the dermis and the subcutis, with an uninvolved
zone of collagen band (Grenz zone) separating the infiltrate from
the epidermis (8,9). The characteristic immunophenotypic
profile of BPDCN is positivity for cluster of differentiation
(CD)56, CD4 and CD123, with a usually negative result for other
T-cell, B-cell and myeloid cell markers (2,3). At
present there is no curative treatment available for BPDCN and its
prognosis is usually poor (10,11).
The present study describes a case of BPDCN in a 79-year-old male
and reviews the differential diagnoses, treatment and prognosis of
BPDCN to further highlight this rare entity.
Case report
Case presentation
In May 2009, a 79-year-old male was admitted to the
Department of Dermatology, Affiliated Yantai Yuhuangding Hospital,
Medical College of Qingdao University (Yantai, China) subsequent to
noting asymptomatic purple and brown plaques on his back that had
been present for one month. The lesions grew progressively. Upon
admission, a skin examination revealed a reddish papule of 3 cm in
diameter and a violaceous nodule of 3 cm in diameter on the upper
and lower mid back, respectively, without superficial ulceration
(Fig. 1A). A skin biopsy was
subsequently performed. Routine laboratory tests were within normal
ranges. A bone marrow aspiration and biopsy were performed and
revealed no evidence of tumor cells. Additionally, a chest computed
tomography (CT) scan and abdominal ultrasonography did not reveal
any other abnormalities.
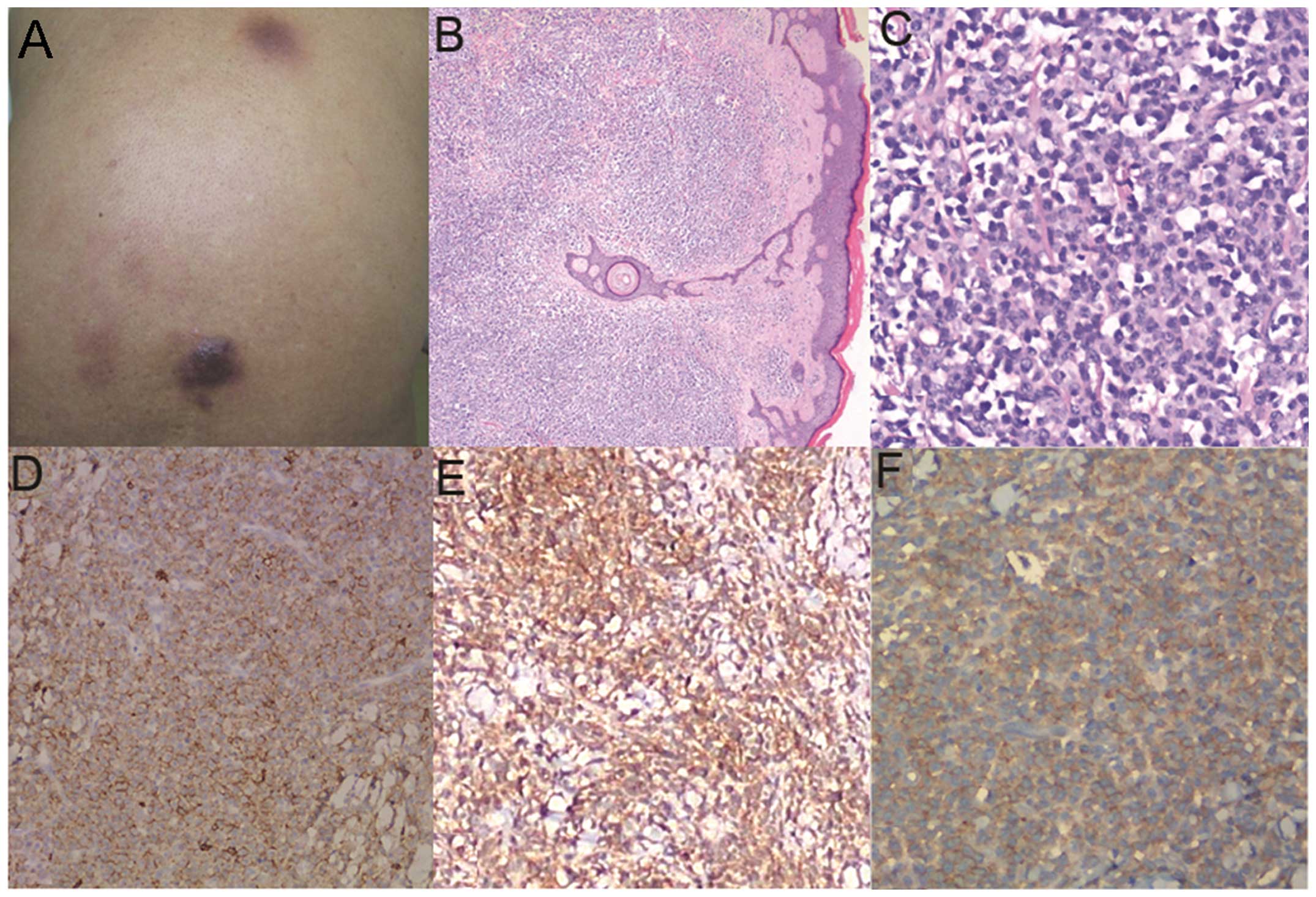
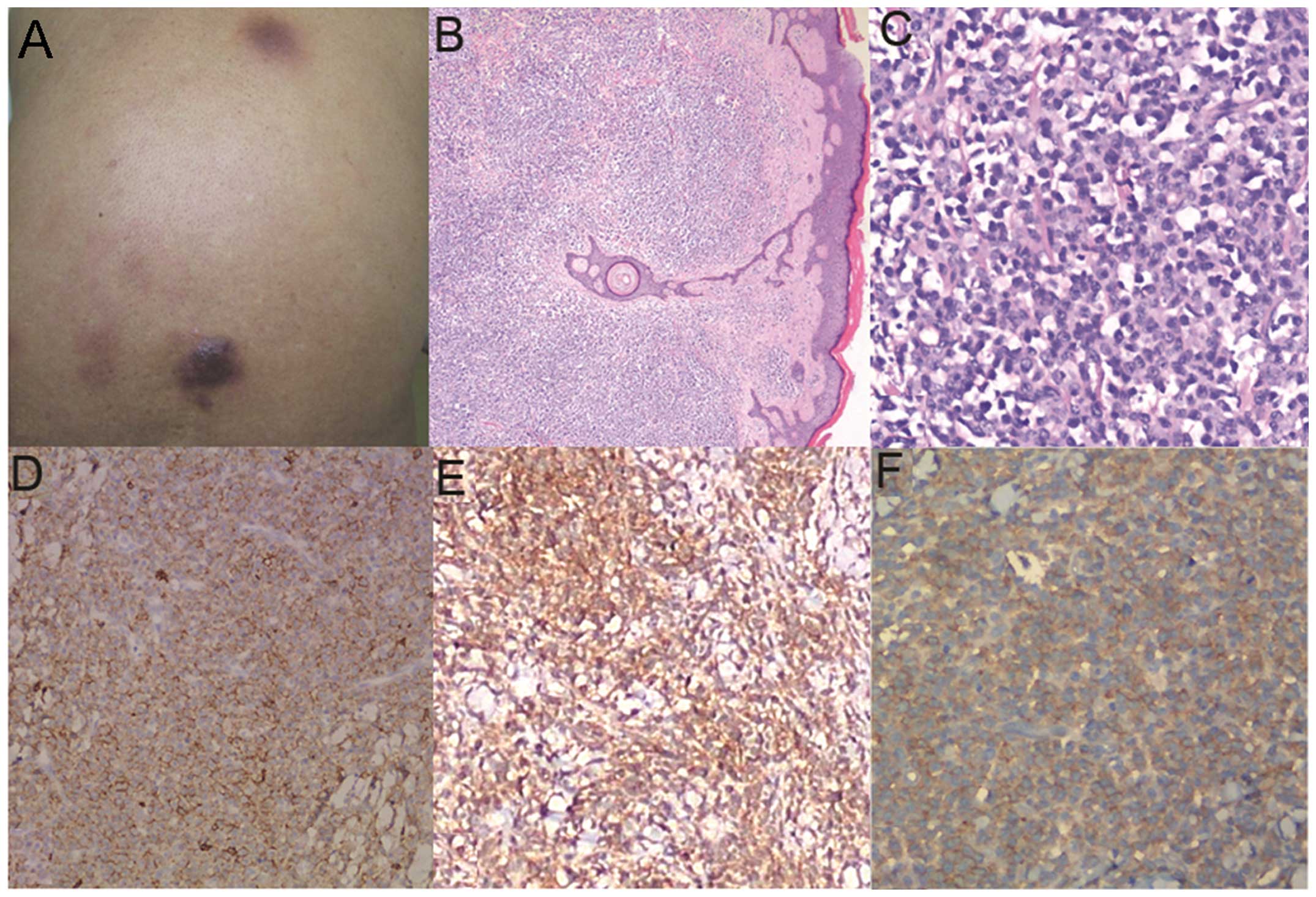 | Figure 1Macroscopic, microscopic and
immunophenotying findings. (A) Gross image showing a reddish papule
and a violaceous nodule, each 3 cm in diameter, on the upper and
lower mid back, respectively. Hematoxylin and eosin (H&E)
staining showing (B) a normal epidermis and a diffuse cellular
infiltration involving the dermis and subcutis, with a homogeneous
and acellular band between tumor compositions and epidermis
(magnification, ×40); and (C) medium-sized tumor cells, with scarce
cytoplasm, finely dispersed chromatin and inconspicuous nucleoli
(magnification, ×200). Immunophenotypic examination revealed that
the tumor cells were (D) cluster of differentiation (CD)4-positive,
(E) CD56-positive, and (F) CD123-positive (Envision, ×200; Dako,
Glostrup, Denmark). |
Pathological findings
The histological examination of the skin biopsy
performed upon admission revealed that the reddish papule exhibited
a dense and diffuse infiltrate of monomorphous medium-sized cells
in the dermis and subcutis. An uninvolved zone of collagen band was
observed in the upper dermis (Fig.
1B). The tumor cells exhibited round to ovoid nuclei, with fine
chromatin, scanty cytoplasm and inconspicuous nucleoli (Fig. 1C).
Immunohistochemical and in situ
hybridization (ISH) findings
Immunohistochemistry showed that the tumor cells
were positive for CD4, CD56, CD123 (Fig. 1D–F) and CD43, but negative for CD3,
CD5, CD20, CD30, CD45RO, CD79α, CD68, anaplastic lymphoma kinase,
paired box 5, myeloperoxidase, granzyme B, T-cell intracellular
antigen-1 and terminal deoxynucleotidyl transferase (TdT). The
investigations for Epstein-Barr virus (EBV) infection by ISH for
EBV-encoded small RNAs yielded a negative result. The patient was
treated with local radiotherapy alone (50 Gy total, 25 times over
five weeks) and succumbed to multiple organ failure five months
later, in October 2009.
Written informed consent was obtained from the
patient for publication of this case study and any accompanying
images.
Discussion
BPDCN is an extremely uncommon disease entity that
poses great diagnostic challenges for dermatologists and
pathologists. Due to the rarity of this disease, the etiology,
pathogenesis and natural history of BPDCN have not yet been fully
elucidated.
BPDCN is typically a disease that occurs in the
elderly, but it can also occur in children. Clinically, BPDCN is
highly aggressive, with a median survival time of 12–14 months
(10,11). The majority of patients with BPDCN
experience disease rapid progression that spreads to the bone
marrow, the blood and the organs or tissues (7). The patient in the present study
presented with skin lesions as the first symptom of onset, with no
evidence of extracutaneous involvement, however, rapid disease
progression occurred prior to mortality. Therefore, it is necessary
to rapidly determine the correct diagnosis and provide effective
treatment.
BPDCN must be distinguished from the accumulation of
plasmacytoid dendritic cells associated with acute myeloid
leukemia. These two diseases possess great similarities regarding
the clinical and histopathological features. Immunophenotypic
analysis can be useful in this respect. BPDCN is usually positive
for CD56, but negative for granzyme B, whereas in the cutaneous
accumulation of plasmacytoid dendritic cells associated with acute
myeloid leukemia, the results are the opposite (7). Another important differential
diagnosis for BPDCN is cutaneous natural killer (NK)/T-cell
lymphoma. In addition to the absence of EBV and cytotoxic
molecules, a lack of patchy necrosis, vascular invasion and
cellular pleomorphism are important in the histological morphology
of BPDCN in order to distinguish the disease from NK/T-cell
lymphoma (12). In recent years,
further antigens associated with plasmacytoid dendritic cell
neoplasms have been successively found, such as CD2-associated
protein, T-cell leukemia 1, CD303/BDCA-2 and CD304/BDCA-4 (13,14).
These markers could aid in differentiating BPDCN from myelocytic
malignancies and T- or NK/T-cell lymphomas.
At present, there is no effective or uniform
treatment approach for BPDCN. A radical treatment plan for acute
leukemia was previously reported to be of some success in acquiring
complete remission in certain BPDCN patients, however, these
patients usually relapsed within several months (15). The patient in the present study was
treated with radiotherapy and succumbed five months later. Pagano
et al (16) suggested that
systematic preventive intrathecal chemotherapy should be indicated
in the treatment of BPDCN, as the central nervous system may be a
persistent blast-cell sanctuary.
A few factors, including an age of <40 years
(11), lesions restricted to the
skin (17) and strong TdT
expression in the tumor cells (18), have been reported to be associated
with a more favorable prognosis. However, the underlying mechanisms
by which these factors affect the prognosis remain unclear. The
present patient did not show extracutaneous involvement, but
experienced a rapidly progressive clinical course, with a short
survival time. This suggested that lesions restricted to the skin
are not adequately proven as an independent index for
prognosis.
In summary, the present study reports a case of
BPDCN presenting with cutaneous involvement alone in a patient who
experienced rapid disease progress prior to mortality. Although
numerous types of lymphoma or leukemia can primarily or secondarily
involve the skin, BPDCN, despite its rarity, should also be
considered in the differential diagnosis. Additionally, the present
findings further highlight the ineffectiveness of conventional
radiotherapy in treating this unique disease and also alerts
clinicians to the requirement to establish treatment
modalities.
References
|
1
|
Facchetti F, Jones DM and Petrella T:
Blastic plasmacytoid dendritic cell neoplasm. WHO Classification of
Tumours of Haematopoietic and Lymphoid Tissues. Swerdlow SH, Campo
Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J and Vardiman JW:
4th edition. IARC Press; Lyon, France: pp. 145–147. 2008
|
|
2
|
Lucioni M, Novara F, Fiandrino G, et al:
Twenty-one cases of blastic plasmacytoid dendritic cell neoplasm:
focus on biallelic locus 9p21.3 deletion. Blood. 118:4591–4594.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hashikawa K, Niino D, Yasumoto S, et al:
Clinicopathological features and prognostic significance of CXCL12
in blastic plasmacytoid dendritic cell neoplasm. J Am Acad
Dermatol. 66:278–291. 2012. View Article : Google Scholar
|
|
4
|
Cota C, Vale E, Viana I, et al: Cutaneous
manifestations of blastic plasmacytoid dendritic cell neoplasm -
morphologic and phenotypic variability in a series of 33 patients.
Am J Surg Pathol. 34:75–87. 2010. View Article : Google Scholar
|
|
5
|
Yang CS, Wang J and Chang TK: Congenital
blastic plasmacytoid dendritic cell neoplasm. Pediatr Blood Cancer.
58:109–110. 2012. View Article : Google Scholar
|
|
6
|
Muljono A, Graf NS and Arbuckle S: Primary
cutaneous lymphoblastic lymphoma in children: series of eight cases
with review of the literature. Pathology. 41:223–228. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dargent JL, Delannoy A, Pieron P, et al:
Cutaneous accumulation of plasmacytoid dendritic cells associated
with acute myeloid leukemia: a rare condition distinct from blastic
plasmacytoid dendritic cell neoplasm. J Cutan Pathol. 38:893–898.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li Y, Li Z, Lin HL, Chen XH and Li BL:
Primary cutaneous blastic plasmacytoid dendritic cell neoplasm
without extracutaneous manifestation: case report and review of the
literature. Pathol Res Pract. 207:55–59. 2011. View Article : Google Scholar
|
|
9
|
López V, Martí N, Ferrández A, Martin JM
and Jordá E: An atypical presentation of a blastic plasmacytoid
dendritic cell tumors. J Cutan Pathol. 37:e50–e52. 2010. View Article : Google Scholar
|
|
10
|
Assaf C, Gellrich S, Whittaker S, et al:
CD56-positive haematological neoplasms of the skin: a multicentre
study of the Cutaneous Lymphoma Project Group of the European
Organisation for Research and Treatment of Cancer. J Clin Pathol.
60:981–989. 2007. View Article : Google Scholar
|
|
11
|
Petrella T, Bagot M, Willemze R, et al:
Blastic NK-cell lymphomas (agranular CD4+CD56+ hematodermic
neoplasms): a review. Am J Clin Pathol. 123:662–675. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pongpruttipan T, Kummalue T, Bedavanija A,
et al: Aberrant antigenic expression in extranodal NK/T-cell
lymphoma: a multi-parameter study from Thailand. Diagn Pathol.
6:792011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rizvi H, Paterson JC, Tedoldi S, et al:
Expression of the CD2AP adaptor molecule in normal, reactive and
neoplastic human tissue. Pathologica. 104:56–64. 2012.PubMed/NCBI
|
|
14
|
Julia F, Dalle S, Duru G, et al: Blastic
plasmacytoid dendritic cell neoplasms: clinico-immunohistochemical
correlations in a series of 91 patients. Am J Surg Pathol.
38:673–680. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dietrich S, Andrulis M, Hegenbart U, et
al: Blastic plasmacytoid dendritic cell neoplasia (BPDC) in elderly
patients: results of a treatment algorithm employing allogeneic
stem cell transplantation with moderately reduced conditioning
intensity. Biol Blood Marrow Transplant. 17:1250–1254. 2001.
View Article : Google Scholar
|
|
16
|
Pagano L, Valentini CG, Pulsoni A, et al;
GIMEMA-ALWP (Gruppo Italiano Malattie EMatologiche dell’Adulto,
Acute Leukemia Working Party). Blastic plasmacytoid dendritic cell
neoplasm with leukemic presentation: an Italian multicenter study.
Haematologica. 98:239–246. 2013. View Article : Google Scholar :
|
|
17
|
Bekkenk MW, Jansen PM, Meijer CJ and
Willemze R: CD56+ hematological neoplasms presenting in the skin: a
retrospective analysis of 23 new cases and 130 cases from the
literature. Ann Oncol. 15:1097–1108. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jaye DL, Geigerman CM, Herling M, Eastburn
K, Waller EK and Jones D: Expression of the plasmacytoid dendritic
cell marker BDCA-2 supports a spectrum of maturation among CD4+
CD56+ hematodermic neoplasms. Mod Pathol. 19:1555–1562. 2006.
View Article : Google Scholar : PubMed/NCBI
|