Introduction
Granular cell tumors (GCTs) are rare soft tissue
neoplasms that were first reported by Abrikossoff in 1926 (1). GCTs have been frequently identified in
various organs including the breast, urinary bladder, testis,
ovary, esophagus, heart, head and neck (2,3). The
incidence rate of thyroid GCTs is extremely low. Only 11 cases have
been reported in the English language literature (3–13). The
rarity of thyroid GCTs and characteristics mimicking malignancy
results in a diagnostic challenge for surgeons on clinical
examination. Thyroid GCTs are therefore unlikely to be diagnosed
correctly on initial examination unless pathological and
immunohistochemical results are available (5,13).
Numerous lines of evidence are required to contribute to an
accurate diagnosis. Even though the number of thyroid GCTs is
increasing, our understanding of these tumors requires further
research. An increase in the number of cases of thyroid GCTs is
expected to be publically reported. The present case study
describes a novel case of thyroid GCT, with a description of the
primary aspects of its clinical and pathological characteristics.
Written informed consent was obtained from the patient’s
family.
Case report
Patient history
A 14-year-old Chinese female was referred to the
West China Hospital of Sichuan University (Chengdu, China), for
evaluation of a thyroid incidentaloma. The patient presented with a
3-month history of a neck lump without thyrotoxicosis or symptoms
of hypothyroidism. The mass (~2.5×2.0 cm) was located in the right
thyroid lobe without cervical lymphadenectasis.
Patient examination
Laboratory examinations, including thyroid function
tests, carcinoembryonic antigen, calcitonin and serum calcium
levels were in the normal range. A thyroid ultrasound disclosed
that the mass consisted of numerous thyroid nodules, and the
biggest nodule showed an irregular shape, infiltrative margins,
intranodular avascularity and a shape taller than width. The mass
was subsequently classified as grade 5 according to the Thyroid
Imaging Reporting and Data System (14). Furthermore, fine needle aspiration
cytology of the thyroid nodule indicated a high likelihood of
malignancy. The patient had no history of family thyroid disease or
external irradiation.
Diagnosis and treatment
Taken together, these features gave rise to a
diagnosis for malignancy and a thyroidectomy was performed.
Intraoperatively, the frozen section revealed a tumor that was
derived from epithelial or mesenchymal tissue. Macroscopically, the
tumor had progressively invaded the surrounding tissues and
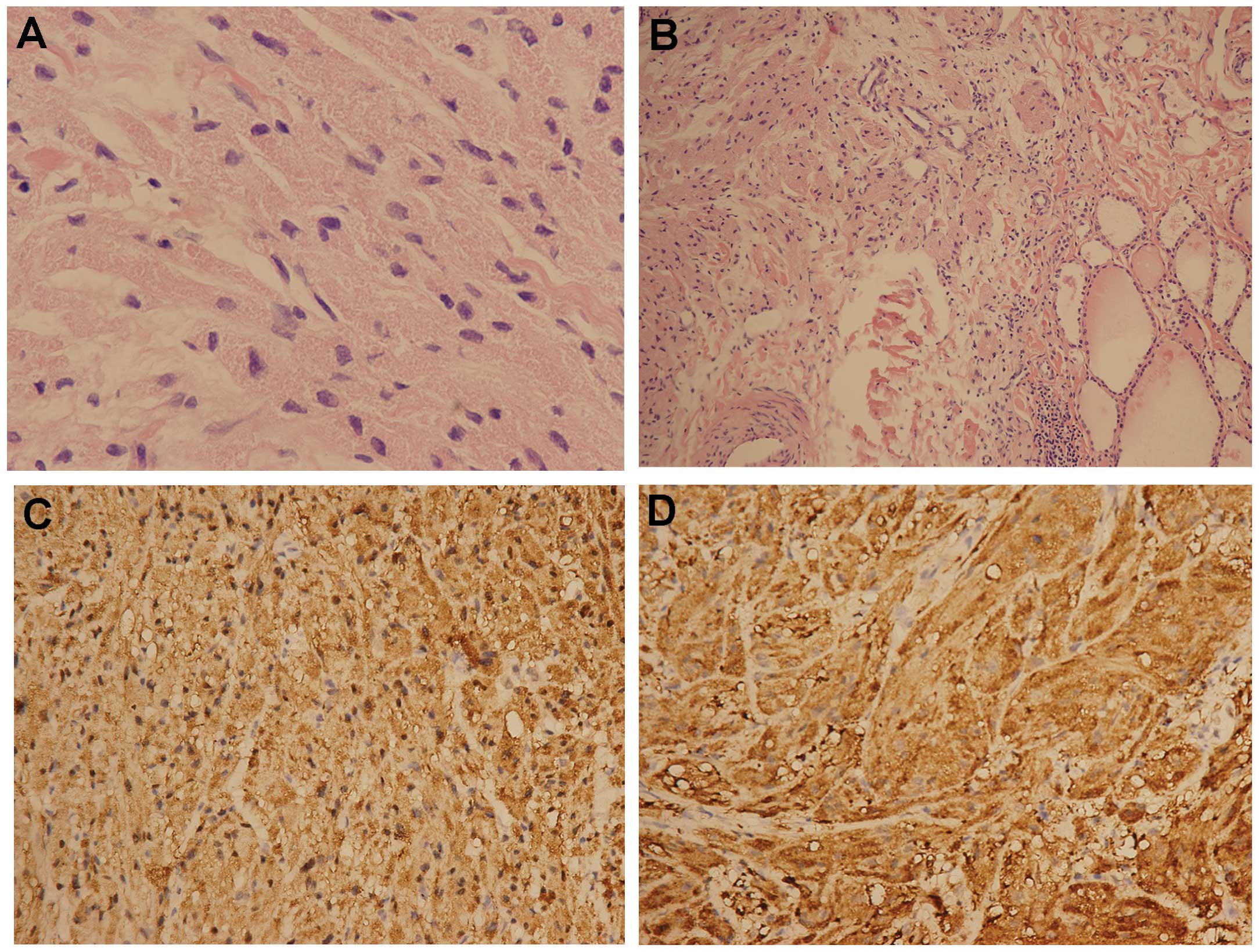
resembled a follicular neoplasm. The tumor was histopathologically
characterized by nests of epithelioid cells with an oval or spindle
deep-dyed large, hyperchromatic nucleolus and an abundant granular
eosinophilic cytoplasm. A few of the cells showed heteromorphism,
and there was no mitotic activity (Fig.
1A). The nests were separated by a septate fiber, as well as
interdigitated with surrounding thyroid follicles (Fig. 1B) and the adjacent ipsilateral
cricothyroid muscle. Immunohistochemical analysis indicated that
the tumor cells originated from Schwann cells due to positive
staining for S-100 protein (Fig.
1C), neuron-specific enolase (Fig.
1D) and CD68. The tumor cells were negative for thyroid
transcription factor-1 and thyroglobulin.
Postoperative outcomes
Postoperatively, the clinical course of the patient
was uneventful. Medication with levothyroxine at a daily dose of
62.5 μg was only administered in order to maintain the serum
thyrotropin at a level <0.5 mU/l. Chemotherapy or radioiodine
treatment was not performed. The patient had no recurrence and
remained healthy during the 14-month post-operative follow-up
visit.
Discussion
GCTs are rare soft tissue neoplasms, which may occur
at any age and at most anatomical locations (2). GCTs of the thyroid, however, are
extremely rare. Due to the rarity of the lesion, preoperative and
intraoperative diagnoses of thyroid GCTs remain challenging
(3–5,8–10,15–17).
Clinically, the majority of patients are asymptomatic (4–13). One
case has been reported of nonspecific symptoms, such as weakness,
anxiety and palpitation (3).
Laboratory examinations, including thyroid function tests,
carcinoembryonic antigen, calcitonin and serum calcium levels, are
useful for differential diagnosis but are nonspecific. The gold
standard for diagnosis of GCTs depends on the results obtained from
pathological and immunohistochemical analysis. The criteria to
distinguish between pathological types of GCT are necrosis,
spindling, vesicular nuclei with prominent nucleoli, increased
mitotic activity (>2/10 high-power fields), high
nuclear/cytoplasmic ratio and pleomorphism (17). Tumors with three or more of these
criteria are considered to have malignant behavior. Those with one
or two features are termed as ‘atypical granular cell tumors’.
Cases that meet none of these criteria, or have only a focal
pleomorphism, are classified as benign. The clinical routine of
differential diagnosis of thyroid GCTs occurs predominantly from
two aspects. Firstly, a number of benign/malignant tumors display a
granular appearance, mimicking GCTs, such as Hurthle cell papillary
thyroid carcinoma, follicular Hurthle cell tumor of the thyroid, as
well as medullary thyroid cancer. These tumors need to be excluded
from the diagnosis. Secondly, the distinction in pathological
category of granular cell tumors is essential. GCTs were initially
considered to be myogenic in origin, but high positive rates for
S-100 protein and neuron-specific enolase detected by
immunohistochemistry suggests that a Schwann cell derivation is
more likely (15). At present,
surgical excision is the only treatment option (18), and to date, radiation or
chemotherapy as not been proposed. Most thyroid GCTs are benign,
and patients have a favorable prognosis (9). Malignant GCTs are relatively uncommon,
constituting 1–2% of all granular cell tumors (16), and there is little information on
the response of malignant GCTs to therapeutic modalities, other
than surgical intervention. Local recurrence has been reported
after incomplete excision as early as 3 months after surgical
removal of the tumor (13).
Follow-up examinations are vital to observe the curative
effects.
In the present case, the clinical manifestations and
laboratory examinations were not unusual. The ultrasound raised
suspicion of the possibility of a thyroid carcinoma, and fine
needle aspiration cytology of the thyroid nodule indicated a high
likelihood of malignancy. A surgical intervention was performed
since a tumor was suspected on fine needle aspiration biopsy.
Sections analyzed from the intraoperative frozen tumor specimen
failed to facilitate a diagnosis. A thyroid GCT was finally
diagnosed by postoperative pathology and immunohistochemistry.
According to the six histological criteria for assessing the
character of thyroid GCTs (3), the
presenting case was classified as a benign GCT with atypical
changes, since none of the criteria were met, other than focal
pleomorphism and occasional spindle cell. The specimen did not meet
the standard of atypical GCTs. Hematoxylin and eosin-stained
sections showed a partially circumscribed neoplasm, consisting of
oval to spindle cells, a hyperchromatic nucleus and an abundant
granular eosinophilic cytoplasm, as well as a few of the cells
displaying heteromorphism (a large nucleus and dense cytoplasm)
without mitotic activity. Immunohistochemical analysis showed
positive expression of S-100, neuron-specific enolase and CD68, but
was negative for thyroid transcription factor-1 and thyroglobulin.
The tumor was surgically removed, and no radiotherapy or
chemotherapy was administered except for a routine medication
following the surgery (oral levothyroxine at a daily dose of 62.5
μg). Post-operative follow-up at 14 months showed that the patient
had experienced a stable recovery with no signs of recurrence or
metastasis.
In conclusion, thyroid GCT is an extremely rare and
highly aggressive tumor with a favorable prognosis. Clinically, the
diagnosis of thyroid GCTs is based on pathology and
immunohistochemistry and surgical resection is currently considered
as the only treatment. In the presented case, routine postoperative
medical management proved efficient, and a long-term follow-up was
performed in order to confirm the outcome of these treatments.
Further accumulation of the clinical and histopathological features
of such rare cases may be of clinical significance in the diagnosis
and treatment of thyroid GCTs.
Acknowledgements
The authors would like to thank Professor Zhanwei
Xiao for invaluable contributions to the preparation of the
study.
References
|
1
|
Abrikossoff A: Über Myome. Virchows
Archiv. 260:215–233. 1926. View Article : Google Scholar
|
|
2
|
Ordóñez NG: Granular cell tumor: a review
and update. Adv Anat Pathol. 6:186–203. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Milias S, Hytiroglou P, Kourtis D and
Papadimitriou CS: Granular cell tumour of the thyroid gland.
Histopathology. 44:190–191. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Igarashi T, Okamura R, Jikuzono T, Shimizu
A, Tsuchiya S and Shimizu K: Malignant granular cell tumor of the
thyroid: a case report. J Basic Clin Med. 2:17–19. 2013.
|
|
5
|
Bowry M, Almeida B and Jeannon JP:
Granular cell tumour of the thyroid gland: a case report and review
of the literature. Endocr Pathol. 22:1–5. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mahoney CP, Patterson SD and Ryan J:
Granular cell tumor of the thyroid gland in a girl receiving
high-dose estrogen therapy. Pediatr Pathol Lab Med. 15:791–795.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liu J and Krishnamouthy S: The importance
of fine needle aspiration in conjunction with radiologic
examination in the evaluation of granular cell tumor presenting as
a thyroid mass: a case report. Int J Clin Exp Pathol. 4:197–199.
2011.PubMed/NCBI
|
|
8
|
Baloch ZW, Martin S and Livolsi VA:
Granular cell tumor of the thyroid: a case report. Int J Surg
Pathol. 13:291–294. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chang SM, Wei CK and Tseng CE: The
cytology of a thyroid granular cell tumor. Endocr Pathol.
20:137–140. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Espinosa-de-Los-Monteros-Franco VA,
Martinez-Madrigal F and Ortiz-Hidalgo C: Granular cell tumor
(Abrikossoff tumor) of the thyroid gland. Ann Diagn Pathol.
13:269–271. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Harp E and Caraway NP: FNA of thyroid
granular cell tumor. Diagn Cytopathol. 41:825–828. 2013. View Article : Google Scholar
|
|
12
|
Min KW, Paik SS, Jun YJ, Han H and Jang
KS: Fine needle aspiration cytology of a granular cell tumour
arising in the thyroid gland. Cytopathology. 23:411–412. 2012.
View Article : Google Scholar
|
|
13
|
Cimino-Mathews A, Illei PB and Ali SZ:
Atypical granular cell tumor of the thyroid: cytomorphologic
features on fine needle aspiration. Diagn Cytopathol. 39:608–611.
2011. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wei X, Li Y, Zhang S and Gao M: A
Meta-analysis of thyroid imaging reporting and data system in the
ultrasonographic diagnosis of 10,437 thyroid nodules. Head Neck.
Sep 22–2014.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Le BH, Boyer PJ, Lewis JE and Kapadia SB:
Granular cell tumor: immunohistochemical assessment of
inhibin-alpha, protein gene product 9.5, S100 protein, CD68, and
Ki-67 proliferative index with clinical correlation. Arch Pathol
Lab Med. 128:771–775. 2004.PubMed/NCBI
|
|
16
|
Goldblum JR and Montgomery E: Soft tissue
tumors. Pathol Case Rev. 7:125–126. 2002. View Article : Google Scholar
|
|
17
|
Fanburg-Smith JC, Meis-Kindblom JM, Fante
R and Kindblom LG: Malignant granular cell tumor of soft tissue:
diagnostic criteria and clinicopathologic correlation. Am J Surg
Pathol. 22:779–794. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lack EE, Worsham GF, Callihan MD, et al:
Granular cell tumor: a clinicopathologic study of 110 patients. J
Surg Oncol. 13:301–316. 1980. View Article : Google Scholar : PubMed/NCBI
|