Introduction
Melanoma is a malignant tumor that originates from
melanocytes, which are the cells that produce the pigment melanin.
Melanoma is the most life-threatening and treatment-resistant skin
cancer. Although 91.2% of melanomas arise from the skin, 5.3% arise
from ocular tissues, 1.3% from mucosal tissues and <1% from the
urethra, with the remainder being of unknown primary origin
(1,2).
Primary pleural melanoma is a rare occurrence. To the best of our
knowledge, only three cases have been reported thus far (3–5). This is
the presentation of an unusual case of primary malignant melanoma
of the pleura in a 36-year-old female patient. Written informed
consent was obtained from the family of the patient.
Case report
A 36-year-old female patient was admitted to the
Union Hospital (Wuhan, China) in September, 2010 due to
intermittent left abdominal pain over the previous ∼6 weeks. The
patient also complained of other symptoms, including dry cough and
dyspnea associated with the pain. No cutaneous mass or ulceration
was identified on physical examination. The chest X-ray revealed a
large amount of pleural effusion in the left hemithorax.
Thoracocentesis was performed at the Department of Thoracic
Surgery, Union Hospital. Macroscopically, the pleural effusion was
black in color, while the cytology revealed abnormalities of the
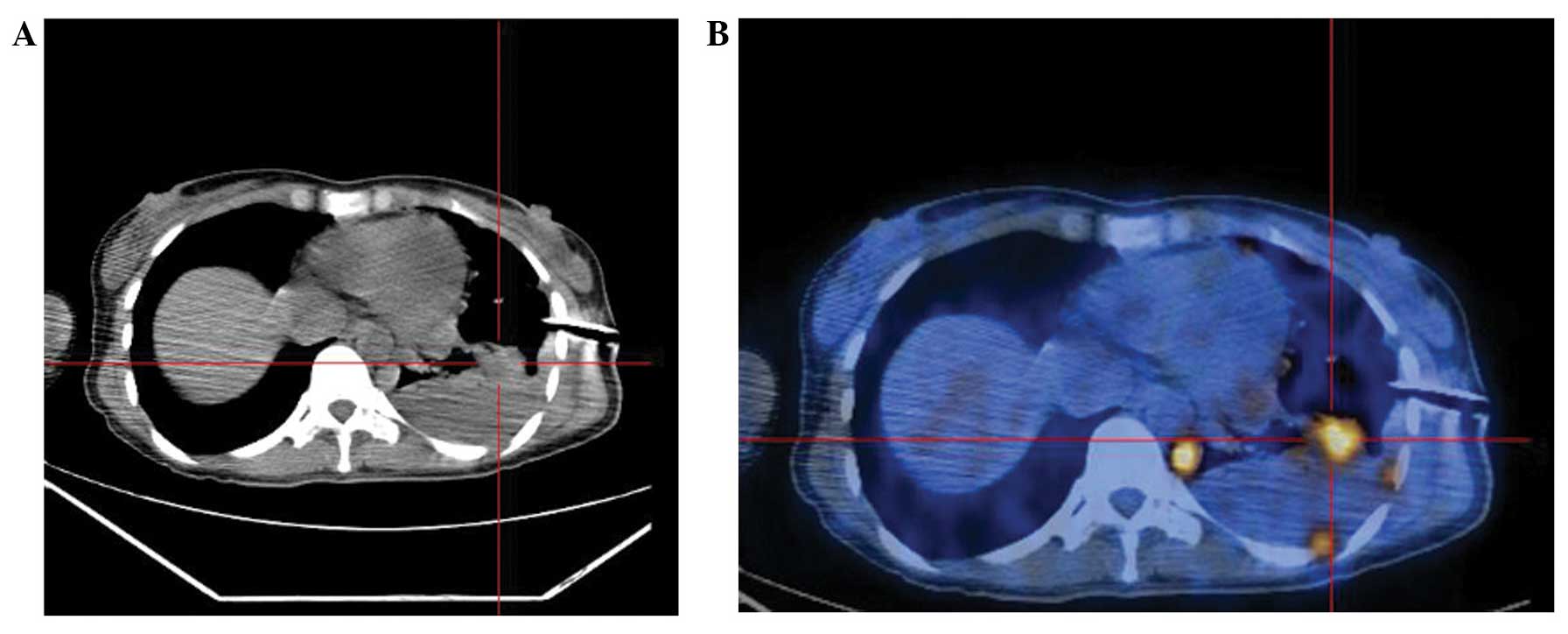
red blood cells. The positron emission tomography/computed
tomography (PET/CT) scanning showed multiple nodular soft tissue
thickenings of the left hemipleura, inferior visceral pleura of the
right lower lobe and right hilum. A lesion with high standardized
uptake value (SUV) was detected and pleural effusion in the left
hemithorax was reconfirmed by the scan (Fig. 1). No other high-SUV lesion was
identified on PET/CT.
A thoracoscopic biopsy was performed and the
histological examination of the pleural mass revealed round to
polygonal cells with large nuclei. On immunohistochemical
examination, the tumor cells were positive for the expression of
intracellular melan-A, human melanoma black-45 (HMB-45), vimentin
(Vim) and S-100 and negative for calretinin and pancytokeratin,
which further confirmed the diagnosis of melanoma. The patient was
then transferred to the Cancer Center of the Union Hospital and
received three cycles of chemotherapy with dacarbazine (200
mg/m2, days 1–3) and cisplatin (30 mg/m2,
days 5–7), in combination with interferon-α2b immunotherapy. Upon
reevaluation, a partial response was achieved following three
cycles of immunochemotherapy.
The patient declined further treatment due to grade
4 neutropenia and grade 3 thrombocytopenia; she remained
asymptomatic for 2 months prior to the development of severe cough
and hemoptysis and was readmitted to the Cancer Center of the Union
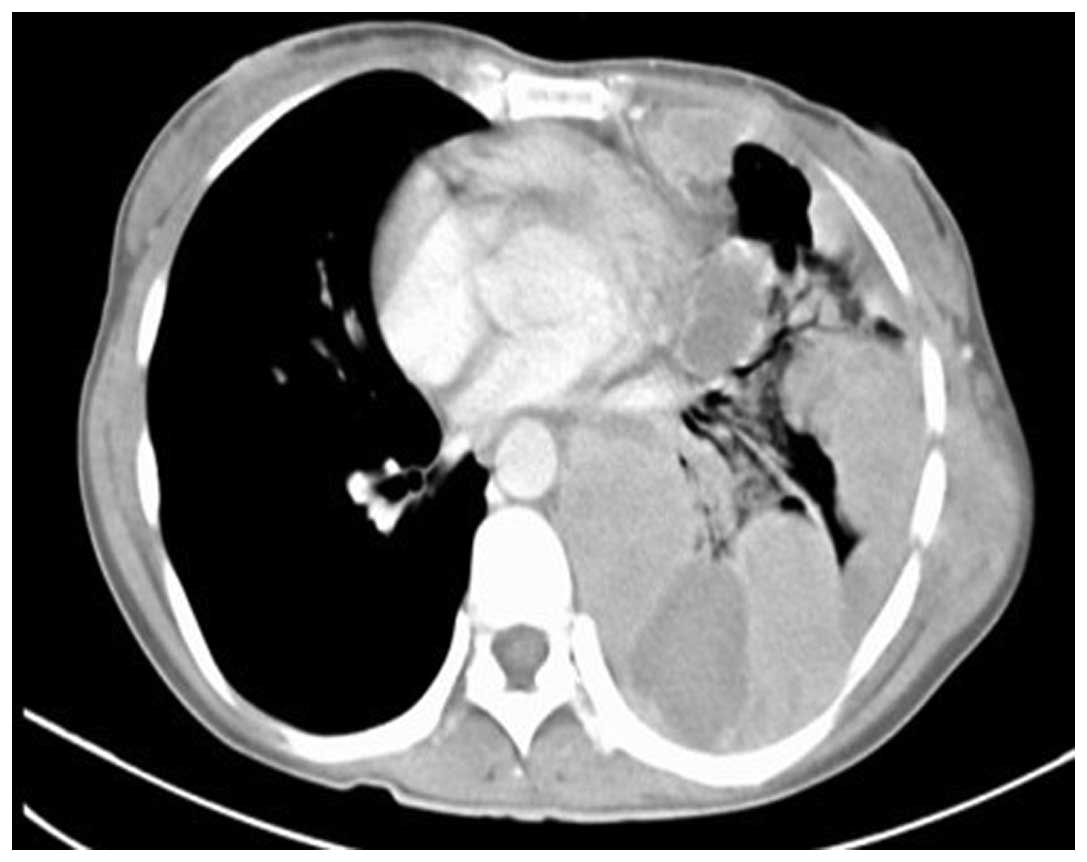
Hospital in January, 2011. A chest CT scan revealed that the masses
in the left pleural cavity had significantly increased in size. The
patient was administered two further cycles of chemotherapy with
dacarbazine and cisplatin, at the same dosage mentioned above.
However, the symptoms of cough and hemoptysis did
not subside and the hemoptysis increased in severity during
chemotherapy. A reevaluation chest CT scan (Fig. 2) was conducted after the fifth cycle
of chemotherapy in April, 2011 and revealed that, in addition to
the increased thickness of the pleura, a sizeable mass with an
unclear boundary infiltrated the interspace of the mediastinum,
subcutaneous tissue of the left chest wall, hilum of the left lung
and right cardiac border. There were no identified metastatic
nodules in the right lung. The patient was unsuccesfully palliated,
exhibiting persistent cough and hemoptysis for 1 month following
treatment completion. The patient eventually succumbed to the
disease after 2 months.
Discussion
The incidence of melanoma has been continuously
increasing over the last few decades. Despite earlier diagnosis,
the prognosis of patients with melanoma remains poor. Primary
pleural melanoma is a rare entity, with only three cases reported
worldwide thus far (3–5). However, metastasis of malignant melanoma
to the pleura or lung is relatively common. Furthermore, the
symptoms of pleural melanoma are often mistaken for other types of
primary pleural cancer. It is therefore important to distinguish
primary pleural melanomas from metastatic or other types of primary
pleural cancer.
Three basic clinical criteria should be referred to
when establishing a diagnosis of primary melanoma of the pleura: i)
No previously removed skin tumor, unless the pathological
examination did not reveal malignancy and the slides are available
for reevaluation; ii) a solitary tumor in the surgical specimen
from the pleura; and iii) no demonstrable melanoma in other
locations at the time of surgery (6).
The present case fulfilled these criteria. The patient had not
undergone any skin operation. At the time of diagnosis, only a
solitary tumor on the pleura was identified on PET/CT imaging.
However, metastatic lesions appeared and gradually increased in
size during the follow-up period.
Pleural mesothelioma shares certain clinical and
imaging characteristics with pleural melanoma. The key points for
differential diagnosis lie in the expression levels of certain
immunohistochemical markers: Premelanosomes, melan-A, Vim, S-100
and HMB-45 are well-defined surface markers for melanoma, while
cytokeratin (CK)5/6, CK8/18, carcinoembryonic antigen, Vim,
melanocortin and calretinin are considered to be mesothelioma
markers.
A popular view on melanoma growth (7) is that there are eight pathological and
clinical levels in a classic melanoma model of growth and
development: Precursor melanocyte, commonly acquired or congenital
nevus with the presence of normal melanocytes, dysplastic nevus
with structural and architectural atypia, radial growth melanoma,
non-tumorigenic primary melanoma without the capacity to
metastasize, vertical growth melanoma, primary melanoma invading
the dermis with the potential ability to metastasize and, finally,
metastatic melanoma. The histogenesis of malignant melanoma of the
pleura has not been fully elucidated. Patients with thick melanomas
exhibit an increased risk of developing lymph node and visceral
metastases (8). Therefore, it is
hypothesized that the mechanism of pleural melanoma development
involves cutaneous nevus cells entering dermal lymphatic vessels
and subsequently traveling via the lymphatic system to the pleura.
However, due to the limited number of reported cases of pleural
melanoma, this theory has not been definitively proven.
Notably, it was identified that, among the four
reported cases, including the present case, one patient displayed a
malignant amelanotic melanoma, one case was not recent enough to
obtain detailed information and the remaining two patients
displayed sizeable congenital nevi. In a study by Mohanty et
al (4), an Indian 50-year-old
male farmer exhibited a giant congenital ‘bathing suit’ hairy
nevus, ranging from small dots to extensive hyperpigmented hairy
regions, extending anteroposteriorly to cover the entire lower
extremity below the waist. In the present case, the 36-year-old
Chinese female patient also exhibited a large congenital nevus
covering almost half of the right lower extremity. Based on the
abovementioned hypothesis and the latter two cases, it may be
concluded that individuals exhibiting sizeable congenital skin nevi
may be at higher risk of developing primary pleural melanoma. Olsen
et al (9) reported that the
highest melanoma burden is always among individuals with high nevus
counts, with patients displaying ≥25 common and/or ≥1 atypical nevi
constituting a high-risk group. Normal and atypical nevi are
considered to be precursor lesions for melanoma and they are
difficult to discriminate based on clinical or histopathological
characteristics. The ABCDE rule may be applied for the clinical
diagnosis of an atypical nevus: The lesion is considered atypical
when it is asymmetrical (A), with uneven borders (B), multiple
colors (C), diameter >5 mm (D) and elevation (E) above the
surface with a maculopapular aspect (10). Although a number of findings suggest
that common nevi, atypical nevi and melanomas share certain common
molecular triggers that may define a pathogenic pathway (11), fluorescence in-situ hybridization
(FISH) has entered the field of melanoma diagnosis in recent years.
Gerami et al (12) reported a
high sensitivity (87%) and specificity (95%) for diagnosing
melanoma with a combination of four FISH probes that target 6p25
(RREB1), 6q23 (MYB), 11q13 (CCND1) and chromosome 6 centromere.
However, there is no single method that allows for a definitive
diagnosis of melanoma with either atypical or common nevi. Thus, it
is necessary to carefully analyze the patterns of clinical
expression, pathological characteristics and abnormalities of
molecular genetics.
Surgery remains the mainstay of treatment for
melanoma; however, its prognosis does not appear to be promising,
based on our experience with pulmonary melanoma. Wilson and Moran
(13) reported that five of eight
patients succumbed to metastatic disease 4–32 months after their
surgical procedures. The treatments approved by the Food and Drug
Administration for patients with advanced melanoma are limited and
they include immunotherapy, chemotherapy, molecularly targeted
therapy and conventional chemotherapeutic agents. The patient in
the present case received conventional immunotherapy and
chemotherapy and eventually succumbed due to the rapid disease
progression. There have been significant advances in the treatment
of melanoma over the last few years, with an improved understanding
of the involved molecular pathways and the critical role of the
immune system in this process (14).
Mitogen-activated protein kinase pathway inhibition and the
blockade of immune checkpoints are currently the focus of
investigation in the treatment of metastatic melanoma. In
particular, combining active therapies to overcome resistance is
key to making further advances. However, the knowledge and
accumulated experience regarding the diagnosis and treatment of
primary pleural melanomas are currently limited and the
presentation of more cases is required to optimize treatment.
Acknowledgements
This study was funded by National Natural Science
Foundation of China (grant no. 81102074).
References
|
1
|
Chang AE, Karnell LH and Menck HR: The
National Cancer Data Base report on cutaneous and noncutaneous
melanoma: a summary of 84,836 cases from the past decade. The
American College of Surgeons Commission on Cancer and the American
Cancer Society. Cancer. 83:1664–1678. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
The Brazilian National Cancer Institute.
http://www2.inca.gov.br/wps/wcm/connect/tiposdecancer/site/home/pele_melanomaJanuary
18–2014
|
|
3
|
Smith S and Opipari MI: Primary pleural
melanoma. A first reported case and literature review. J Thorac
Cardiovasc Surg. 75:827–831. 1978.PubMed/NCBI
|
|
4
|
Mohanty PP, Pasricha R, Gupta A, et al:
Malignant melanoma of pleura in a patient with giant congenital
‘bathing suit’ hairy nevus. Int J Clin Oncol. 9:410–412. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ohata Y, Haga T, Ogata S, et al: Malignant
amelanotic melanoma of the pleura without primary skin lesion: An
autopsy case report. Acta Med Okayama. 63:379–384. 2009.PubMed/NCBI
|
|
6
|
Maeda R, Isowa N, Onuma H, et al: Primary
malignant melanoma of the lung with rapid progression. Gen Thorac
Cardiovasc Surg. 57:671–674. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rezze GG, Leon A and Duprat J: Dysplastic
nevus (atypical nevus). An Bras Dermatol. 85:863–871. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bertolotto C: Melanoma: From melanocyte to
genetic alterations and clinical options. Scientifica (Cairo).
2013:6352032013.PubMed/NCBI
|
|
9
|
Olsen CM, Carroll HJ and Whiteman DC:
Estimating the attributable fraction for cancer: A meta-analysis of
nevi and melanoma. Cancer Prev Res (Phila). 3:233–245. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Roesch A, Burgdorf W, Stolz W, Landthaler
M and Vogt T: Dermatoscopy of ‘dysplastic nevi’: a beacon in
diagnostic darkness. Eur J Dermatol. 16:479–493. 2006.PubMed/NCBI
|
|
11
|
Ko JM, Velez NF and Tsao H: Pathways to
melanoma. Semin Cutan Med Surg. 29:210–217. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gerami P, Jewell SS, Morrison LE, et al:
Fluorescence in situ hybridization (FISH) as an ancillary
diagnostic tool in the diagnosis of melanoma. Am J Surg Pathol.
33:1146–1156. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wilson RW and Moran CA: Primary melanoma
of the lung: a clinicopathologic and immunohistochemical study of
eight cases. Am J Surg Pathol. 21:1196–1202. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Voskoboynik M and Arkenau HT: Combination
therapies for the treatment of advanced melanoma: a review of
current evidence. Biochem Res Int. 2014:3070592014. View Article : Google Scholar : PubMed/NCBI
|