Introduction
Chronic neutrophilic leukemia (CNL) is a rare
myeloproliferative neoplasm characterized by sustained mature
neutrophilic leukocytosis with few or no circulating immature
granulocytes, hepatosplenomegaly and hypercellular bone marrow with
a predominance of myeloid mature cells. In addition, no
Philadelphia chromosome or BCR-ABL1 fusion gene are
detected. Generally affects older adults and both genders (1,2). The cause
of CNL is not known (1). The majority
of patients have a poor prognosis, with a median survival of <3
years (3). Treatment has consisted
largely of cytoreductive agents such as hydroxyurea, with an
allogenic bone marrow transplant being the only curative treatment
(4).
The present study reports the case of a patient with
CNL complicated with Sweet's syndrome (SS) and hemorrhagic brain
lesions. The study also describes the multiple therapeutic
strategies and the difficulties in managing this disease.
Case report
Presentation and diagnosis
A 59-year-old Caucasian female, with a past history
of hypertension, was referred to The Francisco Gentil Portuguese
Institute of Oncology (Porto, Portugal) in October 2010, presenting
with asthenia, shortness of breath, abdominal pain, pallor,
splenomegaly (6 cm below the costal margin) and profuse lower limb
oedema. Laboratory analysis showed macrocytic anemia and
leukocytosis [haemoglobin level, 8.4 g/dl (normal range, 11.5–16.5
g/dl); mean cell volume, 117.3 fl (normal range, 76.0–96.0 fl);
white blood cell count, 51.33×109/l (normal range,
4.0–11.0×109/l); with 90% neutrophils; and platelet
count, 173×109/l (normal range,
150–400×109/l); a raised lactate dehydrogenase level,
392 U/l (normal range, 67–248 U/l); and a raised vitamin B12 level,
>2000 pg/ml (normal range, 191–663 pg/ml)] and mild hepatic
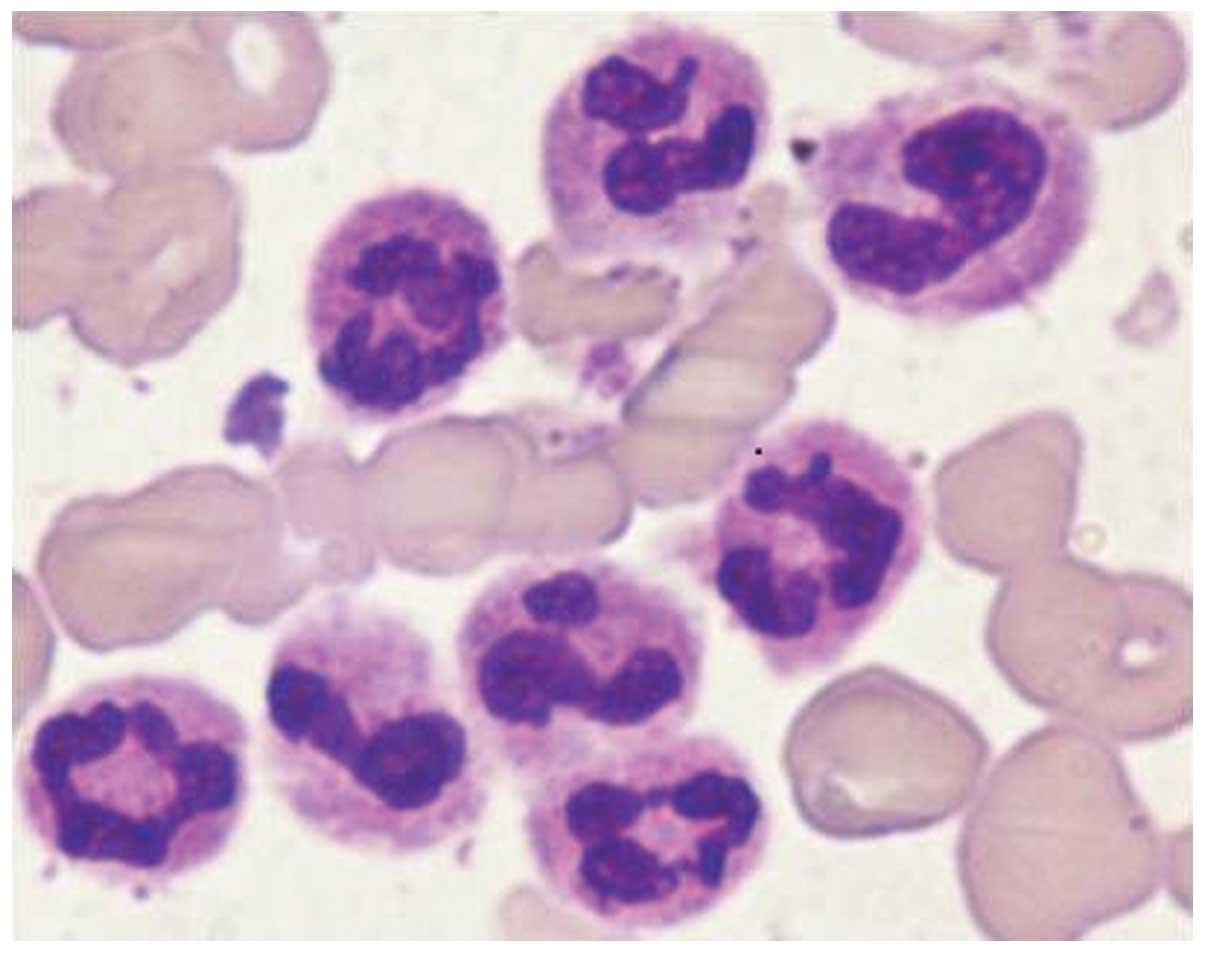
dysfunction. Bone marrow aspiration revealed hypercellular marrow
with a clear predominance of segmented neutrophils, few immature
granulocytes and no myeloblasts (Fig.
1). The biopsy confirmed these findings plus the presence of
diffuse reticulin fibrosis. The karyotype was normal and the
BCR-ABL1 and BCR-PDGFRA fusion genes were not
detected. Mutation analysis of the JAK2, MPL and
CALR genes was negative. Causes of leukemoid reaction,
including other malignancies, severe infections or inflammatory
conditions, drugs, severe hemorrhage or acute hemolysis were
excluded based on obtaining a detailed clinical history, physical
examination, imaging and laboratory studies, and the diagnosis of
CNL was determined.
Treatment and evolution
Cytoreduction with hydroxyurea (1,500 mg/day) was
started, resulting in initial hematological improvement. One month
later, fever and erythematous, well-demarcated and painful
subcutaneous nodular lesions developed in the right breast, right
upper limb and suprapubic region. These symptoms were reversed
following administration of ceftriaxone (1 g/day; duration, 3 days)
followed by 14 days of levofloxacin (500 mg/day) and suspension of
hydroxyurea. Meanwhile, disease progression was documented with
increasing splenomegaly (10 cm below the costal margin), peripheral
blood neutrophilia (12.08×109/l; normal range,
2.0–7.5×109/l), anaemia (haemoglobin 7.7 g/dl; normal
range, 11.5–16.6 g/dl) and the development of deep vein thrombosis
of the left lower limb. Intensive treatment with acute leukemia
induction-like chemotherapy was proposed, but was postponed due to
fever and profuse new skin lesions. The largest lesion (15×10 cm),
located in the right thigh, was ulcerated with extensive loss of
skin tissue. A skin biopsy revealed predominantly lobular
neutrophilic panniculitis compatible with SS. Improvement was
achieved with prednisolone (1 mg/kg) and amoxicillin and clavulanic
acid (875/125 mg/twice per day) for a duration of 2 weeks. Upon
steroid administration, a reduction in spleen size (3 cm below the
costal margin) and recovery of the hematological values were
observed, and a partial hematological response was achieved with
low doses of corticosteroids (40 mg/day) and hydroxyurea (500
mg/day). Six months later, while the skin lesions were recovering,
worsening of the anemia, thrombocytopenia and splenomegaly (20 cm
below costal margin) led to the administration of 400 mg/day
imatinib for one month. No hematological improvement was observed
and the patient required blood transfusions. When intensive
chemotherapy was finally proposed at 15 months post-diagnosis, the
patient presented with a mild headache and gait imbalance. Brain
computed tomography and magnetic resonance imaging were performed,
showing multiple hemorrhagic lesions, and the hypothesis of
cerebral nervous system invasion by CNL was consequently
considered. The lumbar puncture, even without trauma, showed a
persistently hematic and neutrophilic cerebrospinal fluid, with
negative cultures. Intensive chemotherapy with high-dose
cytarabine, daunorubicin and cyclosporine (protocol SWOG 9126)
(5) was administered for two cycles.
During treatment, several infectious complications and another set
of erythematous skin lesions were observed (Fig. 2). The skin lesions were resolved using
corticosteroids (1 mg/kg/day; duration, 2 weeks); and large
spectrum antibiotic treatment (meropenem, amikacin, vancomycin and
voriconazol) was concomitant. The final histology was inconclusive.
Following the chemotherapy, the spleen was reduced in size, the
cytopenia was improved and the neurological symptoms were resolved,
along with the brain imaging changes.
No siblings were available for allogeneic
hematopoietic progenitor transplant, so this treatment could not be
considered, and the disease was therefore only controlled for four
months. When progression was documented, best supportive and
palliative care was instituted with oral cytoreduction and
transfusion support. The patient succumbed at 28 months
post-diagnosis.
Discussion
The first case of CNL was described in 1920 by Tuohy
(6), and since then, not much has
been elucidated with regard to its pathogenesis and treatment due
to the rarity of this myeloproliferative neoplasm. CNL equally
affects the two genders and is more common in the elderly
population (>60 years) (1,4). In total, ~150 cases have been described
(1), however, a review performed in
2006 indicated that only 40 cases met the rigid criteria of the
World Health Organisation classification (7). In the present study, CNL was considered
following the proper exclusion of secondary causes of neutrophilia,
such as occult malignancy, ongoing infections and other
inflammatory conditions (8). The
diagnosis was based on peripheral blood leukocytosis with
neutrophilia, the presence of hepatosplenomegaly, hypercellular
bone marrow with a predominance of myeloid lineage (mature forms),
and the absence of the BCR-ABL1 fusion gene and the
Philadelphia chromosome. It was essential to exclude
BCR-ABL1-positive chronic myelogenous leukemia (CML), the
main variant that encodes the p230 protein, since similar to CNL,
the condition exhibits peripheral blood neutrophilia. Although
BCR-ABL1-positive CML was previously considered to be a form
of CNL (9,10), it is now considered a form of CML
(2). The BCR-PDGFRA
rearrangement and the JAK2 and CALR mutations were
also tested for in the present study. These mutations have been
identified in myeloproliferative disorders, but only JAK2
has been reported in CNL (11–13).
Recently, Maxson et al reported the association between
receptor for colony-stimulating factor 3 (CSF3R) mutations
and CNL and atypical CML (14), which
could be a promising marker of the disease (15). In the present case, the karyotype was
normal, but nearly 10% of CNL cases are associated with cytogenetic
abnormalities, including trisomy 8, 9, 21 and deletion of 11(q),
12(p), 17(p) and 20(q), the latter possibly being associated with a
more favorable prognosis (16–18).
SS, a neutrophilic dermatosis characterized by the
development of erythematous, tender plaques or nodules frequently
with fever and leukocytosis, has been associated with hematological
malignancies (19,20). The differential diagnosis is wide and
includes infectious disorders, as well as neoplastic conditions
such as leukemia cutis (19). To the
best of our knowledge, only two cases of SS have previously been
reported in association with CNL (21,22). In
the present patient, SS was histological confirmed following a
second febrile episode of cutaneous lesions, and was successfully
treated with prednisolone. Corticosteroids are the standard
treatment for this condition, but antibiotics may assist,
particularly when lesions became secondarily infected. Spontaneous
remissions can occur (19); this may
explain the apparent response to antibiotics in the first episode
(although this was not histological-proven SS) and justified their
use on the other relapses.
During disease progression, the patient presented
with neurological symptoms caused by brain hemorrhagic lesions. In
CNL, two possible causes may be responsible for this: Invasion of
the central nervous system and/or thrombocytopenia. While
thrombocytopenia and abnormal platelet function have been reported
as causes of the bleeding tendency in CNL (23,24) by
certain studies, others have demonstrated either invasion and mass
formation of neutrophils in the brain parenchyma upon autopsy
(25), or extensive infiltration of
mature and immature neutrophils, resulting in the destruction of
vascular walls (26). Based on the
absence of other systemic hemorrhagic manifestations in the present
study, these last explanation appear more likely.
There is no standard therapy for CNL. Hydroxyurea
has been shown to control the disease temporarily, while intensive
chemotherapy confers an increased risk of mortality by infection or
hemorrhage (27). The only curative
treatment is allogeneic bone marrow transplant, however, the age of
the majority of CNL patients excludes this therapeutic approach
(28). In the present case,
hydroxyurea was efficient for less than one year, and imatinib
treatment was attempted one month with no response. This selective
tyrosine kinase inhibitor has proven valid against atypical
myeloproliferative neoplasms harboring mutations in the
ABL1, KIT and platelet-derived growth factor receptor
(PDGFRB or PDGFRA) genes (29,30). In
the absence of an identified molecular marker, the success of this
therapeutic approach in anecdotal reports is believed to be due to
unknown molecular mechanisms. The study by Choi et al
reported the case of a CNL patient carrying t(15;19)(q13;p13.3) in
which cytogenetic remission was achieved following daily treatment
with 400 mg imatinib (31). In the
present case, the two cycles of intensive chemotherapy resulted in
a short partial response of four months.
The overall prognosis of patients with CNL is poor,
with a median survival time of 30 months (3,7). Death is
usually due to cerebral hemorrhage, blastic transformation or
fulminant infection (32,33). In spite of therapeutic intervention,
the present patient followed the natural history of the disease.
The rarity of CNL makes clinical trials unlikely to be conducted,
and the majority of our knowledge is based on case reports and
small series. Novel genetic markers, such as CSF3R, will provide a
better understanding of this disorder, and provide novel diagnostic
tools and therapeutic targets.
References
|
1
|
Bain B, Brunning R and Vardiman J: Chronic
neutrophilic leukaemiaIn: WHO Classification of Tumours of
Haematopoietic and Lymphoid Tissues. Swerdlow S, Campo E and Harris
NL: IARC Press; France: pp. 38–39. 2008
|
|
2
|
Vardiman J and Hyjek E: World health
organization classification, evaluation and genetics of the
myeloproliferative neoplasm variants. Hematology Am Soc Hematol
Educ Program. 2011:250–256. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Reilly JT: Chronic neutrophilic leukaemia:
a distinct clinical entity? Br J Haematol. 116:10–18. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bohm J and Schaefer HE: Chronic
neutrophilic leukaemia: 14 new cases of an uncommon
myeloproliferative disease. J Clin Pathol. 55:862–864. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
List AF, Kopecky KJ, Qillman CL, et al:
Benefit of cyclosporine modulation of drug resistance in patients
with poor-risk acute myeloid leukemia: a Southwest Oncology Group
study. Blood. 98:3212–3220. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tuohy EL: A case of splenomegaly with
polymorphonuclear neutrophil hyperleukocytosis. Am J Med Sci.
160:18–25. 1920. View Article : Google Scholar
|
|
7
|
Elliott MA: Chronic neutrophilic leukemia
and chronic myelomonocytic leukemia: WHO defined. Best Pract Res
Clin Haematol. 19:571–593. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sakka V, Tsiodras S,
Giamarellos-Bourboulis EJ and Giamarellou H: An update on the
etiology and diagnostic evaluation of a leukemoid reaction. Eur J
Intern Med. 17:394–398. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Melo JV: The diversity of BCR-ABL fusion
proteins and their relationship to leukemia phenotype. Blood.
88:2375–2384. 1996.PubMed/NCBI
|
|
10
|
Pane F, Frigeri F, Sindona M, et al:
Neutrophilic-chronic myeloid leukemia: a distinct disease with a
specific molecular marker (BCR/ABL with C3/A2 junction). Blood.
88:2410–2414. 1996.PubMed/NCBI
|
|
11
|
Klampfl T, Gisslinger H, Harutyunyan AS,
et al: Somatic mutations of calreticulin in myeloproliferative
neoplasms. N Engl J Med. 369:2379–2390. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nangalia J, Massie CE, Baxter EJ, et al:
Somatic CALR mutations in myeloproliferative neoplasms with
nonmutated JAK2. N Engl J Med. 369:2391–2405. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ortiz-Cruz K, Amog-Jones G and Salvatore
JR: Chronic neutrophilic leukemia with JAK2 gene mutation. Commun
Oncol. 9:127–131. 2012. View Article : Google Scholar
|
|
14
|
Maxson JE, Gotlib J, Pollyea DA, et al:
Oncogenic CSF3R mutations in chronic neutrophilic leukemia and
atypical CML. N Engl J Med. 368:1781–1790. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Elliott MA and Tefferi A: Chronic
neutrophilic leukemia 2014: Update on diagnosis, molecular genetics
and management. Am J Hematol. 89:651–658. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Terré C, Garcia I, Bastie JN, et al: A
case of chronic neutrophilic leukemia with deletion (11)(q23).
Cancer Genet Cytogenet. 110:70–71. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chen Y, Wang S and Wang W: Deletion of
chromosome 17 as a novel cytogenetic finding in chronic
neutrophilic leukemia: A case report. Oncol Lett. 5:1704–1706.
2013.PubMed/NCBI
|
|
18
|
Frank MB, Norwood TH and Willerford DM:
Chimeric del20q in a case of chronic neutrophilic leukemia. Am J
Hemat. 64:229–231. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cohen PR: Sweet's syndrome - a
comprehensive review of an acute febrile neutrophilic dermatosis.
Orphanet J Rare Dis. 2:342007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ratzinger G, Burgdorf W, Zelger BG and
Zelger B: Acute febrile neutrophilic dermatosis: a histopathologic
study of 31 cases with review of literature. Am J Dermatopathol.
29:125–133. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gan GG, Pasagna JF, Eow GI and Nadarajan
VS: Chronic neutrophilic leukaemia. Singapore Med J. 48:e74–e76.
2007.PubMed/NCBI
|
|
22
|
Castanet J, Lacour JP, Garnier G, et al:
Neutrophilia dermatosis associated with chronic neutrophilia
leukemia. J Am Acad Dermatol. 29:290–292. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zittoun R, Réa D, Ngoc LH and Ramond S:
Chronic neutrophilic leukemia. A study of four cases. Ann Hematol.
68:55–60. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Shigekiyo T, Miyagi J, Chohraku M, et al:
Bleeding tendency in chronic neutrophilic leukemia. Int J Hematol.
88:240–242. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kako S, Kanda Y, Sato T, et al: Early
relapse of JAK2 V617F-positive chronic neutrophilic leukemia with
central nervous system infiltration after unrelated bone marrow
transplantation. Am J Hematol. 82:386–390. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Noguchi T, Ikeda K, Yamamoto K, et al:
Severe bleeding tendency caused by leukemic infiltration and
destruction of vascular walls in chronic neutrophilic leukemia. Int
J Hematol. 74:437–441. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Elliott MA, Hanson CA, Dewald GW, Smoley
SA, Lasho TL and Tefferi A: WHO-defined chronic neutrophilic
leukemia: a long-term analysis of 12 cases and a critical review of
the literature. Leukemia. 19:313–317. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Goto H, Hara T, Tsurumi H, Tanabashi S and
Moriwaki H: Chronic neutrophilic leukemia with congenital
Robertsonian translocation successfully treated with allogeneic
bone marrow transplantation in a young man. Intern Med. 48:563–567.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Pardanani A and Tefferi A: Imatinib
targets other than bcr/abl and their clinical relevance in myeloid
disorders. Blood. 104:1931–1939. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Apperley JF, Gardembas M, Melo JV, et al:
Response to imatinib mesylate in patients with chronic
myeloproliferative diseases with rearrangements of the
platelet-derived growth factor receptor beta. N Engl J Med.
347:481–487. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Choi IK, Kim BS, Lee KA, et al: Efficacy
of imatinib mesylate (STI571) in chronic neutrophilic leukemia with
t(15;19): case report. Am J Hematol. 77:366–369. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Elliott MA, Dewald GW, Tefferi A and
Hanson CA: Chronic neutrophilic leukemia (CNL): a clinical,
pathologic and cytogenetic study. Leukemia. 15:35–40. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Amato D, Memon S and Wang C: Myeloblastic
transformation of chronic neutrophilic leukaemia. Br J Haematol.
142:1482008. View Article : Google Scholar : PubMed/NCBI
|