Introduction
Two main types of lymphoma have been described to
date, namely Hodgkin's and non-Hodgkin's lymphomas. Hodgkin's
lymphomas rarely disseminate to the extralymphatic organs; by
contrast, non-Hodgkin's lymphomas (NHLs) often invade
extralymphatic organs (1). The most
common histological type of primary pancreatic lymphoma (PPL) is
NHL. The gastrointestinal (GI) tract is the most common site of
extranodal NHL, accounting for 15–20% of all NHL cases (2). Although secondary involvement of the
pancreas is often observed in cases of GI lymphoma, PPL is an
extremely rare disease that may mimic pancreatic carcinoma. Under
2% of all extranodal malignant lymphomas and 0.5% of all pancreatic
masses are PPLs (2). Behrns et
al (1) defined the diagnostic
criteria of PPL as follows: Mass predominantly located within the
pancreas, with grossly involved lymph nodes confined to the
peripancreatic region, no palpable superficial lymphadenopathy, no
hepatic or splenic involvement, no mediastinal nodal enlargement on
chest radiography and normal white blood cell count (1). Clinically, PPL is most likely to be
misdiagnosed as pancreatic cancer (3). The cure rate of PPL is higher compared
with that of pancreatic adenocarcinoma (2). This is the case report of a patient with
a pancreatic head mass, diagnosed as diffuse large B-cell lymphoma
following endoscopic ultrasound (EUS)-guided fine-needle aspiration
(FNA) biopsy. Written informed consent was obtained from the
patient.
Case report
A 57-year-old male patient was admitted with
complaints of abdominal pain and 15% weight loss over the last 3
months. Jaundice, nausea and vomiting were added to the complaints
over the last 2 weeks. The physical examination revealed jaundice,
cachexia and abdominal tenderness. Organomegaly or lymphadenopathy
were not detected. The patient had no family history of cancer, was
not a smoker and had no history of alcohol abuse.
The laboratory test results revealed indirect
hyperbilirubinemia (total bilirubin, 16.4 mg/dl; conjugated
bilirubin, 14.3 mg/dl), hyperamylasemia (817 U/l) and
hyperlipasemia (2,249 U/l). The liver function enzymes were normal;
however, the γ-glutamyl transferase (GGT), alkaline phosphatase
(ALP) and lactate dehydrogenase (LDH) levels were increased to 333,
585 and 3,325 U/l, respectively. The erythrocyte sedimentation rate
was increased (94 mm/h) and the tumor markers were normal. The
β2-microglobulin level of the patient was 9.42 mg/l (normal range,
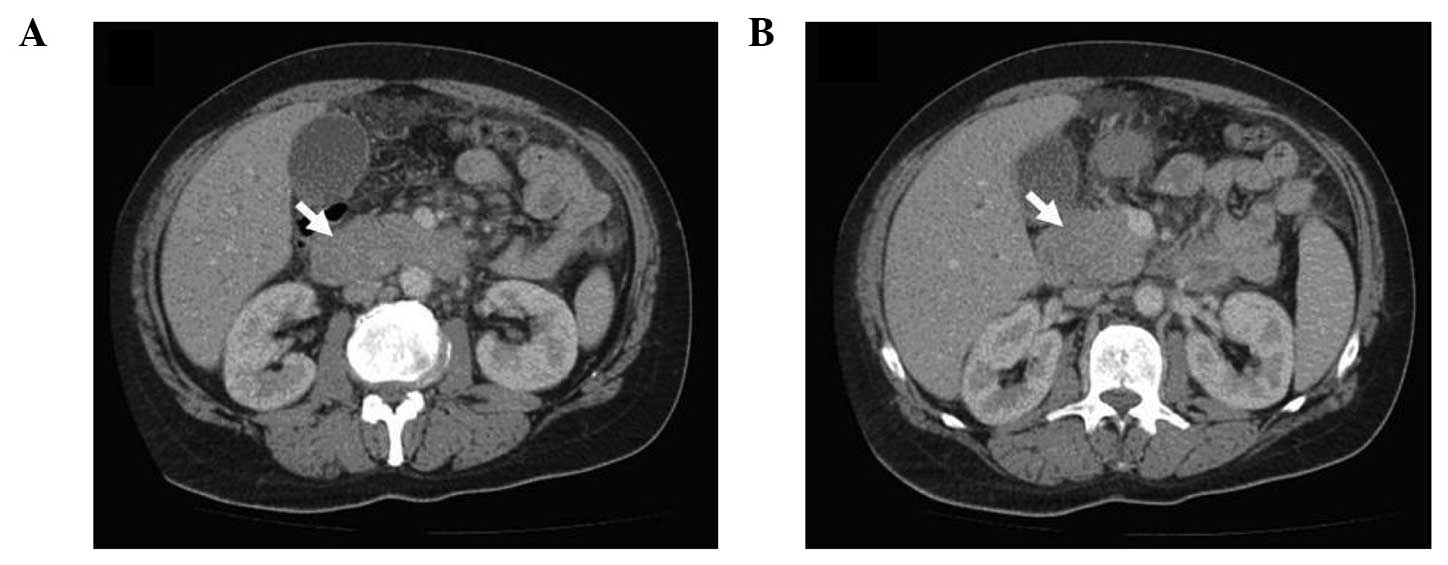
1.09–2.53 mg/l). The abdominal computed tomography (CT) revealed a
4×3-cm hypodense lesion in the head of the pancreas. Compression of
the duodenum and common bile duct by the mass and multiple
pathological lymphadenopathies were also observed (Fig. 1A and B). The EUS revealed increased
lobularity of the pancreas with hyperechoic bands, irregularity of
the main pancreatic duct and dilation of the common bile duct and
biliary tree (Fig. 2). The
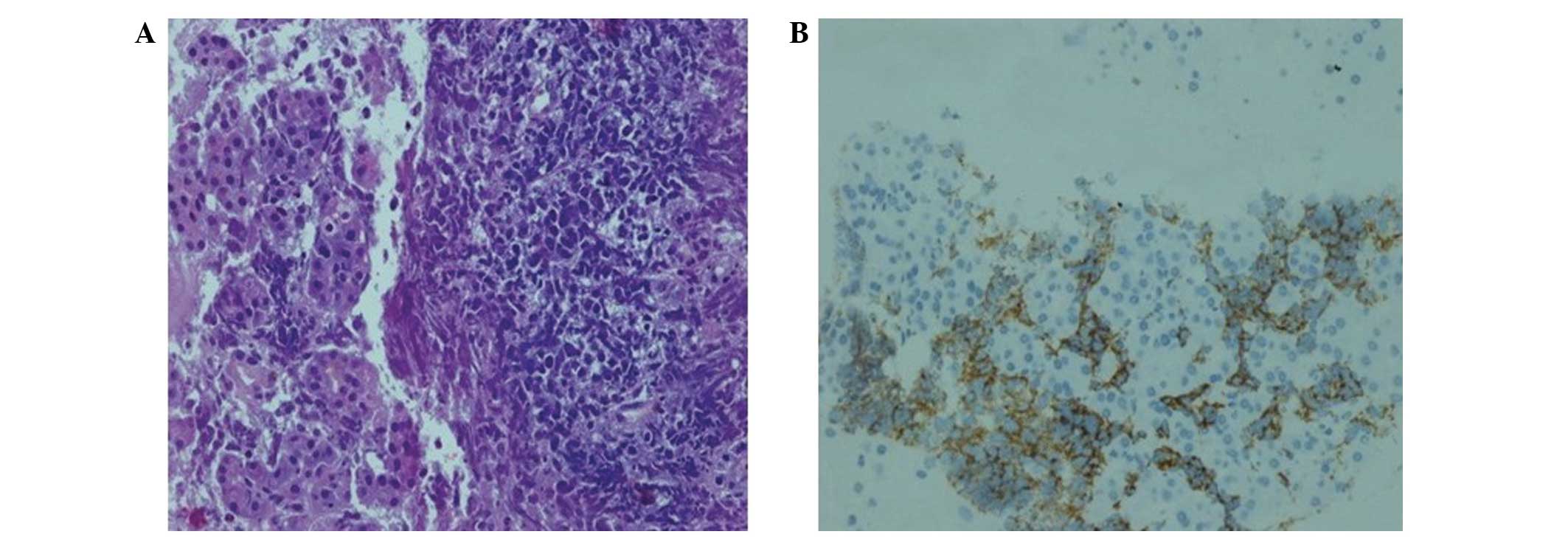
pathological evaluation of EUS-guided FNA biopsy (with a 22 G
needle) revealed that the tumor was CD20-positive and CD3- and
pancytokeratin-negative, with a high Ki-67 proliferation index
(70%), findings consistent with diffuse large B-cell lymphoma
(Fig. 3A and B). The final diagnosis
was PPL and the patient went into remission after receiving three
cycles of treatment with rituximab, doxorubicin, cyclophosphamide,
vincristine and prednisolone (R-CHOP regimen).
Discussion
PPL is a rare entity. The clinical manifestations
and radiological findings of PPL should be differentiated from
those of chronic pancreatitis, including autoimmune cases, and
occupying lesions, such as pancreatic carcinoma. PPL accounts for
<1% of all pancreatic lesions (3).
In a previous review, among 207 cases of malignant pancreatic
tumors, only 3 cases (1.5%) were pancreatic lymphomas (4). Volmar et al (5) evaluated the pathological results of
1,050 FNA biopsies of pancreatic lesions and reported that only 14
cases (1.3%) were pancreatic lymphomas. Pancreatic lymphoma is a
disease exhibiting a male predominance (male:female ratio, 7:1)
(2). The age of the patients and
duration of the symptoms are usually similar to those of pancreatic
adenocarcinoma (2). The most common
presenting symptom reported is abdominal pain (83%), followed by
abdominal mass (58%), weight loss (50%), jaundice (37%), acute
pancreatitis (12%), small-bowel obstruction (12%) and diarrhea
(12%) (3). Frequent symptoms of NHL,
such as fever, chills and night sweats, are rare in PPL (6). The patient in this study exhibited
abdominal pain, weight loss, jaundice, nausea, vomiting and acute
pancreatitis on admission. The majority of PPLs occur in the head
of the pancreas, although this tumor may also be found in the body
and tail (3). In a previousstudy,
>50% of the patients presented with an epigastric mass, the
diameter of which was >6 cm in 70% of the cases (7).
The laboratory tests for PPL are non-specific. Tumor
burden, β2-microglobulin levels >2 mg/l and high LDH levels are
poor prognostic markers (8). In the
present case, the levels of total and conjugated bilirubin,
amylase, lipase, GGT, ALP, LDH and β2-microglobulin were increased.
Although anectodal cases with increased carbohydrate antigen 19-9
(CA19-9) levels have been reported, the CA19-9 level was normal in
the present case. Imaging is crucial for the diagnosis of PPL.
Transabdominal ultrasonography, EUS, CT and magnetic resonance
imaging are well-established modalities for evaluating pancreatic
lesions (8). Two different
morphological patterns of pancreatic involvement are observed,
namely a localized, well-circumscribed tumor pattern and a diffuse
enlargement pattern, infiltrating or replacing the majority of the
pancreatic gland (9), as in the
present case. Certain radiological findings may help differentiate
PPL from the more common pancreatic adenocarcinoma: Bulky,
localized pancreatic head tumor without significant Wirsung duct
dilatation, enlarged lymph nodes below the level of the renal
veins, and invasive and infiltrating growth through to the
retroperitoneal or upper abdominal organs and the GI tract
(9).
The presence of calcification or necrosis rules out
NHL. Peripancreatic adenopathy, diffusely increased lobularity,
hyperechoic bands and enlargement of the pancreas with minimally
dilated pancreatic and intrahepatic bile ducts were observed.
Imaging techniques may suggest PPL, but are unable to distinguish
between PPL and pancreatic adenocarcinoma (6,10).
Therefore, the definitive diagnosis of PPL is based on the
cyto/histological examination (6).
Alternatively, a laparoscopy or laparotomy may be performed to
conduct a biopsy of the pancreatic mass or lymph nodes (10). EUS-guided tissue sampling of the
pancreatic mass is the optimal approach, as it is highly accurate.
Sampling with a core needle is also possible using EUS. In the
present case, diagnosis was based on EUS-guided FNA biopsy.
The treatment of PPL consists of chemotherapy or
radiotherapy (3). Behrns et al
(1) reported that the median survival
of PPL patients treated by chemotherapy or radiotherapy alone was
13 and 22 months, respectively, whereas it was ≤26 months with
combined chemoradiotherapy. Therefore, the first treatment choice
for PPL should be a combination of chemotherapy and radiotherapy,
rather than surgery. Due to the advances in EUS-guided biopsy
techniques, surgery is preferred only when EUS-guided FNA is not
available, or when the diagnosis is not possible by FNA biopsy. It
has already been proven that pancreatic resection alone does not
improve the survival rate of PPL (3).
Three cycles of R-CHOP were administered to the patient in this
case, who responded well, achieving remission.
In conclusion, we presented a rare case of PPL
presenting with abdominal pain, weight loss and obstructive
jaundice, diagnosed by EUS-guided FNA. PPL should be considered in
the differential diagnosis of pancreatic masses and its management
differs from that of other types of pancreatic tumors.
Glossary
Abbreviations
Abbreviations:
|
PPL
|
primary pancreatic lymphoma
|
|
GI
|
gastrointestinal
|
|
NHL
|
non-Hodgkin's lymphoma
|
|
CT
|
computed tomography
|
|
EUS
|
endoscopic ultrasound
|
|
FNA
|
fine-needle aspiration
|
References
|
1
|
Behrns KE, Sarr MG and Strickler JG:
Pancreatic lymphoma: Is it a surgical disease? Pancreas. 9:662–667.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Haji AG, Sharma S, Majeed KA, Vijaykumar
DK, Pavithran K and Dinesh M: Primary pancreatic lymphoma: Report
of three cases with review of literature. Indian J Med Paediatr
Oncol. 30:20–23. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hai Lin, Li SD, Hu XG and Li ZS: Primary
pancreatic lymphoma: Report of six cases. World J Gastroenterol.
12:5064–5067. 2006.PubMed/NCBI
|
|
4
|
Reed K, Vose PC and Jarstfer BS:
Pancreatic cancer: 30 year review (1947 to 1977). Am J Surg.
138:929–933. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Volmar KE, Routbort MJ, Jones CK and Xie
HB: Primary pancreatic lymphoma evaluated by fine-needle
aspiration: Findings in 14 cases. Am J Clin Pathol. 121:898–903.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Arcari A, Anselmi E, Bernuzzi P, Bertè R,
Lazzaro A, Moroni CF, Trabacchi E, Vallisa D, Vercelli A and
Cavanna L: Primary pancreatic lymphoma. Report of five cases.
Haematologica. 90:ECR092005.
|
|
7
|
Tuchek JM, De Jong SA and Pickleman J:
Diagnosis, surgical intervention and prognosis of primary
pancreatic lymphoma. Am Surg. 59:513–518. 1993.PubMed/NCBI
|
|
8
|
Tondini C, Giardini R, Bozzetti F,
Valagussa P, Santoro A, Bertulli R, Balzarotti M, Rocca A, Lombardi
F and Ferreri AJ: Combined modality treatment for primary
gastrointestinal non-Hodgkin's lymphoma: The Milan Cancer Institute
experience. Ann Oncol. 4:831–837. 1993.PubMed/NCBI
|
|
9
|
Merkle EM, Bender GN and Brambs HJ:
Imaging findings in pancreatic lymphoma: Differential aspects. AJR
Am J Roentgenol. 174:671–675. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rose JF, Jie T, Usera P and Ong ES:
Pancreaticoduodenectomy for primary pancreatic lymphoma.
Gastrointest Cancer Res. 5:32–34. 2012.PubMed/NCBI
|