Introduction
Desmoplastic fibroma of the bone is an extremely
rare, lytic, locally aggressive but non-metastatic, primary bone
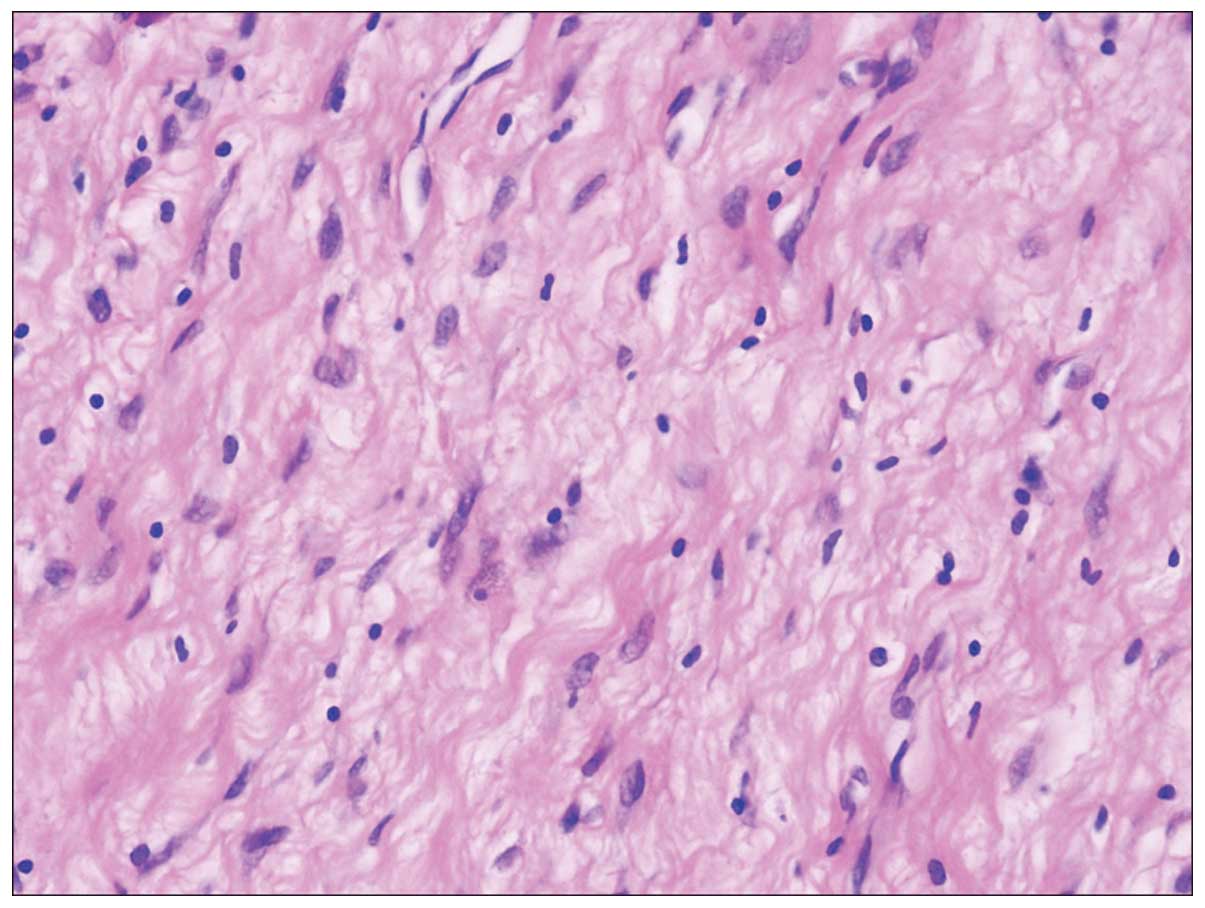
tumor. Histologically, desmoplastic fibroma of the bone is formed
of wavy fibroblasts and abundant collagenous tissue, and bears a
close resemblance to a desmoid tumor of the soft tissues. It is a
slowly progressing, locally invasive tumor, which exhibits a
characteristic production of collagen fibers (1). The most common location is the mandible,
followed by the extremities, head and spine. The incidence is
estimated at 0.06% among all bone tumors and 0.3% among benign bone
tumors (1–4). Desmoplastic fibroma of the bone occurs
most often in the first three decades of life and is found equally
among men and women (5). The most
common symptoms include pain and swelling, and 12% of patients
present with pathological fractures. However, a number of patients
may be asymptomatic and thus, the tumor is often identified
incidentally (6). On radiographs, the
lesion is lytic, sometimes poorly limited, and exhibits low signal
intensity on T2-weighted magnetic resonance imaging. The diagnosis
of the disease is predominantly based on pathological examination.
The recurrence rates in patients treated with or without resection
are 17 and 55–72%, respectively (6).
The disease was first identified by Jaffe in 1958
(7). To date, ~200 cases of
desmoplastic fibroma of the bone have been reported in the
literature. Of these, 13 have been reported in the femur (8–19), with
only two in the proximal femur (8,13) and the
remaining located in the distal femur (9–12,14–17,19,20).
To the best of our knowledge, the current study presents the
longest published follow-up of desmoplastic fibroma of the bone.
Written informed consent was obtained from the patient.
Case report
In April 1981, a 21-year-old female presented to The
First Hospital of Jilin University (Changchun, Jilin, China) with
slight lameness and pain in the proximal right thigh that had
persisted for the last month. One day prior to admission, the pain
worsened. A physical examination revealed no evident abnormalities,
with the exception of tenderness and pain on percussion of the
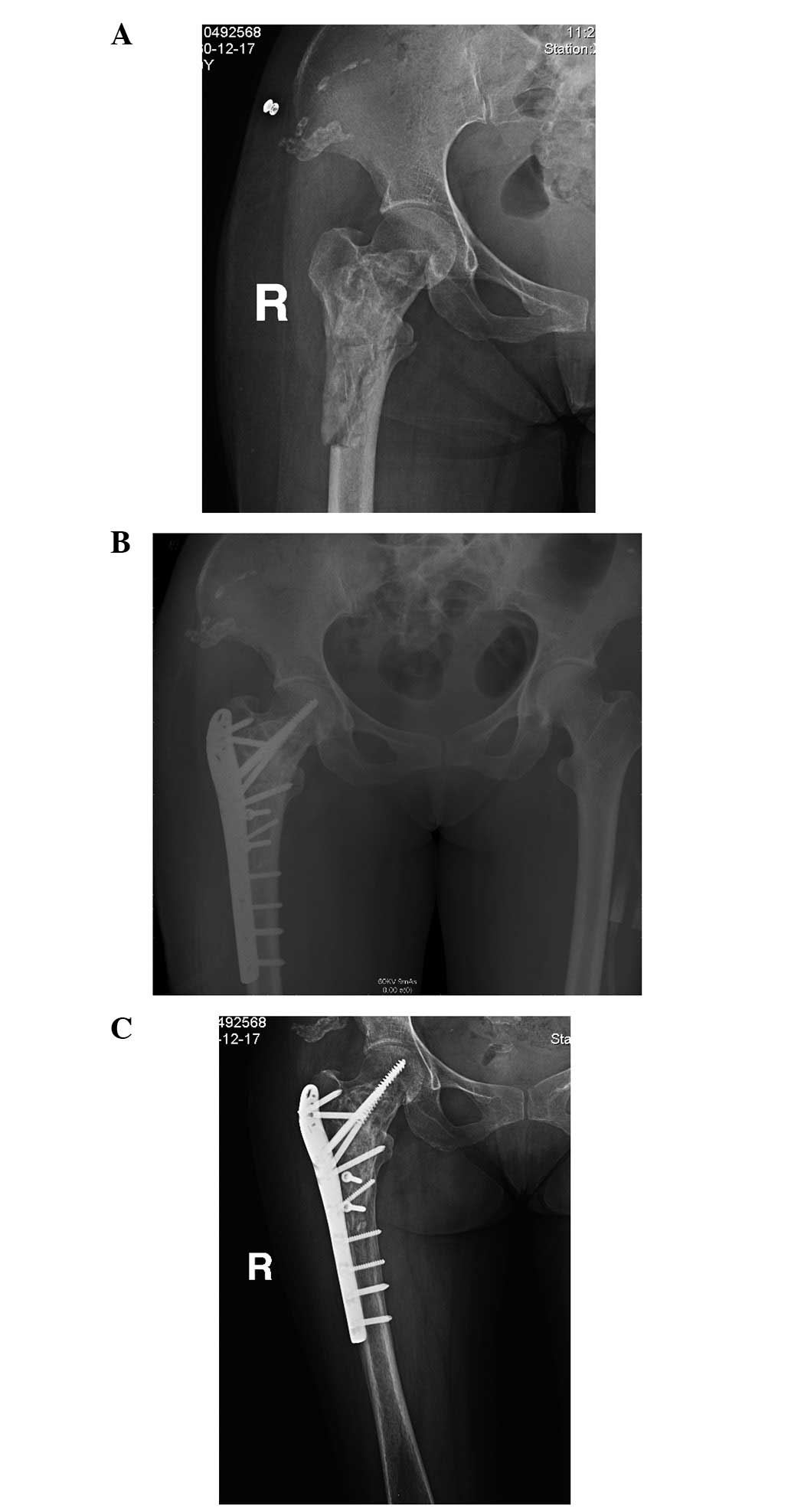
locality. Radiography showed a lytic, cystic, low-density lesion in
the proximal femur and femoral neck (Fig.
1). The lesion was expansile and the cortex was slightly
eroded. The margins were intact and sclerotic. The initial
diagnosis at admission was of a bone cyst, based on radiological
evidence, that revealed a well-defined, centrally located,
metaphyseal-diaphyseal lucent lesion, which exhibited expansion and
thinning of the cortices. The patient underwent curettage and an
allogeneic bone graft was applied. Histological examination
revealed sparse, spindle-shaped cells with low mitotic activity,
surrounded and separated from one another by abundant collagenous
tissue. Additionally, there was no necrosis (Fig. 2). Thus, based on the aforementioned
postoperative analyses and previous case, a diagnosis of
desmoplastic fibroma was determined. The patient was advised to
remain on bed-rest for three months. Despite this, one month later,
the patient suffered a pathological fracture from a fall while
walking (Fig. 3A). Surgery consisting
of an open reduction and internal fixation was performed (Fig. 3B). The fracture healed after eight
months (Fig. 3C), and the patient's
leg was partially weight-bearing. The patient was followed up at
one or two year intervals with physical and radiological
examinations. After 28 years of follow-up, the patient was able to
bear weight on the leg and has not experienced recurrence.
Discussion
The present study reports the case of a 21-year-old
female with a desmoplastic fibroma who was initially diagnosed with
a bone cyst of the proximal femur at the age of 21, was treated
with curettage and an allograft, and did well for 28 years. This
case is quite similar to four other published studies of a
desmoplastic fibroma of the proximal femur (8,13). In all
these reported cases, the patients were all initially diagnosed
with bone cysts at young age based on radiological evidence and
treated accordingly before the final diagnosis of desmoplastic
fibroma was determined. Based on the diagnostic history of previous
patients, as well as postoperative analyses, the diagnosis of bone
cyst was dismissed in favor of demoplastic fibroma in the present
case.
Desmoplastic fibroma of the bone is an extremely
rare bone tumor that resembles a desmoid tumor of the soft tissues.
In 1958, Jaffe (7) first
differentiated this bony lesion from other fibromas of bone, and
termed it ‘desmoplastic fibroma’ based on the presence of
fibroblasts and abundant collagenous tissue (21).
In comparison to the 13 reported cases of
desmoplastic fibroma of the femur (8–20), the
patient presented in the current case exhibited desmoplastic
fibroma of the proximal femur, which is extremely rare. Among the
13 cases reported previously, only two cases exhibited desmoplastic
fibroma of the proximal femur (8,13).
Radiographically, the current case presented as a lytic
metadiaphyseal lesion, with a honeycomb appearance without matrix
mineralization, which is consistent with the radiological
manifestations of a bone cyst, as well as the findings of the
previous cases. Therefore, diagnosis of desmoplastic fibroma based
on radiological evidence alone remains a challenge. The two cases
of desmoplastic fibroma of the proximal femur reported previously
(8,13)
underwent bone curettage and bone grafts, as performed in the
present case. However, both patients exhibited pathological
fractures and subsequently underwent a second surgical procedure
for internal fixation (8,13). These findings indicate that for
desmoplastic fibroma of the proximal femur, internal fixation must
be performed at an early stage, as fibroma may affect the
mechanical stability of the bone.
The differential diagnosis of a desmoplastic fibroma
should consider aggressive fibromatosis. Aggressive fibromatosis,
also known as a desmoid tumor, was described prior to desmoplastic
fibroma and is defined as a rare mesenchymal neoplasia composed of
collagenous tissue and spindle-shaped cells (7). The majority of desmoid tumors are
abdominal (69%); they can be localized intra-abdominally, within
the abdominal wall and also extra-abdominally (7,21). As the
intraosseus variant is desmoplastic fibroma, morphological
differentiation is unlikely.
The clinical manifestations of desmoplastic fibroma
include pain and swelling as the disease progresses. The diagnosis
of desmoplastic fibroma by radiography alone is challenging. Plain
X-ray shows an osteolytic, expansile, medullary lesion with
well-defined sclerotic margins, which is often located in the
metaphysis. The cortex is usually thin and there are intralesional
trabeculae, resembling soap bubbles. Computed tomography is used to
detect intraosseus tumor extension and cortical involvement, while
magnetic resonance imaging demonstrates the separation of the
intraosseus tumor from the bone, and is used to assess extraosseus
tumor growth and for pre-operative planning (1,2,21). The radiologic differential diagnosis
includes non-ossifying fibroma, fibrous dysplasia, adamantinoma,
bone cysts, giant cell tumors and metastases.
The treatment of desmoplastic fibroma varies, but
may include curettage, resection (intralesional, marginal or wide)
with or without an allograft, cryosurgery, and amputation in
recurrent cases (1–4,22,23). The rates of recurrence are 55–72%
without resection and 17% with resection (1,22,24–26).
Metastases have not been reported. The therapy for desmoplastic
fibroma is strongly dependent on the region of the body that is
affected and the aggressive nature of the lesion. When a resection
is feasible, as in the mandible and long bones, it should be
performed, as a resection has the lowest rate of recurrence
(1). Nedopil et al (21) suggested that in isolated intraosseus
lesions without evidence of extension in adjacent soft tissus, and
when resection is associated with a higher risk due to anatomical
conditions, a risk-benefit analysis should be performed. In these
cases, thorough curettage may be adequate management, as it reduces
the surgical duration, has a lower risk of infection and
facilitates a faster recovery. Once the decision has been made,
close post-operative observation, including clinical and
radiographic examination, is necessary to detect a recurrent lesion
as early as possible. We believe that curettage and allografts may
not be sufficient to treat desmoplastic fibroma and propose an
intralesional resection and close follow-up in all cases to prevent
recurrence.
In conclusion, desmoplastic fibroma in the femur is
rare, particularly in the proximal femur. The disease is easily
misdiagnosed and treated as a bone cyst. Management strategies
should involve observations of the clinical manifestations and
confirmation of the diagnosis with histological examination. To
prevent recurrence, an intralesional resection and close follow-up
after surgery are strongly recommended. In the present case, there
was no recurrence of the tumor over a 28-year follow-up period.
References
|
1
|
Böhm P, Kröber S, Greschniok A, Laniado M
and Kaiserling E: Desmoplastic fibroma of the bone. A report of two
patients, review of the literature and therapeutic implications.
Cancer. 78:1011–1023. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rabin D, Ang LC, Megyesi J, Lee DH and
Duggal N: Desmoplastic fibroma of the cranium: Case report and
review of the literature. Neurosurgery. 52:950–954. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ikeshima A and Utsunomiya T: Case report
of intra-osseous fibroma: A study on odontogenic and desmoplastic
fibromas with a review of the literature. J Oral Sci. 47:149–157.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Said-Al-Naief N, Fernandes R, Louis P,
Bell W and Siegal GP: Desmoplastic fibroma of the jaw: A case
report and review of literature. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod. 101:82–94. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Crim JR, Gold RH, Mirra JM, Eckardt JJ and
Bassett LW: Desmoplastic fibroma of bone: Radiographic analysis.
Radiology. 172:827–832. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hauben E and Cleton-Jansen AM: Fibrogenic
tumours: desmoplastic fibroma of boneWHO Classification of Tumours
of Soft Tissue and Bone. Fletcher CDM, Bridge JA, Hogendoorn P and
Mertens F: 5. 4th. IARC; Lyon: pp. 2982013
|
|
7
|
Jaffe HL: Tumors and Tumorous Conditions
of the Bones and Joints. Lea and Febiger; Philadelphia: 1958
|
|
8
|
Lichtman EA and Klein MJ: Case report 302.
Desmoplastic fibroma of the proximal end of the left femur.
Skeletal Radiol. 13:160–163. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wadhwa V, Suh KJ, Yi JH and Chhabra A:
Incidental lesion in the femoral metaphysis. Desmoplastic fibroma
of the bone. Skeletal Radiol. 42:1739–1740, 1775–1776. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Clayer M and Oakeshott R: Clin Orthop
Relat Res. Allograft bone in the treatment of desmoplastic fibroma.
A case report. Clin Orthop Relat Res. 219–224. 1994.PubMed/NCBI
|
|
11
|
Rastogi S, Varshney MK, Trikha V, Khan SA
and Mittal R: Desmoplastic fibroma: A report of three cases at
unusual locations. Joint Bone Spine. 75:222–225. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chan KW, Pun WK and Choi CH: Desmoplastic
fibroma of bone. Pathology. 19:201–203. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
GrubePagola P and Valle-Landa JC:
Desmoplastic fibroma of the femur. Radiologia. 55:359–361. 2013.(In
Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Doya H and Yaoita M: Case of desmoplastic
fibroma in the femur. Seikei Geka. 17:754–756. 1966.(In Japanese).
PubMed/NCBI
|
|
15
|
Matsumori S, Watabe E, Toyoshima Y and
Yagi Y: Primary desmoplastic fibroma of the femur. Seikei Geka.
23:275–281. 1972.PubMed/NCBI
|
|
16
|
Bertoni F, Calderoni P, Bacchini P and
Campanacci M: Desmoplastic fibroma of bone. A report of six cases.
J Bone Joint Surg Br. 66:265–268. 1984.PubMed/NCBI
|
|
17
|
Petrovichev NN, Filippova NA,
Annamukhammedov A and Karapetian RM: Case of desmoplastic fibroma
of the femur. Arkh Patol. 47:55–58. 1985.(In Russian). PubMed/NCBI
|
|
18
|
Nielsen GP, O'Connell JX, Dickersin GR and
Rosenberg AE: Collagenous fibroma (desmoplastic fibroblastoma): A
report of seven cases. Mod Pathol. 9:781–785. 1996.PubMed/NCBI
|
|
19
|
Gao S, Cai Q, Yao W, Wang J, Zhang P and
Wang X: Desmoplastic (collagenous) fibroma of the femur: A case
report and review of the literature. Oncol Lett. 6:1285–1288.
2013.PubMed/NCBI
|
|
20
|
Yokouchi M, Ueno Y, Nagano S, et al:
Extended curettage and heat ablation for desmoplastic fibroma of
the distal femur with a 12-year follow-up period: A case report.
Oncol Lett. 8:1103–1106. 2014.PubMed/NCBI
|
|
21
|
Nedopil A, Raab P and Rudert M:
Desmoplastic fibroma: A case report with three years of clinical
and radiographic observation and review of the literature. Open
Orthop J. 8:40–46. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Papagelopoulos PJ, Mavrogenis AF,
Mitsiokapa EA, et al: Current trends in the management of
extra-abdominal desmoid tumours. World J Surg Oncol. 4:212006.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Daneyemez M, Akay KM and Izci Y:
Desmoplastic fibroma of the cervical spine. Eur Spine J.
14:799–802. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Gedikoglu G, Aksoy MC and Ruacan S:
Fibrocartilaginous mesenchymoma of the distal femur: Case report
and literature review. Pathol Int. 51:638–642. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Iatrou IA, TheologieLygidakis N and
Leventis MD: Case report: Desmoplastic fibroma of the mandible in a
child presenting with TMJ dysfunction. Eur Arch Paediatr Dent.
9:105–108. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Perlick L, Zander D, Wallny T and Zhou H:
Desmoplastic fibroma of the fibula. A difficult clinical,
radiological and histological diagnosis. Zentralbl Chir.
125:895–899. 2000.(In German). View Article : Google Scholar : PubMed/NCBI
|