Introduction
Primary liver cancer (PLC) ranks as the 5th most
common cancer worldwide and the 3rd most prevalent in China
(1,2).
The majority of PLCs are hepatocellular carcinoma (HCC) or
intrahepatic cholangiocarcinoma (ICC); however, combined HCC and
cholangiocarcinoma (CC) in a single liver (cHCC-CC) is reported to
account for 0.4–14.2% of cases (3–7). Allen and
Lisa (8) classified cHCC-CC into
three subtypes: Type A, separate nodules of HCC and CC; type B,
contiguous masses of HCC and CC; and type C, individual masses
intermingling, with components of HCC and CC. Type C is regarded to
be the real cHCC-CC classification, and the majority of cases of
cHCC-CC reported are type C (9).
Types A or B, also known as double separate masses of HCC and ICC,
are extremely rare in clinical practice, particularly type A. It
has been reported that clinicopathological characteristics and
surgical outcomes generally differ between types A, B and C,
although this is poorly understood at present (10). The current study reports the case of a
patient diagnosed with HCC and ICC occurring as two separate
nodules.
Case report
A 47-year-old male was admitted to West China
Hospital of Sichuan University (Chengdu, China) in February 2014
without any symptoms and tumor was discovered by physical
examination. Physical examination revealed two nodules in the right
lobe of the patient's liver. No history of drug or alcohol abuse
was reported, however, the patient was positive for hepatitis B
virus (HBV). Abdominal ultrasound, enhanced computed tomography
(CT) and initial laboratory tests were scheduled. The laboratory
test results revealed that the blood hemoglobin (HGB) levels and
white blood cell and platelet counts were all within the normal
range. However, a liver function test revealed that aspartate
aminotransferase and alanine aminotransferase levels were mildly
elevated, and albumin levels were found to be decreased, with a
normal total bilirubin concentration. A HBV DNA titer of
5×103 copies/l was detected. Levels of the tumor markers
α-fetoprotein (AFP; 2.1 µg/µl; normal range, 0–8 µg/µl),
carcinoembryonic antigen (2.1 µg/ml; normal range, 0–5 µg/ml) and
carbohydrate antigen (CA) 125 (16.2 U/ml; normal range, 0–35 U/ml)
were all within the normal limits, however, the CA19-9 level was
marginally elevated. The abdominal ultrasound revealed two tumors
in segment (S) VII (tumor A) and S VI (tumor B), with liver echo
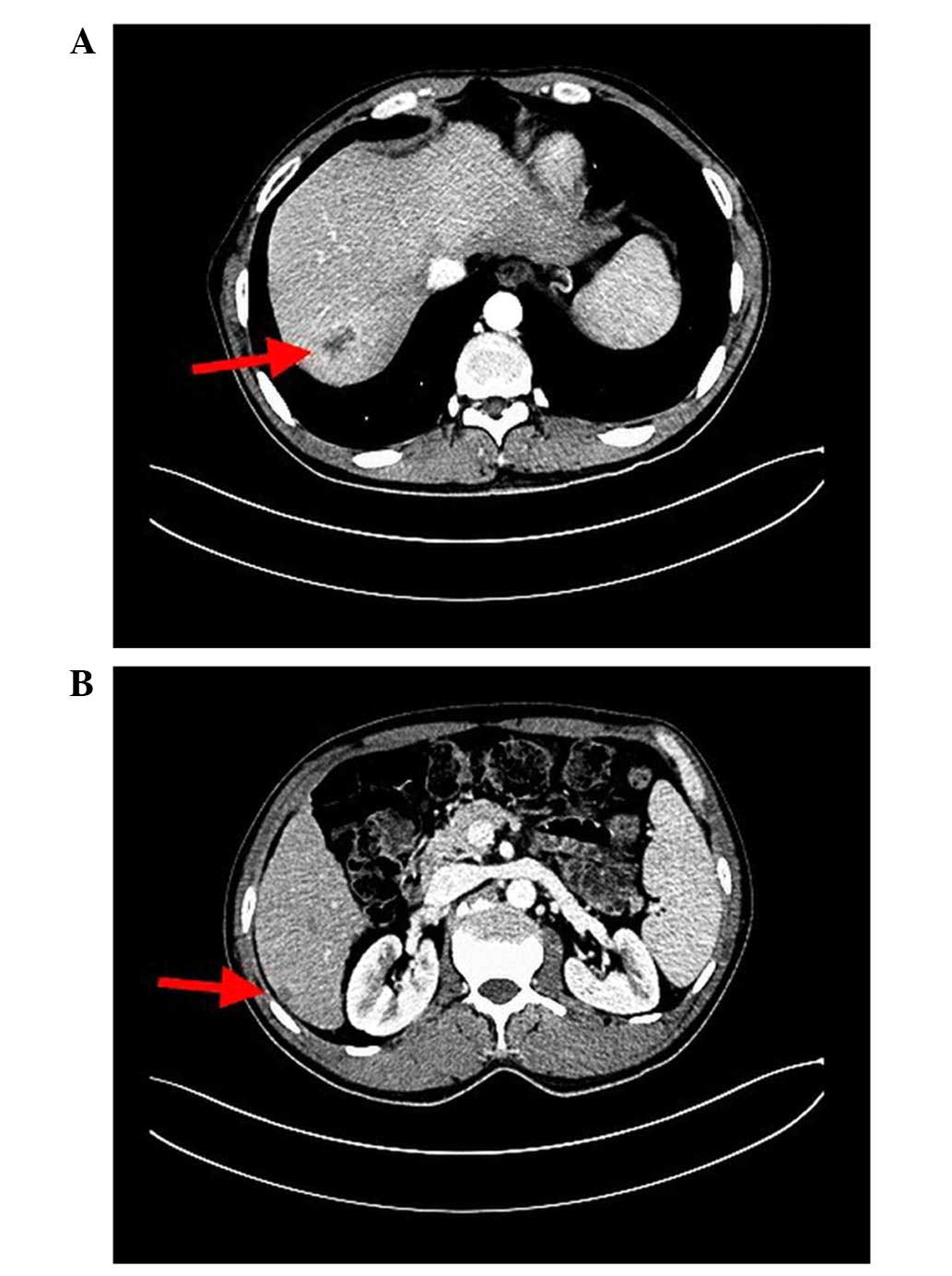
enhancement. In addition, enhanced spiral CT scanning of the upper
abdomen showed that the two masses, tumors A and B, were both
located in the right posterior lobe and measured 4 cm and 1 cm in
diameter, respectively (Fig. 1).
Esophageal varices were also observed. Enhanced CT imaging revealed
that tumor A was heterogeneously enhanced in the arterial phase,
and enhancement decreased in the portal venous phase, while tumor B
was heterogeneously enhanced in these two phases.
Based on these findings, primary HCC with
intrahepatic metastasis was the initial diagnosis; there was no
evidence of extrahepatic lesions on enhanced brain and chest CT
imaging and bone scanning. Therefore, surgical resections of liver
S VI and VII were performed under full anesthesia within 110 min.
The patient experienced ~200 ml blood loss during surgery, and no
blood transfusion was required. Following an uneventful recovery,
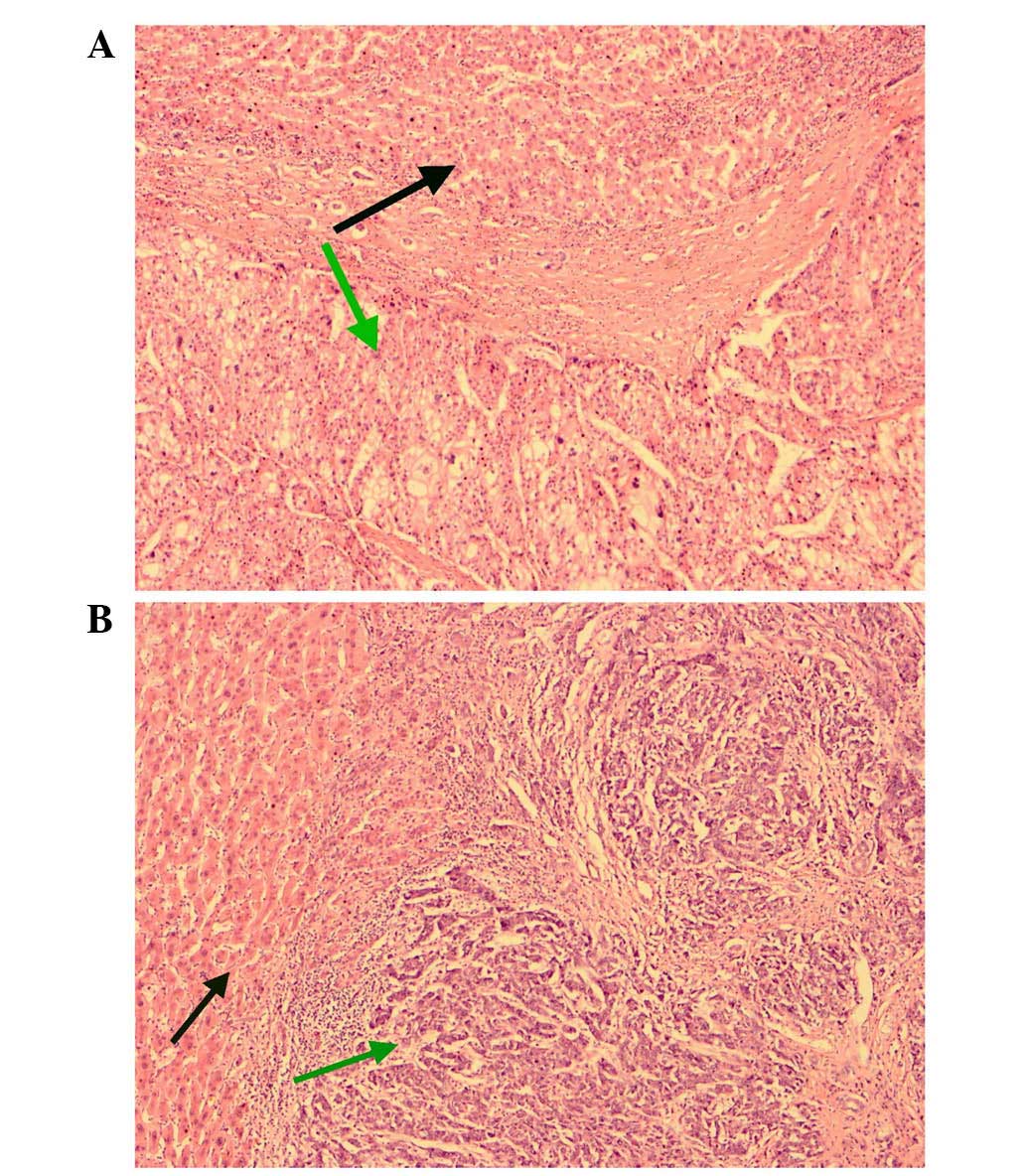
the patient was discharged on the 7th day after surgery. The biopsy
of the liver revealed cirrhosis with an Ishak score of 6 (11). Tumor A was found to be moderately
differentiated HCC with a complete capsule and without tumor
thrombus. By contrast, tumor B was a poorly differentiated
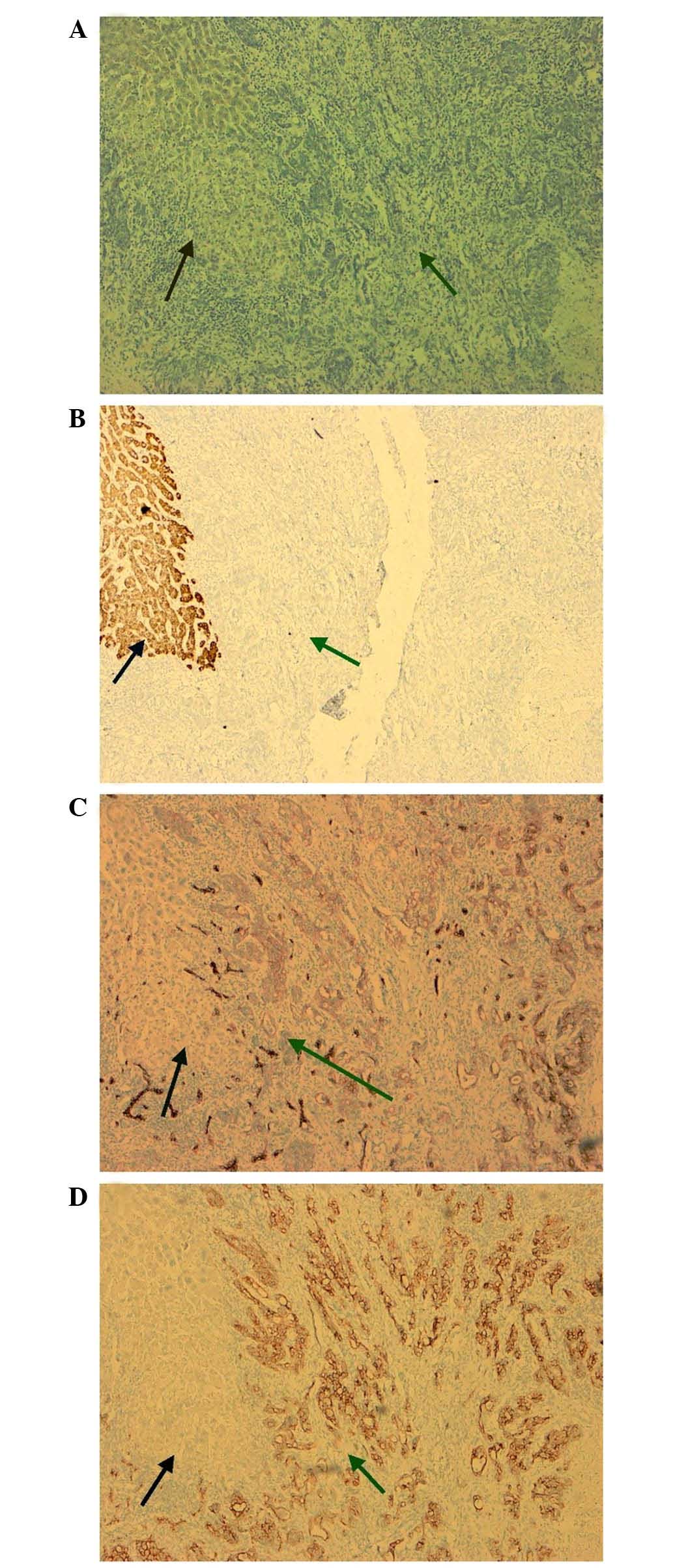
adenocarcinoma with liver capsule violation (Fig. 2). In order to elucidate the source of
tumor B, an immunohistochemical analysis of the tumor was
performed. The cells of tumor B stained positively for cytokeratins
(CKs) 7 and 19, and negatively for hepatocyte antigen (Hepa) and
AFP (Fig. 3). Thus, these finding
indicated that tumor B had a biliary origin, confirming a diagnosis
of ICC. During the 8 months of follow-up, the patient has undergone
liver ultrasonography and tumor marker tests at 3-month intervals,
and no signs of recurrence have been observed. No further treatment
has been administered.
The patient provided written informed consent for
the publication of this report.
Discussion
The simultaneous occurrence of HCC and ICC in a
single liver, in the form of separated nodules, is extremely rare.
To the best of our knowledge, there have been no previous reports
about the incidence of the type A cHCC-CC, and only several English
language case reports are available in the literature (12).
It is well-established that HCC is closely
associated with HBV or hepatitis C virus (HCV) infections (2,13), while
HBV or HCV infections are also risk factors for ICC (14). In the present report, the patient had
a long history of HBV infection, including increasing HBV DNA
titers, and no standard antiviral treatments were administered.
Tumor markers are intrinsically linked to certain
tumors, however, tumor markers cannot necessarily be used to
confirm an exact final diagnosis (15). For example, the level of blood CA19-9,
a tumor marker of ICC, may also increase when HCC invades the
biliary tract; therefore, elevated levels cannot conclusively
diagnose a liver mass as ICC, but may suggest the possibility of
ICC. In the present report, the AFP level of the patient, which is
regarded to be the most significant tumor maker of HCC (16), was within the normal limits, however,
CA19-9 was marginally elevated. Thus, whilst they provide some
information, tumor markers cannot be used as the sole foundation of
the diagnosis, and the final diagnosis depends on pathological
assessment of biopsied specimens.
The pathological characteristics of HCC and ICC also
differ from one another: According to the consensus of pathological
immunohistochemical examinations, Hepa and AFP are reliable markers
for HCC (17), while CK7 and CK19 are
valuable markers for differentiating ICC from HCC (18). In the present report, tumor A was a
typical HCC mass, and tumor B cells stained positively for CK7,
CK19 and CK20, and negatively for Hepa and AFP. Negative AFP and
Hepa staining indicated that the tumor did not originate from
hepatocytes, while the CK7 and CK19 positive staining suggested
that the tumor arose from cholangiocytes (19,20).
The use of abdominal ultrasound to detect liver
masses is common for screening and follow-up; however, the
characterization of a malignant tumor by ultrasound often leads to
ambiguity due to the variable and non-specific features observed
using this modality, and is limited to the experience of the
sonologist (21). HCC and ICC masses
may perform differently on enhanced CT imaging: ICC typically
appears with peripheral enhancement on the early phase, and mild
centripetal progression of enhancement in the venous phase, while
HCC generally exhibits enhancement in the whole tumor during the
hepatic arterial phase and negative enhancement during the portal
venous phase (‘fast in and out’) (22). The biomolecular mechanism of
enhancement differences on spiral CT between HCC and ICC is related
to the differential expression of vascular endothelial growth
factor (23). However, it remains
difficult to characterize tumors of small diameter or with atypical
features by CT imaging. In the present report, the diameter of the
ICC nodule in S VI was ~1 cm, and the CT image revealed irregular
enhancement in the arterial and venous phases; thus, it could not
be fully distinguished from certain metastatic tumors (24). Therefore, even combining the tumor
marker and imaging findings, correctly diagnosing the double
primary hepatic masses as HCC and ICC preoperatively was still
challenging.
Hepatectomy is the primary treatment option for all
malignant liver tumors, however, different approaches to lymph node
dissection are usually taken between HCC and ICC (25). It is essential to dissect lymph nodes
for ICC, but not for HCC (26). In
the present case, the patient only underwent liver resection and
not lymph node dissection, due to the misdiagnosis of tumor B
preoperatively. Despite this, the patient has experienced
disease-free survival to date, owing to the small diameter of the
tumor and absence of lymph node metastasis. It may be possible to
avoid uncertainty regarding the necessity for lymph node dissection
by implementing frozen section biopsy intraoperatively, when the
evidence from preoperative tests is unable to fully eliminate the
possibility of ICC (10).
In summary, the present study reported an extremely
rare case of PLC consisting of double hepatic tumors, with HCC and
ICC occurring simultaneous at separate locations within a single
liver. In such cases, it is difficult to determine a diagnosis
preoperatively due to uncharacteristic performances on tumor marker
analysis and imaging studies; the final diagnosis depends on
pathological and immunohistochemical examination of biopsy
specimens. Surgery remains the primary treatment option. The
present case highlights the potential value of frozen section
biopsy performed intraoperatively that may alert surgeons to the
necessity for lymph node dissection.
References
|
1
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Estimating the world cancer burden: Globocan 2000. Int J Cancer.
94:153–156. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chan AC, Cheung TT, Fan ST, Chok KS, Chan
SC, Poon RT and Lo CM: Survival analysis of high-intensity focused
ultrasound therapy versus radiofrequency ablation in the treatment
of recurrent hepatocellular carcinoma. Ann Surg. 257:686–692. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jarnagin WR, Weber S, Tickoo SK, Koea JB,
Obiekwe S, Fong Y, DeMatteo RP, Blumgart LH and Klimstra D:
Combined hepatocellular and cholangio-carcinoma: Demographic,
clinical and prognostic factors. Cancer. 94:2040–2046. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tang D, Nagano H, Nakamura M, Wada H,
Marubashi S, Miyamoto A, Takeda Y, Umeshita K, Dono K and Monden M:
Clinical and pathological eatures of Allen's type C classification
of resected combined hepatocellular and cholangiocarcinoma: A
comparative study with hepatocellular carcinoma and
cholangiocellular carcinoma. J Gastrointest Surg. 10:987–998. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Goodman ZD, Ishak KG, Langloss JM,
Sesterhenn IA and Rabin L: Combined
hepatocellular-cholangiocarcinoma. A histologic and
immunohistochemical study. Cancer. 55:124–135. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kassahun WT and Hauss J: Management of
combined hepatocellular and cholangiocarcinoma. Int J Clin Pract.
62:1271–12782008. View Article : Google Scholar
|
|
7
|
Kim KH, Lee SG, Park EH, et al: Surgical
treatments and prognoses of patients with combined hepatocellular
carcinoma and cholangiocarcinoma. Ann Surg Oncol. 2009.16(3):
623–629. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Allen RA and Lisa JR: Combined liver cell
and bile duct carcinoma. Am J Pathol. 25:647–655. 1949.PubMed/NCBI
|
|
9
|
Yano Y, Yamamoto J, Kosuge T, Sakamoto Y,
Yamasaki S, Shimada K, Ojima H, Sakamoto M, Takayama T and Makuuchi
M: Combined hepatocellular and cholangiocarcinoma: a
clinicopathologic study of 26 resected cases. Jpn J Clin Oncol.
33:283–287. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cao J, Huang L, Liu C, Li J, Zhang X, Shen
J, Li J, Lu L, Xu F, Yan J, Wu M, Lau WY and Yan Y: Double primary
hepatic cancer hepatocellular carcinoma and intrahepatic
cholangiocarcinoma) in a single patient: A clinicopathologic study
of 35 resected cases. J Gastroenterol Hepatol. 28:1025–1031. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Everhart JE, Wright EC, Goodman ZD,
Dienstag JL, Hoefs JC, Kleiner DE, Ghany MG, Mills AS, Nash SR,
Govindarajan S, et al: HALT-C Trial Group: Prognostic value of
Ishak fibrosis stage: Findings from the hepatitis C antiviral
long-term treatment against cirrhosis trial. Hepatology.
51:585–594. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Maganty K, Levi D, Moon J, Bejarano PA,
Arosemena L, Tzakis A and Martin P: Combined hepatocellular
carcinoma and intrahepatic cholangiocarcinoma: Outcome after liver
transplantation. Dig Dis Sci. 55:3597–3601. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Franssen B, Alshebeeb K, Tabrizian P,
Marti J, Pierobon ES, Lubezky N, Roayaie S, Florman S and Schwartz
ME: Differences in surgical outcomes between hepatitis B- and
hepatitis C-related hepatocellular carcinoma: A retrospective
analysis of a single North American center. Ann Surg. 260:650–656.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shaib YH, El-Serag HB, Davila JA, Morgan R
and McGlynn KA: Risk factors of intrahepatic cholangiocarcinoma in
the United States: A case-control study. Gastroenterology.
128:620–626. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mant D and Primrose J: CEA monitoring in
colorectal cancer is not a waste of time. BMJ. 18:3482014.
|
|
16
|
Shim JH, Yoon DL, Han S, Lee YJ, Lee SG,
Kim KM, Lim YS, Lee HC, Chung YH and Lee YS: Is serum
alpha-fetoprotein useful for predicting recurrence and mortality
specific to hepatocellular carcinoma after hepatectomy? A test
based on propensity scores and competing risks analysis. Ann Surg
Oncol. 19:3687–3696. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jeng KS, Sheen IS, Jeng WJ, Yu MC, Hsiau
HI, Chang FY and Tsai HH: Activation of the sonic hedgehog
signaling pathway occurs in the CD133 positive cells of mouse liver
cancer Hepa 1–6 cells. Onco Targets Ther. 6:1047–1055. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Massani M, Stecca T, Fabris L, Caratozzolo
E, Ruffolo C, Furlanetto A, Morton S, Cadamuro M, Strazzabosco M
and Bassi N: Isolation and characterization of biliary epithelial
and stromal cells from resected human cholangiocarcinoma: A novel
in vitro model to study tumor-stroma interactions. Oncol Rep.
30:1143–1148. 2013.PubMed/NCBI
|
|
19
|
Moritoki Y, Ueno Y, Kanno N, Yamagiwa Y,
Fukushima K, Gershwin ME and Shimosegawa T: Amniotic epithelial
cell-derived cholangiocytes in experimental cholestatic ductal
hyperplasia. Hepatol Res. 37:286–294. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Xu J, Sasaki M, Harada K, Sato Y, Ikeda H,
Kim JH, Yu E and Nakanuma Y: Intrahepatic cholangiocarcinoma
arising in chronic advanced liver disease and the
cholangiocarcinomatous component of hepatocellular
cholangiocarcinoma share common phenotypes and
cholangiocarcinogenesis. Histopathol. 59:1090–1099. 2011.
View Article : Google Scholar
|
|
21
|
Stuntz R, Kochert E, Kehrl T and Schrading
W: The effect of sonologist experience on the ability to determine
endotracheal tube location using transtracheal ultrasound. Am J
Emerg Med. 32:267–269. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kim TK, Jang HJ and Wilson SR: Imaging
diagnosis of hepatocellular carcinoma with differentiation from
other pathology. Clin Liver Dis. 9:253–279. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wagner K, Peters M, Scholz A, Benckert C,
Ruderisch HS, Wiedenmann B and Rosewicz S: Activin A stimulates
vascular endothelial growth factor gene transcription in human
hepatocellular carcinoma cells. Gastroenterology. 126:1828–1843.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kang Y, Lee JM, Kim SH, Han JK and Choi
BI: Intrahepatic mass-forming cholangiocarcinoma: Enhancement
patterns on gadoxetic acid-enhanced MR images. Radiology.
264:751–760. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Amini N, Ejaz A, Spolverato G, Maithel SK,
Kim Y and Pawlik TM: Management of lymph nodes during resection of
hepatocellular carcinoma and intrahepatic cholangiocarcinoma: A
systematic review. J Gastrointest Surg. 18:2136–2148. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Popescu I and Dumitrascu T:
Curative-intent surgery for hilar cholangiocarcinoma: Prognostic
factors for clinical decision making. Langenbecks Arch Surg.
399:693–705. 2014. View Article : Google Scholar : PubMed/NCBI
|