Introduction
Breast cancer diagnosed during pregnancy or the
postpartum period is known as pregnancy-associated breast cancer
(PABC). Breast cancer is the second most common neoplasia in
pregnancy, following cervical cancer (1). The incidence of PABC is ~1:3,000–10,000
in developed countries, an incidence that appears to be increasing
as a result of delayed childbearing (2). Breast cancer is most likely to
metastasize to bone, followed by the lungs and liver. The overall
incidence of bone metastasis from breast advanced neoplasia is
65–75% (3). The associated
complications of bone metastasis include osteolytic lesions, pain,
hypercalcemia, fracture and nerve compressions (4). In the literature, there are few reports
about osteolytic lesions in pregnancy and no data regarding the
treatment of such femoral fractures. Furthermore, to the best of
our knowledge, there is currently no information on breast cancer
diagnosis secondary to the detection of bone metastases in
pregnancy.
The present study reports the management of a case
of PABC, which was diagnosed by the presence of bone metastasis,
and reviews the relevant literature.
Case report
In April 2012, a 41-year-old 29-week primigravida
was referred to Salesi Hospital (Ancona, Italy) for a severe
lumbosciatica in the left side, refractory to medical therapy, and
a risk of preterm delivery. The patient's personal and family
history was negative for major disease. Spinal magnetic resonance
imaging and an electromyography of the left leg were performed, and
no abnormalities were detected. Analgesic treatment and
neurosurgical counseling were performed. During the neurosurgical
exam, a spontaneous pathological fracture of the left femur
occurred. Femoral X-rays (Fig. 1)
revealed an osteolytic lesion on the distal third of the left femur
diaphysis.
Damage control orthopedic principals were applied
and an external fixator was placed for temporary femoral
stabilization. Initially, the bone lesion was suspected for
metastatic breast cancer. A biopsy specimen from the intraosseus
lesion was obtained. Bilateral breast ultrasound was conducted and
a 6.5×3.5 cm hypoechoic lesion involving the lower-inner quadrant
of the left breast with increased vascularity was identified. Serum
analysis of tumor markers [carcinoembryonic antigen, cancer antigen
(CA) 19-9, CA 72-4 and CA 15-3] revealed increased levels of CA
72-4. Histological evaluation of the femoral lesion resulted in a
diagnosis of metastases from breast adenocarcinoma.
Immunohistochemical analysis revealed the presence of estrogen
(40%) and progesterone receptors (90%), as well as MIB1
proliferative activity (25%). Human epidermal growth factor
receptor-2/neu expression, evaluated through HercepTest kit (Dako,
Glostrup, Denmark), was negative. Neoplastic cells were positive
for cytokeratin 7, mammaglobin and cytokeratin 8/18 (antibody
Cam5,2), while negative for cytokeratin 20, thyroid transcription
factor 1 and cromogranine. It was suggested by the oncologist that
the cancer was staged following delivery, to facilitate planning of
the subsequent treatment program. A multidisciplinary meeting
between the patient, gynecologist, orthopedic surgeon, oncologist
and neonatologist was conducted to discuss the appropriate timing
of the childbirth. Following receipt of informed consent, a
cesarean section was performed at 32 gestational weeks and a vital
male was born (weight, 1720 g; Apgar, 8/9).
Following delivery, the external fixation was
removed and an intramedullary nail was inserted for definitive
treatment of femoral fracture (Fig.
2).
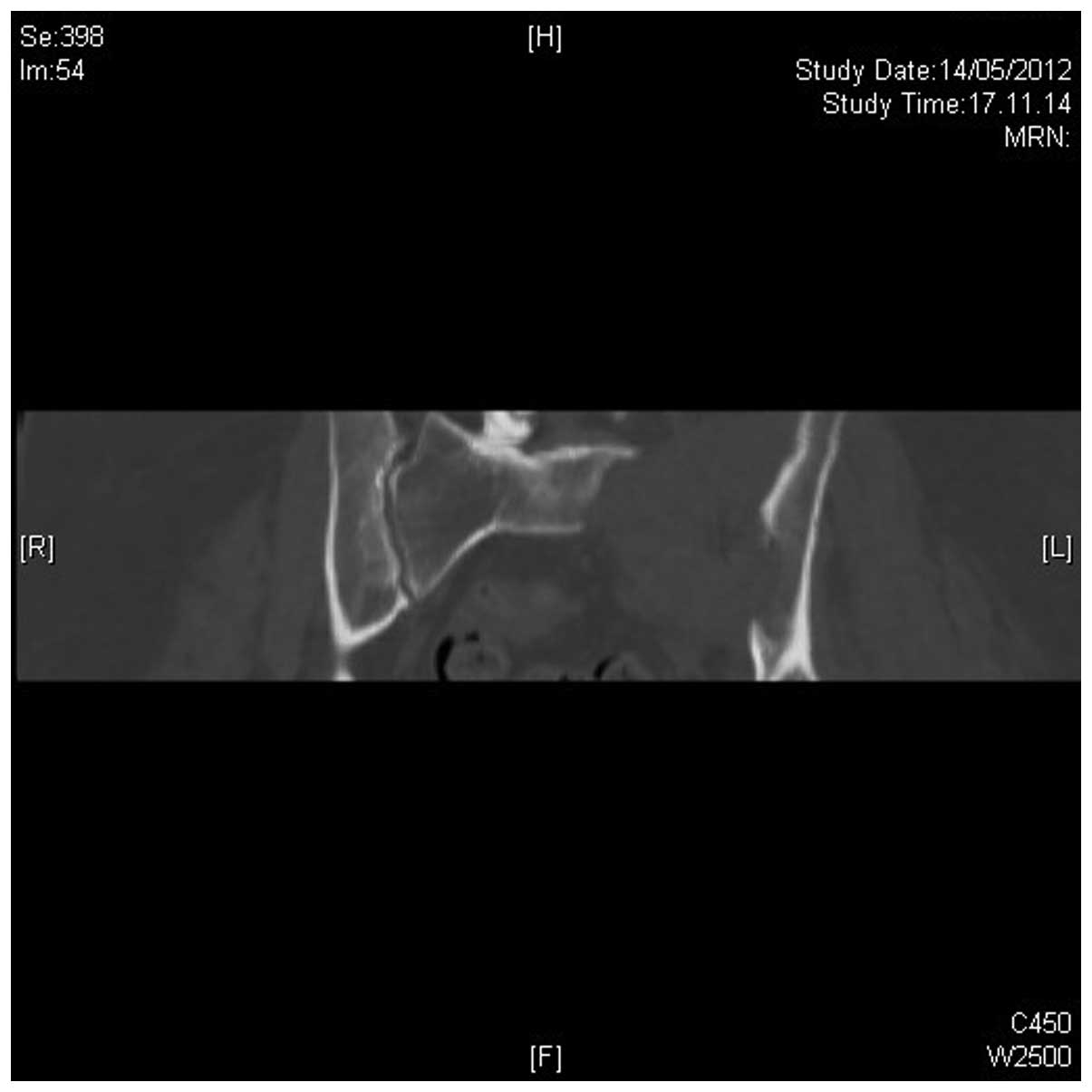
A computed tomography (CT) scan of the chest was
performed and identified a left breast lesion and abnormal
bilateral intrapulmonary nodules. CT of the neck revealed abnormal
laterocervical lymph nodes bilaterally. Cerebral CT was negative,
while CT of the abdomen revealed an 8.4×6.2 cm hyper-vascularized
mass on the sacroiliac joint, inducing a wide area of left
sacroiliac bone lysis. A bone scintigraphy was performed, and
femoral and sacroiliac joint scans demonstrated high uptake.
The patient underwent CT-guided percutaneous
radiofrequency thermoablation of the sacroiliac lesion, which
resulted in pain relief. The procedure was performed at the
Department of Interventional Radiology, Umberto I Hospital (Ancona,
Italy) in the CT room under aseptic conditions by an interventional
radiologist (Dr Enrico Paci) and an orthopedic surgeon (Dr Rocco
Politano) with anesthesiological assistance. The percutaneous
approach and needle route were preliminarily assessed by the
orthopedic surgeon and interventional radiologist according to
imaging data and the position of the lesion with regard to the
neurovascular structures. The first CT scan was obtained using an
adhesive marker plate with radiopaque coordinates (GuideLines;
Beekley Medical, Bristol, CT, USA) to determine the route of the
needle from the skin to the lesion. Local anesthesia was
administered following skin preparation and sterilization. The
Radiofrequency StarBurst®, SEMI-FLEX Electrosurgical Device,
AngioDynamics (Queensbury, NY, USA) was directly introduced through
the soft tissue above the lesion due to erosion of the cortical
bone by the mass. The RITA® StarBurst SEMI-FLEX Device has a
flexible trocar that is able to bend if required, for example, in
order to fit into the CT gantry. The device is able to bend to a
radius of ~2 inches/~5 cm. Subsequently, an additional CT scan was
performed to monitor the needle's direction, and verify the correct
deployment of the five electrode/needles. Ablation was performed at
two subsequent needle positions, from depth to surface, for a total
time of <15 min (Fig. 3).
Adjuvant treatment with oral Tamoxifen (20 mg/day)
and intramuscular GnRH-a (Decapeptyl®; 11.25 mg every 3 months)
commenced in association with intravenous Zoledronic acid (4 mg
every 3–4 weeks), prescribed due to its action on osteoclasts and
antitumor properties. Follow-up CT of the chest and abdomen was
performed two months subsequent to thermoablation of the sacroiliac
lesion and the commencement of adjuvant treatment. The chest CT
revealed a reduction in the size of the left breast lesion (4×5
cm), and abdominal CT revealed a significant decrease in the
sacroiliac lesion with a maximum diameter of 6 cm. Four months
following delivery, the patient underwent monolateral
mastectomy.
A follow-up 18 months post-percutaneous
radiofrequency thermoablation of the sacroiliac lesion, the patient
exhibited no metastatic bone pain and CT revealed a reduction in
the lesion and bone formation of anterior cortical bone of the
sacroiliac. Furthermore, femoral X-ray indicated fracture healing
and a reduction of the lesion. CT of the chest and abdomen was also
conducted and revealed analogous findings compared with previous CT
scans (Fig. 4). Written informed
consent was obtained from the patient for the publication of this
study.
Discussion
Though breast cancer is the second most common
cancer in pregnant women, it occurs relatively infrequently
(2), and metastatic breast cancer
during pregnancy is a rare event. In the literature there are few
studies regarding this topic. A review of the literature identified
eleven reported cases of metastatic breast cancer in pregnant
women. The primary diagnosis of breast cancer had been reached
prior to pregnancy in nine of these cases (5). These nine women subsequently presented
with metastasis or breast cancer progression during pregnancy.
Initial diagnosis of metastatic disease in pregnancy was made in
the remaining two cases (6,7). It is well established that bone is a
frequent site for metastases among patients with breast cancer,
with a reported frequency of 65–75% (3). The present case is a notable example of
breast cancer initially diagnosed in pregnancy at 30 gestational
weeks, as a result of a pathological femoral fracture. It is well
known that pregnancy induces reversible bone turn-over and loss,
particularly in the second and third trimester, with a significant
decrease in bone mineral density (8).
It may be hypothesized that these changes in bone metabolism
enhance the severity of bone metastasis in pregnancy, considering
that the bone microenvironment has a crucial role in the
development of malignant bone lesions. In fact, an increase in bone
resorption results in enhanced release of growth factors, which may
promote bone tumor formation (9).
Furthermore, since there are few studies regarding
osteolytic lesions in pregnancy and no data on the treatment of
such femoral fractures in the literature, to the best of our
knowledge, the present case report is the first to report the
management of pathological femoral fracture secondary to breast
cancer in pregnancy. Traumatic injuries are detected in 6–7% of
pregnant women (10). These are the
most common non-obstetric risk factors for miscarriage and preterm
delivery. Damage control orthopedic principles are applied when
early total care is impossible (11).
In addition, previous studies have reported rare cases of fractures
due to transient osteoporosis during pregnancy, which may be
treated with internal fixation or arthroplasty (10,12).
A significant dilemma for obstetricians and
oncologists arises following the diagnosis of metastasis from
breast cancer in pregnancy. This is due to the fact that metastatic
cancer must be treated as incurable and the quality of life of the
patient, as well as the newborn, must be considered. In the present
case, percutaneous radiofrequency thermoablation of the sacroiliac
lesion had an essential role in improving the quality of life of
the patient by exerting marked pain relief.
References
|
1
|
Fedarapalli P and Jain S: Breast cancer in
pregnancy. J Obstet Gynaecol. 26:1–4. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Genin AS, Lesieur B, Gligorov J, Antoine
M, Selleret L and Rouzier R: Pregnancy-associated breast cancers:
Do they differ from other breast cancers in young women? Breast.
21:550–555. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Coleman RE: The clinical use of bone
resorption markers in patients with malignant bone disease. Cancer.
94:2521–2533. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mundy GR: Metastasis to bone: Causes,
consequences and therapeutic opportunities. Nat Rev Cancer.
2:584–593. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Litton JK, Theriault RL and
Gonzalez-Angulo AM: Breast cancer diagnosis during pregnancy.
Womens Health (Lond Engl). 5:243–249. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
El-Safadi S, Wuesten O and Muenstedt K:
Primary diagnosis of metastatic breast cancer in the third
trimester of pregnancy: A case report and review of the literature.
J Obstet Gynaecol Res. 38:589–592. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Azim HA Jr and Peccatori FA: Treatment of
metastatic breast cancer during pregnancy: We need to talk! Breast.
17:426–428. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tranquilli AL, Giannubilo SR and
Corradetti A: Ultrasound measurement of pregnancy-induced changes
in maternal bone mass: A longitudinal, cross-sectional and
biochemical study. Gynecol Endocrinol. 18:258–262. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gnant M, Dubsky P and Hadji P:
Bisphosphonates: prevention of bone metastases in breast cancer.
Recent Results Cancer Res. 192:65–91. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ahmadi A, Fakheri T, Amini-Saman J,
Amanollahi O, Mordi M, Nasrabadi MA, Gholipour Y, Dehghani R and
Bazargan-Hejazi S: Traumatic injuries in pregnant women: A case of
motor vehicle accident for ‘Ground Round’ discussion. J Inj
Violence Res. 3:55–59. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Barraco RD, Chiu WC, Clancy TV, Como JJ,
Ebert JB, Hess LW, Hoff WS, Holevar MR, Quirk JG, Simon BJ and
Weiss PM: EAST Practice Management Guidelines Work Group: Practice
management guidelines for the diagnosis and management of injury in
the pregnant patient: The EAST Practice Management Guidelines Work
Group. J Trauma. 69:211–214. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Emami MJ, Abdollahpour HR, Kazemi AR and
Vosoughi AR: Bilateral subcapital femoral neck fractures secondary
to transient osteoporosis during pregnancy: A case report. J Orthop
Surg (Hong Kong). 20:260–262. 2012.PubMed/NCBI
|