Introduction
Non-small cell lung cancer (NSCLC) is the most
common neoplasm and remains the leading cause of cancer-related
mortality worldwide (1). In 2008, a
total of 1.6 million new cases of lung cancer were diagnosed
worldwide, accounting for 13% of all cancer cases. Furthermore,
lung cancer accounted for 1.4 million mortalities and 18% of all
cancer-related mortalities worldwide in 2008 (1). The most common symptoms of lung cancer
include fatigue, loss of appetite, shortness of breath, cough, pain
and blood in the sputum (2). The
majority of lung cancer cases (80%) are classified as NSCLC
(3). Of these patients, >65%
present with locally advanced or metastatic disease (4). Surgical resection is the most effective
treatment for early-stage NSCLC. However, despite complete surgical
resection, 30–75% of patients with stage I–IIIA NSCLC suffer a
relapse and succumb to the disease (1,5,6). The most common sites of recurrence are
the regional lymph nodes, lung, liver, bone, brain and adrenal
gland (7). We experienced three cases
of rare solitary omental metastasis of NSCLC, which had been
subjected to surgical resection.
This study describes the clinical characteristics
and outcome of the three patients with solitary omental metastasis
of NSCLC and also reviews the literature reported previously. The
study was approved by the ethics committee of Osaka Medical Center
for Cancer and Cardiovascular Diseases (Osaka, Japan), and written
informed consent was obtained from the patient or the patient's
family.
Case report
Case 1
A 72-year-old female with a history of cigarette
smoking [Brinkman index (BI), 525] who had a left lower lobe lung
cancer (squamous cell carcinoma) underwent left lower lobe
resection and mediastinal lymph node dissection. Postoperative
chemotherapy was not enforced. The solitary abdominal tumor was
diagnosed with 18F-fluorodeoxyglucose positron emission
tomography and computed tomography (PET/CT) 4 months after
pneumonectomy and was referred to the Department of Surgery at the
Osaka Medical Center for Cancer and Cardiovascular Diseases.
Physical examination was not noteworthy. The laboratory examination
revealed serum carcinoembryonic antigen (CEA) of 3.3 ng/dl (normal
range, 0–5 ng/dl) and CA19-9 of 41 U/ml (normal range, <37
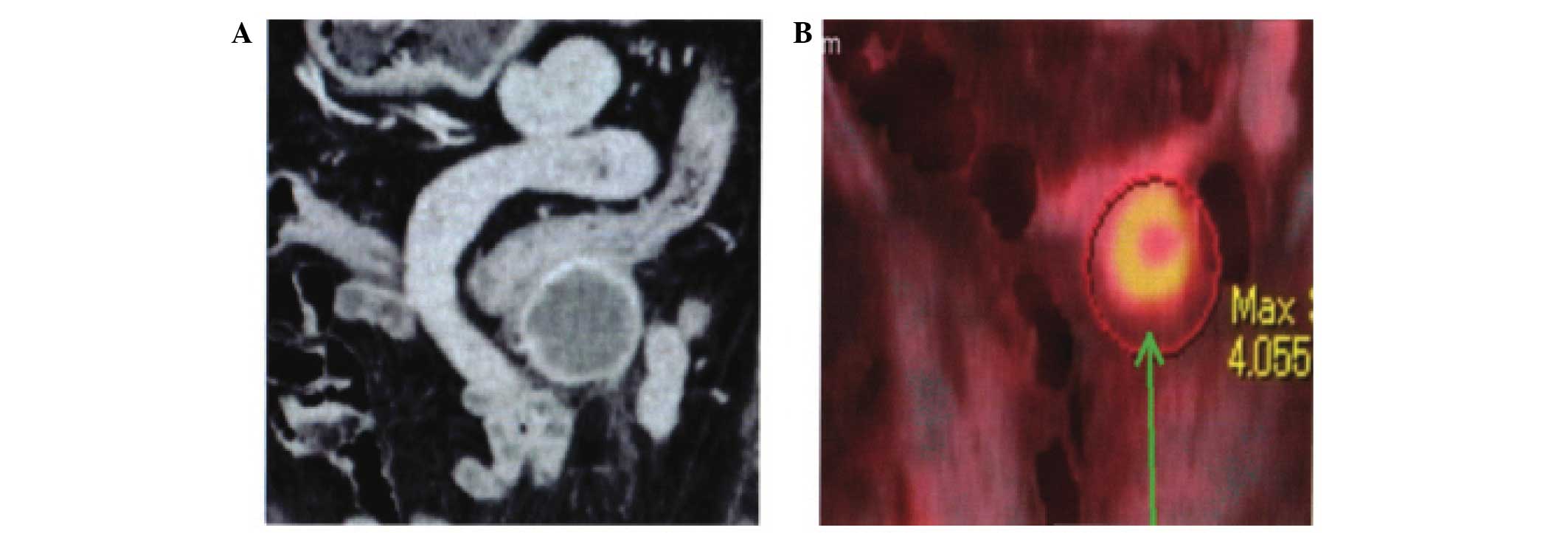
U/ml). A CT examination was performed and revealed an enhanced
solitary tumor measuring 30×26 mm around the stomach (Fig. 1A). The maximum standardized uptake
value (SUV Max) was 4.055 on the PET/CT (Fig. 1B). Laparotomy was performed and a
tumor was detected in the greater omentum, which had invaded into
the transverse colon. The tumor was resected, and partial resection
of the transverse colon was also performed. Histopathological
examination with hematoxylin and eosin revealed poorly
differentiated invasive squamous cell carcinoma. The patient was
followed up without postoperative chemotherapy and succumbed to
recurrent disease in the mesenteric lymph nodes, liver, lung and
peritoneum 8 months after the second surgery.
Case 2
A 64-year-old male with a history of cigarette
smoking (BI, 500) who had a cancer of the left pulmonary hilum
(pleomorphic carcinoma) underwent chemotherapy. The first regimen,
which included cisplatin (CDDP; 80 mg/m2) plus
vinorelbine (VNR; 25 mg/m2), was stopped due to the
occurrence of diarrhea. The second regimen was carboplatin (area
under the plasma concentration time curve 5) plus gemcitabine
(1,000 mg/m2). The patient suffered a recurrence in the
mediastinal lymph node 14 months after chemotherapy and radiation
therapy (60 Gy/30 fr) was performed. The metastatic lymph node
demonstrated a complete response. A solitary omental tumor appeared
46 months and 70 months after the initial start of treatment and
the patient was subjected to surgery twice. Physical examination
was not noteworthy. The laboratory examination revealed a CEA of
20.6 ng/ml and a CA19-9 of 5 U/ml at the first recurrence. The
second recurrent case revealed a CEA of 14.3 ng/ml and a CA19-9 of
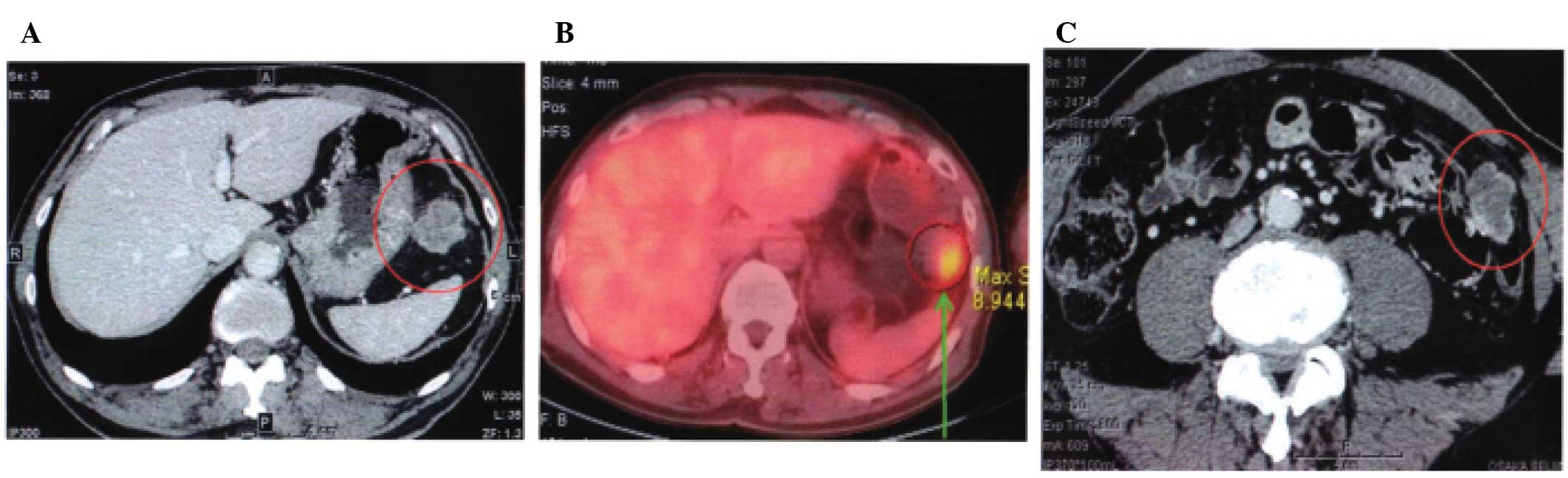
12 U/ml. A CT scan revealed an abdominal tumor measuring 34×23 mm
around the stomach for the first time (Fig. 2A). The SUV Max for the first recurrent
omental tumor was 8.944 from the PET/CT (Fig. 2B). The second recurrence appeared
beside the transverse colon as a 30×25-mm enhanced tumor.
Laparotomy was performed twice and each solitary nodule was
identified in the greater omentum. The histological examination
confirmed that the omental tumor was a metastasis from lung
pleomorphic carcinoma. The second recurrent tumor was also
identical to the primary pleomorphic lung carcinoma. Eight months
after the second surgery, recurrent tumors appeared in the
pancreas, para-aortic lymph nodes and the peritoneum, and the
patient underwent chemotherapy (pemetrexed; 500
mg/m2).
Case 3
A 59-year-old male with a history of cigarette
smoking (BI, 1140) who suffered a cancer of the left pulmonary
hilum (pleomorphic carcinoma) underwent chemotherapy. The regimens
used were CDDP (80 mg/m2) plus VNR (25
mg/m2). A solitary abdominal tumor was detected with CT
6 months after the start of chemotherapy, and the patient was
referred for surgery. Physical examination was not noteworthy.
Laboratory studies revealed a CEA of 1.7 ng/ml, cytokeratin 19
fragment of 12 U/ml (normal range, 0–2.8 ng/ml) and neuron specific
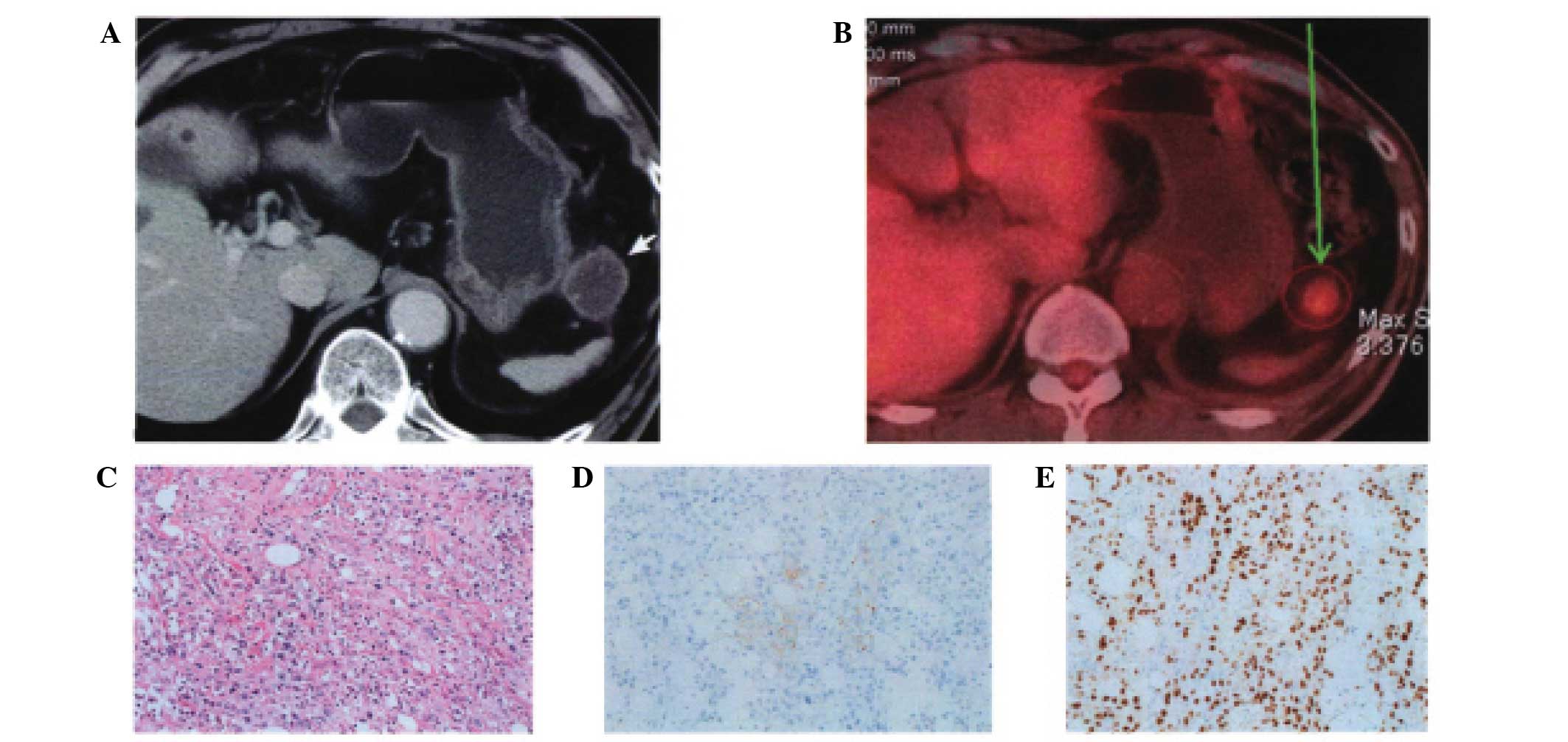
enolase of 11.6 ng/ml (normal range, <16.3 ng/ml). CT
examination revealed an intra-peritoneal tumor measuring 28×26 mm
around the stomach (Fig. 3A). The SUV
Max was 3.376 with PET/CT (Fig. 3B).
The tumor had infiltrated into the stomach wall and pancreas tail,
and it was resected with a combination of partial gastrectomy,
distal pancreatectomy and splenectomy. The histological examination
revealed that tumor cells had invaded into the spleen, pancreas and
stomach wall, accompanied by massive vascular invasion. The tumor
cells were composed of spindle-shaped polygonal tumor cells and
demonstrated no clear differentiation trend (Fig. 3C). Immunohistochemical examination
revealed that the tumor cells expressed vimentin cytokeratin 5/6,
anti-cytokeratin CAM5.2 and p63, but did not express TTF-1 and
Napsin A (Fig. 3D and E).
Postoperative chemotherapy (S-1, 80 mg/m2) was
performed. The patient demonstrated no recurrence 20 months after
surgery.
Discussion
In this study, we have reported three cases of an
extremely rare solitary metastatic omental tumor from NSCLC, which
had been surgically resected at our department. The three cases
that we experienced were incidentally diagnosed with CT and/or
PET-CT and had no symptoms. There have only been a few studies of
solitary omental metastasis from NSCLC. Therefore, we reviewed a
total of seven cases, comprising four cases reported in the past
(8–10)
and our three cases. The characteristics of the patients as well as
the treatment administered and the outcome of treatment are shown
in Tables I and II. The mean age of patients was 58.6
(44–72) years old. The male to female ratio was 6:1. A history of
smoking was observed in all patients. Surgical resection for
omental tumors was performed in all cases. The histology of the
primary site revealed pleomorphic carcinoma in three cases out of
seven (43%). Considering that pleomorphic carcinoma in NSCLC is
extremely rare (0.3% of all lung cancers), omental metastasis is
assumed to be relatively common in pleomorphic carcinoma of the
lung (11). Pulmonary pleomorphic
carcinoma was identified as a specific type of lung cancer with
pleomorphic sarcomatoid or sarcomatous elements by the 1999 World
Health Organization classification (12). Pulmonary pleomorphic carcinoma has a
more aggressive clinical course and demonstrates a poorer outcome
than other NSCLCs (11,13,14).
Fujiwara et al reported on cases of gastrointestinal
metastasis of NSCLCs (15). These
authors reported that three cases out of nine with gastrointestinal
metastasis revealed a histology of pleomorphic carcinoma. These
results indicate that pulmonary pleomorphic carcinoma has a
tendency to metastasize to the abdominal region. Previous studies
reveal that the common extrathoracic metastatic sites are the brain
(32%), bone (23%), liver (9%), adrenal gland (6%) and
gastrointestinal tracts (0.5%) (7,15,16). Omental metastasis of NSCLC is
extremely rare and studies of solitary omental metastasis which
were subjected to surgery are few. Omental metastasis from NSCLC is
considered to be formed through the vascular or lymphatic vessels.
Oshika and Hashimoto reported on two patients who suffered gastric
wall metastasis following resection of omental metastasis, which
may indicate that lung cancer cells first metastasize to the
gastric wall through the vascular vessels and then metastasize to
the omentum through the lymphatic vessels (9). Stomach metastasis from NSCLC is also
extremely rare and there have been few studies to date (17,18).
 | Table I.Characteristics and treatment of
primary non-small cell lung cancer. |
Table I.
Characteristics and treatment of
primary non-small cell lung cancer.
| No. | First author
(ref.) | Age | Gender | Histological
type | Stage | Treatment for primary
tumor | Time to
metastasis |
|---|
| 1 | Nakamura et al
(8) | 61 | M | Large cell
carcinoma | IV | Resection | 0 |
| 2 | Oshika et al
(9) | 44 | M | Large cell
carcinoma | IV | Resection | 0 |
| 3 |
| 60 | M | Adenocarcinoma | IB | Resection | 0 |
| 4 | Tamura et al
(10) | 50 | M | Pleomorphic
carcinoma | IA | Resection | 5 months |
| 5 | Present case 1 | 72 | F | Squamous cell
carcinoma | IB | Resection | 4 months |
| 6 | Present case 2 | 64 | M | Pleomorphic
carcinoma | IIIB | Chemotherapy;
radiationa | 46
monthsb |
| 7 | Present case 3 | 59 | M | Pleomorphic
carcinoma | IIIB | Chemoradiation | 6 months |
 | Table II.Treatment outcome of solitary omental
metastasis from non-small cell lung cancer. |
Table II.
Treatment outcome of solitary omental
metastasis from non-small cell lung cancer.
|
|
|
| Recurrence following
omentectomy |
|
|---|
|
|
|
|
|
|
|---|
| No. | Treatment for omental
tumor | Infiltration | Perioda | Treatment | Outcomec |
|---|
| 1 | Resection;
chemoradiation | None |
| None | 13 months
(relapse-free) |
| 2 | Resection;
chemotherapy | None |
| None | 14 months
(relapse-free) |
| 3 | Resection;
chemotherapy | None |
| None | 14 months
(relapse-free) |
| 4 | Resection | None | 3 weeks | None | 7 months,
deceased |
| 5 | Resection | Colon | 3 months | None | 8 months,
deceased |
| 6 | Resection | None | 24
monthsb | Resection | 40 months, alive |
|
| Resection | None | 8 months | Chemotherapy | with
recurrenced |
| 7 | Resection;
chemotherapy | Stomach,
pancreas | None | Chemotherapy | 20 months, alive with
recurrence |
Due to the limited number of cases with solitary
omental metastasis, the significance of the surgical approach for
solitary omental carcinoma remains unclear. Table II reveals that with the exception of
two patients (#4 and our case 1), the patients survived more than
one year; our case 2 survived 40 months and case 3 survived 20
months following resection of omental metastasis. Therefore,
surgical intervention for solitary omental metastasis from NSCLC
should be considered if no other metastasis is detected.
Chemotherapy following resection of omental metastasis may be
required, since long-time survivors (our case 2 and 3) continued
postoperative chemotherapy.
In conclusion, although omental metastasis from
NSCLC is extremely rare, it should be considered when a patient
with history of NSCLC, particularly if the histology is pleomorphic
carcinoma, has a solitary tumor around the stomach. Surgical
resection for solitary omental metastasis from NSCLC may be
indicated if no other metastasis is detected.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Iyer S, Roughley A, Rider A and
Taylor-Stokes G: The symptom burden of non-small cell lung cancer
in the USA: A real-world cross-sectional study. Support Care
Cancer. 22:181–187. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lozano R, Naghavi M, Foreman K, et al:
Global and regional mortality from 235 causes of death for 20 age
groups in 1990 and 2010: A systematic analysis for the Global
Burden of Disease Study. Lancet. 380:2095–2128. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Morgensztern D, Ng SH, Gao F and Govindan
R: Trends in stage distribution for patients with non-small cell
lung cancer: A National Cancer Database survey. J Thorac Oncol.
5:29–33. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rubins J and Unger M: Colice GL the
American College of Chest Physicians: Follow-up and surveillance of
the lung cancer patient following curative intent therapy: ACCP
evidence-based clinical practice guideline (2nd edition). Chest.
(132 Suppl)3:S355–S367. 2007. View Article : Google Scholar
|
|
6
|
Arriagada R, Bergman B, Dunant A, et al:
Cisplatin-based adjuvant chemotherapy in patients with completely
resected non-small-cell lung cancer. N Engl J Med. 350:351–360.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sugimura H, Nichols FC, Yang P, Allen MS,
Cassivi SD, Deschamps C, Williams BA and Pairolero PC: Survival
after recurrent nonsmall-cell lung cancer after complete pulmonary
resection. Ann Thorac Surg. 83:409–417. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nakamura T, Jibiki M, Ikari H, et al: A
case report of unknown-origin tumor metastasized to mediastinal
lymph nodes and omentum. Haigan Jpn J Lung Cancer. 33:7931993.
|
|
9
|
Oshika Y and Hashimoto H: Two cases of
non-small cell lung cancer with metastasis to the omentum. Haigan
Jpn J Lung Cancer. 48:118–122. 2008. View Article : Google Scholar
|
|
10
|
Tamura R, Kobayashi H, Imai Y, et al: A
case report of omental metastasis of pleomorphic carcinoma of the
lung which regrowed surprisingly fast after surgical resection. Jpn
J Gastroenterol Surg. 43:299–305. 2010. View Article : Google Scholar
|
|
11
|
Rossi G, Cavazza A, Sturm N, et al:
Pulmonary carcinoma with pleomorphic, sarcomatoid, or sarcomatous
elements: a clinocopathologic and immunohistochemical study of 75
cases. Am J Surg Pathol. 27:311–324. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Travis WD, Colby TV, Corrin B, et al:
Histological Typing of Lung and Pleural Tumours (World Health
Organization, International Histological Classification of Tumours)
(3rd). New York: Springer. 1999. View Article : Google Scholar
|
|
13
|
Fishback NF, Travis WD, Moran CA, et al:
Pleomorphic (spindle/giant cell) carcinoma of the lung. A
clinicopathologic correlation of 78 cases. Cancer. 73:2936–2945.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mochizuki T, Ishii G, Nagai K, Yoshida J,
Nishimura M, Mizuno T, Yokose T, Suzuki K and Ochiai A: Pleomorphic
carcinoma of the lung clinicopathological characteristics of 70
cases. Am J Surg Pathol. 32:1727–1735. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fujiwara A, Okami J, Tokunaga T, Maeda J,
Higashiyama M and Kodama K: Surgical treatment for gastrointestinal
metastasis of non-small-cell lung cancer after pulmonary resection.
Gen Thorac Cardiovasc Surg. 59:748–752. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Antler AS, Ough Y, Pitchumoni CS, Davidian
M and Thelmo W: Gastrointestinal metastases from malignant tumors
of the lung. Cancer. 49:170–172. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nakamura H, Mizokami Y, Iwaki Y, Shiraishi
T, Ohtsubo T, Miura S, et al: Lung cancer with metastases to the
stomach and duodenum. Reports of three cases. Dig Endosc.
15:210–215. 2003. View Article : Google Scholar
|
|
18
|
Aokage K, Yoshida J, Ishii G, et al:
Long-term survival in two cases of resected gastric metastasis of
pulmonary pleomorphic carcinoma. J Thorac Oncol. 3:796–799. 2008.
View Article : Google Scholar : PubMed/NCBI
|