Introduction
Acute epidural hematoma (AEDH) mostly occurs
following head trauma, and may result in skull fracture and tearing
of the middle meningeal artery or venous systems. Spontaneous AEDH
is extremely rare, and may be caused by infections of the adjoining
sinus or air cell structures, dural vascular anomalies, tumors or
coagulopathies (1).
Hepatocellular carcinoma (HCC) is one of the most
common malignant tumors worldwide, with a high incidence in
Southeast Asia and sub-Saharan Africa, where hepatitis B and C are
prevalent (2). HCC commonly
metastasizes to the lung, regional lymph nodes, peritoneum and
adrenal glands (3). Although osseous
metastasis, including metastasis to the vertebral body, sternum,
ribs and long bones, is not uncommon and demonstrates an incidence
between 2 and 16% in HCC, metastasis to the cranium is rare, with
an incidence of 0.4–1.6% (4–6). Brain metastasis of HCC is also rare,
with a similar incidence of 0.65% recently reported (7).
The development of spontaneous AEDH from metastatic
HCC of the skull is extremely rare, and only 6 cases have been
previously reported in the literature (3–6,8,9). The
present study reports the case of a patient with spontaneous AEDH
that developed from a skull metastasis of HCC, and the clinical
presentation and pathogenesis are discussed with a review of the
literature. Written informed consent was obtained from the
patient's family.
Case report
In April 2008, a 41-year-old male was admitted to
Chonnam National University Hwasun Hospital and Medical School
(Hwasun, Jeollanam, South Korea) for the sudden onset of a
headache, associated with vomiting and followed by drowsiness
lasting several hours. On admission, no scalp wound or palpable
mass was detected. The patient demonstrated right-sided motor
weakness and a Glasgow Coma Scale (GCS) score (10) of 12/15 (eye opening, 3; verbal, 3;
motor, 6), with reactive pupils. Pathological reflex was not noted.
Based on these findings, a diagnosis of intracranial hemorrhage was
promptly proposed. The patient had been diagnosed with HCC
accompanied by jaundice and abdominal pain at the Samsung Medical
Center (Seoul, South Korea) 1 year prior (May 2007), based on the
results of abdominal magnetic resonance imaging and serological
findings. Over the year following diagnosis with HCC, the patient
received four sessions of transarterial chemoembolization for the
treatment of HCC at the Samsung Medical Center. The patient was
then transferred to Chonnam National University Hwasun Hospital and
Medical School for radiotherapy of multiple bone metastases,
involving multiple ribs and the pelvic bone, as detected by a
positron emission tomography-computed tomography (CT) scan
performed in February 2008. In April 2008, the platelet counts were
below normal limits (73×103/mm3; normal
range, 130–450×103/mm3), but blood
coagulation profiles, including prothrombin (13.5 sec; normal
range, 11.0–14.9 sec) and activated partial thromboplastine (30.2
sec; normal range, 26.5–41.0 sec) times, were within normal
limits.
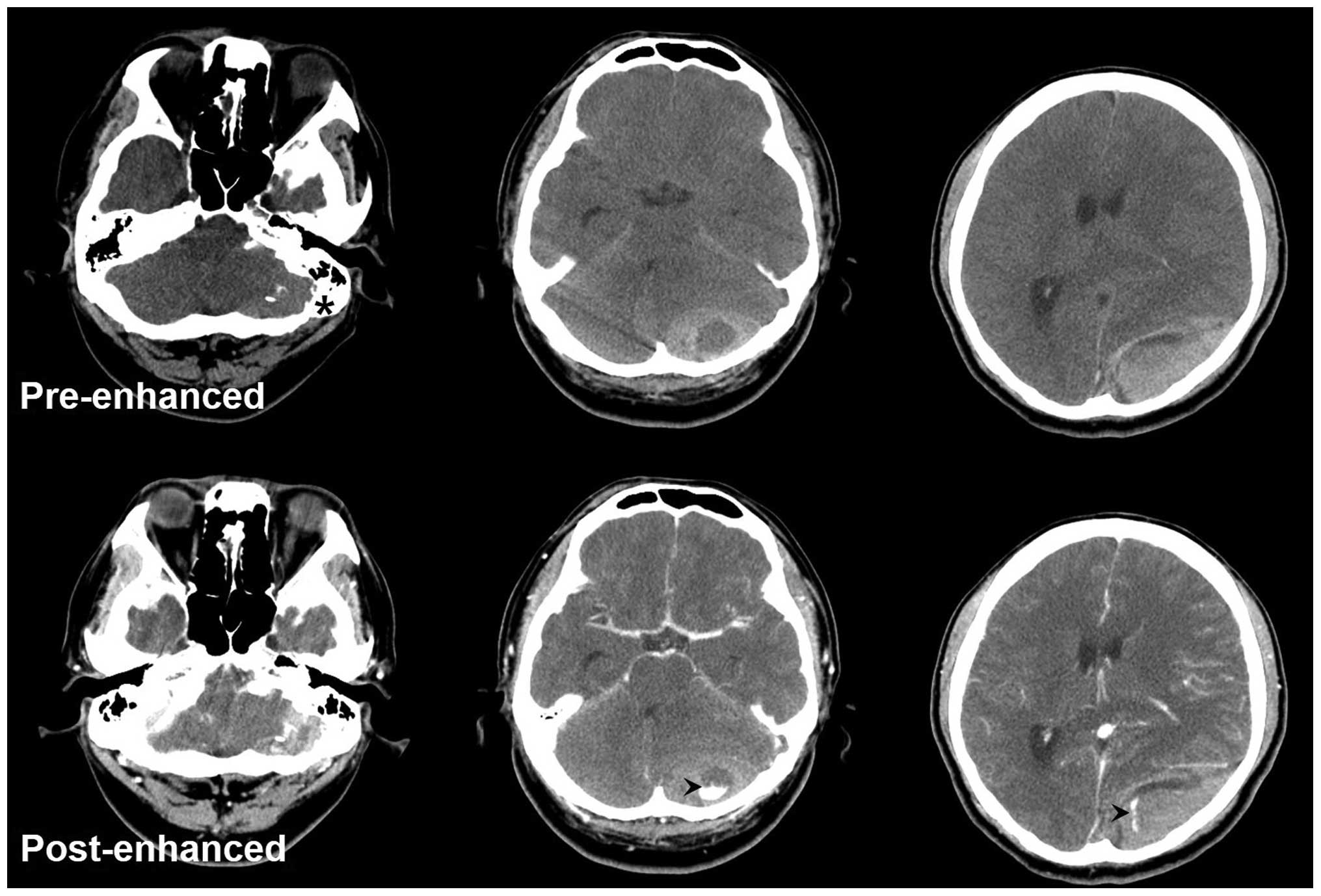
A head CT scan revealed a large AEDH located in the
left parieto-occipital area and posterior fossa, and a midline
shifting. The CT scan also revealed a heterogeneously enhanced mass
that was associated with a lytic cranial lesion in the left
occipital bone (Fig. 1). A left-sided
parieto-occipital craniotomy and evacuation of AEDH was performed.
No evidence of head trauma, including skull fractures or scalp
contusion, was detected. A mixed-stage (acute and subacute)
hematoma was located in the epidural space, with no gross invasion
of the dura. Additionally, a soft mass demonstrating osteolytic
change on the occipital bone was found. The soft mass demonstrated
continuity with the hematoma in the parieto-occipital region and
growth to the muscle close to the foramen magnum. The large
epidural hematoma was completely removed.
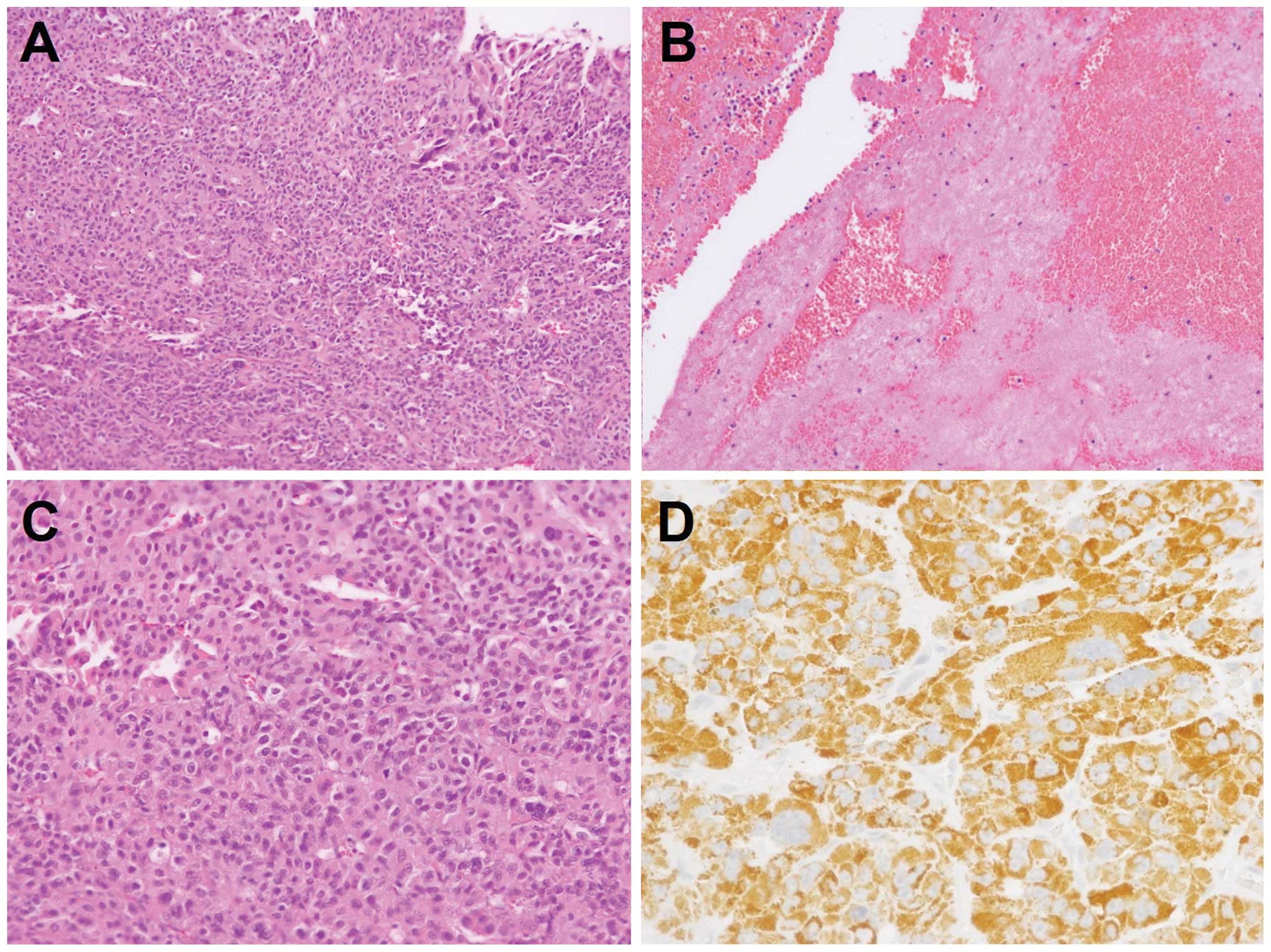
Histopathological examination of the lesion revealed
a highly cellular epithelial tumor intermingled with fresh blood
clots (Fig. 2A–B). The tumor cells
contained abundant eosinophilic cytoplasm and were arranged in a
compact trabecular pattern (Fig. 2C).
Immunohistochemical analysis using the monoclonal mouse anti-human
Hep Par 1 antibody (clone OCH1E5; cat. no. M7158; 1:100; Dako,
Glostrup, Denmark) revealed marked cytoplasmic expression of Hep
Par 1 (Fig. 2D). The
histopathological diagnosis was metastatic hepatocellular
carcinoma. Postoperatively, the patient experienced a sudden
deterioration of mental status due to the obstructive
hydrocephalus, which was resolved using extraventricular
ventricular drainage. The patient gradually recovered to normal
status 2 months subsequent to the surgery. However, the patient
succumbed to hepatic failure due to HCC progression 4 months
subsequent to the surgery.
Discussion
Metastatic intracranial tumors, including intraaxial
and extraxial lesions, are the most common type of brain tumor,
with an incidence of ≥40% (11).
Common primary neoplasms of metastatic intracranial tumors are lung
cancer, breast cancer, melanoma and colorectal cancer (12). Intracranial hemorrhage from brain
tumors is not common, and accounts for 0.9–11% of all spontaneous
intracranial hemorrhages. The majority of these intracranial
hemorrhages occur in an intratumoral or intracerebral location, and
therefore, occurrence in an epidural location is exceptional
(13).
The development of spontaneous AEDH has been
previously reported to have developed from several malignant
lesions involving the skull, including lung cancer, ovarian cancer,
esophageal cancer, Ewing's sarcoma and Langerhans cell histocytosis
lesions (11,14–17).
Spontaneous AEDH of skull metastases from HCC is a rare condition,
and only 6 cases have been previously reported in the literature
(Table I) (3–6,8,9). Based on
the review of the cases, the majority of AEDH patients experience a
severe headache followed by neurological deficits, including the
deterioration of consciousness or hemiparesis (3,4,6,8,9). Osteolytic changes are frequently
detected in the radiographic and intraoperative findings (4,5,8).
 | Table I.Previously published cases of
spontaneous acute epidural hematoma from skull metastasis of
hepatocellular carcinoma. |
Table I.
Previously published cases of
spontaneous acute epidural hematoma from skull metastasis of
hepatocellular carcinoma.
| First author, year
(ref) | Age, years | Gender | Osteolytic change on
CT scan | Clinical
manifestations | Coagulopathy | Postoperative
outcomes |
|---|
| Nakagawa et
al, 1992 (9) | 52 | M | No | Headache Mental
deterioration | Yes | Succumbed to liver
failure subsequent to 1 month |
| Hayashi et al,
2000 (3) | 70 | M | No | Headache Left
hemiparesis Palpable mass | Yes | Succumbed to
pneumonia subsequent to 2 months |
| McIver et al,
2001 (8) | 50 | M | Yes | Palpable mass Slurred
speech Right hemiparesis | Unknown | No neurological
deficits on most recent follow-up |
| Kanai et al,
2008 (4) | 56 | M | Yes | Palpable mass
Headache Mental deterioration | No | Succumbed to liver
failure subsequent to 3 weeks |
| Kim et al,
2010 (5) | 53 | M | Yes | Mental
deterioration | Yes | Succumbed to
multi-organ failure 5 days following surgery |
| Woo et al,
2010 (6) | 46 | M | No | Headache Mental
deterioration | Yes | Persistent vegetative
state |
| This case | 41 | M | Yes | Headache Vomiting
Mental deterioration | No | Succumbed to liver
failure subsequent to 4 months |
Skull metastasis of HCC is relatively rare, in
contrast to the incidence of skull metastasis in lung, breast,
thyroid and prostate cancers (18).
Based on the review of the literature, however, ~10% (7/68) of
patients with skull HCC metastasis presented with intracranial
hemorrhagic events (18). An
increased incidence of hemorrhagic events is also found in the
intracerebral metastasis of HCC. Recent data revealed that more
than one-half of brain metastases in HCC patients exhibited
intratumoral or extratumoral hemorrhagic change (7).
It is unclear why skull metastasis from HCC causes
epidural hematoma more frequently than other tumors. However,
several characteristics of HCC may contribute to intracranial
bleeding. First, HCC contains numerous sinusoid-like vessels, and
the fragility of these vessels may lead to hemorrhage and the
formation of the epidural hematoma (3–6,8,9). Second,
coagulopathy caused by hepatic dysfunction may increase the risk of
tumor bleeding (3,5,6,9). Third, the destructive growth of
metastatic HCC may lead to the breakdown of the vessel structures
in the peritumoral tissue, as demonstrated in osteolytic change
(5,6,8). Fourth,
injury of the main feeders from the external carotid artery or the
surrounding venous structures, induced by a trivial accident, may
be involved (5,6,8).
In conclusion, spontaneous AEDH from skull
metastasis is a rare event in HCC patients. Once a sudden and
unpredicted neurological deficit occurs in a HCC patient diagnosed
with skull metastasis, however, the possibility of spontaneous AEDH
developing from skull metastasis should be considered.
Glossary
Abbreviations
Abbreviations:
|
AEDH
|
acute epidural hematoma
|
|
CT
|
computed tomography
|
|
HCC
|
hepatocellular carcinoma
|
References
|
1
|
Zheng FX and Chao Y: Spontaneous
intracranial extradural hematoma: Case report and literature
review. Neurol India. 57:324–326. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
El-Serag HB: Hepatocellular carcinoma: An
epidemiologic view. J Clin Gastroenterol. 35(Suppl 2): S72–S78.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hayashi K, Matsuo T, Kurihara M, Daikoku
M, Kitange G and Shibata S: Skull metastasis of hepatocellular
carcinoma associated with acute epidural hematoma: A case report.
Surg Neurol. 53:379–382. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kanai R, Kubota H, Terada T, Hata T,
Tawaraya E and Fujii K: Spontaneous epidural hematoma due to skull
metastasis of hepatocellular carcinoma. J Clin Neurosci.
16:137–140. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kim BG, Yoon SM, Bae HG and Yun IG:
Spontaneous intracranial epidural hematoma originating from dural
metastasis of hepatocellular carcinoma. J Korean Neurosurg Soc.
48:166–169. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Woo KM, Kim BC, Cho KT and Kim EJ:
Spontaneous epidural hematoma from skull base metastasis of
hepatocellular carcinoma. J Korean Neurosurg Soc. 47:461–463. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Han MS, Moon KS, Lee KH, Cho SB, Lim SH,
Jang WY, Jung TY, Kim IY and Jung S: Brain metastasis from
hepatocellular carcinoma: The role of surgery as a prognostic
factor. BMC Cancer. 13:5672013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
McIver JI, Scheithauer BW, Rydberg CH and
Atkinson JL: Metastatic hepatocellular carcinoma presenting as
epidural hematoma: Case report. Neurosurgery. 49:447–449. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nakagawa Y, Yoshino E, Suzuki K, Tatebe A
and Andachi H: Spontaneous epidural hematoma from a hepatocellular
carcinoma metastasis to the skull - Case report. Neurol Med Chir
(Tokyo). 32:300–302. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Teasdale G and Jennett B: Assessment of
coma and impaired consciousness. A practical scale. Lancet.
2:81–84. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kumar PM and Manisha M: Epidural hematoma
secondary to solitary skull metastasis from an ovarian carcinoma.
Asian J Neurosurg. 9:112–114. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Johnson JD and Young B: Demographics of
brain metastasis. Neurosurg Clin N Am. 7:337–344. 1996.PubMed/NCBI
|
|
13
|
Wakai S, Yamakawa K, Manaka S and Takakura
K: Spontaneous intracranial hemorrhage caused by brain tumor: Its
incidence and clinical significance. Neurosurgery. 10:437–444.
1982. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen HC, Shen WC, Chou DY and Chiang IP:
Langerhans cell histiocytosis of the skull complicated with an
epidural hematoma. AJNR Am J Neuroradiol. 23:493–495.
2002.PubMed/NCBI
|
|
15
|
Ellis MJ and McDonald PJ: Acute epidural
hematoma secondary to skull metastasis from esophageal carcinoma.
Can J Neurol Sci. 34:491–493. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Simmons NE, Elias WJ, Henson SL and Laws
ER: Small cell lung carcinoma causing epidural hematoma: Case
report. Surg Neurol. 51:56–59. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yamashita Y, Kumabe T, Kobayashi T, Abiko
H, Seki H and Yoshimoto T: Ewing's sarcoma at the occipital bone
presenting as acute epidural hematoma: A case report. No Shinkei
Geka. 25:567–571. 1997.(In Japanese). PubMed/NCBI
|
|
18
|
Hsieh CT, Sun JM, Tsai WC, Tsai TH, Chiang
YH and Liu MY: Skull metastasis from hepatocellular carcinoma. Acta
Neurochir (Wien). 149:185–190. 2007. View Article : Google Scholar : PubMed/NCBI
|