Introduction
Esophageal carcinoma (EC) is one of the most common
malignancies in the world, while esophageal squamous cell carcinoma
(ESCC) is the main histopathological subtype of EC in Eastern Asian
countries, including China (1).
Although the therapeutic treatments for ESCC such as surgery,
chemotherapy, radiotherapy and target therapy, have improved in
recent years, the five-year survival rate for patients with
resectable disease is <40% (2,3). Thus, an
increasing interest exist on the prognostic and therapeutic value
of biological markers that participate in the carcinogenesis and
progression of ESCC.
Human epidermal growth factor receptor (EGFR) 2
(HER2), also known as Erb-B2 receptor tyrosine kinase 2 and
c-erbB2, is a member of the EGFR family, whose abnormal activation
appears to be involved in tumor development and progression in ESCC
(4,5).
In addition, HER2 is a therapeutic target in several types of
cancer. Previous studies have observed that the oncogene
HER2/neu was overexpressed in 2.0–19.1% cases of ESCC
(6–13), and increased protein expression levels
of HER2 have been previously observed in EC (14,15) and
ESCC (6,7). However, the role of HER2 in ESCC remains
controversial (6,7,9,10,12,16–19).
Multidrug resistance protein 1 (MRP1), as a member of the adenosine
triphosphate-binding cassette transporter family, has been
implicated in resistance to cancer therapeutics (20). High expression levels of MRP1 have
been observed in various solid tumors such as lung cancer, and the
expression levels of MRP1 have been reported to inversely correlate
with prognosis in patients with lung cancer (21–23). In
addition, patients with Barrett's carcinoma treated with
neoadjuvant chemotherapy who exhibited high messenger RNA
expression levels of MRP1 presented prolonged survival, compared
with those patients whose levels of MRP1 were low (24). However the role of MRP1 expression in
patients with ESCC remains unclear.
The aim of the present retrospective study was to
determine the clinical significance of HER2 and MRP1 expression in
a large-scale cohort study involving patients with ESCC who had
undergone surgical resection. For that purpose, the protein
expression levels of HER2 and MRP1 were detected by
immunohistochemistry (IHC), and the association between the
clinicopathological features of this disease and the prognostic
value of HER2 and MRP1 expression in patients with ESCC was
evaluated.
Materials and methods
Patients
Between June 2002 and June 2010, all the consecutive
cases of patients with clinical resectable ESCC who had been
treated at the Department of Medical Oncology of Zhejiang Cancer
Hospital (Hangzhou, China) were retrospectively reviewed. The
present study was approved by the institutional review board of
Zhejiang Cancer Hospital, and all the patients provided written
informed consent for participation in the study. All the patients
included in the study had been subjected to complete resection, and
none had received neoadjuvant treatment. Those patients who
succumbed to the disease within 30 days following surgery were
excluded from the study. Cancer stage was determined during the
postoperative pathological examination, and included the status of
primary tumor invasion, regional lymph nodes and distant
metastases, according to the 7th edition of the Cancer Staging
Manual published by the American Joint Committee on Cancer
(25). Long-term postoperative
follow-up consisted of a telephone interview conducted every three
months for the first three years, every six months during the
fourth and fifth year, and every year thereafter. The date of the
last follow-up was April 30, 2014. Overall survival (OS) was
defined from the time of diagnosis until the date of mortality or
until the date of the last follow-up visit. Progression-free
survival (PFS) was measured from the time of completion of the
surgery until the time of documented tumor recurrence or mortality.
The present study was conducted according to the REporting
recommendations for tumor MARKer prognostic studies guidelines
(26).
Immunohistochemistry
Immunohistochemical analyses were performed by the
avidin-biotin peroxidase method, using ultraView Universal DAB
Detection Kit (Ventana Medical Systems, Inc., Tucson, AZ, USA). For
this purpose, paraffin sections of 4 mm thickness were excised from
paraffin blocks, and subsequently immunostained with rabbit
monoclonal primary antibodies against HER2 (catalogue no. 4B5;
dilution, 1:100; Roche Diagnostics GmbH, Mannheim, Germany) and
MRP1 (catalogue no. H-70; dilution, 1:100; Santa Cruz
Biotechnology, Inc., Dallas, TX, USA). The primary antibodies were
detected with an automated staining system (BenchMark XT; Roche
Diagnostics GmbH).
Next, the slides were washed with phosphate-buffered
saline (PBS) three times, and incubated with the secondary antibody
provided in the ultraView DAB Detection Kit (Fuzhou Maixin Biotech.
Co., Ltd, Fujian, China). The colorimetric reaction was developed
with 3,3′-diaminobenzidine. Counterstaining was performed with
hematoxylin. All steps were conducted at room temperature. For the
negative control, the primary antibody was replaced with PBS.
The immunostaining results were independently
examined by two clinical pathologists who were blinded to the
patients' information, using a DM4000B light microscope (Leica,
Wetzlar, Germany). For each sample, five high-power fields
(magnification, ×400) were randomly selected. The percentage of
positive cells and the intensity of the staining were assessed, and
a semi-quantitatively score ranging from 0 to 3 was assigned to the
samples accordingly. The staining intensity was scored as follows:
i) 0, no staining; ii) 1, weak staining; iii) 2, moderate staining;
and iv) 3, strong staining. This score was then multiplied by the
percentage of positively stained cells present in the sample, as
follows: i) 0, no staining; ii) 1, ≤10% of stained cells; iii) 2,
11–25% of stained cells; iv) 3, 26–50% of stained cells; and v) 4,
≥51% of stained cells. The resulting scores were used to classify
the samples as follows: i) 0, negative staining; ii) 1–4, weak
positive staining; iii) 5–8, moderate staining; and iv) 9–12,
strong positive staining.
Statistical analysis
The correlation between the expression levels of
HER2 and MRP1 and the patient's clinicopathological factors was
analyzed using Fisher's exact test or χ2 test.
Univariate and multivariate analyses were performed with
Kaplan-Meier survival curves and Cox proportional hazard model,
respectively. Log-rank test was used to evaluate the significance
of the differences observed between pairs of survival
probabilities. P<0.050 was considered to indicate a
statistically significant difference. Statistical data were
calculated with SPSS version 18.0 software (SPSS Inc., Chicago, IL,
USA).
Results
Patient's characteristics
The cohort of 829 patients with ESCC whose
expression levels of MRP1 were analyzed in the present study
exhibited a female:male ratio of 1.0:4.5 and a median age of 59
years (range, 34–78 years). Among the 829 patients, 768 patients
also detected HER-2 expression. ESCC was observed to be well
differentiated in 110 cases (13.3%), moderately differentiated in
561 cases (67.7%), poorly differentiated in 153 cases (18.4%) and
undifferentiated in 5 cases (0.6%). The enrolled patients were
staged pathologically as I (n=61), II (n=335) and III (n=433).
Complete resection was confirmed histologically in all patients.
Locoregional lymph node metastasis was observed in 477 patients
(57.5%). A total of 260 patients who presented poor prognostic
factors, metastatic disease or recurrence following operation,
received adjuvant radiotherapy and/or chemotherapy subsequently to
surgery. A total of 762 patients were available for survival
analysis, with a median duration of postoperative follow-up of 32
months (range, 1.03–102.00 months). Among them, 733 patients were
followed-up for >3 years. The clinicopathological factors,
staging and survival of the patients included in the present study
have been previously reported (27,28).
Association between HER2 and MRP1
expression and clinicopathological features
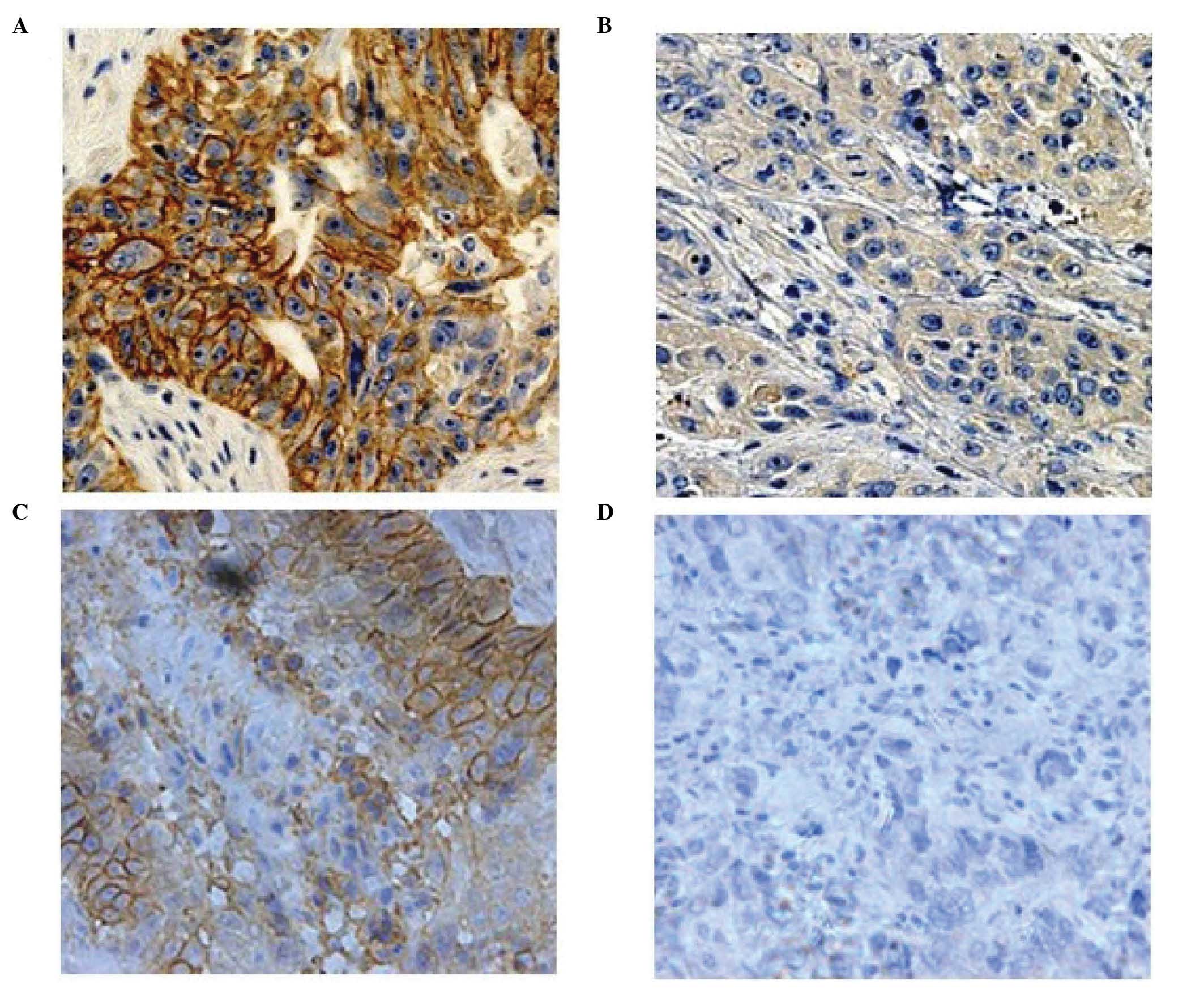
In ESCC tissues, HER2 exhibited membrane staining,
while MRP1 displayed membrane and cytoplasmic staining (Fig. 1). A total of 768 patients were
available for evaluation of HER2 expression. Among them, 543 cases
(70.7%) were observed to be negative, 170 cases (22.1%) were scored
as 1, 37 cases (4.8%) as 2 and 18 cases (2.3%) as 3. For
statistical analysis, samples with a final score of 0 were
considered to exhibit low expression levels of HER2, whereas those
with a final score of 1–3 were considered to display high
expression levels of HER2. Among the 829 cases who were assessed
for MRP1 expression by IHC, 326 (39.3%), 291 (35.1%), 144 (17.4%)
and 68 (8.2%) cases were scored as 0, 1, 2 and 3, respectively. For
statistical analysis, samples with a final score of 0 or 1 were
considered to exhibit low expression levels of MRP1, while those
with a final score of 2 or 3 were considered to display high
expression levels of MRP1.
The associations between the expression levels of
HER2 and MRP1 and the clinicopathological features of the patients
are presented in Table I. A
significant correlation was observed between the expression levels
of HER2 and gender (P<0.050), tumor size (P=0.013) and
venous/lymphatic invasion (P=0.039). However, no significant
correlation was identified between MRP1 expression and any of the
clinicopathological factors analyzed. Furthermore, high expression
levels of HER2 were positively correlated with high expression
levels of MRP1 (P=0.001).
 | Table I.Analysis of the association between
the expression levels of HER2 and MRP1 and the clinicopathological
features of patients with esophageal squamous cell carcinoma. |
Table I.
Analysis of the association between
the expression levels of HER2 and MRP1 and the clinicopathological
features of patients with esophageal squamous cell carcinoma.
|
| HER2 expression
levels (no. of patients) | MRP1 expression
levels (no. of patients) |
|---|
|
|
|
|
|---|
| Characteristics | Total | Low | High | P-value | Total | Low | High | P-value |
|---|
| Gender |
|
|
| 0.000 |
|
|
| 0.516 |
| Male | 627 | 466 | 161 |
| 678 | 499 | 179 |
|
|
Female | 141 | 77 | 64 |
| 151 | 115 | 36 |
|
| Age (years) |
|
|
| 0.760 |
|
|
| 0.702 |
| ≥55 | 491 | 349 | 142 |
| 527 | 388 | 139 |
|
|
<55 | 277 | 194 | 83 |
| 302 | 226 | 76 |
|
| Smoking |
|
|
| 0.163 |
|
|
| 0.532 |
|
Never | 179 | 134 | 45 |
| 202 | 153 | 49 |
|
|
Ever | 589 | 409 | 180 |
| 627 | 461 | 166 |
|
| Alcohol
consumption |
|
|
| 0.178 |
|
|
| 0.755 |
|
Never | 256 | 189 | 67 |
| 282 | 207 | 75 |
|
|
Ever | 512 | 354 | 158 |
| 547 | 407 | 140 |
|
|
Differentiation |
|
|
| 0.216 |
|
|
| 0.055 |
|
Intermediate/well | 622 | 447 | 175 |
| 671 | 507 | 164 |
|
|
Poor/undifferentiated | 144 | 96 | 48 |
| 158 | 107 | 51 |
|
| Tumor size
(cm) |
|
|
| 0.013 |
|
|
| 0.671 |
|
<5 | 442 | 297 | 145 |
| 464 | 341 | 123 |
|
| ≥5 | 326 | 246 | 80 |
| 365 | 273 | 92 |
|
| Depth of
invasion |
|
|
| 0.678 |
|
|
| 0.362 |
|
T1+T2 | 160 | 111 | 49 |
| 171 | 122 | 49 |
|
| T3 | 608 | 432 | 176 |
| 658 | 492 | 166 |
|
| Lymph node
metastasis |
|
|
| 0.347 |
|
|
| 0.126 |
| N0 | 321 | 232 | 89 |
| 352 | 273 | 79 |
|
| N1 | 214 | 148 | 66 |
| 232 | 162 | 70 |
|
| N2 | 159 | 106 | 53 |
| 169 | 120 | 49 |
|
| N3 | 74 | 57 | 17 |
| 76 | 59 | 17 |
|
| Clinical stage |
|
|
| 0.647 |
|
|
| 0.456 |
|
I+II | 358 | 256 | 102 |
| 396 | 298 | 98 |
|
|
III | 410 | 287 | 123 |
| 433 | 316 | 117 |
|
| Venous/lymphatic
invasion |
|
|
| 0.039 |
|
|
| 0.094 |
| No | 622 | 450 | 172 |
| 672 | 506 | 166 |
|
|
Yes | 146 | 93 | 53 |
| 157 | 108 | 49 |
|
| Perineural
invasion |
|
|
| 0.050 |
|
|
| 0.219 |
| No | 588 | 426 | 162 |
| 638 | 466 | 172 |
|
|
Yes | 180 | 117 | 63 |
| 191 | 148 | 43 |
|
| Adjuvant
radio/chemotherapy |
|
|
| 0.269 |
|
|
| 0.196 |
| No | 517 | 359 | 158 |
| 569 | 429 | 140 |
|
|
Yes | 251 | 184 | 67 |
| 260 | 185 | 75 |
|
Survival analysis
During the follow-up, 397 patients succumbed to
ESCC, while recurrence or metastasis occurred in 470 patients. The
metastatic areas included the supraclavicular lymph node,
mediastinal lymph node, liver, lung, skeleton and brain.
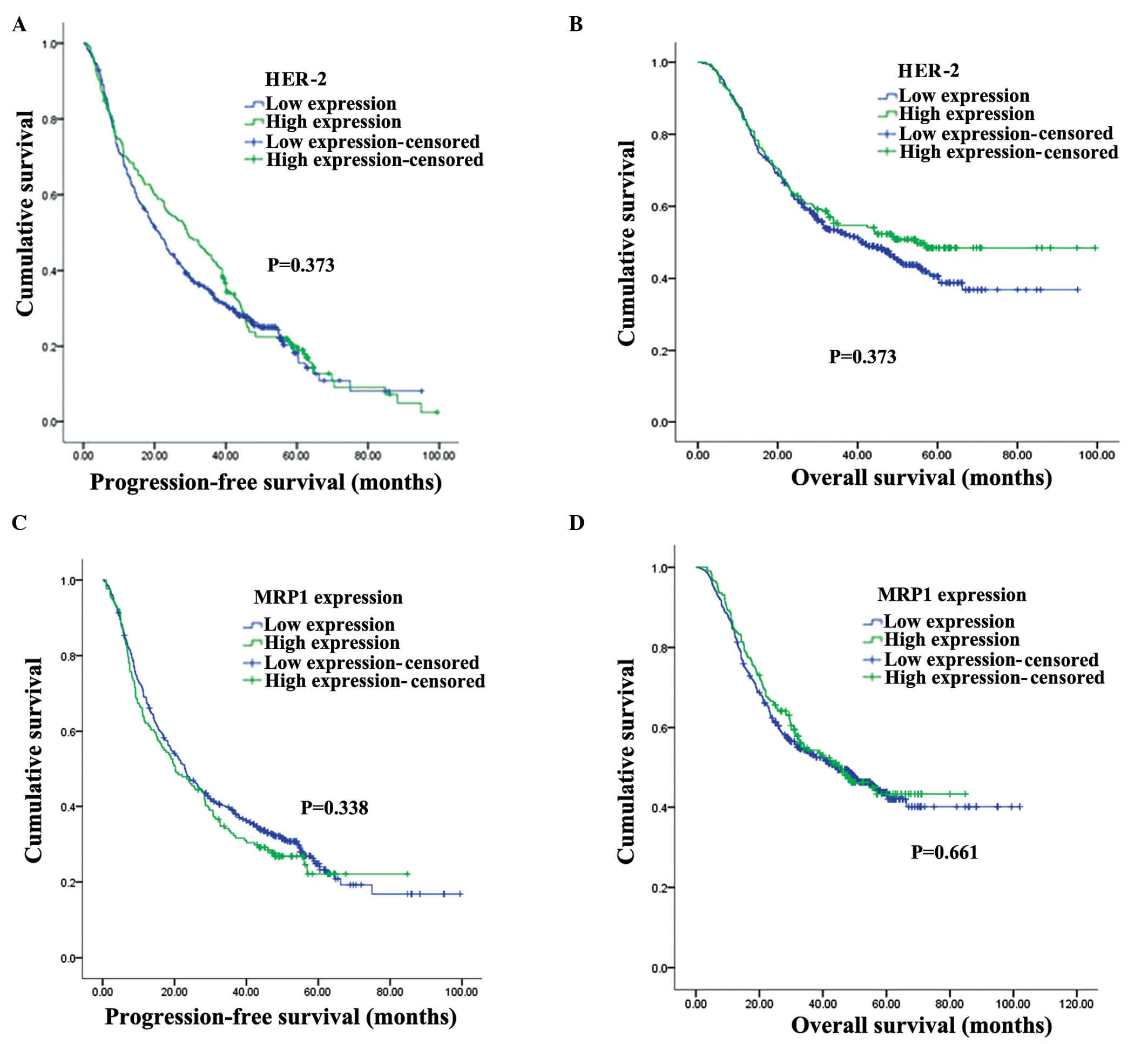
In univariate analysis, gender, differentiation,
depth of invasion, clinical stage, adjuvant radiotherapy or
chemotherapy and lymph node metastasis were significantly
correlated with the patients' PFS and OS (P<0.050) (Table II). However, the graphic pattern of
the Kaplan-Meier estimate curves (Fig.
2) suggested that the expression levels of HER2 or MRP1 did not
have any impact on prognosis (log-rank, P>0.050). In
multivariate analysis, tumor location, clinical stage and lymph
node metastasis were identified as independent factors of prognosis
in patients with ESCC (Table III).
However, the expression levels of HER2 or MRP1 were not observed to
be independently associated with PFS and OS in these patients
(Table III).
 | Table II.Univariate analysis of factors that
influence the survival of patients with esophageal squamous cell
carcinoma. |
Table II.
Univariate analysis of factors that
influence the survival of patients with esophageal squamous cell
carcinoma.
|
| Progression-free
survival | Overall
survival |
|---|
|
|
|
|
|---|
| Factors | No. of
patients | P-value | No. of
patients | P-value |
|---|
| Gender |
| 0.009 |
| 0.018 |
|
Male | 554 |
| 645 |
|
|
Female | 108 |
| 129 |
|
| Age (years) |
| 0.339 |
| 0.843 |
|
≥55 | 416 |
| 491 |
|
|
<55 | 246 |
| 283 |
|
| Smoking |
| 0.315 |
| 0.177 |
|
Never | 156 |
| 186 |
|
|
Ever | 506 |
| 588 |
|
| Alcohol
consumption |
| 0.869 |
| 0.199 |
|
Never | 218 |
| 266 |
|
|
Ever | 444 |
| 508 |
|
| Location |
| 0.400 |
| 0.149 |
|
Upper/middle | 274 |
| 338 |
|
|
Lower | 388 |
| 436 |
|
|
Differentiation |
| 0.000 |
| 0.000 |
|
Intermediate/well | 528 |
| 618 |
|
|
Poor/undifferentiated | 134 |
| 155 |
|
| Tumor size
(cm) |
| 0.164 |
| 0.023 |
|
<5 | 369 |
| 444 |
|
| ≥5 | 293 |
| 330 |
|
| Depth of
invasion |
| 0.000 |
| 0.000 |
|
T1+T2 | 131 |
| 168 |
|
| T3 | 531 |
| 606 |
|
| Lymph node
metastasis |
| 0.000 |
| 0.000 |
| N0 | 261 |
| 331 |
|
| N1 | 178 |
| 212 |
|
| N2 | 152 |
| 160 |
|
| N3 | 71 |
| 71 |
|
| Clinical stage |
| 0.000 |
| 0.000 |
|
I+II | 297 |
| 374 |
|
|
III | 365 |
| 400 |
|
| Venous/lymphatic
invasion |
| 0.473 |
| 0.373 |
| No | 531 |
| 629 |
|
|
Yes | 131 |
| 145 |
|
| Perineural
invasion |
| 0.203 |
| 0.919 |
| No | 531 |
| 604 |
|
|
Yes | 131 |
| 170 |
|
| Adjuvant
radio/chemotherapy |
| 0.049 |
| 0.002 |
| No | 425 |
| 524 |
|
|
Yes | 237 |
| 250 |
|
| Human epidermal
growth factor receptor 2 |
| 0.373 |
| 0.196 |
| Low
expression levels | 432 |
| 515 |
|
| High
expression levels | 178 |
| 194 |
|
| Multidrug
resistance protein 1 |
| 0.338 |
| 0.661 |
| Low
expression levels | 423 |
| 496 |
|
| High
expression levels | 239 |
| 278 |
|
 | Table III.Multivariate analysis of
progression-free survival and overall survival in patients with
esophageal squamous cell carcinoma. |
Table III.
Multivariate analysis of
progression-free survival and overall survival in patients with
esophageal squamous cell carcinoma.
|
| Progression-free
survival | Overall
survival |
|---|
|
|
|
|
|---|
| Factors | Hazard ratio | 95% CI | P-value | Hazard ratio | 95% CI | P-value |
|---|
| Gender |
|
| 0.021 |
|
| 0.051 |
|
Male | Ref. |
|
| Ref. |
|
|
|
Female | 0.732 | 0.563–0.954 |
| 0.756 | 0.567–1.008 |
|
| Tumor location |
|
| 0.027 |
|
| NR |
|
Upper/middle | Ref. |
|
| NR |
|
|
|
Lower | 1.235 | 1.024–1.489 |
| NR | NR |
|
| Clinical stage |
|
| 0.020 |
|
| 0.014 |
|
I+II | Ref. |
|
| Ref. |
|
|
|
III | 1.507 | 1.069–2.129 |
| 1.640 | 1.104–2.435 |
|
| Lymph node
metastasis |
|
| 0.000 |
|
| 0.000 |
| N0 | Ref. |
|
| Ref. |
|
|
| N1 | 1.170 | 0.826–1.656 |
| 1.342 | 0.893–2.015 |
|
| N2 | 1.516 | 1.021–2.251 |
| 2.181 | 1.395–3.409 |
|
| N3 | 2.260 | 1.463–3.491 |
| 1.640 | 1.104–2.435 |
|
|
Differentiation |
|
| 0.061 |
|
| 0.085 |
|
Intermediate/well | Ref. |
|
| Ref. |
|
|
|
Poor/undifferentiated | 1.240 | 0.999–1.553 |
| 1.233 | 0.972–1.564 |
|
Discussion
HER2 is a therapeutic target in several tumors such
as breast cancer (29–32), and a predictive factor of response to
chemotherapy in various solid malignancies (33–36). In
order to identify improved prognostic indicators for ESCC, the
clinicopathological features of patients with ESCC were
investigated in the present study. In previous studies, the number
of copies of the HER2/neu gene was analyzed by
fluorescence or chromogenic in situ hybridization, and the
protein expression levels of HER2 were evaluated by IHC (6,7,9,10,12,16–19).
Previous studies examining the association between the expression
levels of HER2 (as determined by IHC) and prognosis in patients
with ESCC have reported conflicting results (Table IV). These discrepancies may be due to
the following reasons: i) Different quality of the studies; ii)
multiple factors that may influence prognosis were not considered
in all the studies; iii) different laboratory techniques were
employed in different studies, including the use of different
antibodies to detect HER2 and MRP1; and iv) small size of the
samples used in the studies (≤250 patients; Table IV). The association between HER2
expression and prognosis in EC has not been reported thus far.
 | Table IV.Previous studies describing the
prognostic significance of the expression levels of human epidermal
growth factor receptor 2 in ESCC, as determined by IHC or ISH. |
Table IV.
Previous studies describing the
prognostic significance of the expression levels of human epidermal
growth factor receptor 2 in ESCC, as determined by IHC or ISH.
| First author, year
(reference) | Type of cancer | Prognostic
effect | Sample size (no. of
patients) | Method |
|---|
| Hardwick, 1997
(19) | ESCC, AC | No effect | 205 | IHC |
| Friess, 1999
(12) | ESCC, AC | No effect | 39 | IHC |
| Mimura, 2005
(9) | ESCC | Unfavorable | 66 | IHC, ISH |
| Reichelt, 2007
(10) | ESCC, AC | No effect | 251 | IHC, ISH |
| Sato-Kuwabara, 2009
(6) | ESCC | Unfavorable | 188 | IHC, ISH |
| Stoecklein, 2008
(37) | ESCC, AC | No effect | 101 | ISH |
| Schoppmann, 2010
(11) | ESCC, AC | No effect | 341 | IHC, ISH |
| Birner, 2011
(38) | ESCC, AC | Unfavorable | 330 | IHC, ISH |
| Zhan, 2012
(7) | ESCC | Unfavorable | 145 | IHC, ISH |
| Kato, 2013
(16) | ESCC | No effect | 245 | IHC, ISH |
| Wang, 2013
(39) | ESCC | Unfavorable | 72 | IHC |
| Wang, 1999
(18) | ESCC | No effect | 117 | IHC |
In the present study, a large cohort of 829 patients
with ESCC and long follow-up was analyzed, and no correlation was
observed between the expression levels of HER2 or MRP1 and the
postoperative survival time exhibited by these patients. To the
best of our knowledge, the present study is the first large-scale
study conducted to evaluate the prognostic role of MRP1 expression
in patients with ESCC who had been treated with primary surgery. In
the present study, a significant association was observed between
survival and clinical stage, lymph node metastasis and poor
differentiation in patients with ESCC. However, the present study
is affected by certain limitations, including its retrospective and
single-hospital nature. Thus, multicenter and prospective studies
are required to further validate the results of the present study.
In addition, the protein expression levels of HER2 and MRP1 were
solely examined by IHC in the present study, which may not be
completely consistent with their gene expression levels.
In summary, the results of the present study
indicated that the expression levels of MRP1 and HER2, as
determined by IHC analysis, were not associated with survival rate
in patients with ESCC. This result indicates that HER2 or MRP1
expression may not serve as informative prognostic biomarkers.
Therefore, further studies are required to clarify the mechanism
behind the expression of MRP1 and HER2 in patients with ESCC.
Acknowledgements
The present study was supported by the Province
Important Technology and Science Program (Special Feature of Major
Province Scientific and Technological Program 2011, grant no.
2011C13039-1), and the National Natural Science Foundation of China
(Beijing, China) (General Program; grant nos. 81172081 and
81372210).
References
|
1
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2013. CA Cancer J Clin. 63:11–30. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cunningham D, Allum WH, Stenning SP,
Thompson JN, Van de Velde CJ, Nicolson M, Scarffe JH, Lofts FJ,
Falk SJ, Iveson TJ, et al: MAGIC Trial Participants: Perioperative
chemotherapy versus surgery alone for resectable gastroesophageal
cancer. N Engl J Med. 355:11–20. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Omloo JM, Lagarde SM, Hulscher JB, Reitsma
JB, Fockens P, van Dekken H, Ten Kate FJ, Obertop H, Tilanus HW and
van Lanschot JJ: Extended transthoracic resection compared with
limited transhiatal resection for adenocarcinoma of the mid/distal
esophagus: Five-year survival of a randomized clinical trial. Ann
Surg. 246:992–1001. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Andl CD, Mizushima T, Nakagawa H, Oyama K,
Harada H, Chruma K, Herlyn M and Rustgi AK: Epidermal growth factor
receptor mediates increased cell proliferation, migration, and
aggregation in esophageal keratinocytes in vitro and in vivo. J
Biol Chem. 278:1824–1830. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rowinsky EK: Signal events: Cell signal
transduction and its inhibition in cancer. Oncologist. 8(Suppl 3):
5–17. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sato-Kuwabara Y, Neves JI, Fregnani JH,
Sallum RA and Soares FA: Evaluation of gene amplification and
protein expression of HER2/neu in esophageal squamous cell
carcinoma using Fluorescence in situ Hybridization (FISH) and
immunohistochemistry. BMC Cancer. 9:62009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhan N, Dong WG, Tang YF, Wang ZS and
Xiong CL: Analysis of HER2 gene amplification and protein
expression in esophageal squamous cell carcinoma. Med Oncol.
29:933–940. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chan DS, Twine CP and Lewis WG: Systematic
review and meta-analysis of the influence of HER2 expression and
amplification in operable oesophageal cancer. J Gastrointest Surg.
16:1821–1829. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mimura K, Kono K, Hanawa M, Mitsui F,
Sugai H, Miyagawa N, Ooi A and Fujii H: Frequencies of HER2/neu
expression and gene amplification in patients with oesophageal
squamous cell carcinoma. Br J Cancer. 92:1253–1260. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Reichelt U, Duesedau P, Tsourlakis MCh,
Quaas A, Link BC, Schurr PG, Kaifi JT, Gros SJ, Yekebas EF, Marx A,
et al: Frequent homogeneous HER2 amplification in primary and
metastatic adenocarcinoma of the esophagus. Mod Pathol. 20:120–129.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Schoppmann SF, Jesch B, Friedrich J, Wrba
F, Schultheis A, Pluschnig U, Maresch J, Zacherl J, Hejna M and
Birner P: Expression of HER2 in carcinomas of the esophagus. Am J
Surg Pathol. 34:1868–1873. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Friess H, Fukuda A, Tang WH, Eichenberger
A, Furlan N, Zimmermann A, Korc M and Büchler MW: Concomitant
analysis of the epidermal growth factor receptor family in
esophageal cancer: Overexpression of epidermal growth factor
receptor mRNA but not of c-erbB-2 and c-erbB-3. World J Surg.
23:1010–1018. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Suzuki H, Abo S, Kitamura M, Hashimoto M,
Izumi K, Terada K and Sugiyama T: Gene amplification of int-2 and
erbB in human esophageal cancer: Relationship to
clinicopathological variables. Cancer Invest. 15:411–415. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nakamura T, Nekarda H, Hoelscher AH,
Bollschweiler E, Harbeck N, Becker K, Siewert JR and Harbec N:
Prognostic value of DNA ploidy and c-erbB-2 oncoprotein
overexpression in adenocarcinoma of Barrett's esophagus. Cancer.
73:1785–1794. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Polkowski W, van Sandick JW, Offerhaus GJ,
ten Kate FJ, Mulder J, Obertop H and van Lanschot JJ: Prognostic
value of Laurén classification and c-erbB-2 oncogene overexpression
in adenocarcinoma of the esophagus and gastroesophageal junction.
Ann Surg Oncol. 6:290–297. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kato H, Arao T, Matsumoto K, Fujita Y, et
al: Gene amplification of EGFR, HER2, FGFR2 and MET in esophageal
squamous cell carcinoma. Int J Oncol. 42:1151–1158. 2013.PubMed/NCBI
|
|
17
|
Thompson SK, Sullivan TR, Davies R and
Ruszkiewicz AR: HER2/neu gene amplification in esophageal
adenocarcinoma and its influence on survival. Ann Surg Oncol.
18:2010–2017. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang LS, Chow KC, Chi KH, Liu CC, Li WY,
Chiu JH and Huang MH: Prognosis of esophageal squamous cell
carcinoma: Analysis of clinicopathological and biological factors.
Am J Gastroenterol. 94:1933–1940. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hardwick RH, Barham CP, Ozua P, Newcomb
PV, Savage P, Powell R, Rahamin J and Alderson D:
Immunohistochemical detection of p53 and c-erbB-2 in oesophageal
carcinoma; no correlation with prognosis. Eur J Surg Oncol.
23:30–35. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Leonard GD, Fojo T and Bates SE: The role
of ABC transporters in clinical practice. Oncologist. 8:411–424.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Galimberti S, Marchetti A, Buttitta F,
Carnicelli V, Pellegrini S, Bevilacqua G and Petrini M: Multidrug
resistance related genes and p53 expression in human non small cell
lung cancer. Anticancer Res. 18:2973–2976. 1998.PubMed/NCBI
|
|
22
|
Yokoyama H, Ishida T, Sugio K, Inoue T and
Sugimachi K: Immunohistochemical evidence that P-glycoprotein in
non-small cell lung cancers is associated with shorter survival.
Surg Today. 29:1141–1147. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Tews DS, Nissen A, Külgen C and Gaumann
AK: Drug resistance-associated factors in primary and secondary
glioblastomas and their precursor tumors. J Neurooncol. 50:227–237.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Langer R, Specht K, Becker K, Ewald P,
Bekesch M, Sarbia M, Busch R, Feith M, Stein HJ, Siewert JR and
Höfler H: Association of pretherapeutic expression of
chemotherapy-related genes with response to neoadjuvant
chemotherapy in Barrett carcinoma. Clin Cancer Res. 11:7462–7469.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sobin LH, Gospodarowicz MK and Wittekind
C: Title section/chapter. TNM Classification of Malignant Tumours
(7th). (Hoboken, NJ). Wiley-Blackwell. 4552009.
|
|
26
|
McShane LM, Altman DG, Sauerbrei W, Taube
SE, Gion M and Clark GM: Statistics Subcommittee of the NCI-EORTC
Working Group on Cancer Diagnostics: REporting recommendations for
tumour MARKer prognostic studies (REMARK). Br J Cancer. 93:387–391.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Xu XL, Zheng WH, Fu ZX, Li ZP, Xie HX, Li
XX, Jiang LH, Wang Y, Zhu SM and Mao WM: Topo2A as a prognostic
biomarker for patients with resectable esophageal squamous cell
carcinomas. Med Oncol. 32:3962015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Xu XL, Zheng WH, Tao KY, Li XX, Xu WZ,
Wang Y, Zhu SM and Mao WM: p53 is an independent prognostic factor
in operable esophageal squamous cell carcinoma: A large-scale study
with a long follow-up. Med Oncol. 31:2572014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Konecny G, Pauletti G, Pegram M, Untch M,
Dandekar S, Aguilar Z, Wilson C, Rong HM, Bauerfeind I, Felber M,
et al: Quantitative association between HER2/neu and steroid
hormone receptors in hormone receptor-positive primary breast
cancer. J Natl Cancer Inst. 95:142–153. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Owens MA, Horten BC and Da Silva MM: HER2
amplification ratios by fluorescence in situ hybridization and
correlation with immunohistochemistry in a cohort of 6,556 breast
cancer tissues. Clin Breast Cancer. 5:63–69. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Parums DV: Current status of targeted
therapy in non-small cell lung cancer. Drugs Today (Barc).
50:503–525. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Pollock NI and Grandis JR: HER2 as a
therapeutic target in head and neck squamous cell carcinoma. Clin
Cancer Res. 21:526–533. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kontopodis E, Kentepozidis N,
Christophyllakis CH, Boukovinas I, Kalykaki A, Kalbakis K, Vamvakas
L, Agelaki S, Kotsakis A, Vardakis N, et al: Docetaxel, gemcitabine
and bevacizumab as salvage chemotherapy for HER2-negative
metastatic breast cancer. Cancer Chemother Pharmacol. 75:153–160.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lee HJ, Seo AN, Kim EJ, Jang MH, Suh KJ,
Ryu HS, Kim YJ, Kim JH, Im SA, Gong G, et al: HER2 heterogeneity
affects trastuzumab responses and survival in patients with
HER2-positive metastatic breast cancer. Am J Clin Pathol.
142:755–766. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Partridge AH, Rumble RB, Carey LA, Come
SE, Davidson NE, Di Leo A, Gralow J, Hortobagyi GN, Moy B, Yee D,
et al: Chemotherapy and targeted therapy for women with human
epidermal growth factor receptor 2-negative (or unknown) advanced
breast cancer: American Society of Clinical Oncology Clinical
Practice Guideline. J Clin Oncol. 32:3307–3329. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Raben D, Helfrich B, Chan DC, Ciardiello
F, Zhao L, Franklin W, Barón AE, Zeng C, Johnson TK and Bunn PA Jr:
The effects of cetuximab alone and in combination with radiation
and/or chemotherapy in lung cancer. Clin Cancer Res. 11:795–805.
2005.PubMed/NCBI
|
|
37
|
Stoecklein NH, Hosch SB, Bezler M, Stern
F, Hartmann CH, Vay C, Siegmund A, Scheunemann P, Schurr P, Knoefel
WT, et al: Direct genetic analysis of single disseminated cancer
cells for prediction of outcome and therapy selection in esophageal
cancer. Cancer Cell. 13:441–453. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Birner P, Jesch B, Friedrich J, Riegler M,
Zacherl J, Hejna M, Wrba F, Schultheis A and Schoppmann SF:
Carbonic anhydrase IX overexpression is associated with diminished
prognosis in esophageal cancer and correlates with HER2 expression.
Ann Surg Oncol. 18:3330–3337. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wang G, Zhang W, Jiang W and Luan L:
Overexpression of HER2 associated with the progression of
esophageal cancer patients. Hepatogastroenterology. 60:1972–1978.
2013.PubMed/NCBI
|