Introduction
Spontaneous pneumothorax in patients with
osteosarcoma is a well-known phenomenon. It occurs as a
complication of pulmonary metastases of osteosarcoma or during
chemotherapy. Pneumothorax is a clinical emergency (1,2). The
incidence rate of the pneumothorax in osteosarcoma patients is
extremely low; spontaneous pneumothorax occurs in <2% of
patients with pulmonary metastases (3). Pneumothorax affects respiratory function
and endangers patient life by interfering with the treatment of
osteosarcoma. Subsequently, pneumothorax significantly decreases
quality of life and increases the risk of mortality in osteosarcoma
patients (4). It reported that
<10% of sarcoma patients with spontaneous pneumothorax survive
for >2 years following the initial diagnosis of pneumothorax
(5). Surgical resection is considered
the best treatment for this complication (3). Here, we present a case of bilateral
spontaneous pneumothorax with pulmonary metastases. We observed
that pneumothorax developed after the formation of bullae through
chest computed tomography (CT). In addition, all of these events
occurred after the patient had received chemotherapy. Written
informed consent was obtained from the patient's family.
Case report
A 40-year-old female presented with right lower lip
numbness in 2007 and a mass was identified on the right mandibular
area in April 2008. CT revealed right mandibular body bone
destruction and a soft tissue mass. Following resection of the
right mandible, osteosarcoma was revealed by biopsy. The right
mandible osteosarcoma relapsed in February 2009. Following surgery,
the patient was treated with four cycles of dacarbazine +
ifosfamide + epirubicin. However, the osteosarcoma relapsed once
more in June 2013. In September of the same year bilateral
pulmonary metastases was confirmed by CT. The patient was then
treated with one cycle of adriamycin (ADM) and cisplatin (DDP).
Chest CT revealed left liquid pneumothorax on 12 December 2013.
Following tube drainage therapy, the left liquid pneumothorax was
cured and another cycle of ADM + DDP was administered. The patient
suffered from severe anemia and thus, chemotherapy could not be
applied regularly (every 3 weeks). Notably, the occurrence of
pneumothorax was observed during the long intervals between
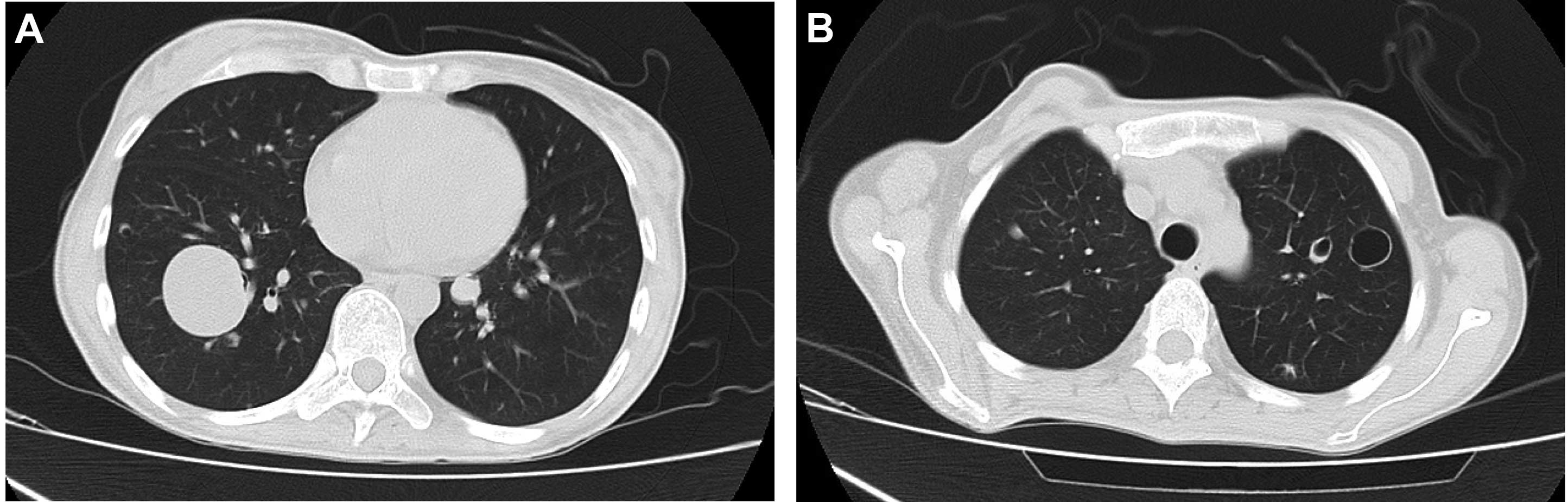
chemotherapy treatments. We compared the chest CT results taken on
27 May 2014 (Fig. 1) with those taken
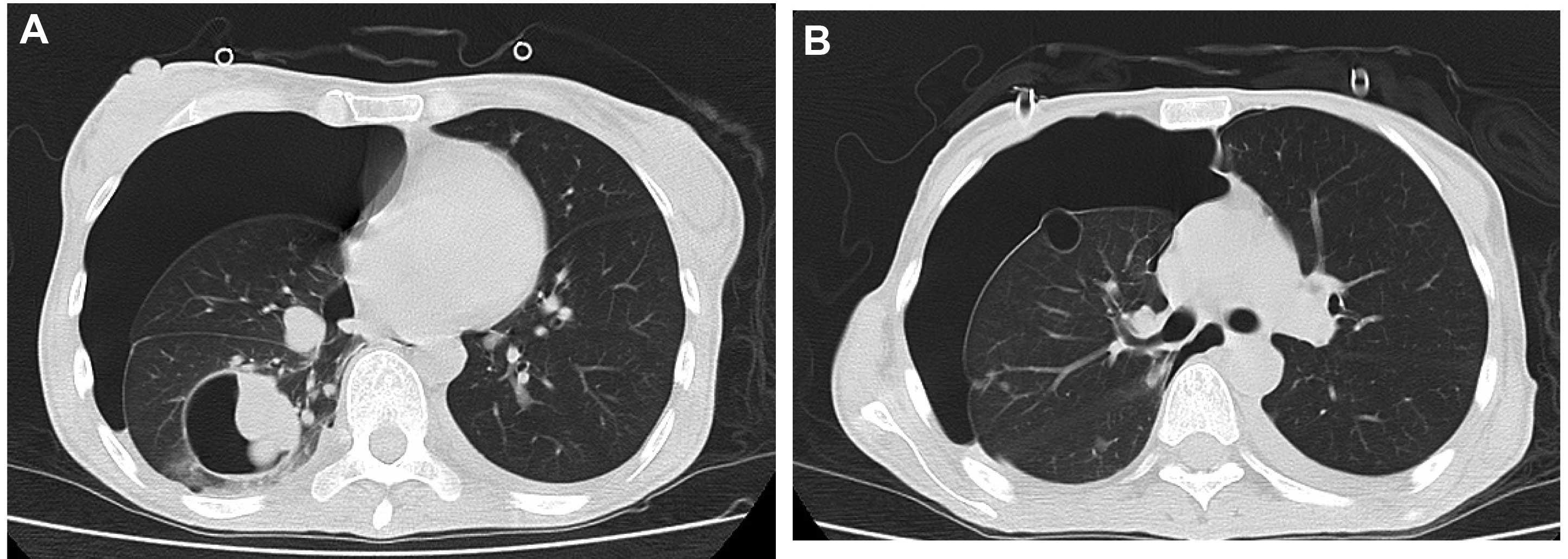
on 14 July 2014 (Fig. 2). It was
observed that bullae were present on the site of the pulmonary
metastases. When pneumothorax occurred, the bullae disappeared. We
hypothesize that the pneumothorax occurred due to the rupture of
the bullae. In October 2014, the patient succumbed to the disease
due to hemorrhage of the primary osteosarcoma lesions.
Discussion
In the present case, we identified that pulmonary
metastases cause the formation of bullae. When the bullae ruptured,
pneumothorax occurred in our osteosarcoma patient. We also consider
that chemotherapy could play a significant role in delaying the
onset of pneumothorax. Effective chemotherapy may prevent the
growth of the tumor, and delay the appearance of the bullae.
The association of spontaneous pneumothorax with
osteosarcoma is well known (1,6,7). Patients with osteosarcoma that have
pulmonary metastases have a higher risk of spontaneous pneumothorax
than patients with pulmonary metastatic carcinoma, but the reason
for this remains unclear (8). It is
also unclear whether there is any correlation between pneumothorax
and lung metastasis (9). Regardless
of whether patients with osteosarcoma have pulmonary metastases,
those who receive chemotherapy have a higher risk of spontaneous
pneumothorax than those who do not (8). It has been hypothesized that the
pneumothorax was the result of ruptures of the necrotic subpleural
micrometastasis in patients treated with chemotherapy (2). However, Smevik and Klepp reported that
the bullous change caused the metastatic pulmonary disease, and
that the peripheral tumor produced partial bronchial obstruction
and caused a ball-valve phenomenon (8). This case provided us with radiographic
evidence of this phenomenon.
Through studying this patient, we identified an
association between the bullae on the site of the pulmonary
metastasis and the pneumothorax. By comparing the chest CT film
before and after the occurrence of pneumothorax, we identified that
the bullae near to the pleura had disappeared when the pneumothorax
occurred and thus, we hypothesize that the rupture of the bullae
may have caused pneumothorax to occur. Although the pathogenesis of
spontaneous pneumothorax is not clear, we conclude that the
metastases under the pleura and the enlargement of the bullae are
necessary for the phenomenon. However, the reason why the
ball-valve phenomenon occurred in pulmonary metastases in
osteosarcoma while it is rarely observed in other lung tumors is
unknown. The answer should be elucidated following further research
on the molecular biology in the future.
References
|
1
|
Laucius JF, Brodovsky HS and Howe CD:
Spontaneous pneumothorax and pneumomediastinum as complications of
sarcoma. J Thorac Cardiovasc Surg. 64:467–471. 1972.PubMed/NCBI
|
|
2
|
D'Angio GJ and Iannoccone G: Spontaneous
pneumothorax as a complication to pulmonary metastases in malignant
tumors of childhood. Am J Roentgenol Radium Ther Nucl Med.
86:1092–1102. 1961.PubMed/NCBI
|
|
3
|
Nakada T, Okumura S, Kuroda H, et al:
Outcome of radical surgery for pulmonary metastatic osteosarcoma
with secondary spontaneous pneumothorax: Case series report. Ann
Thorac Cardiovasc Surg. 20:574–577. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bielack SS, Kempf-Bielack B, Branscheid D,
et al: Second and subsequent recurrences of osteosarcoma:
Presentation, treatment, and outcomes of 249 consecutive
cooperative osteosarcoma study group patients. J Clin Oncol.
27:557–565. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hoag JB, Sherman M, Fasihuddin Q and Lund
ME: A comprehensive review of spontaneous pneumothorax complicating
sarcoma. Chest. 138:510–518. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Swaney JJ and Cangir A: Spontaneous
pneumothorax in metastatic osteogenic sarcoma. J Pediatr.
82:165–166. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Spittle MF, Heal J, Harmer C and White WF:
The association of spontaneous pneumothorax with pulmonary
metastases in bone tumors of children. Clin Radiol. 19:400–403.
1968. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Smevik B and Klepp O: The risk of
spontaneous pneumothorax in patients with osteogenic sarcoma and
testicular cancer. Cancer. 49:1734–1737. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yamamoto T and Mizuno K: Spontaneous
pneumothorax without any detectable pulmonary metastases in a
patient with osteosarcoma. Int Orthop. 23:361–362. 1999. View Article : Google Scholar : PubMed/NCBI
|