Introduction
Xanthogranulomas are known to develop in the
gallbladder and kidney (1,2). However, rare cases of
xanthogranulomatous inflammation have additionally been reported in
other organs, including the stomach, colon, pancreas and uterus
(3–6).
Despite being a benign disease, this uncommon inflammation can
progressively invade adjacent organs, mimicking malignant tumor,
which often leads to unnecessary resection. Preoperative diagnosis
of xanthogranulomatous inflammation is difficult and its' features
are unknown (1–6). A xanthogranuloma occurring in the
stomach is rare, and to the best of our knowledge, only a few cases
have been reported to date (6–16). In such
cases, the disease was preoperatively misdiagnosed as a submucosal
tumor or advanced gastric cancer, and gastrectomy was performed
(6–16). Due to the rarity of
xanthogranulomatous gastritis, incidence and mortality rates remain
unclear. In addition, no optimal treatments have been identified
for this condition. The present study reports a rare case of
xanthogranulomatous gastritis of the remnant stomach following
partial gastrectomy, mimicking a malignant tumor. Written informed
consent was obtained from the patient
Case report
A 64-year-old man previously underwent a wide
resection of the stomach, following a Billroth-I reconstruction for
a gastric ulcer (details unknown). Approximately 40 years after
this, in July 2014, the patient presented to Kawagoe
Gastrointestinal Hospital (Kawagoe, Japan) due to tarry stools. A
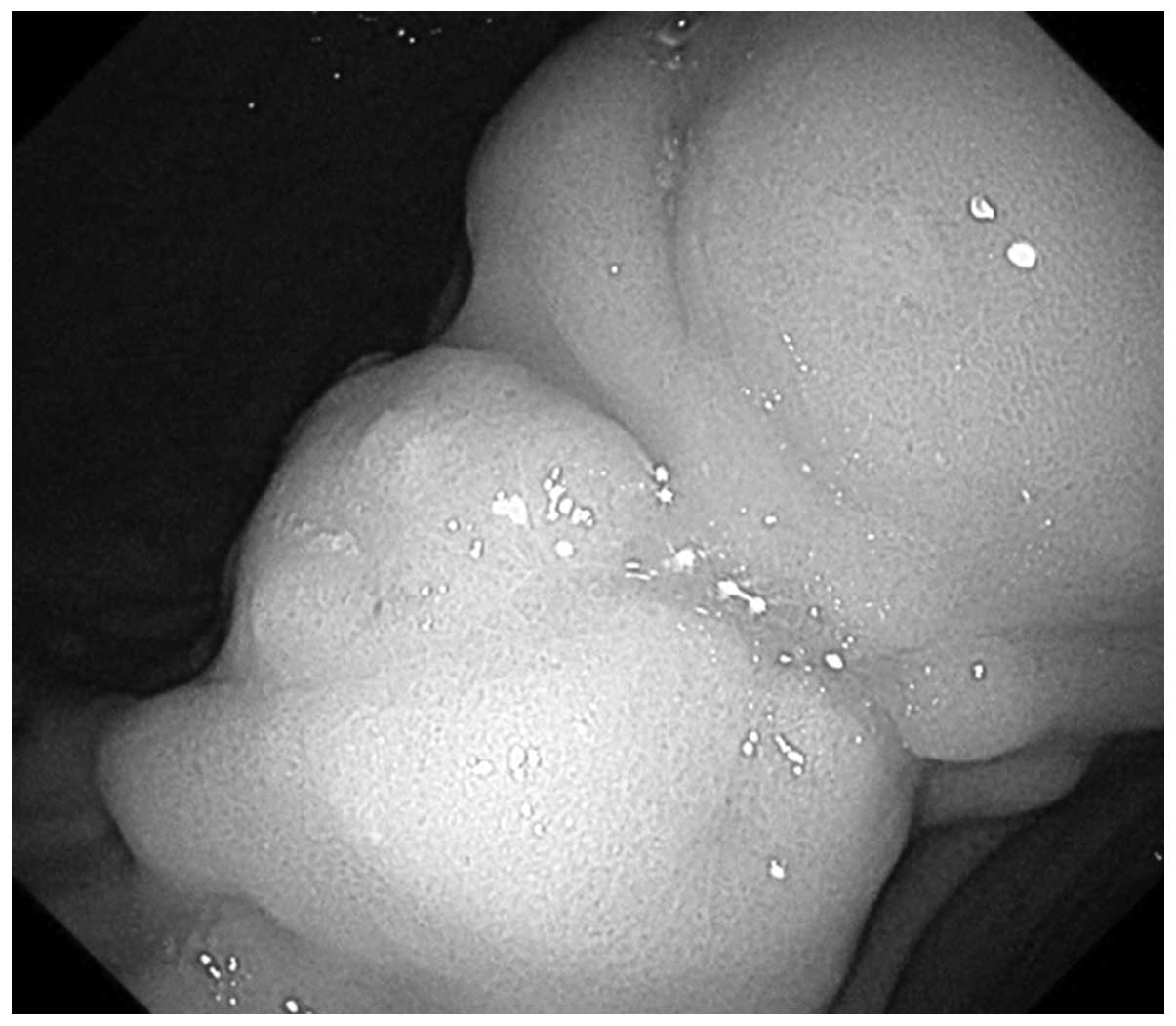
gastrointestinal endoscopy was performed, leading to identification
of a gastric lesion at the previous suture line of the lesser
curvature of the remnant stomach, which was elevated and appeared
to indicate a submucosal tumor (SMT) with an ulcerated lesion
(Fig. 1). The patient was then
referred to Keio University Hospital (Tokyo, Japan) in August 2014.
There was no increase in the serum levels of carcinoembryonic
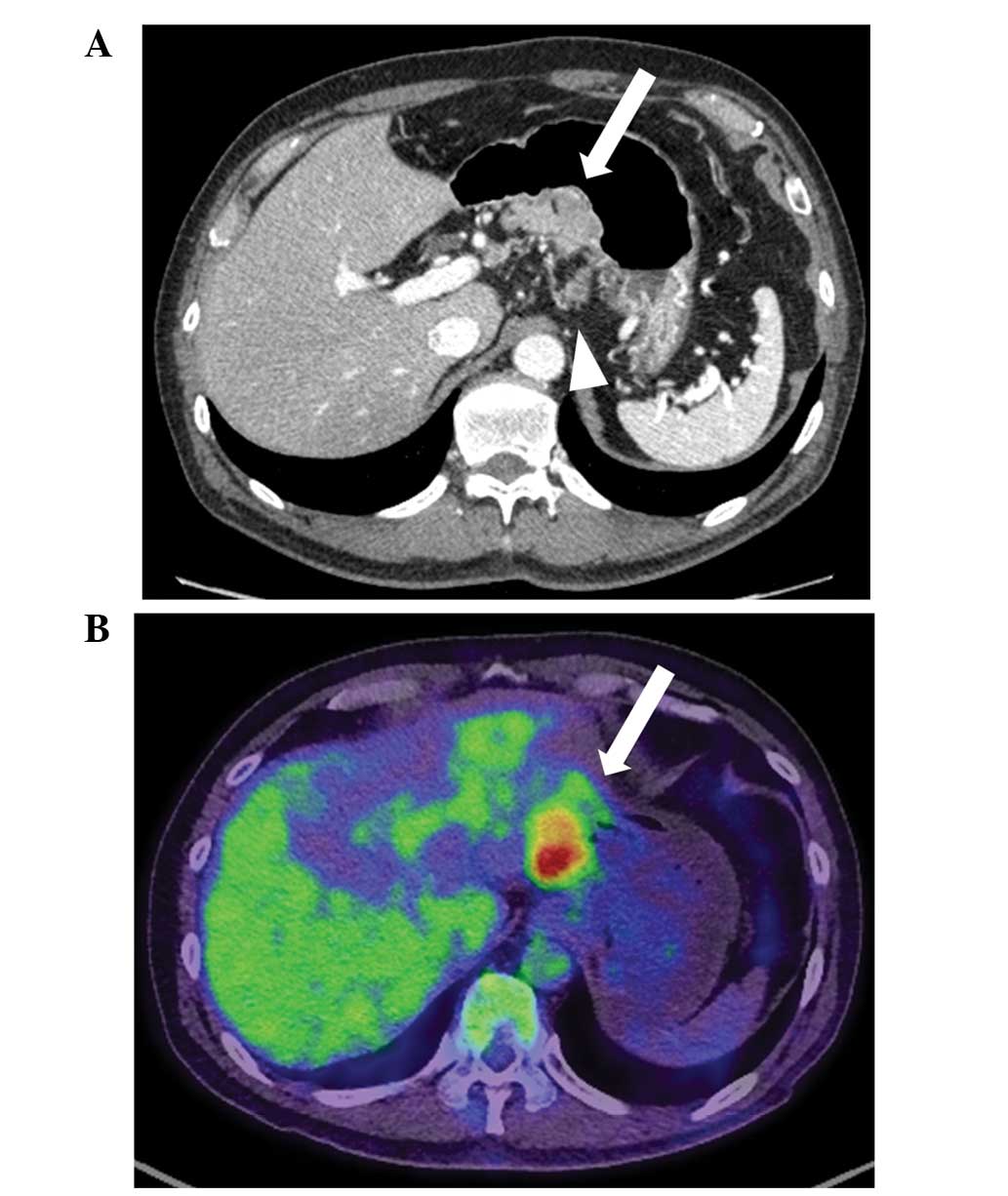
antigen or carbohydrate antigen 19–9. Computed tomography revealed
wall thickening in the lesser curvature of the remnant stomach and
swollen regional lymph nodes (Fig.
2A). Positron emission tomography (PET) revealed uptake of the
fluorodeoxyglucose (FDG) radiotracer by the tumor (Fig. 2B), with a maximum standard uptake
value (SUV) of 8.41 at the early phase and 7.94 at the late phase.
Biopsy specimens from the lesion indicated chronic gastritis with
regenerative changes and intestinal metaplasia.
Although not indicated by the pathological findings,
it was suspected that the tumor was a highly malignant entity, and
was potentially a malignant gastrointestinal stromal tumor (GIST)
or remnant gastric cancer with extended submucosal invasion due to
the marked FDG uptake. As a curative resection appeared possible,
complete resection of the remnant stomach was performed, with a
lymphadenectomy and splenectomy. According to the Japanese Gastric
Cancer Treatment Guidelines 2010 (ver. 3), these procedures are
required for the performance of curative resection for advanced
remnant gastric cancer (17).
Open surgery was performed, which revealed severe
adhesion of the left hepatic lobe and gastric wall. The lesion was
located at the lesser curvature of the remnant stomach and was
relatively similar to a lipoma. However, the regional lymph nodes
were swollen; thus, the intended procedures were performed as
planned. The specimens were removed, and a Roux-en-Y reconstruction
was performed. The post-operative course was positive, and the
patient was discharged from hospital 13 days after surgery.
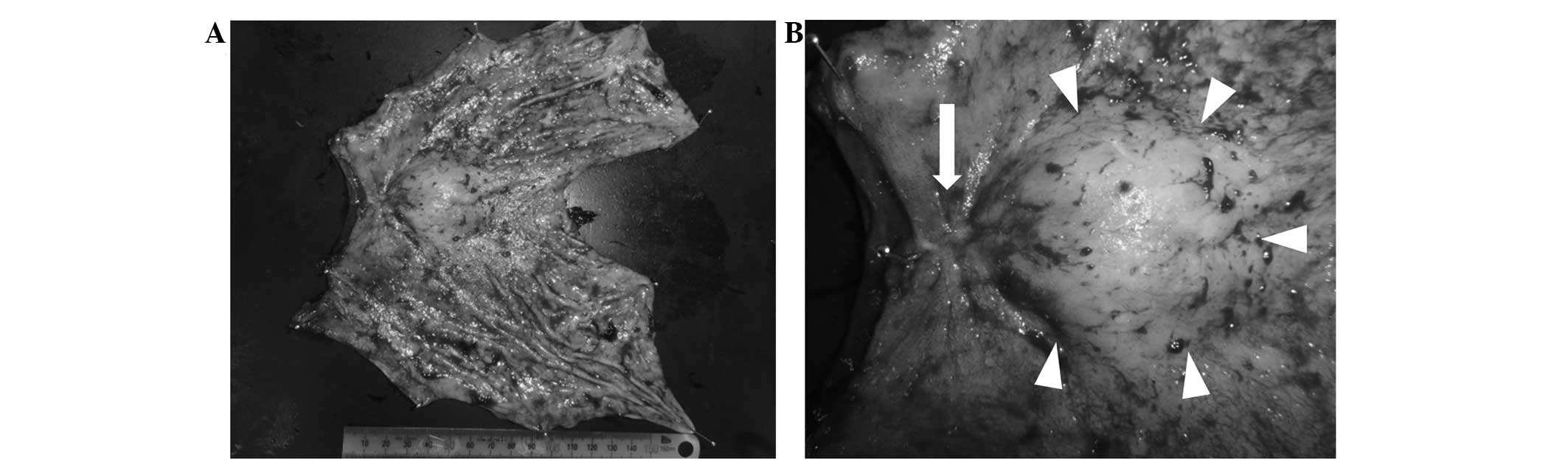
Macroscopically, the tumor was soft, measuring 65×40
mm, and appeared to be a combination of a slightly depressed lesion
and SMT (Fig. 3). Histological
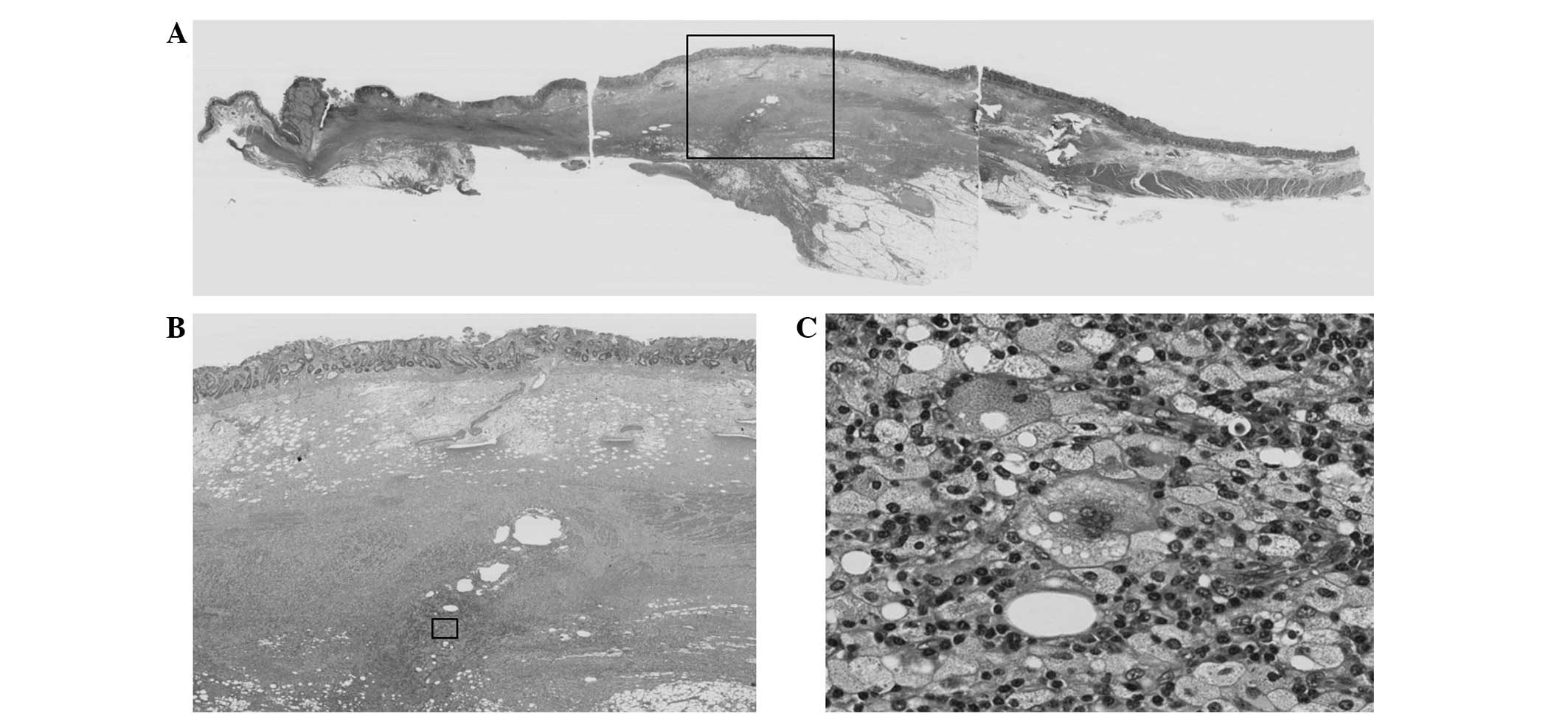
analysis of the resected remnant stomach revealed
xanthogranulomatous inflammation with foamy histiocytes and plasma
cells from the submucosal to subserosal layers (Fig. 4). Chronic gastritis with regenerative
changes and intestinal metaplasia was observed on the surface of
the type 0-IIc lesion. A small number of multinucleated giant cells
were observed in the marginal sinuses of the resected lymph nodes.
However, no cancer cells were observed in the resected specimens.
Therefore, the tumor was diagnosed as xanthogranulomatous
gastritis.
At follow-up 1 year after surgery, there was no
evidence of recurrence of inflammation. The patient continues to
undergo postoperative gastrectomy follow-up.
Discussion
Xanthogranulomatous inflammation is a rare
inflammatory lesion characterized by marked proliferative fibrosis,
with infiltration of foamy histiocytes and other acute and chronic
inflammatory cells (13). These
lesions are common in the gallbladder as xanthogranulomatous
cholecystitis and in the kidney as xanthogranulomatous
pyelonephritis (1,2). However, rare cases of
xanthogranulomatous inflammation have additionally been reported in
other organs, including the stomach, colon, pancreas and uterus
(3–6).
The occurrence of xanthogranuloma of the stomach is rare, and only
a few cases have been reported to date (6–16). To the
best of our knowledge, this is the first reported case of
xanthogranulomatous gastritis in the remnant stomach.
The pathogenesis of xanthogranuloma remains to be
elucidated, although it is proposed to be a chronic lesion
associated with infection, immunological disorders, lymphatic
obstruction and lipid transport (14). It is additionally speculated that
xanthogranulomatous cholecystitis results from sterile chronic
inflammation due to extravasation of bile into the gallbladder wall
with involvement of the Rokitansky-Aschoff sinuses or via a small
mucosal ulceration (18). Although no
studies have described a correlation between xanthogranulomatous
gastritis and previous gastric surgery, the pathogenesis in the
present case may be associated with the response following the
previous surgery, as the tumor was located at the previous suture
line. In addition, Guarino et al (11) suggested the potential correlation of
bile reflux into the stomach following a wide gastrectomy
subsequent to Billroth-I reconstruction with the development of
xanthogranulomatous gastritis.
As in the present case, xanthogranulomatous
gastritis has been misdiagnosed as SMT and gastric cancer in
previous reports (6–16). Although not indicated by pathological
findings, a malignant gastric tumor was initially suspected, for
example a malignant GIST or gastric cancer, due to the gross
features observed by endoscopy and the marked FDG uptake observed
during PET. A diagnosis of xanthogranulomatous gastritis was not
considered. Despite a low incidence, it is clear that the
possibility of an inflammatory tumor should be included in the
differential diagnosis of malignant tumors. However, none of the
previously reported cases were definitively diagnosed prior to
surgical resection. Therefore, distinguishing xanthogranulomatous
gastritis from other malignancies remains difficult. In addition,
xanthogranulomatous gastritis combined with gastric cancer should
be considered in these cases (14,16).
In the present case, endoscopic evaluation revealed
an elevated ulcerated lesion. Biopsy specimens did not indicate
malignancy. However, this result did not definitively
contraindicate advanced gastric cancer; thus, the tumor was
‘overdiagnosed’ and a radical resection was performed.
Histopathologically, on the surface of the lesion, only chronic
gastritis with regenerative changes and intestinal metaplasia was
observed. In addition, the layer of muscularis propria was lacking,
and the laminar structure of the gastric wall was not retained. It
was speculated that destruction of the laminar structure occurred
due to the inflammation, or that it had potentially been altered
during the previous surgery. The ulcerated section of the lesion
may have been associated with the xanthogranulomatous inflammation
itself or with the previous suture line.
PET is an imaging method that has a significant role
in the evaluation of a wide range of malignancies (19). The SUV is used as a semi-quantitative
measure of the degree of metabolic activity in abnormal tissues. In
general, inflammation is indicated by intense FDG uptake, which may
additionally indicate malignancy, due to the intense glucose
metabolism in inflammatory cells. Previous studies have noted that
it is challenging to differentiate between xanthogranulomatous
inflammation and malignancy using PET (13,20).
Therefore, arriving at a clinical diagnosis of xanthogranulomatous
gastritis may be difficult and may only be established via
histological examination.
In conclusion, to the best of our knowledge, the
present case is the first report of xanthogranulomatous gastritis
of the remnant stomach mimicking a malignant tumor. Therefore,
inflammatory tumors should be considered in the differential
diagnosis of malignant tumors, even though distinguishing them from
other tumors remains challenging.
Glossary
Abbreviations
Abbreviations:
|
GIST
|
gastrointestinal stromal tumor
|
|
SMT
|
submucosal tumor
|
|
PET
|
positron emission tomography
|
|
FDG
|
fluorodeoxyglucose
|
|
SUV
|
standard uptake value
|
References
|
1
|
Benbow EW: Xanthogranulomatous
cholecystitis. Br J Surg. 77:255–256. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Korkes F, Favoretto RL, Bróglio M, Silva
CA, Castro MG and Perez MD: Xanthogranulomatous pyelonephritis:
Clinical experience with 41 cases. Urology. 71:178–180. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Oh YH, Seong SS, Jang KS, Chung YW, Paik
CH, Park YW and Han DS: Xanthogranulomatous inflammation presenting
as a submucosal mass of the sigmoid colon. Pathol Int. 55:440–444.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nishimura M, Nishihira T, Hirose T,
Ishikawa Y, Yamaoka R, Inoue H and Tatsuta M: Xanthogranulomatous
pancreatitis mimicking a malignant cystic tumor of the pancreas:
Report of a case. Surg Today. 41:1310–1313. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Russack V and Lammers RJ:
Xanthogranulomatous endometritis. Report of six cases and a
proposed mechanism of development. Arch Pathol Lab Med.
114:929–932. 1990.PubMed/NCBI
|
|
6
|
Zafisaona G and Kermarec J: Inflammatory
fibrous histiocytoma of the stomach. Apropos of a case of
xanthogranuloma? Arch Anat Cytol Pathol. 35:149–153. 1987.(In
French). PubMed/NCBI
|
|
7
|
Kubosawa H, Yano K, Oda K, Shiobara M,
Ando K, Nunomura M and Sarashina H: Xanthogranulomatous gastritis
with pseudosarcomatous changes. Pathol Int. 57:291–295. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lai HY, Chen JH, Chen CK, Chen YF, Ho YJ,
Yang MD and Shen WC: Xanthogranulomatous pseudotumor of stomach
induced by perforated peptic ulcer mimicking a stromal tumor. Eur
Radiol. 16:2371–2372. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lespi PJ: Gastric xanthogranuloma
(inflammatory malignant fibrohistiocytoma). Case report and
literature review. Acta Gastroenterol Latinoam. 28:309–310.
1998.(In Spanish). PubMed/NCBI
|
|
10
|
Parsons MA: Xanthogranulomatous gastritis:
An entity or a secondary phenomenon? J Clin Pathol. 46:580–581.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Guarino M, Reale D, Micoli G, Tricomi P
and Cristofori E: Xanthogranulomatous gastritis: Association with
xanthogranulomatous cholecystitis. J Clin Pathol. 46:88–90. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang L, Huang X and Li J: Xanthogranuloma
of the stomach: A case report. Eur J Surg Oncol. 18:293–295.
1992.PubMed/NCBI
|
|
13
|
Tsukada T, Nakano T, Miyata T, Sasaki S
and Higashi K: Xanthogranulomatous gastritis mimicking malignant
GIST on F-18 FDG PET. Ann Nucl Med. 26:752–756. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kinoshita H, Yamaguchi S, Sakata Y, Arii
K, Mori K and Kodama R: A rare case of xanthogranuloma of the
stomach masquerading as an advanced stage tumor. World J Surg
Oncol. 9:672011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Banerjee S, Shah S, Chandran BS, Pulimood
A and Mathew G: Chronic perforation in isolated xanthogranulomatous
gastritis. Trop Gastroenterol. 31:45–47. 2010.PubMed/NCBI
|
|
16
|
Aikawa M, Ishii T, Nonaka K, Nakao M,
Ishikawa K, Arai S, Kita H, Miyazawa M, Koyama I, Motosugi U and
Ban S: A case of gastric xanthogranuloma associated with early
gastric cancer. Nihon Shokakibyo Gakkai Zasshi. 106:1610–1615.
2009.(In Japanese). PubMed/NCBI
|
|
17
|
Japanese Gastric Cancer Association:
Japanese gastric cancer treatment guidelines (ver. 3). Gastric
Cancer. 14:113–123. 2011.PubMed/NCBI
|
|
18
|
Goodman ZD and Ishak KG:
Xanthogranulomatous cholecystitis. Am J Surg Pathol. 5:653–659.
1981. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Czernin J, Allen-Auerbach M and Schelbert
HR: Improvements in cancer staging with PET/CT: Literature-based
evidence as of September 2006. J Nucl Med. 48(Suppl 1): S78–S88.
2007.
|
|
20
|
Makino I, Yamaguchi T, Sato N, Yasui T and
Kita I: Xanthogranulomatous cholecystitis mimicking gallbladder
carcinoma with a false-positive result on fluorodeoxyglucose PET.
World J Gastroenterol. 15:3691–3693. 2009. View Article : Google Scholar : PubMed/NCBI
|