Introduction
Primary thyroid lymphoma (PTL) is a relatively rare
malignant tumor, which accounts for <5% of all thyroid
malignancies and ~3% of all extranodal lymphomas (1). The two most common subtypes of PTL are
diffuse large B-cell lymphoma (DLBCL) and mucosa-associated
lymphoid tissue (1). Other subtypes
of PTL include follicular lymphoma and classic Hodgkin's lymphoma
of T-cell origin (2). Clinical signs
of PTL include a rapidly enlarging mass in the neck, hoarseness and
dyspnea; other symptoms, such as weight loss and fever, may also be
present. The treatment and prognosis of PTL depend on the specific
subtype and staging. A 5-year survival of 90% has been reported in
correctly diagnosed and treated PTL patients (2), so a timely and accurate diagnosis of PTL
is required for successful treatment and a good prognosis.
Aggressive PTL is rare, and there is limited literature regarding
its imaging characteristics (3). In
the present study, two cases of PTL in two elderly patients are
reported. Both cases presented as enlarged thyroid and were
associated with extensive invasion into adjacent structures. The
ultrasonographic features of the two cases are described in the
present report. Written informed consent was obtained from both
patients.
Case reports
Case 1
In August 2014, 63-year-old female patient presented
to The First Affiliated Hospital of Wannan Medical College (Wuhu,
China) with a 2-month history of a rapidly growing mass in the
front of her neck. The patient had no symptoms of dyspnea,
hoarseness, dysphagia, dysphasia or stridor. On physical
examination, the right thyroid lobe was noted to be enlarged and
firm. There was a palpable mass in the front of her neck, which
moved during swallowing. The patient had no history of Hashimoto's
thyroiditis (HT), and her thyroid function test was within the
normal range [free T3 (FT3), 4.89 pmol/l; normal range, 3.5–6.5
pmol/l; free T4 (FT4), 18.73 pmol/l; normal range, 11.5–22.7
pmol/l; ultrasensitive thyroid stimulating hormone (TSH3UL), 0.591
milli international units (mIU)/l; normal range, 0.55–4.78 mIU/l;
antithyroglobulin antibody (ATG-Ab), 25.90; normal range, 0–60
units (U)/ml; thyroid peroxidase antibody (TPO-Ab), 38.70 U/ml;
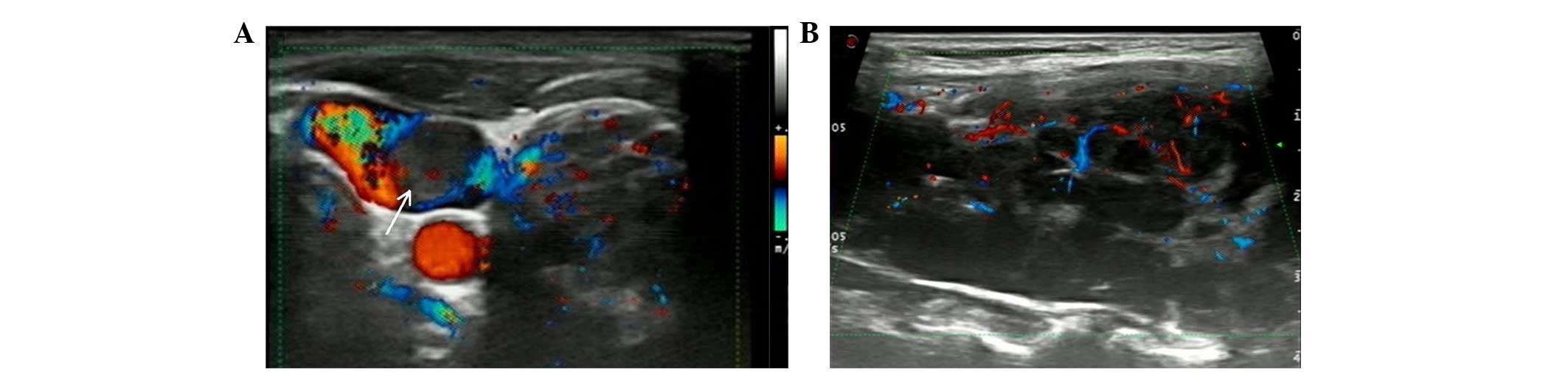
normal range, 0–60 U/ml]. Ultrasonography (US; Mylab 90; Esaote,
Genoa, Italy) revealed an irregular shaped mass in the right lobe
of the thyroid. The mass, which measured ~6×5 cm in size, extended
to the right submandibular region and invaded the right internal
jugular vein (RIJV) and adjacent muscles (Fig. 1A). The mass was heterogeneously
hypoechoic. There were increased twisted blood flow signals, but no
defined calcification, hemorrhage or necrotic portion were observed
within the mass, which exhibited indistinct margins and posterior
acoustic enhancement (PAE) (Fig. 1B).
The subsequent surgery performed on the patient confirmed the
presence of the mass in the right lobe of the thyroid.
Lymphadenopathies invaded the RIJV, which was partly occluded, and
the adjacent muscles. Therefore, the surgery included
thyroidectomy, and resection of part of the RIJV and adjacent
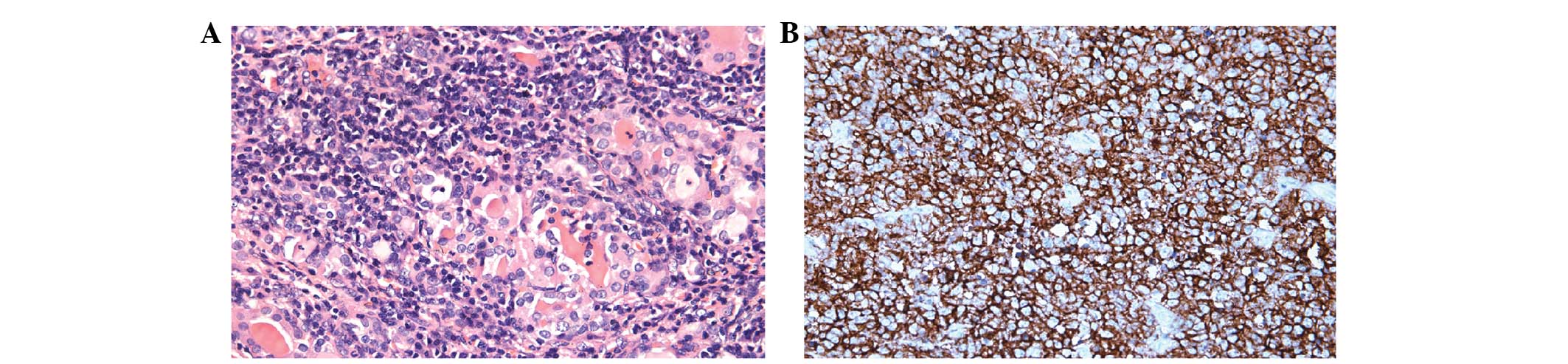
muscles. Postoperative histopathology and immunohistochemical
examinations using a BX53 microscope (Olympus Corporation, Tokyo,
Japan) confirmed primary DLBCL (Fig.
2): Hematoxylin and eosin (Wuxi Jiangyuan Industrial Technology
and Trade Corporation, Wuxi, China) staining showed follicular
atrophy of the thyroid and incubation of tissues with monoclonal
mouse anti-human cluster of differentiation (CD)20 antibody (cat.
no. 0001; 1:100; Fuzhou Maixin Biotechnology Development Co., Ltd.,
Fuzhou, China) at 25°C for 30 min revealed strong CD20 expression.
The postoperative course was uneventful, and the patient was
additionally treated with chemotherapy at the Second People's
Hospital of Wuhu (Wuhu, China).
Case 2
In July 2013, a 60-year-old male patient was
transferred to The First Affiliated Hospital of Wannan Medical
College with a 1-month history of a rapidly enlarged thyroid and
several nodules in the front of his neck. The patient had no
symptoms of dyspnea, hoarseness, dysphagia, dysphasia or stridor.
On physical examination, the whole thyroid was observed to be
diffusely enlarged and firm. There were several palpable nodules in
his neck, and the enlarged thyroid did not move during swallowing.
The patient had no history of HT, and his thyroid function was
markedly reduced (FT3, 1.52 pmol/l; normal range, 3.5–6.5 pmol/l;
FT4, 5.75 pmol/l; normal range, 11.5–22.7 pmol/l; TSH3UL, 5.892
mIU/l, normal range 0.55–4.78 mIU/l; ATG-Ab, 37.20 U/ml; normal
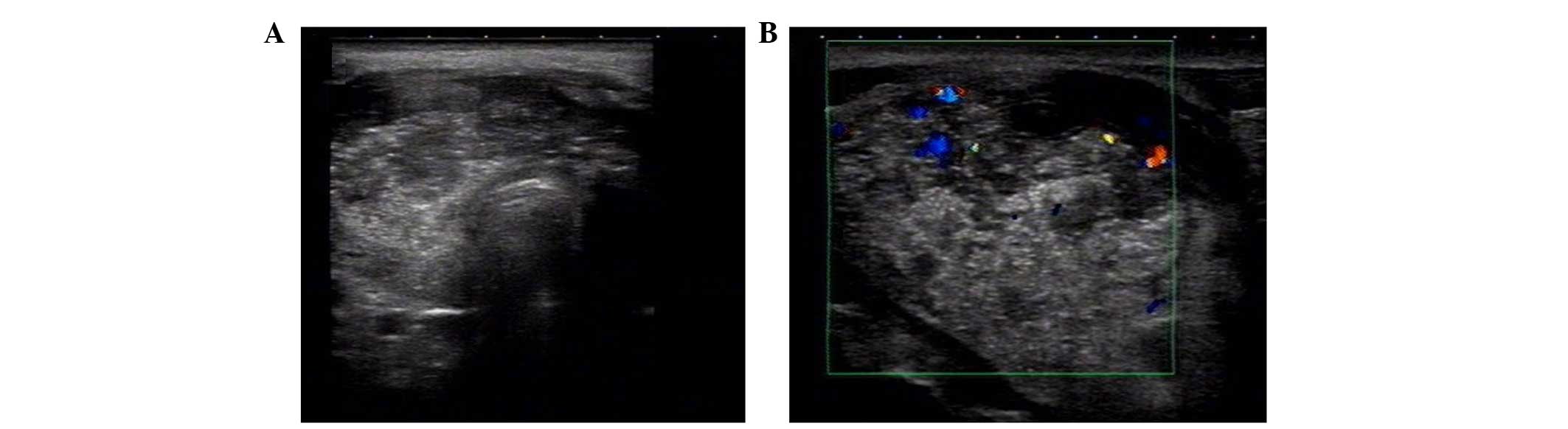
range, 0–60 U/ml; TPO-Ab, 58.70 U/ml; normal range, 0–60 U/ml). US
revealed that the thyroid was diffusely asymmetrically enlarged
with unclear boundaries, and the whole gland was non-uniformly
hypoechoic. There were multiple calcified spots, but no defined
hemorrhage or necrotic portion were observed within the whole gland
(Fig. 3A). Color Doppler US displayed
rare blood flow signals (Fig. 3B). A
number of enlarged lymph nodes were detected, and the adjacent
muscles in the front of his neck were invaded. Fine-needle
aspiration biopsy (FNA; 22G, 70 mm needle; Hakko Medical Co., Ltd.,
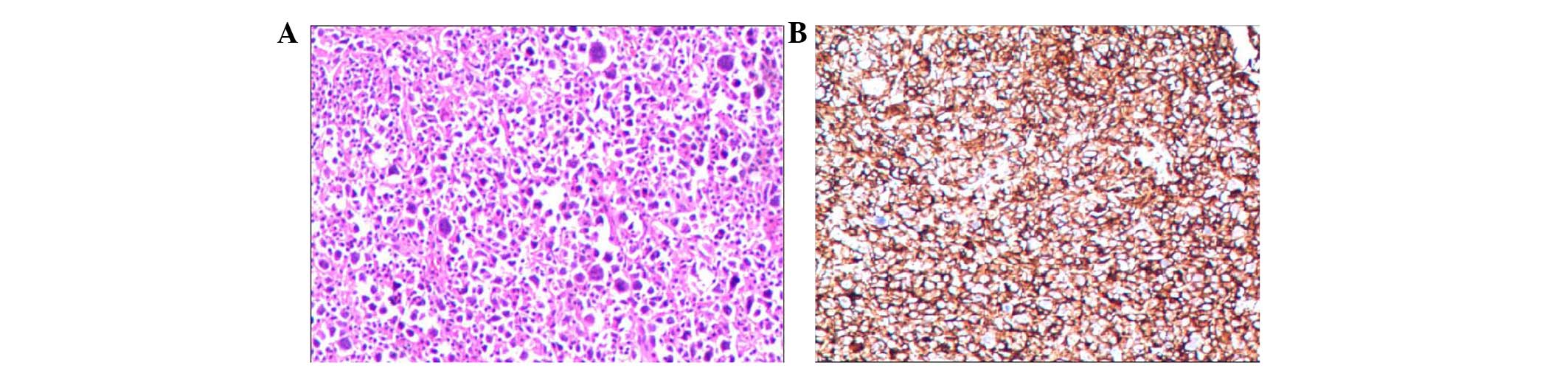
Tokyo, Japan) and subsequent histopathology and immunohistochemical
examinations using a BX53 microscope (Olympus Corporation)
confirmed primary DLBCL (Fig. 4):
Tissues were incubated with mouse anti-human CD20 antibody (cat.
no. 0001; Fuzhou Maixin Biotechnology Development Co., Ltd.) at
25°C for 30 min, which revealed that CD20 was widely expressed. The
patient was only treated with chemotherapy at the Second People's
Hospital of Wuhu (Wuhu, China).
Discussion
The most common clinical presentation of PTL is a
rapidly growing goiter and other compressive symptoms, including
dyspnea, hoarseness, dysphagia, dysphasia and stridor (4). The majority of patients with PTL are
elderly women, and the condition is usually associated with HT
(5). However, none of the present
patients had compressive symptoms or HT. In addition, case 2 was a
male patient. These characteristics rarely appear in the existing
literature (6).
Computed tomography (CT) is generally used for
evaluating the involvement of surrounding structures and displaying
cervical and mediastinal nodal diseases in cases of PTL (7). Magnetic resonance imaging (MRI) is more
accurate and sensitive than CT in diagnosing soft-tissue lesions
(8), but positron emission tomography
(PET) has been proved superior in diagnostic accuracy of PTL,
compared with CT and MRI (9).
However, the present cases had not undergone CT, MRI or PET, but
only US, and the ultrasonographic findings are described in the
present report.
US is the imaging modality of choice for thyroid
pathology, and the typical ultrasonographic feature of PTL is the
presence of a circumscribed mass or diffuse heterogeneous
hypoechoic parenchyma with structures resembling septa (10). When presenting as a diffuse
heterogeneous hypoechoic parenchyma, the ultrasonographic imaging
features of PTL are very similar to those of HT (11). By contrast, cervical lymphadenopathies
are normally present in the majority of patients with PTL, whereas
calcification is never detected in HT and seldom detected in PTL,
according to previous studies (12).
The patient of case 2 had no history of HT, numerous enlarged lymph
nodes were detected in his neck and multiple calcified spots were
detected in his enlarged thyroid, which indicated malignancy. When
presenting as a mass, PTL normally displays homogenous
echogenicity, PAE, and lack of calcification, necrosis and cystic
degeneration (13), while the
surrounding structures are rarely invaded by PTL (12). Notably, PAE is the most common
ultrasonographic feature of PTL, and it may also be detected in
cystic lesions and solid benign tumors, but rarely detected in
malignant masses (14). The
ultrasonographic features of the patient of case 1 revealed a
heterogeneous hypoechoic mass that invaded adjacent structures,
including the RIJV and muscles. These features implied anaplastic
thyroid carcinoma (ATC) rather than PTL. However, there was PAE and
no defined calcification, hemorrhage or necrotic portion within the
mass of the present case, which indicated PTL rather than ATC.
Thus, it is difficult to distinguish PTL from ATC by US alone.
Therefore, thyroid masses should undergo palpation-guided FNA
biopsy, while non-palpable masses should undergo US-guided FNA
biopsy for accurate diagnosis prior to surgical operation.
There is limited literature about blood flow signals
in PTL. The blood flow signals in benign tumors are generally
travelling naturally and present a uniform distribution, while
malignant tumors are normally characterized by twisted blood flow
signals and a non-uniform distribution (6). The characteristics of the blood flow
signals in the patient of case 1 were coincident with those of
malignant tumors. By contrast, color Doppler US of case 2 displayed
rare blood flow signals, which may be due to the small size of the
tumor's blood vessels, thus being difficult for color Doppler US to
display blood flow signals, contrarily to what has been previously
reported in the literature (13).
Due to its interference with gas and bone, US has
difficulty in displaying organizational structure in the deep neck
(14). However, the ultrasonographic
imaging features of the present cases demonstrated clear invasion,
which may be due to the fact that the invasion was superficial, and
is indicative of malignant lesion in US. The tumor thrombosis of
case 1 only occluded part of the RIJV lumen, thus the patient had
no symptoms of RIJV occlusion. The tumor in case 2 only invaded the
adjacent muscles, while the esophagus, trachea, carotid artery and
jugular vein presented no sign of invasion.
In conclusion, the ultrasonographic features of PTL
are complicated and variable. US is a valuable imaging method in
assessing PTL, but it is difficult to establish a diagnosis by US
alone. Therefore, pathology should be performed to confirm this
disease. In summary, the present report describes the
ultrasonographic features of two rare cases of PTL.
Acknowledgements
The present study has been supported by funding from
the First Affiliated Hospital of Wannan Medical College Program
(grant no., WK2015ZF).
References
|
1
|
Walsh S, Lowery AJ, Evoy D, McDermott EW
and Prichard RS: Thyroid lymphoma: Recent advances in diagnosis and
optimal management strategies. Oncologist. 18:994–1003. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Graff-Baker A, Roman SA, Thomas DC,
Udelsman R and Sosa JA: Prognosis of primary thyroid lymphoma:
Demographic, clinical, and pathologic predictors of survival in
1,408 cases. Surgery. 146:1105–1115. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Xia Y, Wang L, Jiang Y, Dai Q, Li X and Li
W: Sonographic appearance of primary thyroid lymphoma-preliminary
experience. PLoS One. 9:e1140802014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sasai K, Yamabe H, Haga H, Tsutsui K, Dodo
Y, Ishigaki T, Shibamoto Y and Abe M: Non-Hodgkin's lymphoma of the
thyroid. A clinical study of twenty-two cases. Acta Oncol.
35:457–462. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aozasa K: Hashimoto's thyroiditis as a
risk factor of thyroid lymphoma. Acta Pathol Jpn. 40:459–468.
1990.PubMed/NCBI
|
|
6
|
Wang Z, Fu B, Xiao Y, Liao J and Xie P:
Primary thyroid lymphoma has different sonographic and color
Doppler features compared to nodular goiter. J Ultrasound Med.
34:317–323. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Li XB and Ye ZX: Primary thyroid lymphoma:
Multi-slice computed tomography findings. Asian Pac J Cancer Prev.
16:1135–1138. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Takashima S, Nomura N, Noguchi Y,
Matsuzuka F and Inoue T: Primary thyroid lymphoma: Evaluation with
US, CT, and MRI. J Comput Assist Tomogr. 19:282–288. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Baba S, Abe K, Isoda T, Maruoka Y, Sasaki
M and Honda H: Impact of FDG-PET/CT in the management of lymphoma.
Ann Nucl Med. 25:701–716. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kwak JY, Kim EK, Ko KH, Yang WI, Kim MJ,
Son EJ, Oh KK and Kim KW: Primary thyroid lymphoma: role of
ultrasound-guided needle biopsy. J Ultrasound Med. 26:1761–1765.
2007.PubMed/NCBI
|
|
11
|
Nam M, Shin JH, Han BK, Ko EY, Ko ES, Hahn
SY, Chung JH and Oh YL: Thyroid lymphoma: Correlation of radiologic
and pathologic features. J Ultrasound Med. 31:589–594.
2012.PubMed/NCBI
|
|
12
|
Vigliar E, Caleo A, Vitale M, Di Crescenzo
V, Garzi A and Zeppa P: Early cytological diagnosis of extranodal
stage I, primary thyroid Non-Hodgkin lymphoma in elderly patients.
Report of two cases and review of the literature. BMC Surg.
13(Suppl 2): S492013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ota H, Ito Y, Matsuzuka F, Kuma S, Fukata
S, Morita S, Kobayashi K, Nakamura Y, Kakudo K, Amino N and
Miyauchi A: Usefulness of ultrasonography for diagnosis of
malignant lymphoma of the thyroid. Thyroid. 16:983–987. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cho JH, Park YH, Kim WS, Oh SY, Cho SI,
Kang HJ, Na II, Ryoo BY, Yang SH, Kim K, et al: High incidence of
mucosa-associated lymphoid tissue in primary thyroid lymphoma: A
clinicopathologic study of 18 cases in the Korean population. Leuk
Lymphoma. 47:2128–2131. 2006. View Article : Google Scholar : PubMed/NCBI
|