Introduction
The majority of capillary hemangiomas occur
superficially in the cutaneous and mucosal tissues of the face,
neck, nasal vault and oral cavity, particularly in children
(1,2).
Within the nervous system, these tumors have been found in the
spinal cord, the cauda equina and the nerve roots (3–5). According
to the statistics and data analyses performed in a previous study,
vascular lesions comprise 6–7% of all spinal intradural tumors,
including capillary hemangioma, cavernous angiomas, and
arteriovenous and venous malformations (6). Furthermore, capillary hemangiomas that
occur in the intradural extramedullary space are extremely rare.
Due to the rarity of such tumors, incidence and mortality rates
remain unclear. Intradural capillary hemangiomas commonly behave as
space-occupying tumors, which may subsequently lead to chronic
progressive radiculopathy or myelopathy (7). Imaging examination, particularly
magnetic resonance imaging (MRI), aids in the determination of the
size and location of the mass, and whether the mass is benign or
malignant (7). Complete resection is
considered as the most effective treatment of intradural capillary
hemangioma (6). The current study
presents a rare case of intradural extramedullary capillary
hemangioma in a 59-year-old woman, and reviews the previously
reported cases in the literature.
Case report
Case presentation
A 59-year-old woman presented to Lishui Center
Hospital due to backache and right lower limb numbness that had
progressed over 20 days. The patient had no history of coronary
disease, obesity, type II diabetes mellitus or hypertension.
Written informed consent was obtained from the patient for the
publication of the present study.
Clinical analysis and surgery
Upon physical examination, superficial sensations of
the right lateral crural region and dorsum pedis were decreased.
Knee and ankle reflexes were increased. The straight leg raise test
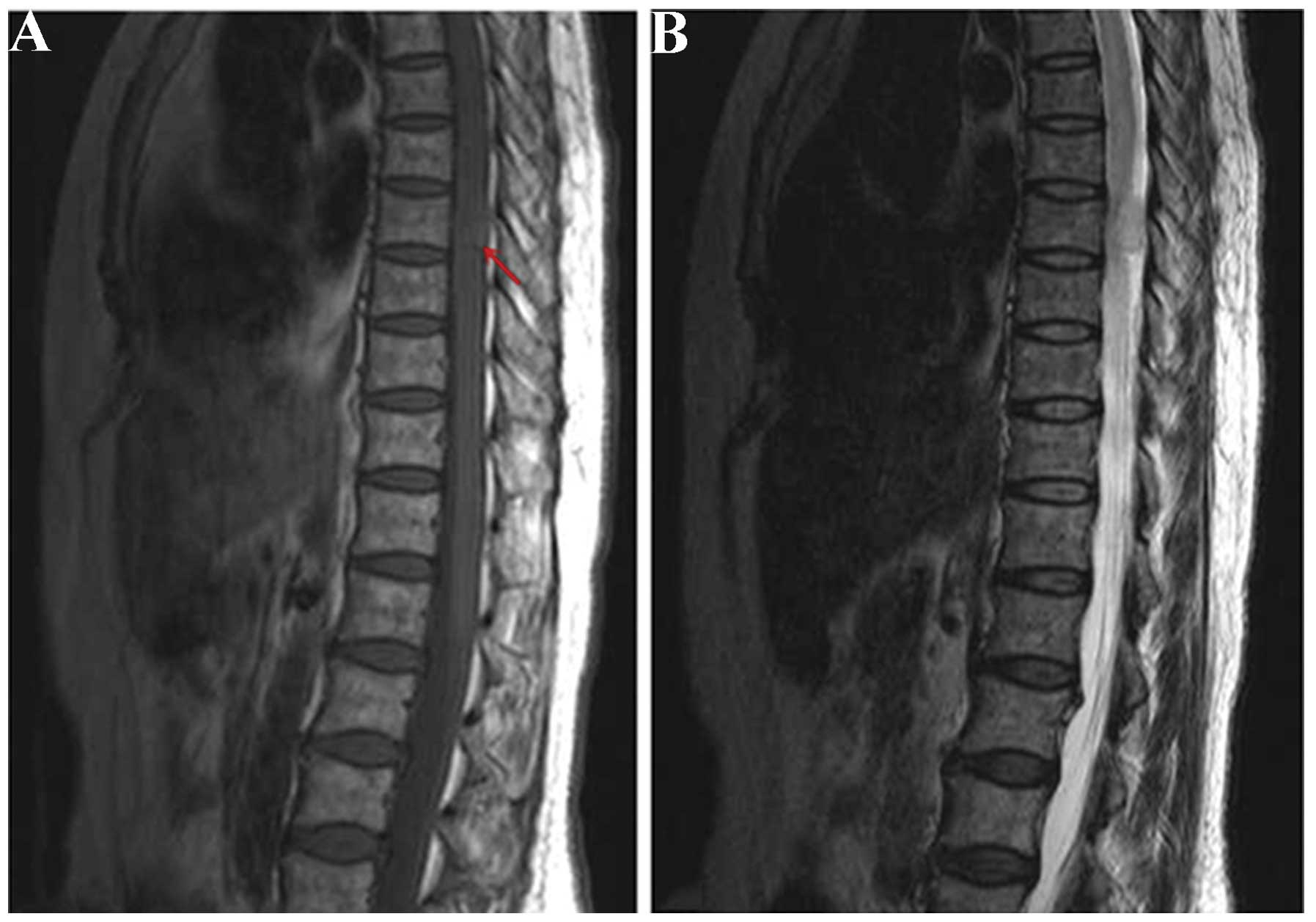
was performed to 90° in each lower extremity. Thoracic MRI
(Magnetom Symphony; Siemens, Munich, Germany) revealed an ovoid,
intradural, extramedullary mass, 2 cm in length and 1 cm in
diameter, at the T8 level. The tumor was isointense with the spinal
cord on T1-weighted images and slightly hyperintense on T2-weighted
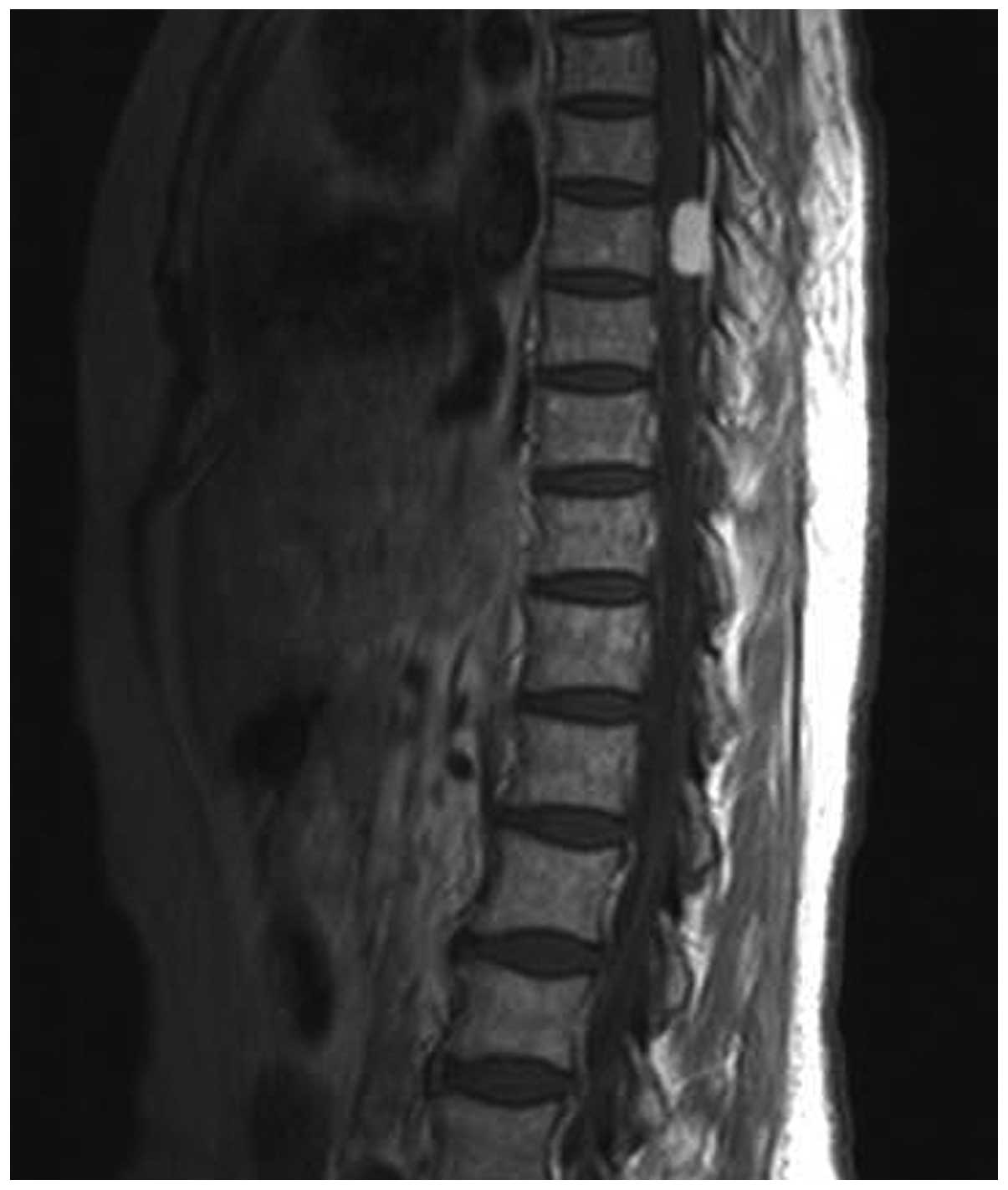
images (Fig. 1A and B). The tumor
showed markedly homogeneous enhancement on contrast-enhanced
T1-weighted images (Fig. 2). A
pre-operative diagnosis of meningioma was considered due to the MRI
features. Further examinations, including routine blood
[hemoglobin, 12 g/l (normal range, 11–16 g/l); red blood cell
count, 3.63×1012/l (normal range,
3.5–5.5×1012/l); white blood cell count, 4,000 cells/ml
(normal range, 4,000–10,000 cells/ml); platelet count, 1,780
cells/ml (normal range, 1,000-3,000 cells/ml); glucose level, 5.75
mmol/l (normal range, 3.9–6.1 mmol/l)], coagulation function
[prothrombin time, 13.4 sec (normal range, 10.5–14.0 sec);
activated partial thromboplastin time, 30.5 sec (normal range,
23.5–36.0 sec); thrombin time, 15.8 sec (14.0–21 sec);
international normalized ratio, 0.9 (normal range, 0.8–1.2)], serum
electrolyte [Na+, 142.6 mmol/l (normal range, 137–147
mmol/l); K+, 4.06 mmol/l (normal range, 3.5–5.3 mmol/l);
Mg2+, 0.92 mmol/l (normal range, 0.64–1.25 mmol/l);
Cl−, 108 mmol/l (normal range, 99–110 mmol/l);
Ca2+, 2.04 mmol/l (normal range, 2.03–2.67 mmol/l)],
electrocardiogram [heart rate, 68 beats per min (normal range,
60–100 beats per min)] and lung function tests [forced vital
capacity (FVC), 2,680 ml (normal range, >2400ml); forced
expiratory volume in 1 sec (FEV1), 2,270 ml (normal range,
>2,000ml); FEV1/FVC ratio, 84% (normal range, >83%); peak
expiratory flow rate, 5.92 l/sec (normla range, 5.5 l/sec)], were
all within normal limits. The patient underwent a T7-T8
laminectomy. Upon completion of the exposure of the dural sac, a
1×1.5×2-cm3 ovoid, well-circumscribed mass was
identified, densely attached to the inner surface of the dura
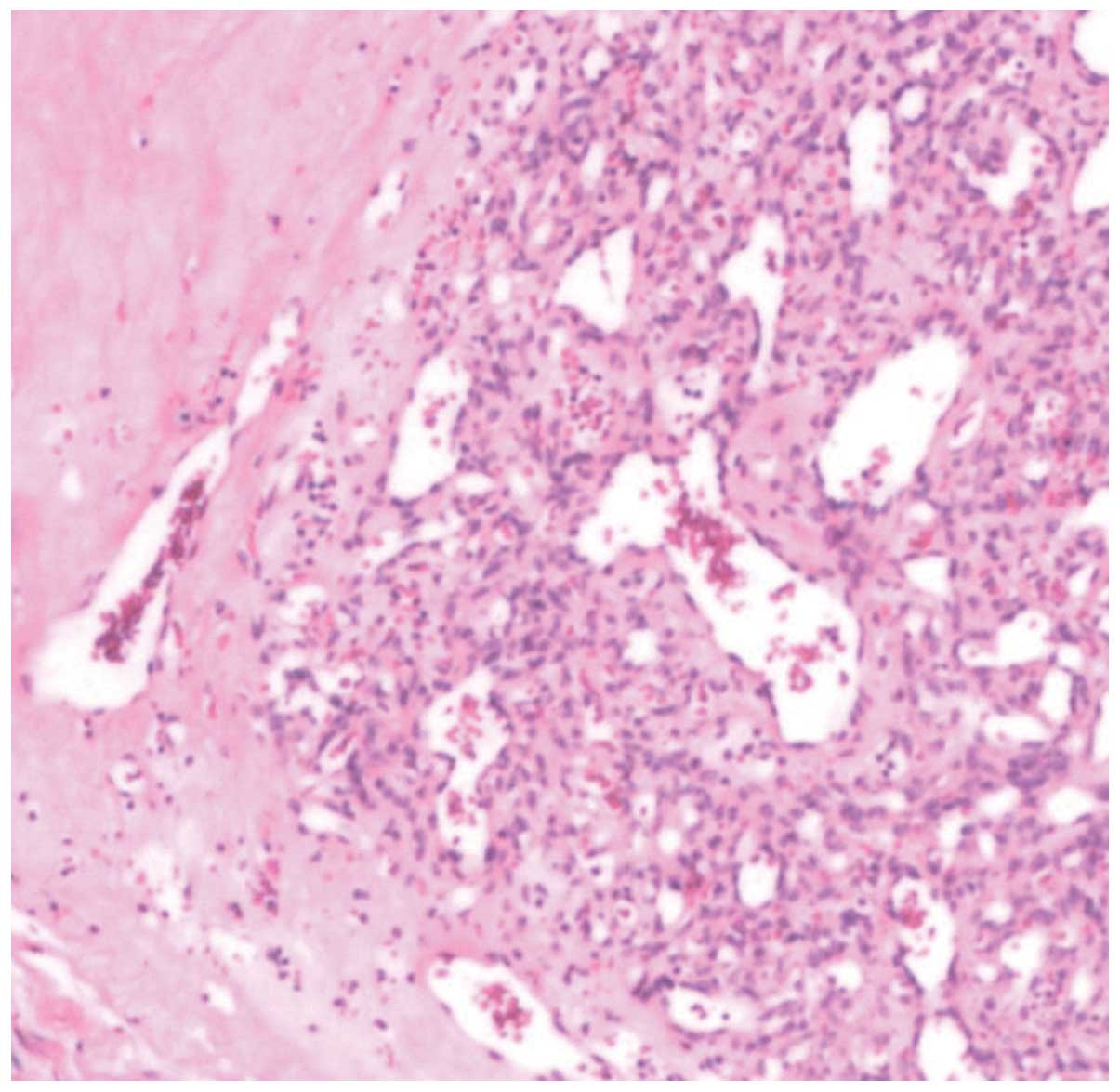
matter. The tumor was completely resected. Resected tissue
speciments were formalin-fixed, paraffin-embedded and cut into 4-µm
sections. Histopathological examinations using hematoxylin and
eosin staining (Sinopharm Chemical Reagent Co., Ltd., Shanghai,
China) revealed that the tumor exhibited the typical histological
findings of a capillary hemangioma, as it was comprised of a
proliferation of capillary-sized vessels (Fig. 3).
Follow-up
The patient was discharged on the 14th
post-operative day following an uneventful recovery. After the
surgery, the patient experienced significant relief from the
backache. After 2 months, sensation and reflexes of the knee and
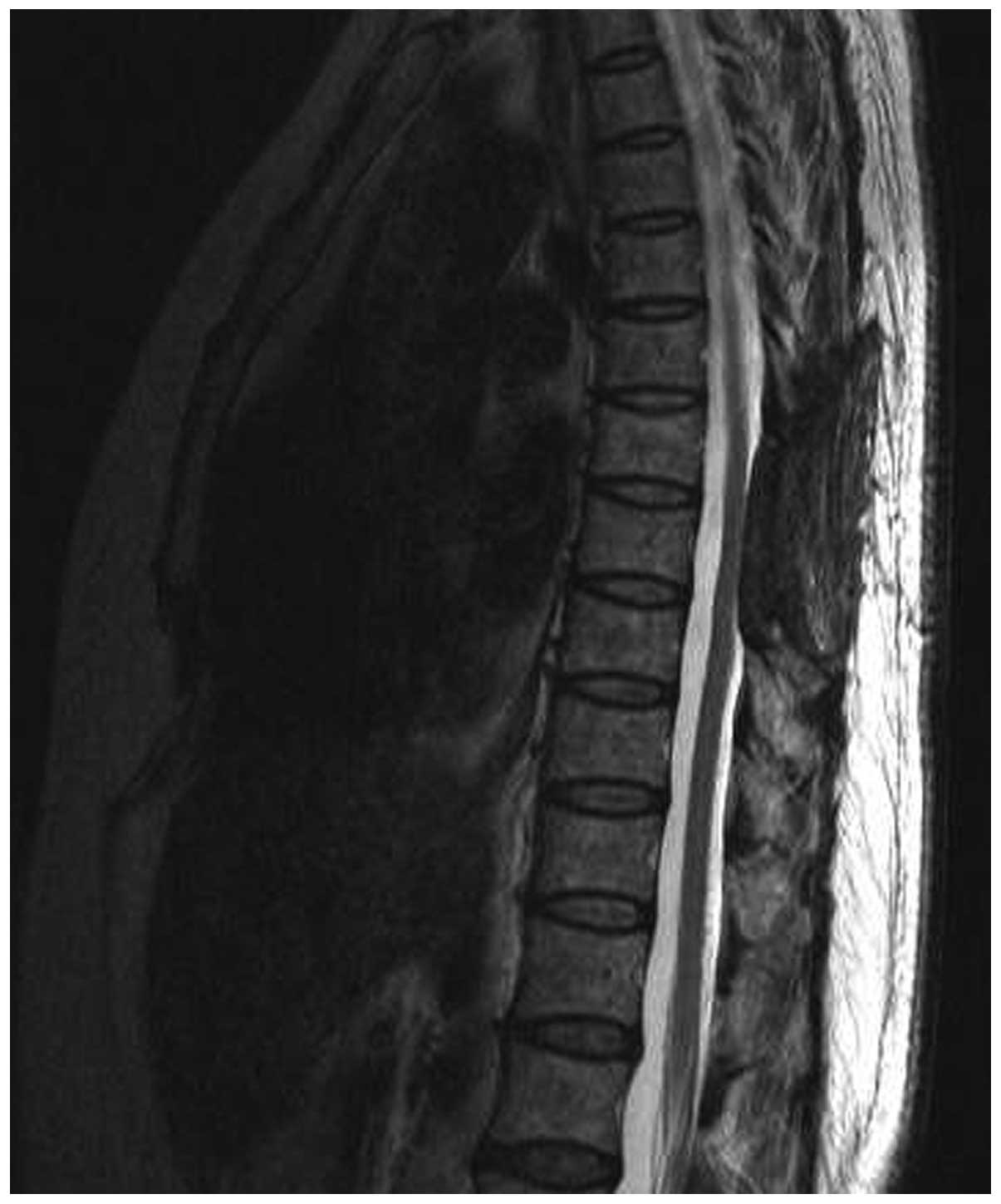
ankle were normal. After 2 years of post-operative follow-up, no
evidence of a recurrent tumor was evident on T2-weighted images
(Fig. 4). The patient is currently
managed with close clinical and radiological follow-up.
Discussion
Capillary hemangioma is a common, benign soft-tissue
tumor that occurs in the skin or mucosa of the head and neck, and
is occasionally located at the intradural extramedullary space
(6). To the best of our knowledge,
>20 cases of intradural extramedullary capillary hemangioma have
been reported (2,7). Based on findings from a previous study,
the blood vessels of spinal intradural capillary hemangioma may
arise from the inner surface of the dura, the pial surface of the
spinal cord or the nerve roots (7).
In the present case, it was found that the inner surface of the
dura was the site of origin. When the tumor is small, patients
often present with no clear clinical symptoms. With the gradual
growth of the tumor, patients present with different symptoms, such
as pain, numbness of limb, lower limbs hypesthesia and other
neurological symptoms, according to the tumor size and location
(7).
Imaging examinations, particularly MRI, are useful
and effective tools in the evaluation of intradural extramedullary
tumors. According to the study by Shin et al, the MRI
findings of spinal capillary hemangiomas show isointensity with the
spinal cord on T1-weighted images and hyperintensity with the
spinal cord on T2-weighted images (8). Choi et al presented the MRI
results of 3 patients and showed tumor hyperintensity on
T2-weighted images and isointensity relative to the spinal cord on
T1-weighted images (7). The MRI
results of the present case were in agreement with these previous
observations.
The differential diagnosis for spinal intradural
capillary hemangioma includes a number of tumors, including
neurinomas, meningiomas, hemangiopericytomas,
hemangioendotheliomas, schwannnomas, cavernous angiomas,
angiolipomas, solitary fibrous tumor paragangliomas, lymphomas,
sarcoidosis, ependymomas and metastasis. MRI plays an important
role in differentiating between these tumors. For example,
meningiomas show isointensity or slight hypointensity on
T1-weighted images, and isointensity or slight hyperintensity on
T2-weighted images (7). On MRI,
necrosis or cystic changes are frequently observed within
neurimomas (7). A heterogeneous salt
and pepper-like appearance of vascular signal voids may be present
in paraganglioma on MRI (7).
Therefore, the clinical utility of MRI should be fully accepted in
the evaluation of intradural extramedullary masses.
A hemangioma may be classified as a capillary,
cavernous or mixed hemangioma. It is possible to differentiate
capillary hemangioma from other hemangioma by means of histological
examination. The classic feature of capillary hemangiomas is a
tumor composed of tightly packed capillary-sized vessels lined by a
single layer of endothelial cells on microscopy (6). Therefore, the presence of different
histological examination features is useful and effective in
distinguishing capillary hemangioma from other tumors.
The treatment of choice for intradural
extramedullary capillary hemangioma is complete surgical excision.
In the present study, a laminectomy and durotomy were performed to
access to the intradural space, and then a total tumor resection
was performed. Due to the excessive vascularity of intradural
extramedullary capillary hemangioma, a complete tumor resection
should be performed, and a piece and piece resection should be
avoided (6). We believe that, as
bleeding of the intradural extramedullary capillary hemangioma may
cause acute spinal cord compression, surgery should be performed
immediately after an intradural extramedullary capillary hemangioma
is found. Other treatments, including radiation therapy and
embolization methods, have not been investigated in the therapy of
intradural extramedullary capillary hemangioma in previously
reported cases (6). Tumor recurrence
has not been reported in previous studies, and no recurrence was
found in the present case. Roncaroli et al (5) reported the cases of 2 patients who
underwent complete resections of spinal capillary hemangiomas, with
no recurrence 10 years after surgery. However, due to the potential
for recurrence, long-term follow-up is required in such cases.
In conclusion, the current study presents an
extremely rare case of spinal intradural capillary hemangioma in a
59-year-old woman. Surgical intervention was successfully performed
and the patient's neurological symptoms improved. This case
suggests that capillary hemangioma should be included in the
differential diagnosis when an ovoid, well-demarcated mass is
observed in the spinal intradural space, and that surgical
treatment should be strongly considered in such cases.
References
|
1
|
Tokuda Y, Uozumi T, Sakoda K, Yamada K,
Yamanaka M, Nomura S and Hamasaki T: Giant congenital capillary
hemangioma of pericranium-case report. Neurol Med Chir (Tokyo).
30:1029–1033. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hida K, Tada M, Iwasaki Y and Abe H:
Intramedullary disseminated capillary haemangioma with localized
spinal cord swelling: Case report. Neurosurgery. 33:1099–1101.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Holtzman RN, Brisson PM, Pearl RE and
Gruber ML: Lobular capillary hemangioma of the cauda equina. Case
report. J Neurosurg. 90(2 Suppl): 239–241. 1999.PubMed/NCBI
|
|
4
|
Roncaroli F, Scheitauer BW and Krauss WE:
Hemangioma of spinal nerve root. J Neurosurg. 91(2 Suppl): 175–180.
1999.PubMed/NCBI
|
|
5
|
Roncaroli F, Scheitauer BW and Krauss WE:
Capillary hemangioma of the spinal cord. Report of four cases. J
Neurosurg. 93(1 Suppl): 148–151. 2000.PubMed/NCBI
|
|
6
|
Nowak DA and Widennka DC: Spinal
intradural capillary haemangioma: A review. Eur Spine J.
10:464–472. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Choi BY, Chang KH, Choe G, Han MH, Park
SW, Yu IK, Park YH and Kim HJ: Spinal intradural extramedullary
capillary hemangioma: MR imaging findings. AJNR Am J Neuroradiol.
22:799–802. 2001.PubMed/NCBI
|
|
8
|
Shin JH, Lee HK, Jeon SR and Park SH:
Spinal intradural capillary hemangioma: MR findings. AJNR Am J
Neuroradiol. 21:954–956. 2000.PubMed/NCBI
|