Introduction
Thymectomy was considered as the only curative
treatment for patients with resectable thymoma (1). Landreneau et al introduced
video-assisted thoracoscopic surgery (VATS) thymectomy in 1992
(2).
Double-lumen endotracheal tube (DLET) anesthesia is
the routine method for VATS thymectomy, which may frequently result
in more complications (3). In rare
circumstances, use of the single-lumen endotracheal tube (SLET) is
mandatory, such as the translocation of the DLET, structural
malformations, and tracheostenosis (4). Double-lung ventilation with SLET
intubation potentially offers improved visualization for certain
thoracoscopic procedures (5).
In the present study, we retrospectively examined
SLET anaesthesia with CO2 insufflation artificial
pneumothorax in VATS thymectomy to determine whether patients
benefit from this type of surgery.
Patients and methods
Patients
In total, 19 patients with bulky thymoma underwent
thoracoscopic resection assisted with artificial pneumothorax via
CO2 insufflation at the Xuzhou Central Hospital
(Jiangsu, China), between January 2014 and April 2015 by the same
surgeon. The study was approved by the Institutional Review Board
of Xuzhou Central Hospital. Informed consent regarding
participation was received from the patients.
Methods
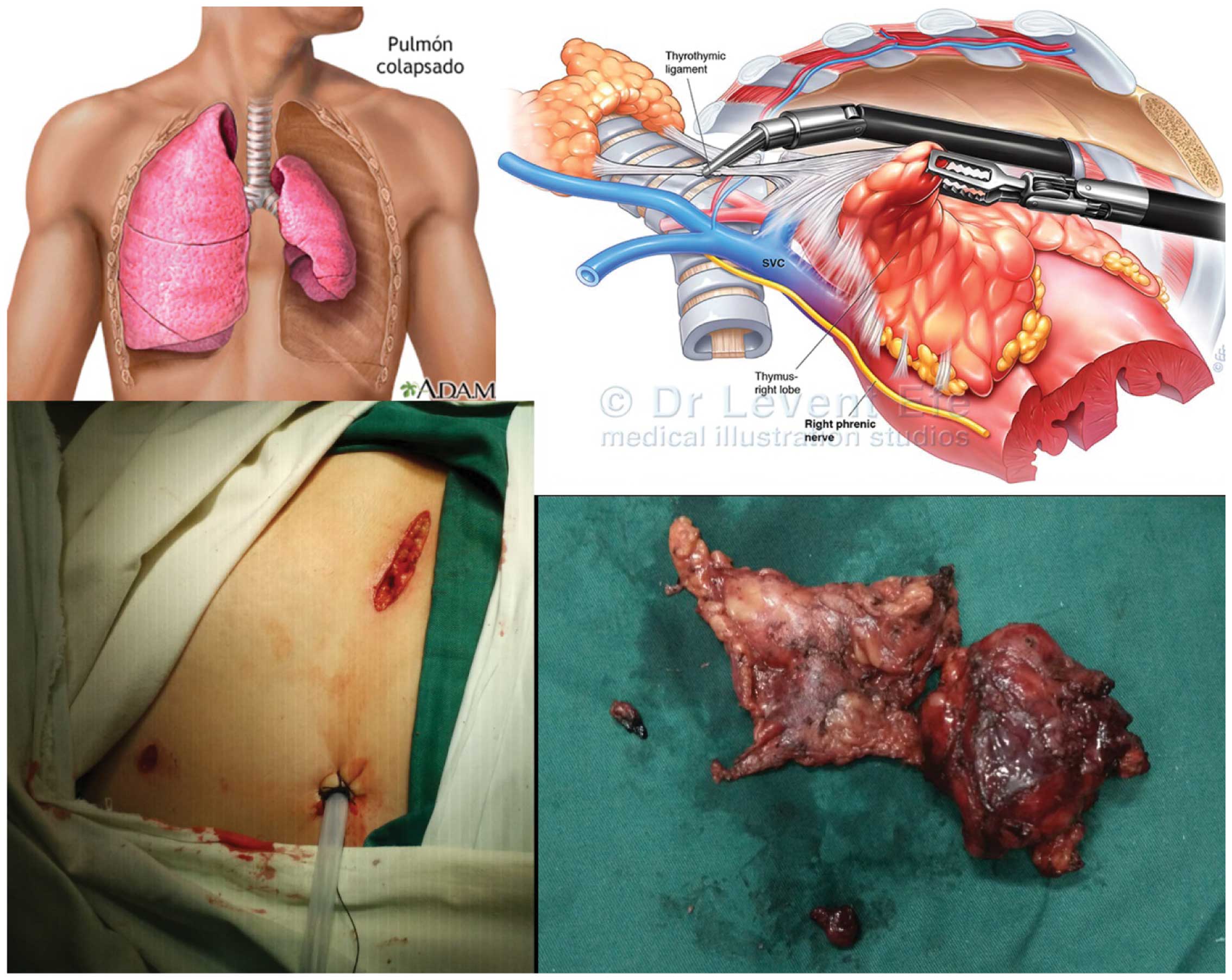
During the procedure, the patients were placed in a
supine position with double-lung ventilation. Firstly, the
thoracoscopy was placed into the thorax for exploration, and
pleural adhesions were separated carefully using an ultrasonic
scalpel (Johnson & Johnson, NY, USA). Artificial CO2
pneumothorax (CO2 pressure = 8 mmHg) was then
established. Three to four ports were made with respect to the
location and the size of the lesion determined by CT (Fig. 1). Generally, the thoracoscopic
thymectomy was performed following the procedures detailed by other
surgeons previously (6). The
dissection was initiated with the inferior thymic poles carefully
mobilized. Subsequently, the anterior mediastinal tissue was swept
along the pericardium and the retrosternum. The innominate vein was
located at the junction with the superior vena cava, and dissection
continued until the thymic vein was located, which was then doubly
clipped. The operation was completed by dissecting directly along
the left pleura to avoid injury to the left phrenic nerve. One of
the manipulating ports was enlarged appropriately for the
extraction of thymus, and a drainage tube was placed
unilaterally.
Results
The operations were performed with unilateral or
bilateral thoracic incisions via single-lumen endotracheal
intubation and double-lung ventilation. This approach provided
excellent exposure of the thoracic cavity and reliable control of
the neuro-vascular structures in the anterior mediastinum. This was
crucial for the extended resection of malignant thymoma. The
operation time was 140.0±51.4 min without conversion to thoracotomy
or sternotomy. The pathological diagnosis was confirmed by
immunohistochemistry resulting in, 5 cases of thymus lipomyoma, 1
case of thymus hyperplasia, 1 case of thymus cyst, 2 cases of type
AB thymoma, 4 cases of type B1 thymoma, 4 cases of type B3 thymoma,
and 2 cases of thymic carcinoma. Furthermore, there were no
complications such as recurrent laryngeal nerve injury, phrenic
nerve injury, pulmonary infection or atelectasis. The patients had
a hospital stay of 5.0±3.0 days.
Discussion
The application of VATS thymectomy was extended with
advances in techniques. VATS thymectomy is optimal compared with
the open approach for early-stage thymoma patients (Masaoka staging
I–II), which indicated shorter postoperative hospital length of
stay (5.26 vs. 8.32 days), less blood loss (114.74 vs. 194.51 ml)
and shorter duration of postoperative drainage (3.87 vs. 5.22
days), respectively (6). Similarly,
it was reported that VATS thymectomy showed less postoperative
complications with similar 5-year overall survival, 5-year
disease-free survival and recurrence rates (7,8). The
superior poles of the thymus may be exposed by CO2
insufflation and neck flexion, without cervical incision (9). In addition, Suda et al reported
that single-port trans-subxiphoid robotic thymectomy assisted with
CO2 gas injection at 8 mmHg provides a good operative
view in the neck region and makes verification of the phrenic nerve
easy (10). Furthermore, Wu et
al reported that uniportal VATS for mediastinal tumour
resection including extended thymectomy was a promising and safe
technique (11).
Notably, the size of the thymoma was not an absolute
contraindication for VATS, because the thymoma with maximal
diameter of ~13 cm was completed through the VATS approach, as
previously reported (6). Furthermore,
DLET and one-lung ventilation may result in a variety of
complications, including hoarseness, hypoxaemia, tracheobronchial
injury, vocal cord injury and re-expansion or oxidative stress
(12,13). Therefore, CO2 infusion
artificial pneumothorax with double-lung ventilation may be a better
option for VATS (4). Of note the
artificial pneumothorax is not suitable for all cases, and DLET
should be prepared in case the need of single-lung ventilation
during the surgery, such as severe pleural adhesion to avoid
pleural tear and bleeding, is required. In addition, the artificial
pneumothorax with CO2 insufflation may result in
deteriorative changes, such as circulatory failure, ventricular
arrhythmias and contralateral pneumothorax. This should be
considered during the surgery assisted with artificial
pneumothorax. However, a moderate-to-low intra-abdominal pressure
>12 mmHg can assist to limit the extent of the
pathophysiological changes (14).
Brock et al reported that one-lung ventilation via a
double-lumen endotracheal tube is safe and convenient for VATS
surgery (15). In conclusion, our
initial experience of 19 cases indicated that VATS thymectomy
assisted with artificial pneumothorax via single-lumen endotracheal
intubation and two-lung ventilation is safe and feasible, and
constitutes a method that may be utilized for patients with other
retrosternal tumors.
Acknowledgements
The simulated graphs of pneumothorax and VATS
procedure were obtained from https://images.search.yahoo.com, for which we extend
thanks to the original authors.
References
|
1
|
Detterbeck FC and Zeeshan A: Thymoma:
current diagnosis and treatment. Chin Med J (Engl). 126:2186–2191.
2013.PubMed/NCBI
|
|
2
|
Landreneau RJ, Dowling RD, Castillo WM and
Ferson PF: Thoracoscopic resection of an anterior mediastinal
tumor. Ann Thorac Surg. 54:142–144. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cerfolio RJ, Bryant AS, Sheils TM, Bass CS
and Bartolucci AA: Video-assisted thoracoscopic surgery using
single-lumen endotracheal tube anesthesia. Chest. 126:281–285.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhang R, Liu S, Sun H, Liu X, Wang Z, Qin
J, Hua X and Li Y: The application of single-lumen endotracheal
tube anaesthesia with artificial pneumothorax in
thoracolaparoscopic oesophagectomy. Interact Cardiovasc Thorac
Surg. 19:308–310. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cheng YL, Huang TW, Lee SC, Wu CT, Chen
JC, Chang H and Tzao C: Video-assisted thoracoscopic surgery using
single-lumen endotracheal tube anaesthesia in primary spontaneous
pneumothorax. Respirology. 15:855–859. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yuan ZY, Cheng GY, Sun KL, Mao YS, Li J,
Wang YG, Wang DL, Gao SG, Xue Q, Huang JF, et al: Comparative study
of video-assisted thoracic surgery versus open thymectomy for
thymoma in one single center. J Thorac Dis. 6:726–733.
2014.PubMed/NCBI
|
|
7
|
Manoly I, Whistance RN, Sreekumar R,
Khawaja S, Horton JM, Khan AZ, Casali G, Thorpe JA, Amer K and Woo
E: Early and mid-term outcomes of trans-sternal and video-assisted
thoracoscopic surgery for thymoma. Eur J Cardiothorac Surg.
45:e187–e193. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu TJ, Lin MW, Hsieh MS, Kao MW, Chen KC,
Chang CC, Kuo SW, Huang PM, Hsu HH, Chen JS, et al: Video-assisted
thoracoscopic surgical thymectomy to treat early thymoma: a
comparison with the conventional transsternal approach. Ann Surg
Oncol. 21:322–328. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lee CY, Kim DJ, Lee JG, Park IK, Bae MK
and Chung KY: Bilateral video-assisted thoracoscopic thymectomy has
a surgical extent similar to that of transsternal extended
thymectomy with more favorable early surgical outcomes for
myasthenia gravis patients. Surg Endosc. 25:849–854. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Suda T, Tochii D, Tochii S and Takagi Y:
Trans-subxiphoid robotic thymectomy. Interact Cardiovasc Thorac
Surg. 20:669–671. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wu CF, Gonzalez-Rivas D, Wen CT, Liu YH,
Wu YC, Chao YK, Heish MJ, Wu CY and Chen WH: Single-port
video-assisted thoracoscopic mediastinal tumour resection. Interact
Cardiovasc Thorac Surg. 21:644–649. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Misthos P, Katsaragakis S, Milingos N,
Kakaris S, Sepsas E, Athanassiadi K, Theodorou D and Skottis I:
Postresectional pulmonary oxidative stress in lung cancer patients.
The role of one-lung ventilation. Eur J Cardiothorac Surg.
27:379–382; discussion 382–383. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Knoll H, Ziegeler S, Schreiber JU,
Buchinger H, Bialas P, Semyonov K, Graeter T and Mencke T: Airway
injuries after one-lung ventilation: a comparison between
double-lumen tube and endobronchial blocker: a randomized,
prospective, controlled trial. Anesthesiology. 105:471–477. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gutt CN, Oniu T, Mehrabi A, Schemmer P,
Kashfi A, Kraus T and Büchler MW: Circulatory and respiratory
complications of carbon dioxide insufflation. Dig Surg. 21:95–105.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Brock H, Rieger R, Gabriel C, Pölz W,
Moosbauer W and Necek S: Haemodynamic changes during thoracoscopic
surgery the effects of one-lung ventilation compared with carbon
dioxide insufflation. Anaesthesia. 55:10–16. 2000. View Article : Google Scholar : PubMed/NCBI
|