Introduction
Intracranial hemangioendothelioma (HE) is a rare
borderline angiomatous tumor with invasive behavior and an
intermediate level of malignancy between that of benign hemangioma
and high-grade malignant angiosarcoma (1). Intracranial epithelioid HE accounts for
<0.02% of all primary intracranial tumors, and the tumor usually
develops in the dura mater, cranium and brain. HE involving
intracranial structures occasionally results in serious local
compressive symptoms, including cranial nerve palsy or a
potentially fatal increase in intracranial pressure. Despite the
low proliferation indices, the clinical course of intracranial HE
can be complicated (2). A total
resection is essential where possible, otherwise radiotherapy
and/or chemotherapy are required (2).
Pre-operative embolization of the feeding-artery is recommended. As
intracranial HE is seldom encountered in clinical practice,
considerable confusion exists with regard to its correct diagnosis
and management. To date, numerous studies have focused on the
histogenetic, histopathological and clinical characteristics of HE
(2–11); by contrast, there have been only
scattered case studies that have described the imaging findings
(12,13). The purpose of the present study was to
analyze the computed tomography (CT) and magnetic resonance imaging
(MRI) characteristics of intracranial HE, and to describe the
pathological features.
Patients and methods
Patients
This study was approved by the Ethical Review
Committee of Huashan Hospital, Fudan University Medical School
(Shanghai, China), and the requirement for patient consent was
waived for this retrospective study. A retrospective review was
performed on 7 patients with surgically and histologically proven
HE at Huashan Hospital (Shanghai, China) between January 2008 and
December 2013. The patients included 1 male and 6 females, with
ages ranging from 13 to 62 years and a median age of 51 years at
the initial diagnosis.
CT
CT examinations were performed using a CT machine
(Somatom Emotion, Siemens, Erlangen, Germany; or LightSpeed, GE
Medical Systems, Milwaukee, WI, USA). A conventional axial scan
(120 kV, 180 mA, 512×512 matrix and a section thickness of 10 mm)
was performed in 3 cases.
MRI
MRI was performed in all 7 patients. All MRI images
were acquired using a 1.5T MRI unit (Signa Excite HD Twinspeed; GE
Medical Systems) or a 3T MR scanner (Signa Excite GEMSOC01, GE
Medical Systems) with a single-channel head coil. Sagittal and
axial, T1-weighted [400-msec repetition time (TR)/15-msec echo time
(TE)] spin-echo (SE) images; axial, T2-weighted (3,000-msec
TR/119-msec TE) fast SE images; and fluid attenuated inversion
recovery (FLAIR; 8,500-msec TR/138-msec TE) images were obtained
for unenhanced MRI; such images were observed using a field of view
(FOV) of 25–35 cm, an image matrix of 256×128 or 256×256, and a
section thickness of 8 mm with a 2-mm gap. Diffusion-weighted (DW)
MRI studies were acquired in the axial plane using a single-shot SE
echo planar imaging sequence with b values of 0 and 1,000
sec/mm2 in five orthogonal directions. Contrast-enhanced
sagittal and axial, T1-weighted, and SE MRI images were obtained
after the administration of gadolinium diethylenetriamine
pentaacetic acid (0.1 mmol/kg body weight; Magnevist, Berlex
Laboratories, Berlin, Germany). Intracranial time-of-flight MR
angiography (MRA) was performed in 1 case using the following
parameters: TR/TE, 20–25/3-7 msec; flip angle, 20°; FOV, 178×200
mm; matrix, 256×196; slice thickness, 1.2 mm (0.6-mm overlap with
the adjacent section); and section slices, 140.
Data analysis
The pre-treatment CT and MRI studies from the
initial presentation were reviewed, and tumor location, size,
shape, attenuation, presence of calcification, signal intensity,
enhancement characteristics, peritumoral edema and associated
hydrocephalus were recorded. Clinical data, such as symptoms and
their duration, treatment and pathological results, were also
reviewed.
Immunohistochemical staining
The tumor tissues were fixed in 10% formalin
(Beijing Solarbio Science & Technology Co., Ltd., Beijing,
China) and paraffin (Shanghai Hualing Health Machinery Plant,
Shanghai, China) embedded for routine processing. For
immunohistochemistry, 5-µm thick sections were deparaffinized using
xylene (Wuxi Yasheng Chemical Co., Ltd. Wuxi, China), rehydrated
using a graded ethanol series (100, 95, 90, 80 and 70%) and treated
with 0.3% H2O2 to block endogenous peroxidase
activity. The sections were then incubated with 10 mmol/l citrate
buffer (pH 6.0; Beijing Solarbio Science & Technology Co.,
Ltd.) at 121°C for 20 min in an autoclave for antigen retrieval.
After rinsing with phosphate-buffered saline (PBS; Beijing Solarbio
Science & Technology Co., Ltd.), the sections were incubated
with 10% goat serum (Gibco; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA) for 1 h at room temperature to block any
nonspecific reactions. The sections were then incubated overnight at
4°C with mouse anti-human monoclonal glial fibrillary acidic
protein (dilution, 1:10; cat. no. M0761), mouse anti-human
monoclonal cluster of differentiation (CD)31 (dilution, 1:100; cat.
no. IR610), mouse anti-human monoclonal CD34 (dilution, 1:4; cat.
no. IR632), rabbit anti-human polyclonal factor VIII (dilution,
1:100; cat. no. A0082), mouse anti-human monoclonal smooth muscle
actin (dilution, 1:400; cat. no. IR611) and mouse anti-human
monoclonal vimentin (dilution, 1:100; cat. no. IR630) antibodies.
The diluted primary antibodies were obtained from Dako (Glostrup,
Denmark). Negative control slides were also processed in parallel
using a nonspecific immunoglobulin IgG (cat. no. HAB5500149;
Sigma-Aldrich, St. Louis, MO, USA) at the same concentration as the
primary antibody. Detection of all antibody reactions was performed
using a streptavidin peroxidase detection kit (Dako) according to
the manufacturer's protocol. After rinsing in PBS, the peroxidase
reaction was visualized by incubating the sections with
diaminobenzidine tetrahydrochloride in 0.05 mol/l Tris buffer (pH
7.6) containing 0.03% H2O2. After washing in
water three times, the sections were counterstained with
hematoxylin (Beijing Solarbio Science & Technology Co., Ltd.),
dehydrated, cleared and coverslipped. The slides wer then
visualized under an optical microscope (CX31; Olympus Corporation,
Tokyo, Japan).
Results
The main clinical manifestations included headache
and dizziness (3 cases), paroxysmal dysesthesia and paresis of the
right limbs (1 case), tinnitus and blurred vision (1 case), and
right orbital eminence (1 case). Furthermore, 1 patient was
asymptomatic and the lesion was incidentally discovered. Symptom
duration ranged between 4 months and 10 years, with a mean of 2
years.
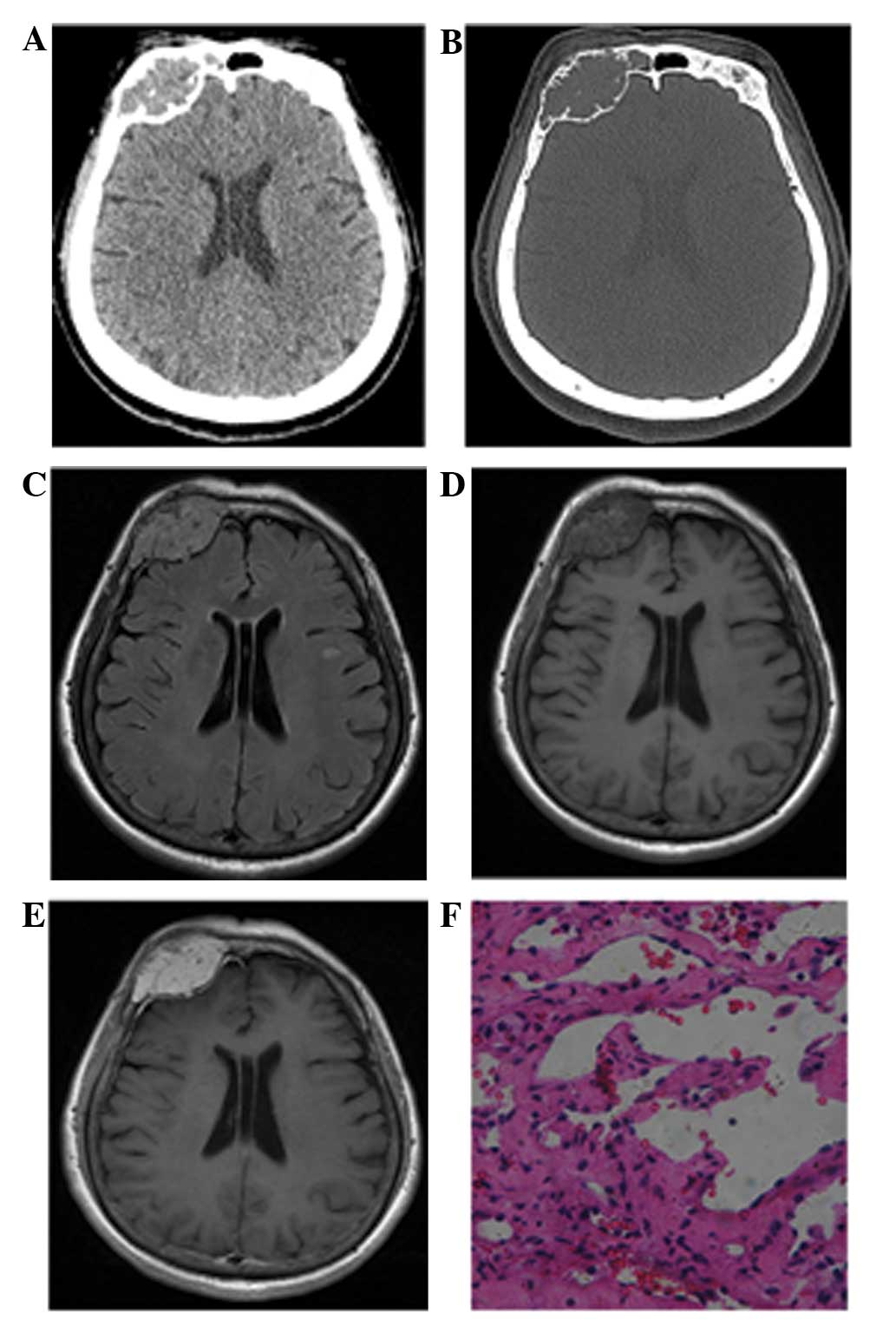
The neuroradiological findings of the HEs are
summarized in Table I. While 2 cases
exhibited lesions in the right side of the skull, 1 in the frontal
bone (Fig. 1) and the other in the
parietal bone, another 2 cases presented with lesions in the
tentorium. Moreover, 1 case presented with a lesion in the cerebral
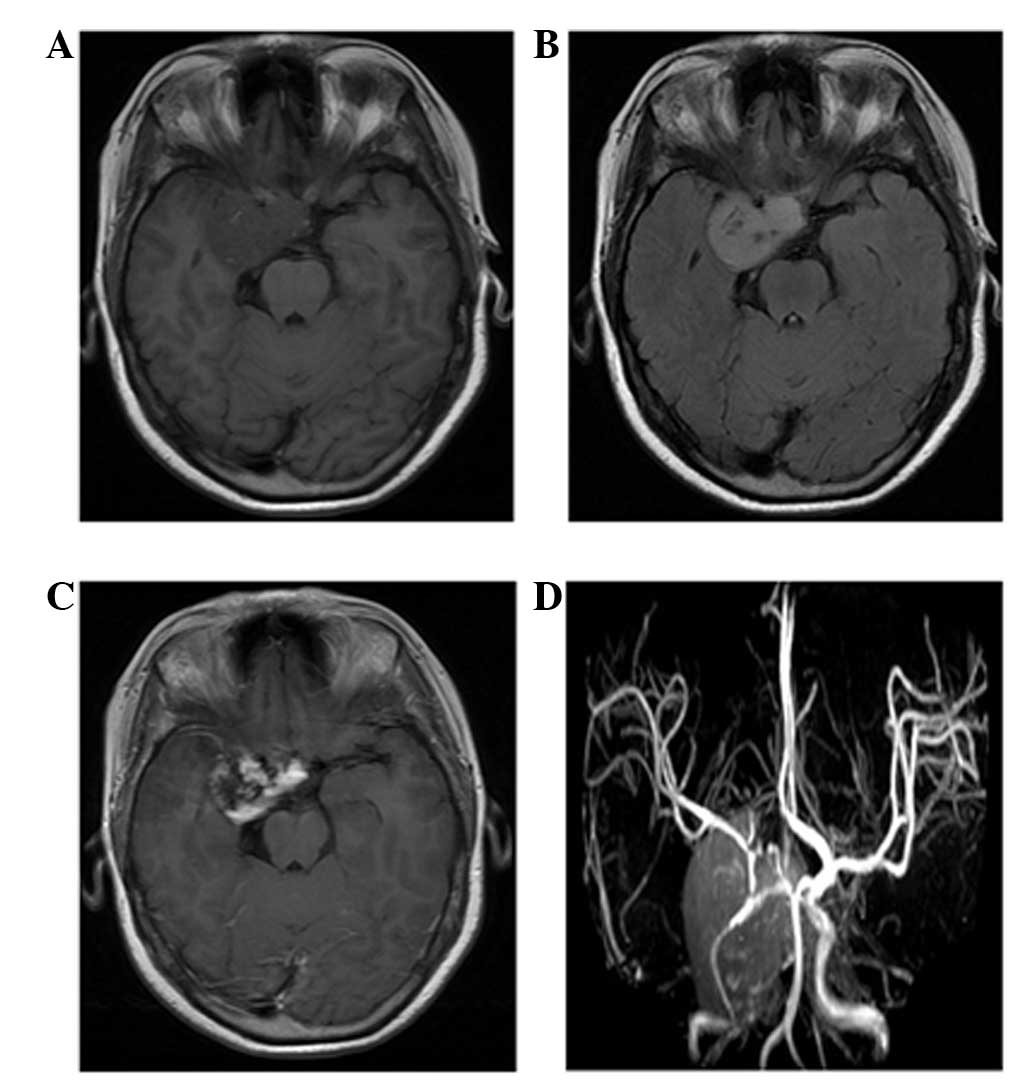
falx, 1 case with a lesion in the right cavernous sinus and 1 case
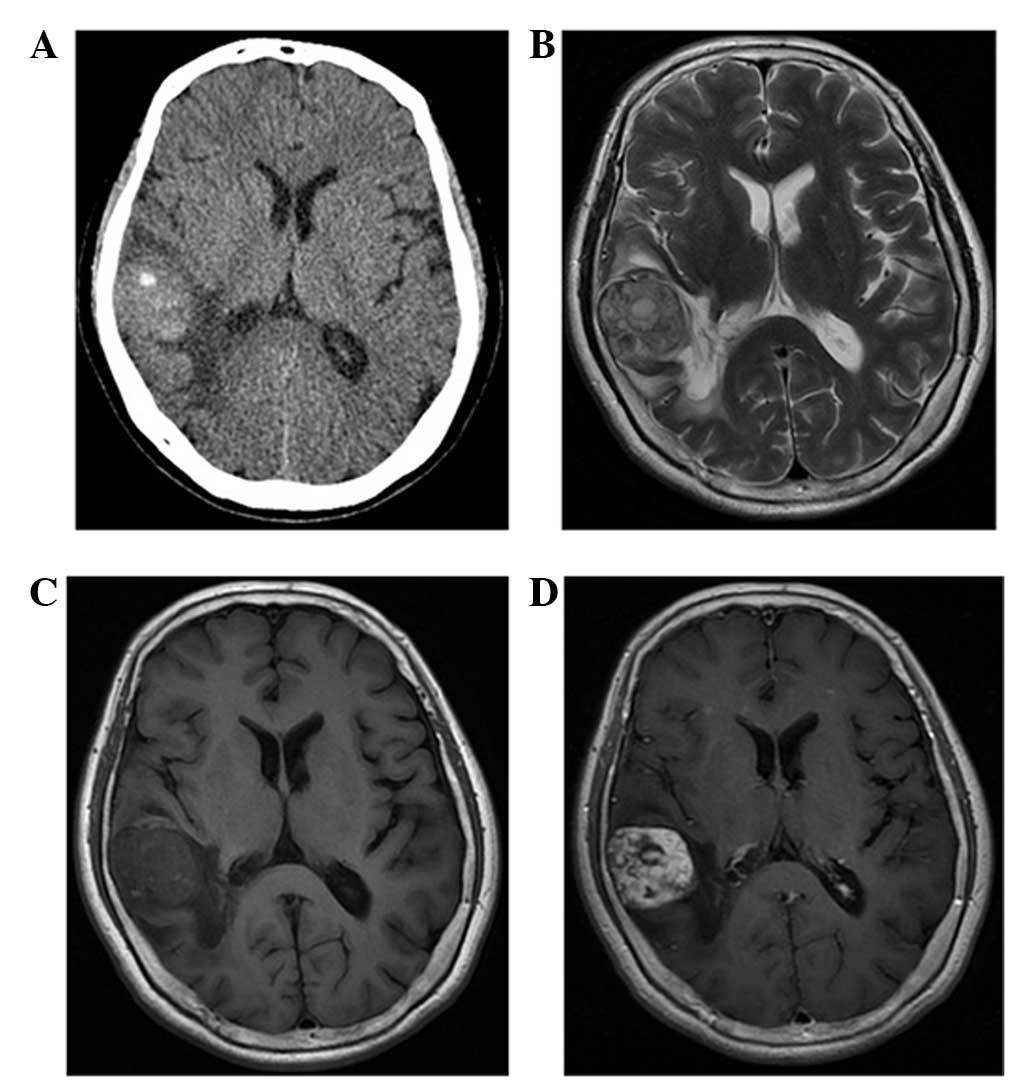
with a lesion in the right temporal lobe (Fig. 2). CT and MRI results showed that 2
masses were round (Fig. 1), whereas
the remaining 5 tumors were lobulated. The total diameter ranged
between 2.1 and 5.3 cm. The 3 patients who underwent CT presented
predominantly with isoattenuation, with radiodensity values ranging
from 32–47 HU, and a dotted calcification was detected in 1 lesion
(Fig. 2A). The 2 lesions originating
from the skull showed local bone destruction and osteolysis. The
cortical bones were discontinuous with sclerotic margins, and
exhibited soft-tissue density and spine-like protuberances
(Fig. 1A). Moreover, 1 case occurred
in the right frontal bone and involved the superior edge of the
right orbit and frontal sinus.
 | Table I.Clinical and neuroradiological feature
in 7 cases of intracranial hemangioendotheliomas. |
Table I.
Clinical and neuroradiological feature
in 7 cases of intracranial hemangioendotheliomas.
| Case no. | Gender | Age, years | Histological
type | Location | Tumor size, mm | Morphology | CT attenuation | T1WI scattered
hyperintense | T2WI signal voids of
vessels | Honeycomb
enhancement | Peritumoral
edema |
|---|
| 1 | F | 56 | Epithelial | Right parietal
bone | 25×24×21 | Round-like |
| + | + | + | − |
| 2 | F | 51 | Epithelial | Tentorium
cerebelli | 50×49×48 | Lobulate | Isoattenuation | + | + | + | + |
| 3 | F | 57 | Epithelial | Right temporal
lobe | 37×30×39 | Lobulate | Isoattenuation | + | + | + | + |
| 4 | F | 62 | Retiform | Right frontal
bone | 50×24×49 | Round-like | Isoattenuation | + | + | + | − |
| 5 | F | 33 | Retiform | Right cavernous
sinus | 30×35×34 | Lobulate |
| + | + | + | − |
| 6 | F | 13 | Epithelial | Cerebral falx | 30×53×28 | Lobulate |
| + | + | + | + |
| 7 | M | 34 | Kaposi | Tentorium
cerebelli | 40×40×30 | Lobulate |
| + | + | + | + |
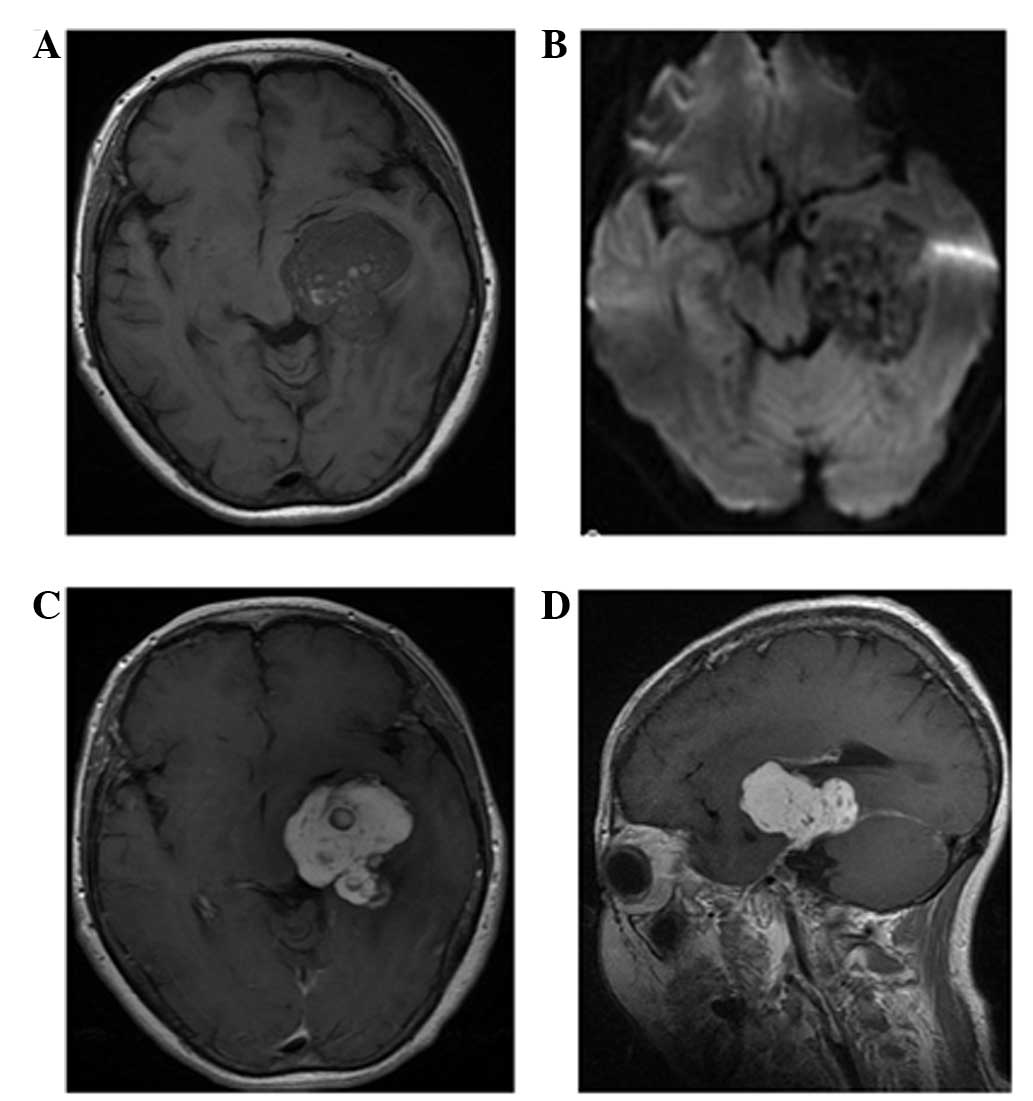
The MRI images of the 7 lesions were primarily
isointense (n=5) or mildly hypointense (n=2) compared with the gray
matter on T1-weighted images. All tumors were scattered
hyperintensely due to intratumoral hemorrhage (Figs. 1D, 2C,
3A and 4A). T2-weighted and FLAIR
images showed that all tumors were inhomogeneously hyperintense to
the cortex. Mild or moderate peritumoral edema was noted in 4
cases, whereas no evident edema signals were observed in the 2
cases with skull lesions and in the case with a lesion in the right
cavernous sinus (Fig. 4). The lesions
exhibited a lobulated and septated appearance due to the
coalescence of multiple high-signal nodules within the tumor
(Fig. 2B). The signal voids in the
vessels were also visible in all cases (Figs. 1C, 2B
and 4B). DW imaging (b=1,000) showed
that 6 tumors were hypointense, whereas 1 tumor was inhomogeneous
with high-low mixed signal compared with that of the white matter
(Fig. 3B).
Contrast-enhanced T1-weighted images showed contrast
enhancement in all tumors. All lesions exhibited inhomogeneous
enhancement consisting of multiple nodules with relatively
homogeneous enhancement compared with the surroundings in the early
stage; such nodules became hyperintense with delayed enhancement.
Additionally, 4 cases demonstrated a marked enhancement, called the
‘dural tail sign’ in the dura adjacent to the tumor. MRA also
revealed ectopic vessels in the basilar region in 1 case (Fig. 4C).
A total resection was performed in 5 patients,
whereas a partial resection was performed in the remaining 2
patients, including the case with the skull invading the dura.
Light microscopy revealed dense spindle and epithelioid cells with
abnormal angiogenesis in 4 cases (cases 1–3 and 6). Tubular
structures and spindle cell proliferation were also observed in
certain regions. An abnormal distribution of endothelial cells
within the lesion and a branching ‘netlike’ vascularization
extending into the reticular formation was observed in 2 cases
(cases 4 and 5). A single case (case 3) presented with endothelial
cells showing evident atypia and vacuoles. Moreover, another case
(case 7) exhibited loosely-arranged spindle-shaped tumor cells with
abundant cleft-like or cribriform small blood vessels in between,
but no evident nuclear atypia or mitoses. Thrombogenesis was also
observed in certain vascular proliferations (Fig. 1F). The immunohistochemistry results
and pathological diagnosis of the HEs are summarized in Table II.
 | Table II.Immunohistochemistry features and
pathological diagnosis of intracranial hemangioendothelioma. |
Table II.
Immunohistochemistry features and
pathological diagnosis of intracranial hemangioendothelioma.
| Case. no | Histological
type | CD34 | CD31 | FVIII | SMA | Vim |
|---|
| 1 | Epithelial | + | − | − | + | − |
| 2 | Epithelial | + | + | + | + | + |
| 3 | Epithelial | + | − | − | + | − |
| 4 | Retiform | + | + | + | − | − |
| 5 | Retiform | + | + | + | − | − |
| 6 | Epithelial | + | + | − | + | − |
| 7 | Kaposi | + | + | − | − | + |
Discussion
HE occurs in the soft tissues of the limbs, liver,
lungs, chest wall or skin. The tumor is rare, and various clinical,
radiological and pathological features have been sporadically
reported (2–16). To the best of our knowledge, the 7
intracranial HE cases enrolled in the current study represent the
largest documented case series. The different forms of HE include
retiform, kaposiform, epithelioid, epithelioid sarcoma-like and
composite HE, as well as endolymphatic papillary angioendothelioma
(17). The incidence of intracranial
epithelioid HE accounts for <0.02% of all primary intracranial
tumors (5,6), whereas retiform and kaposi HE are even
rarer (7,8). In the present study, epithelial-type HE
was more common (4 cases) than HE of the retiform (2 cases) or
kaposi (1 case) types. The endothelial nature of HE is indicated by
the histological features of the tumor and positive staining for
endothelial markers, such as CD34, CD31 and factor VIII-related
antigen.
HE can affect adults and children, with no clear
gender preponderance (13,14,18,19),
However, the gender distribution in the present study was 6:1,
females to males. Clinical symptoms were associated with the
location of the lesion, whereas common symptoms included headaches
and intracranial hypertension. The tumors often grew slowly; thus,
the period from the onset of the first symptom to the time of
diagnosis was relatively long. In the present study, the duration
of symptoms ranged between 4 months and 10 years. HE is a
low-proliferation borderline angiomatous tumor with malignant
behavior, such as local recurrence and metastasis (17). Five cases exhibited a lobulated
appearance, with different margin intensities from the lesion and
the surrounding normal brain tissues. Approximately 50% of the
intra-axial lesions presented with surrounding edema, with mild to
moderate edema around the lesion observed in 4 cases. The 2 cases
that originated from the skull showed expansive bone destruction.
However, the cortical bones of the inner and outer table of the
skull were discontinuous, which suggested that these 2 tumors had
potential malignant biological behavior.
Histopathological examination revealed the different
components of the myxoid matrix within the tumor, and the varying
distribution patterns of the tumor cells and mucus matrix
components. The majority of the abnormal blood vessels within the
tumor were thin-walled ectatic vessels, with lumens of varying
diameter containing red blood cells and thromboses. In the present
study, all tumors appeared as mildly hypointense to isointense on
T1-weighted images and inhomogeneously hyperintense on T2-weighted
images compared with that of the gray matter. Areas with low-signal
intensity or no signal on T1- and T2-weighted images represented
tumor vessels. Furthermore, MRA examination showed abnormal
vascularity in the tumor. Zhang et al (12) previously reported abnormal vessels in
the basilar region of the lesion using CT angiography. All cases in
the present study exhibited a multiple fleck pattern or smaller
punctate hyperintensities on the T1-weighted images, which may be
features of HEs that could promote correct imaging assessment.
Histological examination revealed scattered small hemorrhages and
thromboses in these tumors. Zheng et al (2) reported hemorrhage in approximately
one-quarter of intracranial HE lesions. Moreover, Ibarra et
al (15) proposed that the high
signal in the T1-weighted images is due to the methemoglobin
component of the intravascular thrombi. Another characteristic MRI
finding in HEs is a high incidence of multiple nodular high-signal
lesions with septations on T2-weighted images. The present results
are consistent with the previous study by Bourekas et al
(20), which demonstrated the slow
reflow phenomenon or blood sinus structure within these lesions
(9,16).
All 7 HEs in the present study showed tumor
enhancement, with the lesions demonstrating heterogeneous
enhancement patterns. Histology revealed that the margins were the
most active areas of cell proliferation and contained abundant
vasoganglion forming blood sinus-like structures, whereas the
central region was a solid zone with few blood vessels; this
finding may explain the heterogeneous enhancement of the tumors
(6,11,13,21–23).
The delayed enhancement is possibly associated with the abnormal
proliferation of blood vessels and sinus-like structures. The
appearance of rich vascularity provides important information for
the differential diagnosis and treatment strategy. A dural tail
sign was visible in 4 cases based on the invasive growth pattern of
the tumor.
DW imaging, initially used in stroke imaging, has
been used to study neoplasia. The current study presented HE
lesions with low signals during DW imaging, which suggests the
presence of loose connective tissue spaces and lower cell
components compared with those of the other solid tumors (24). However, the use of DW MRI in
differentiating between the histopathological subtypes of HEs has
not been well described, and its value in forming a differential
diagnosis should be evaluated in large studies.
CT of HE in the skull usually shows a slightly
higher density due to the abundant blood sinuses and small amount
of bleeding between tumor tissues (16). The two cases that originated from the
skull showed extensive bone destruction and osteolysis, as well as
discontinuous cortical bones with sclerotic margins; these findings
suggest a potentially invasive growth characteristic. Moreover, the
observed sparse trabecula bone shadows or spine-like protuberances
with evident edges and apparent enhancements resembled those
reported in previous studies (14–16). Tumor
calcification and periosteal reactions are rarely observed
(25). The two cases described in the
current study presented with expansion of bone due to involvement
of the diploic space, and enhancement, which is similar to the
results of previous studies (14–16).
Differential diagnosis for HE usually includes
meningioma, hemangioma and angiosarcoma (12,23). The
signal intensity on the T2-weighted images was low, which may be
one of the main features of meningiomas, whereas the dural tail
sign can enable correct imaging assessment. Adjacent skull
thickening in meningiomas is a feature of these extra-axial tumors,
which is less common in HEs. Hemangioma exhibit a hive-like or
fence-like structure, with a rapid enhancement at the early stage
and homogeneous enhancement after a delay (15). Primary angiosarcoma of the central
nervous system is an extremely rare malignancy, which exhibits
rapid growth (26). Imaging studies
characteristically show a well-demarcated lesion of the cerebral
hemisphere with avid enhancement (26,27), thus
differentiation from HE is difficult. However, by contrast to HE,
angiosarcomas usually present as a heterogeneous mass with
significant vasogenic edema and intratumoral cyst formation
(26,27).
In conclusion, HE is rare, but should be considered
as a possible diagnosis when a tumor presents as a lobulated mass,
with hemorrhage, signal voids of vessels, a heterogeneous
appearance and delayed enhancement; these factors could potentially
distinguish HE from other primary brain neoplasms. CT and MRI may
be useful in providing an early and accurate diagnosis; each method
is important due to the propensity of the tumor for abundant
vascularization and low-grade malignant biological behavior.
References
|
1
|
Weiss SW and Enzinger FM: Epithelioid
hemangioendothelioma: A vascular tumor often mistaken for a
carcinoma. Cancer. 50:970–981. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zheng J, Liu L, Wang J, Wang S, Cao Y and
Zhao J: Primary intracranial epithelioid hemangioendothelioma: A
low-proliferation tumor exhibiting clinically malignant behavior. J
Neurooncol. 110:119–127. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Baehring JM, Dickey PS and Bannykh SI:
Epithelioid hemangioendothelioma of the suprasellar area: A case
report and review of the literature. Arch Pathol Lab Med.
128:1289–1293. 2004.PubMed/NCBI
|
|
4
|
Hurley TR, Whisler WW, Clasen RA, Smith
MC, Bleck TP, Doolas A and Dampier MF: Recurrent intracranial
epithelioid hemangioendothelioma associated with multicentric
disease of liver and heart: Case report. Neurosurgery. 35:148–151.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hamlat A, Casallo-Quilliano C, Saikali S,
Lesimple T and Brassier G: Epithelioid hemangioendothelioma of the
infundibular-hypothalamic region: Case report and literature
review. J Neurooncol. 67:361–366. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Taratuto AL, Zurbriggen G, Sevlever G and
Saccoliti M: Epithelioid hemangioendothelioma of the central
nervous system. Immunohistochemical and ultrastructural
observations of a pediatric case. Pediatr Neurosci. 14:11–14. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kubota T, Sato K, Takeuchi H and Handa Y:
Successful removal after radiotherapy and vascular embolization in
a huge tentorial epithelioid hemangioendothelioma: A case report. J
Neurooncol. 68:177–183. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Aditya GS, Santosh V, Yasha TC and Shankar
SK: Epithelioid and retiform hemangioendothelioma of the skull
bone-report of four cases. Indian J Pathol Microbiol. 46:645–649.
2003.PubMed/NCBI
|
|
9
|
Cho WS, Kim SK, Park SH and Cho BK:
Intracranial kaposiform hemangioendothelioma: Proposal of a new
malignant variant. J Neurosurg Pediatr. 3:147–150. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mohan SM, Symss NP, Pande A, Chakravarthy
VM and Ramamurthi R: Intracranial epithelioid hemangioendothelioma.
Childs Nerv Syst. 24:863–868. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Palmieri G, Montella L, Martignetti A and
Bianco AR: Interferon alpha-2b at low doses as long-term
antiangiogenic treatment of a metastatic intracranial
hemangioendothelioma: A case report. Oncol Rep. 7:145–149.
2000.PubMed/NCBI
|
|
12
|
Zhang J, Wang Y and Geng D: Intracranial
epithelioid hemangioendothelioma: An unusual CTA finding in one
case. Br J Neurosurg. 24:294–295. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chan YL, Ng HK, Poon WS and Cheung HS:
Epithelioid hemangioendothelioma of the brain: A case report.
Neuroradiology. 43:848–850. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Parajón A and Vaquero J: Meningel
intracranial epithelioid hemangioendothelioma: Case report and
literature review. J Neurooncol. 88:169–173. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ibarra RA, Kesava P, Hallet KK and Bogaev
C: Hemangioendothelioma of the temporal bone with radiologic
findings resembling hemangioma. AJNR Am J Neuroradiol. 22:755–758.
2001.PubMed/NCBI
|
|
16
|
Kim HL, Im SA, Lim GY, Chun HJ, Lee H,
Park HJ and Byun JY: High grade hemangioendothelioma of the
temporal bone in a child: A case report. Korean J Radiol.
5:214–217. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Requena L and Kutzner H:
Hemangioendothelioma. Semin Diagn Pathol. 30:29–44. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mosoia L, Mabrut JY, Adham M, Boillot O,
Ducerf C, Partensky C and Baulieux J: Hepatic epithelioid
hemangioendothelioma: Long-term results of surgical management. J
Surg Oncol. 98:432–437. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lyburn ID, Torreggiani WC, Harris AC,
Zwirewich CV, Buckley AR, Davis JE, Chung SW, Scudamore CH and Ho
SG: Hepatic epithelioid hemangioendothelioma: Sonographic, CT and
MR imaging appearances. AJR Am J Roentgenol. 180:1359–1364. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bourekas EC, Cohen ML, Kamen CS, Tarr RW,
Lanzieri CF and Lewin JS: Malignant hemangioendothelioma
(angiosarcoma) of the skull: Plain film, CT and MR appearance. AJNR
Am J Neuroradiol. 17:1946–1948. 1996.PubMed/NCBI
|
|
21
|
Fernandes AL, Ratilal B, Mafra M and
Magalhaes C: Aggressive intracranial and extra-cranial epithelioid
hemangioendothelioma: A case report and review of the literature.
Neuropathology. 26:201–205. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tancredi A, Puca A and Carbone A:
Multifocal cerebral hemangio-endothelioma. Case report and review
of the literature. Acta Neurochir (Wien). 142:1157–1161. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hodaie M, Becker L, Teshima I and Rutka
JT: Total resection of an intracerebral hemangioendothelioma in an
infant. Case report and review of the literature. Pediatr
Neurosurg. 34:104–112. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Oliveira Rocha PC, Alcantara FP,
Souza-Vianna PE and Brito AP: Cerebral epithelioid
hemangioendothelioma with thoracic simultaneous involvement:
Advanced MRI features. Arq Neuropsiquiatr. 70:637–638. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wold LE, Unni KK, Beabout JW, Ivins JC,
Bruckman JE and Dahlin DC: Hemangioendothelial sarcoma of bone. Am
J Surg Pathol. 6:59–70. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hackney JR, Palmer CA, Riley KO, Cure JK,
Fathallah-Shaykh HM and Nabors LB: Primary central nervous system
angiosarcoma: Two case reports. J Med Case Rep. 6:2512012.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cookston M, Cotter GW, Schlitt M and
Bastian FO: Primary angiosarcoma of the brain. South Med J.
84:517–20. 1991. View Article : Google Scholar : PubMed/NCBI
|