Introduction
Arteriovenous fistulas (AVFs), are lesions with a
single abnormal connection between an artery and a vein that bypass
the capillary system. AVFs are distinct from arteriovenous
malformations (AVMs), which are disfiguring lesions with numerous
arteriovenous connections (1).
Arteriovenous fistulas may occur spontaneously or may be caused by
trauma or surgery (2). AVFs may be
acquired following penetrating or blunt trauma, such as car
accident injuries or stab wounds (3–5). Although
the head and neck tissues are relatively vascularized, AVFs located
in this region are relatively rare, and to the best of our
knowledge, no AVF of the parotid region has previously been
reported in the literature (3,6,7). Incidence and mortality rates vary
depending on the blood vessels affected by AVFs, as well as the
time elapsed prior to treatment (4).
Cases of AVF involving the neck area treated with both endovascular
embolization and surgical resection have been reported (4). AVFs have been successfully managed
surgically or with embolization, however, it is challenging to
predict the optimal treatment method (2,3)
The present study reports the case of a patient with
an arteriovenous fistula of the left parotid region that was
located between the left external jugular vein and the left
external carotid artery, which occurred subsequent to a penetrating
injury.
Case report
A 48-year-old man was referred to the Department of
Oncology of West China Hospital of Stomatology (Chengdu, Sichuan,
China) due to a pulsatile mass located on the left side of the
face, which had been present for 3 years.
The patient's medical history included a penetrating
trauma to his left facial region that occurred 8 years prior to the
appearance of the slowly growing mass. The patient had undergone an
embolization procedure at West China Hospital (Chengdu, China) 5
months previously in order to block the fistula between the
branches of the external jugular vein and the external carotid
artery. However, no evident recession was observed following the
procedure and the patient was referred to the Department of
Oncology, West China Hospital of Stomatology for further
treatment.
A physical examination identified a soft,
compressible and pulsatile mass located at the left parotid region.
Auscultation over the lesion identified a murmur-like bruit.
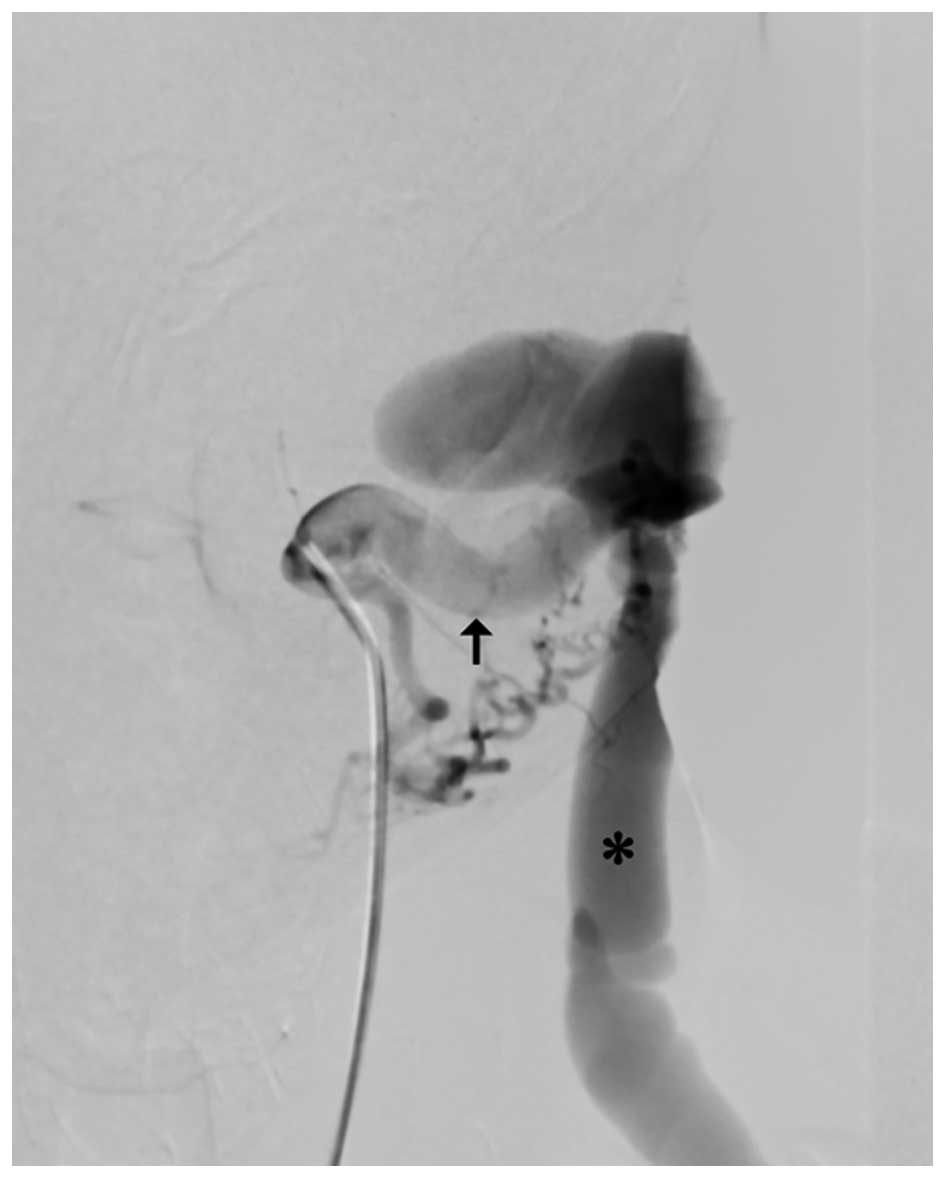
Computed tomography angiography (CTA) of the head and neck region
was performed to identify the nature of the lesion and the feeding
vessels. The CTA revealed an AVF on the left posterior ramus region
that measured 4.0×4.5 cm in diameter and was fed by a branch of the
external carotid artery (Fig. 1). The
identification was corroborated by digital subtraction angiography
(DSA) (Fig. 2) and
three-dimensional-DSA. The pre-surgery examination did not reveal
any evident heart problems.
Since the patient had a history of failed
embolization treatment, a surgical excision was performed without
preoperative embolization. The surgical excision of the AVF was
performed under general anesthetic, using an S-shape incision
anterior to the tragus. Due to the close association between the
facial nerve and the mass, intraoperative facial nerve monitoring
was employed during surgery for identifying the facial nerve. A
partial parotidectomy was performed to expose the mass, while the
facial nerve was protected and gently retracted aside. The feeding
vessels were ligated prior to extirpation of the mass. Following
ligation, the pulsation disappeared and the mass was wholly
excised. The left parotid tissue was then reapproximated and the
overlying skin was closed primarily. Postoperatively, the cosmetic
appearance was satisfying and the patient was free from recurrence
for one year subsequent to surgery.
The present patient provided written informed
consent, and the study was performed in compliance with the
Declaration of Helsinki and was approved by the Ethics Committee of
the West China College of Stomatology (Sichuan University, Chengdu,
Sichuan, China).
Discussion
AVFs are vascular lesions with a single connection
between an artery and a vein, and are commonly attributed to
previous trauma that affected the region, including penetrating
wounds (4), blunt trauma (1) or surgery (8). AVF is defined as a lesion that has a
single communication between an artery and a vein. Therefore, AVF
is a distinct clinical entity from a congenital or acquired
arteriovenous malformation (AVM), which has multiple distinct
connections.
AVF symptoms may vary depending on the location and
size of the fistula. Local symptoms are caused by disturbances to
vessel system resistance, and may include the absence of reversal
of diastolic flow, reversal of flow in the distal vessel,
dilatation of the proximal venous segment, venous hypertension and
incompetent valves. As a fistula enlarges, peripheral blood
pressure changes often occur, and may be followed by heart failure
(9).
AVF may be identified by a palpable thrill,
auscultated bruit over the lesion and by the Branham-Nicoladoni
sign (10); however, imaging
continues to be required for the confirmation and precise location
of the fistula.
While duplex ultrasonography, magnetic resonance
angiography and CTA are practical for the diagnosis of AVF and may
provide important information on the surrounding anatomical
structures, DSA is the standard technique for imaging AVFs
(9). DSA is particularly useful for
surgical planning and for identifying the feeding and draining
vessels. In the present study, CTA was used to confirm the presence
and nature of the lesion as an AVF, to identify the morphology and
surrounding tissue and to assist with therapeutic planning.
The goal of AVF treatment is to remove abnormal
connections and to restore the normal anatomy and function of the
artery and vein. AVFs of the external carotid system have
previously been managed surgically (3) and with embolization (11). Clinically, it is challenging to
predict the optimal treatment to ensure long-term success. Surgical
treatment remains preferable in young patients with AVF of the
extremities, unless the lesions are challenging to access (9). Endovascular techniques are particularly
useful for patients who have comorbidities or lesions that are
challenging to access.
In the present study, surgical therapy was
determined to be the optimal treatment approach for several
reasons. The embolization previously performed on the curent
patient did not result in an evident recession of the mass. Without
surgical intervention, a firm mass would remain in the parotid
salivary region. While this may be an acceptable result in other,
less conspicuous, areas of the body, the highly visible nature of
the salivary region made the mass easily visible. As the mass was
located beneath the parotid and near the facial nerve, it was
challenging to expose and resect the mass while preventing facial
paralysis. In the present study, intraoperative facial nerve
monitoring was employed to fulfill the purpose of preventing facial
paralysis.
To conclude, the present study reports the
successful surgical treatment of a patient with a rare fistula of
the parotid region, located between the external carotid artery and
external jugular vein. The present study demonstrates that, with
the aid of intraoperative facial nerve monitoring, surgical
treatment is a viable option for the successful management of AVF
lesions near the facial nerve following prior embolization
procedures that fail to block the fistula.
Acknowledgements
The authors thank Dr Zhuoyuan Zhang (Department of
Oncology, West China College of Stomatology, Sichuan University,
Chengdu, China), who provided the qualified pictures of the patient
and provided important suggestions for the manuscript.
References
|
1
|
Toros Zer S, Zorlu A, Deveci I, Deveci HS,
Naiboglu B and Gökçeer T: Traumatic arteriovenous fistula of the
upper lip: A case report. J Craniomaxillofac Surg. 38:485–487.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nikfarjam J, Taub PJ, Patel A and Rose E:
Arteriovenous fistula following radial forearm free flap. J
Reconstr Microsurg. 27:295–298. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dell'Amore A, Castriota F, Calvi S,
Magnano D, Noera G and Lamarra M: Post-traumatic carotid-jugular
arterio-venous fistula. Heart Lung Circ. 18:2932009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Robbs JV, Carrim AA, Kadwa AM and Mars M:
Traumatic arteriovenous fistula: Experience with 202 patients. Br J
Surg. 81:1296–1299. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sanborn MR, Nasrallah I, Stanton DC,
Stiefel MF, Hurst RW and Pukenas BA: Acquired arteriovenous fistula
associated with traumatic oroantral fistula: Endovascular
treatment. Head Neck. 35:E138–E141. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kalt M, Knipping L and Mangold G:
Traumatic arteriovenous fistula between superior thyroid artery and
vein. Chirurg. 68:1,304–1,306. 1997.(In German). View Article : Google Scholar
|
|
7
|
Adame N Jr and Bayless P: Carotid
arteriovenous fistula in the neck as a result of a facial
laceration. J Emerg Med. 16:575–578. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chaloupka JC, Kibble MB and Hoffman JC:
Ascending pharyngeal artery-internal jugular vein fistula
complicating radical neck dissection. Neuroradiology. 34:524–525.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sexton JA and Ricotta JJ: Endovascular
approaches to arteriovenous fistula. Adv Surg. 45:83–100. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Martin TJ, Hacein-Bey L and Rhee JS:
Arteriovenous fistula of the lower lip: Case report of combined
intravascular and surgical cure. WMJ. 105:47–50. 2006.PubMed/NCBI
|
|
11
|
Regina G, Impedovo G, Angiletta D, Marotta
V, Lillo A, Pestrichella F and De Blasi R: A new strategy for
treatment of a congenital arteriovenous fistula of the neck. Case
report. Eur J Vasc Endovasc Surg. 32:107–109. 2006. View Article : Google Scholar : PubMed/NCBI
|