Introduction
Severe genital bleeding is one of the most
frequently observed problems affecting women, and may have a
profound effect on physical, social and emotional quality of life
(1). There are a variety of causes of
abnormal uterine bleeding, including leiomyoma, endometrial polyps,
dysfunctional bleeding, endometrial malignancy, arteriovenous
malformation, retained products of conception and gestational
trophoblastic disease (1).
Microwave endometrial ablation (MEA), using a
frequency of 2.45 GHz, was initially developed by Kanaoka et
al (2) at Iseikai Hospital
(Osaka, Japan) for the treatment of functional and organic
menorrhagia. A previous study performed by the present research
group indicated that MEA was useful for the control of menorrhagia
and life-threatening uterine hemorrhage (3). However, MEA guidelines in Japan state
that the treatment is not suitable for endometrial malignancy
(4), and there have been no reports
that have evaluated the effectiveness of MEA for the treatment of
endometrial carcinoma. To the best of our knowledge, there is only
a single previous report of MEA being used to treat abnormal
uterine bleeding caused by endometrial carcinoma (5).
Currently, the typical treatment for endometrial
carcinoma is laparotomy with total abdominal hysterectomy, with or
without pelvic lymphadenectomy (6).
The effectiveness of MEA as a treatment for endometrial carcinoma
remains to be elucidated. In the present three cases, the efficacy
of MEA as a therapeutic option, for the control of massive bleeding
due to advanced and minimally-invasive endometrial carcinoma was
evaluated.
Case report
Case 1
A 59-year-old woman (gravida 7, para 2) was referred
to Shimane University School of Medicine (Izumo, Shimane) in
December 2011 for investigation and treatment of endometrial
carcinoma. The patient had a 10-year history of uterine leiomyoma
and menorrhagia, but no other significant past medical or surgical
history. When the patient began having a small amount of persistent
abnormal vaginal bleeding, she was treated with ethinyl estradiol
and norgestrel (detail unknown), however, the bleeding continued.
An outpatient endometrial cytological examination was performed,
which revealed hyperplasia, indicating a high possibility of
endometrial carcinoma. The patient's general physical examination
was unremarkable. Her hemoglobin level was low (7.8 g/dl; normal
range, 11.4–14.6 g/dl), and cancer antigen 125 (CA125; 17 U/ml;
normal range, <25 U/ml) and carbohydrate antigen 19–9 (25 U/ml;
normal range, <37 U/ml) levels were not elevated.
Transvaginal ultrasonography revealed a highly
echoic lesion in the uterus, measuring 35 × 23 mm. Emergency
magnetic resonance imaging (MRI) revealed an irregular and expanded
endometrium and a uterine mass which measured 40 × 30 mm. The image
additionally indicated potential deep invasion of the myometrium.
Endometrial curettage was attempted in order to obtain a
histological diagnosis of endometrial carcinoma, but the patient
began to bleed profusely. As it was not possible to achieve
hemostasis, emergency treatment was indicated; however, radical
open surgery was not advisable due to the small number of
gynecological oncologists available locally. Therefore, MEA was
used to control the heavy bleeding, prior to proceeding with
pre-planned radical open surgery.
Active bleeding from the uterus persisted during
MEA; however, the estimated intraoperative blood loss was low. The
patient was transfused with 4 units of packed red blood cells, and
did not experience any discomfort, significant bleeding or untoward
side effects over the subsequent several days.
The pathological result of the endometrial curettage
was grade 1 endometrial adenocarcinoma. Curative treatment was
subsequently performed in the form of total abdominal hysterectomy,
bilateral salpingo-oophorectomy and pelvic lymphadenectomy. The
International Federation of Gynecology and Obstetrics (FIGO) stage
was IIIc1 (7), due to lymph node
metastasis. The patient was treated with six 3 week cycles of
paclitaxel (175 mg/m2) and carboplatin chemotherapy
(area under the curve=5; dose, 700 mg), which was well-tolerated.
However, the patient succumbed to disease following recurrence 1
year subsequent to MEA treatment.
Case 2
A 43-year-old nulliparous woman was emergently
transported to Shimane University School of Medicine in February
2012, presenting with shock due to excessive menorrhagia. The
patient had a 10-year history of a submucosal uterine leiomyoma
with menorrhagia, and was known to be mentally disabled. The
patient's general examination was normal. Her lowest hemoglobin
level, prior to transportation to Shimane University School of
Medicine, was 5.1 g/dl.
Emergency MRI revealed an expanded endometrium and a
uterine mass, measuring 30 × 30 × 15 mm (Fig. 1). The image additionally indicated
potential endometrial carcinoma invading the myometrium. The
patient remained in shock, and MEA was suggested in order to
achieve hemostasis and to delay a decision on radical
treatment.
The patient was transfused with 6 units of packed
red blood cells during MEA, and did not experience any discomfort,
significant bleeding or untoward side effects during the
postoperative course.
The result of endometrial curettage performed
immediately prior to MEA was grade 1 endometrial adenocarcinoma.
The patient subsequently underwent total abdominal hysterectomy,
bilateral salpingo-oophorectomy and pelvic lymphadenectomy. The
tumor was classified as FIGO stage IA, due to myometrial invasion
of less than half the myometrial depth and no lymph node
metastases. The patient required no additional therapy and remains
alive without recurrence.
Case 3
A 44-year-old woman (gravida 2, para 2) was referred
to Shimane University School of Medicine in January 2013 with
persistent abnormal vaginal bleeding and severe anemia. The patient
had a history of menorrhagia, but no other significant medical or
surgical history. Her general examination was normal. The patient's
hemoglobin level was 6.2 g/dl and her CA125 level was not
elevated.
MRI revealed uterine adenomyosis, and it was
suggested that this was the cause of the patient's menorrhagia.
There were no observations to suggest malignancy, such as an
expanded endometrium or a uterine mass.
MEA was performed, preceded by dilation and
curettage for diagnosis and to rule out endometrial carcinoma. The
patient demonstrated an unremarkable postoperative course and was
discharged on the following day.
The result of the endometrial curettage was grade 2
endometrial endometrioid adenocarcinoma. The preoperative MRI had
revealed no evidence of myometrial invasion; therefore, the
malignant legion was hypothesized to be localized to the
endometrium, and it was possible that the carcinoma was completely
destroyed by the MEA. The patient was followed-up for 18 months,
and no findings indicating a residual malignant lesion were
identified by computed tomography (CT), positron emission
tomography/CT or MRI examinations.
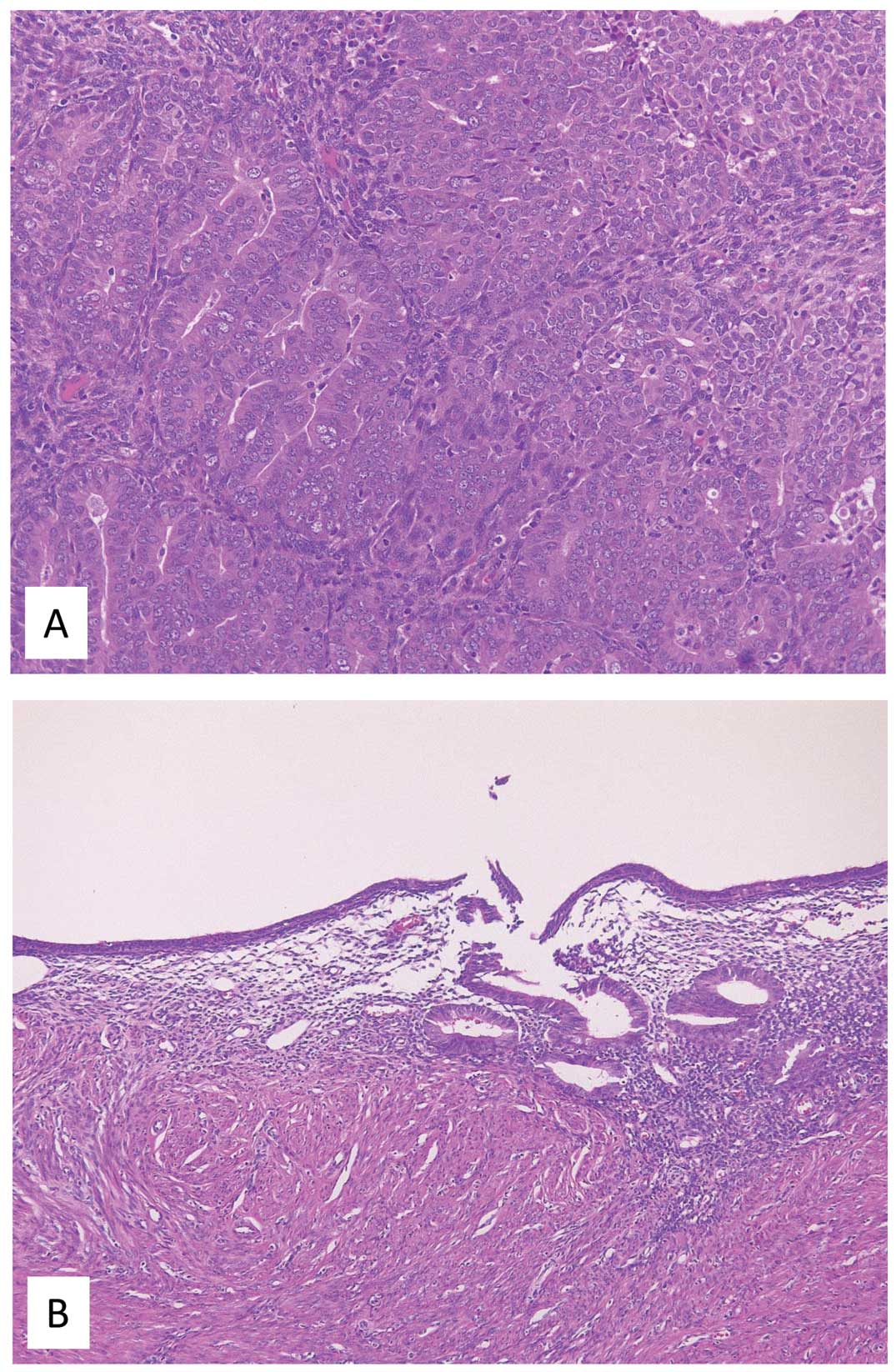
Although it appeared certain that this patient's
carcinoma had been cured by MEA, the risk of recurrence was
discussed. Ultimately, a decision to perform definitive treatment
was reached. The patient underwent total laparoscopic hysterectomy
with bilateral salpingo-oophorectomy. Pathological examination
revealed no evidence of residual carcinoma (Fig. 2A and B). The patient remains alive
without recurrence.
Discussion
The present study group previously reported that MEA
is highly effective for the emergency treatment of life-threatening
uterine hemorrhage (3,8). Prior to the approval of MEA for
insurance coverage in Japan, the present institution obtained
approval to perform the procedure from the ethics committee of
Shimane University Medical Department (Izumo, Japan), and this
committee additionally approved the treatment for the patients in
the present case series. Following comprehensive explanation of the
risks and benefits of MEA, all patients provided written informed
consent.
MEA was performed under spinal anesthesia using a
device consisting of a sounding applicator and a microwave
generator. The 2.45 GHz microwaves were supplied by the Microtaze
AZM-520 generator (Alfresa Pharma Corp., Osaka, Japan). Microwaves
were transmitted at 70 W for ~50 sec. In order to avoid perforating
the uterus, transabdominal ultrasonographic guidance was used.
MEA guidelines state that suspicion of endometrial
malignancy is a contraindication for the use of MEA (4); however, there is no clear evidence
against the use of the procedure in these situations. To the best
of our knowledge, MEA has been used only once in an attempt to
treat endometrial carcinoma-associated uterine bleeding (5). In that case report, the authors
suggested that MEA may be considered a palliative treatment for
elderly women with early endometrial carcinoma who have severe
complications and are therefore unfit for standard treatment
(5). In the current case series,
emergency control of uterine hemorrhage caused by endometrial
carcinoma in two patients was achieved using MEA. In these
patients, elective surgical treatment was subsequently successfully
performed.
The MEA procedure is rapid and demonstrates a low
level of blood loss compared with open surgery. The present
experiences with endometrial carcinoma patients demonstrate that
MEA may be used for emergency palliative control of uterine
bleeding. However, it should be noted that the MEA procedure cannot
be used for curative treatment in patients with advanced-stage
endometrial carcinoma (4). Therefore,
it is recommended that MEA be used for emergency control of
life-threatening uterine hemorrhage, with subsequent laparotomy for
the radical treatment of endometrial carcinoma.
In addition, a patient with endometrial carcinoma
that was undiagnosed at the time of the procedure was treated with
MEA. At the time of hysterectomy, 18 months subsequent to MEA,
there was no malignancy detected following pathological
examination. This suggests that malignant lesions localized to the
endometrium may be treated using MEA.
In conclusion, the current case series concerning 3
patients suggested that MEA may be used to control life-threatening
hemorrhage due to advanced-stage endometrial carcinoma, and may
additionally be used to treat endometrial carcinoma localized to
the endometrium. Future studies of additional cases are required to
confirm the results of the present case series.
References
|
1
|
Cowan BD and Morrison JC: Management of
abnormal genital bleeding in girls and women. N Engl J Med.
324:1710–1715. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kanaoka Y, Hirai K and Ishiko O: Microwave
endometrial ablation for an enlarged uterus. Arch Gynecol Obstet.
269:30–32. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nakayama K, Rahman MT, Rahman M, Ishikawa
M, Yeasmin S, Katagiri A, Iida K, Nakayama N, Aoki S and Miyazaki
K: Microwave endometrial ablation is a highly efficacious way to
emergently control life-threatening uterine hemorrhage. Arch
Gynecol Obstet. 283:1065–1068. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kanaoka Y, Ishikawa N, Asakawa Y and
Nakayama K: Practice Guideline of MEA 2012. https://www.alfresa-pharma.co.jp/microtaze/MEAguideline2012.pdf(In
Japanese). Accessed. February 04–2016
|
|
5
|
Sharp N, Ellard M, Hirschowitz L,
Malthouse S and Johnson N: Successful microwave ablation of
endometrial carcinoma. BJOG. 109:1410–1412. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
He H, Zeng D, Ou H, Tang Y, Li J and Zhong
H: Laparoscopic treatment of endometrial cancer: systematic review.
J Minim Invasive Gynecol. 20:413–423. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lu Z and Chen J: Introduction of WHO
classification of tumours of female reproductive organs. (fourth).
Zhonghua Bing Li Xue Za Zhi. 42:649–650, (In Chinese). PubMed/NCBI
|
|
8
|
Nakayama K, Ishibashi T, Ishikawa M,
Katagiri A, Katagiri H, Iida K, Nakayama N and Miyazaki K:
Microwave endometrial ablation at a frequency of 2.45 GHz for
menorrhagia: Analysis of treatment results at a single facility. J
Obstet Gynecol Res. 40:224–229. 2014. View Article : Google Scholar
|