Introduction
It has been proven that regional radiotherapy, an
integral part of breast-conserving therapy or mastectomy, can
reduce the risk of local-regional recurrence of breast cancer and
improve overall survival (1–5). Conventionally, post-mastectomy regional
irradiation is planned using the two-dimensional data of the
central axis of the treatment field and the wedged tangential pair
treatment beams (6–9). More recently, intensity-modulated
radiation therapy (IMRT), which has the ability to improve dose
conformity and to decrease doses to the surrounding critical
healthy structures (10–12), has been applied in post-mastectomy
regional irradiation. However, ‘step-and-shoot’ IMRT is far from
perfect in the clinical setting, and the development of novel
radiotherapy techniques and devices is required. The optimization
of a radiotherapy plan, the sparing of healthy tissues and the
reduction in treatment time during the radiotherapy workflow are
crucial.
Capable of delivering a highly conformal dose
distribution in a relatively shorter duration, volumetric-modulated
arc therapy (VMAT) (13) has aroused
enormous interest in radiotherapy institutes worldwide. VMAT has
been previously compared with IMRT for the treatment of various
types of cancer at different sites (14–19).
Although it has been well established that VMAT results in improved
delivery efficiency over IMRT (20),
there are few studies on whether VMAT represents a better treatment
plan than IMRT for post-mastectomy regional irradiation.
In the present study, VMAT plans with single arc
(1ARC) and dual arcs (2ARC) were evaluated and compared to
step-and-shoot IMRT technology with regard to plan quality
parameters, including homogeneity/conformity index (HI/CI), mean
dose to the contralateral breast, ipsilateral lung and heart, and
the maximum dose to the spinal cord, as well as the treatment
efficiency parameters, including total treatment time (TTT) and
number of monitor units (MUs).
Materials and methods
Patient selection and image
acquisition
A total of 24 female patients who required
post-mastectomy regional irradiation in the Department of Oncology,
Xinqiao Hospital (Third Military Medical University, Chongqing,
China) between May and October 2013 were selected for enrolment.
Patients aged between 18 and 75 years, with an Eastern Cooperative
Oncology Group score of 0–2 (21) and
adequate function of the liver, kidney, heart and hematopoietic
system were considered eligible for the study. Patients that had
undergone radiotherapy of the axillary or supraclavicular lymph
nodes were excluded from the study. Among the 24 enrolled patients,
there were 11 cases of right-sided breast cancer and 13 cases of
left-sided breast cancer. The median age of the patients was 54
years (range, 21–74 years). All cases involved ductal or lobular
carcinoma in different quadrants and underwent mastectomy. The
stages ranged from pT3N2M0 to pT4N3M0, and required post-mastectomy
regional radiotherapy according to National Comprehensive Cancer
Network guidelines (2013, V1) (22).
Following immobilization of the patients with a thermoplastic
body-fix frame in a supine on the treatment bed, the patients were
scanned using a helical computed tomography (CT) scanner with a
5-mm slice thickness. Scan extension included the underside of the
chin to the upper abdomen. The CT data were transferred to the
commercial treatment planning system (TPS), Oncentra MasterPlan
V4.1 (OMP; Nucletron BV, Veenendaal, The Netherlands), for
contouring of targets and plan design. Written informed consent was
obtained from all patients and the study was approved by the
Medical Ethics Committee of Xinqiao Hospital, Third Military
Medical University.
Definition of target volume and organs
at risk (OARs)
The radiotherapy physicians and planners used a
standardized set of contouring guidelines (23). Target volumes and OARs were delineated
and confirmed by three different qualified radiotherapy physicians.
The clinical target volume (CTV) encompassed the post-operated
chest wall, supraclavicular lymph nodes and internal mammary nodes.
CTV was defined medially at the lateral edge of the sternum,
including the sternal-rib junction, laterally at the preexisting
breast tissue, including the mid axillary line, inferiorly at the
inframammary fold and superiorly at the inferior edge of the
cricoid cartilage. The medial extent of the mastectomy scar was
typically included. Plan target volume (PTV) was obtained by
expanding 3 mm in all directions except toward the skin. The border
of the PTV on the skin side was at least 1 mm from the skin
surface. The surrounding critical healthy tissues, including the
contralateral breast, ipsilateral lung, spinal cord and heart, were
contoured. An extra 3-mm margin was added to the spinal cord as the
planning organ-at-risk volume (PRV).
Planning objective
All subsequent plans were conducted on OMP. For all
patients, the prescribed dose was set to deliver 50 Gy normalized
to 100% in 25 fractions encompassing at least 95% of the PTV, i.e.,
V100%>95%, while ≤2% of any PTV would receive
>110% of its prescribed dose; the PTV ranged from 269.00 to
783.00 cm3 (mean±standard deviation, 519.80±173.39
cm3). Other planning objectives for the OARs were as
follows: Point dose of PRV of spinal cord, <10 Gy; percentage
volume of ipsilateral lung receiving >20 Gy (V20),
<20% and 30 Gy (V30), <10%; percentage volume of
humerus receiving >50 Gy (V50), <5%; and
percentage volume of heart receiving >40 Gy (V40),
<20%. For the T4 patients with skin involvement, a bolus
material with a thickness of 1 cm was added during the whole
course, including immobilization, plan optimization, dosimetric
calculation and radiation delivery.
Planning techniques
Using identical CT datasets and the exact same
contours, all VMAT and IMRT plans were created using 6-MV photon
beams commissioned for a Varian Trilogy Linac, equipped with a
120-leaf Multileaf Collimator (MLC; Varian Medical Systems, Palo
Alto, CA, USA), with a maximal leaf speed of 2.5 cm/sec, a maximal
jaw speed of 1.5 cm/sec, a maximal gantry speed of 6 cm/sec and a
variable dose rate of up to 600 MUs/min. The optimization
constraints and relative priorities were the same for the IMRT, and
1ARC and 2ARC VMAT plans. IMRT beams were equally spaced through
the 200 sector angle in the axial plane, with fixed five gantry
angles delivered in a step-and-shoot mode. 1ARC VMAT consisted of a
single 200° rotation, while 2ARC VMAT consisted of two coplanar
arcs of 200°, optimized simultaneously and delivered with opposite
rotation (clockwise and anticlockwise). The isocenter was placed at
the center of the PTV. For the two VMAT plans, the couch angle was
set as 0° and at the same time, the collimator was set at 10°. The
collapse cone photon dose calculation algorithm was used for all
cases. The dose calculation grid was set at 2.5 mm. Each plan was
formulated by three different radiotherapy physicists and confirmed
by three different radiotherapy physicians.
Evaluation parameters
The dose to the OARs, including the contralateral
breast, ipsilateral lung, double lungs, spinal cord and heart, was
measured and compared among the three planning techniques. The
plans were evaluated according to dose-volume histogram (DVH)
analysis, and plan quality was assessed by calculating the mean
dose to the contralateral breast, ipsilateral lung, double lungs
and heart, and the maximum dose to the spinal cord. The CI and HI
were calculated according to the Radiation Therapy Oncology Group
definition (24,25) as follows: CI = VRI / TV and
HI = Imax / RI, with VRI representing the
volume (V) of the prescribed dose for the PTV, TV as the total
volume of the PTV, Imax representing the maximum dose
and RI as the prescribed dose of the PTV. These two formulae were
therefore changed to CI = VDprescribed / VPTV
and HI = Dmax / Dprescribed. A CI and HI
tendency towards a value of 1 demonstrated that the plan could be
improved. Delivery parameters were recorded in terms of MU per
fraction, mean dose rate, beam-on time, treatment time and TTT
(defined as beam-on plus machine programming and setting time, but
excluding patient positioning and imaging procedures).
Statistical analysis
All data presented in the text, tables and figures
are presented as the mean ± standard deviation. For statistical
analysis, exact Wilcoxon signed rank tests were used to assess any
differences between the treatment parameters. Differences were
considered statistically significant at P<0.05. All computations
were performed using the IBM SPSS statistics program (version 19;
SPSS Inc., Chicago, IL, USA). All statistical tests were
two-sided.
Results
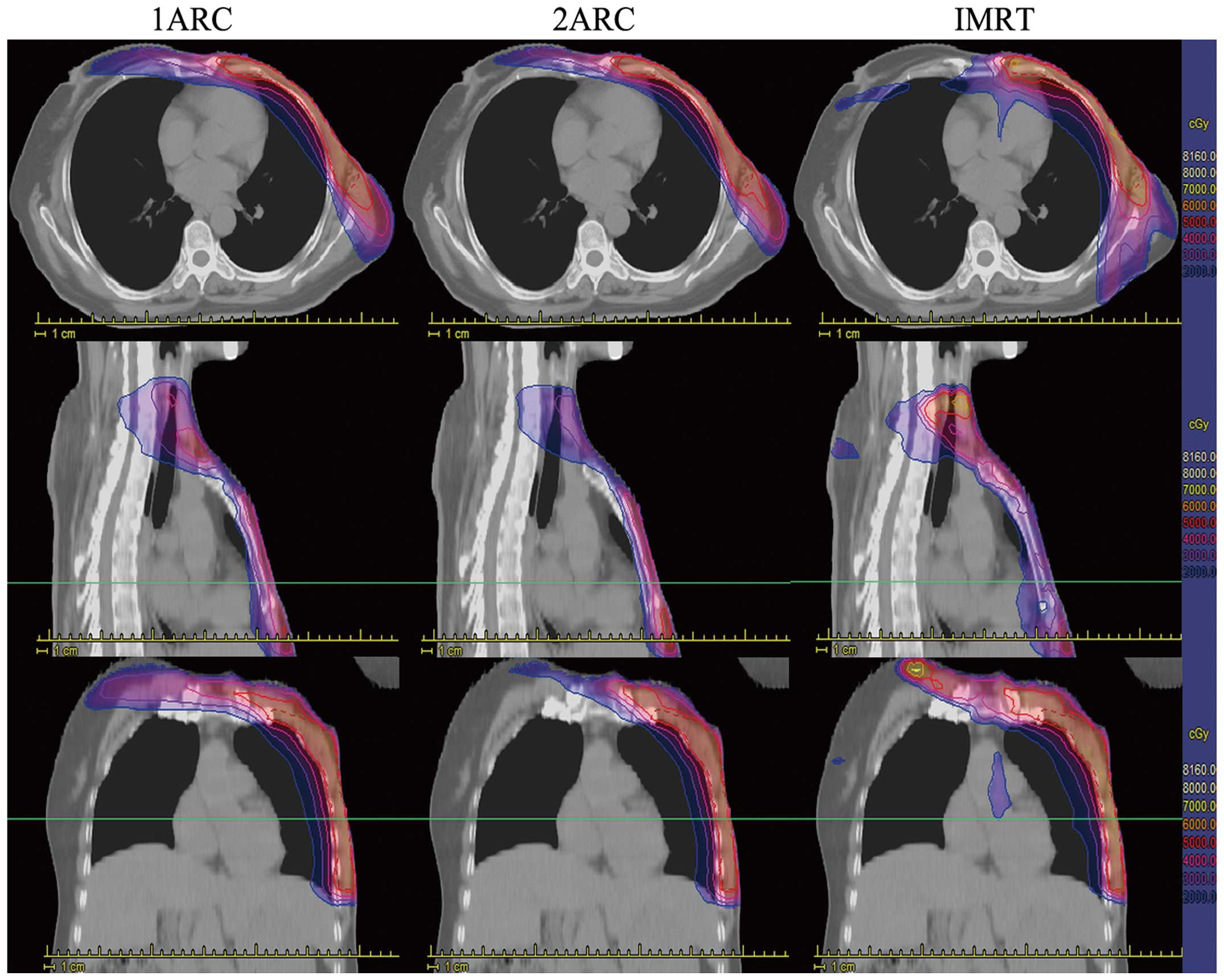
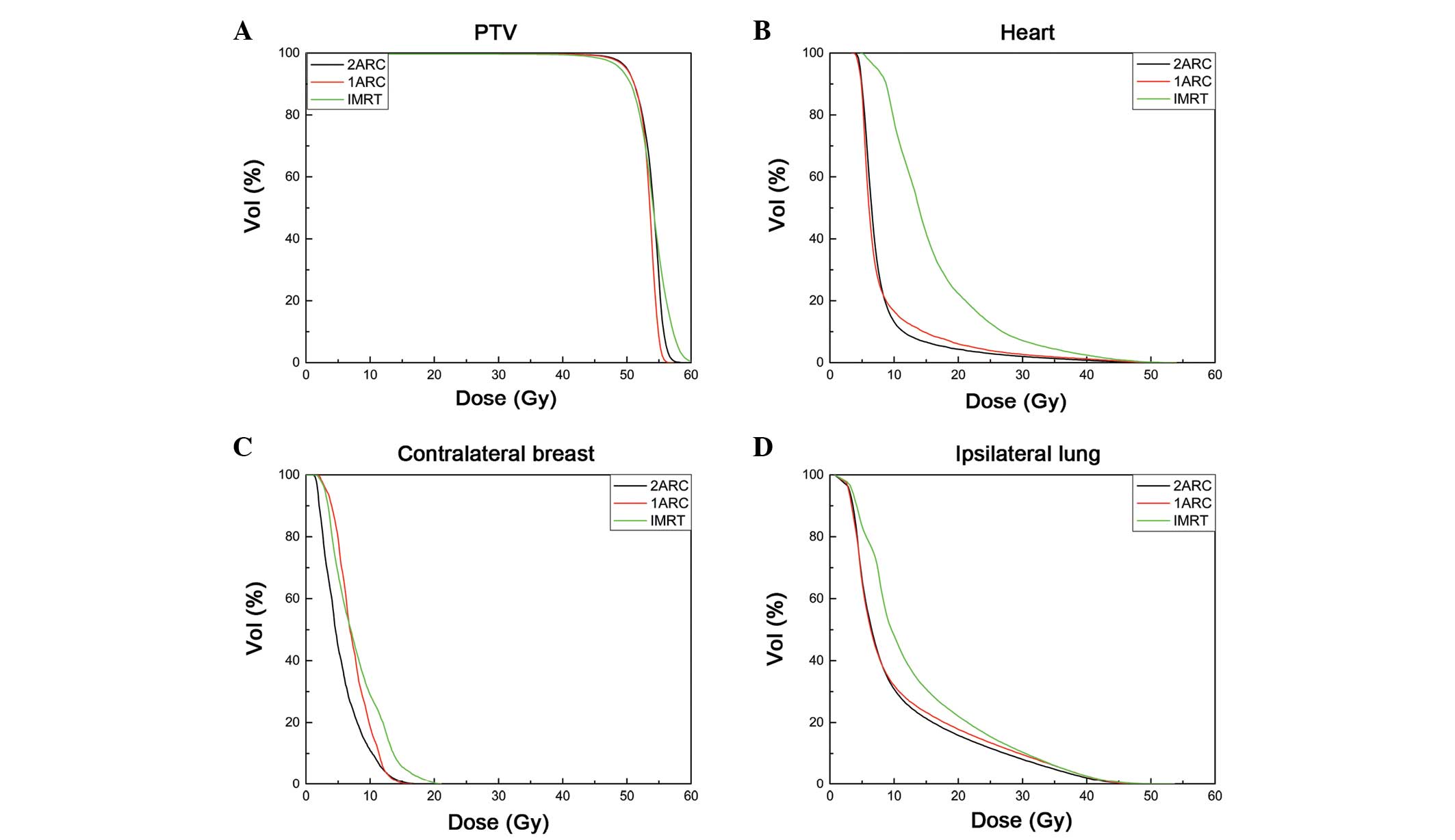
Dose distribution
The typical axial, coronal and sagittal dose
distributions produced by each of the three techniques in one
representative case are displayed in Fig.
1. Fig. 2A demonstrates the mean
DVH of the PTVs, comparing the three techniques for the entire
cohort. Fig. 2B–D reports the average
DVH computed for OARs, including the heart, contralateral breast
and ipsilateral lung. The mean values of the study parameters among
the three different techniques are tabulated in Table I, with their corresponding standard
deviation.
 | Table I.Target coverage and doses to organs at
risk for three techniques (mean ± standard deviation). |
Table I.
Target coverage and doses to organs at
risk for three techniques (mean ± standard deviation).
| Dosimetric
parameters | IMRT | 1ARC | 2ARC | P-valuea | P-valueb | P-valuec |
|---|
| Homogeneity
index |
1.24±0.05 |
1.20±0.06 |
1.15±0.04 | 0.005 | 0.005 | 0.005 |
| Conformity index |
0.71±0.12 |
0.78±0.05 |
0.83±0.04 | 0.005 | 0.005 | 0.005 |
| V30 (Ipsilateral
lung), % |
10.3±3.3 |
8.6±3.4 |
8.2±3.9 | 0.043 | 0.043 | 0.144 |
| V20 (Ipsilateral
lung), % |
22.0±4.6 |
15.5±3.1 |
17.7±4.1 | 0.043 | 0.043 | 0.176 |
| V5 (Ipsilateral
lung), % |
83.0±10.9 |
64.0±7.4 |
65.2±6.7 | 0.063 | 0.063 | 0.686 |
| V30 (double
lungs), % |
5.9±1.6 |
4.1±1.6 |
3.8±1.6 | 0.043 | 0.027 | 0.141 |
| V20 (double
lungs), % |
14.5±5.8 |
11.4±6.2 |
10.3±5.7 | 0.043 | 0.027 | 0.093 |
| V5 (double
lungs), % |
52.9±8.2 |
43.4±6.5 |
43.5±6.7 | 0.080 | 0.080 | 0.893 |
| V10
(contralateral breast), % |
28.9±3.2 |
10.5±0.2 |
10.8±0.1 | 0.005 | 0.005 | 0.345 |
| D15
(contralateral breast), Gy |
13.7±0.2 |
10.5±0.3 |
8.9±0.3 | 0.005 | 0.005 | 0.753 |
| Dmean
ipsilateral lung, Gy |
9.5±2.1 |
8.0±2.5 |
7.9±2.2 | 0.028 | 0.028 | 0.345 |
| Dmean double
lungs, Gy |
7.3±11.6 |
6.0±2.1 |
6.5±16.6 | 0.141 | 0.028 | 0.345 |
|
DmaxSpinalCord, Gy |
9.6±4.3 |
5.2±2.9 |
4.8±2.7 | 0.043 | 0.028 | 0.753 |
| Dmean
heart, Gy |
10.6±5.0 |
7.8±2.7 |
7.2±2.3 | 0.043 | 0.028 | 0.173 |
Target coverage and dose
homogeneity
All the plans were considered acceptable for at
least the 95% PTV volume that received 100% of the prescribed dose.
The 1ARC and 2ARC VMAT plans resulted in a better dose HI compared
with IMRT, with a relative improvement of 7.8 and 3.3%,
respectively. This difference was significant (P<0.05).
Similarly, the 1ARC and 2ARC VMAT plans exhibited a significantly
higher CI than the IMRT (both P<0.05) (Table I). As expected, the 2ARC VMAT plan
produced the best dose CI compared with 1ARC VMAT and IMRT, with a
relative improvement of 6.6% (P<0.01) and 15.7% (P<0.01),
respectively. Similarly, the 2ARC VMAT plan demonstrated a
significantly higher HI than the other two techniques (both
P<0.01) (Table II).
 | Table II.Delivery parameters of three
different treatment techniques (mean ± standard deviation). |
Table II.
Delivery parameters of three
different treatment techniques (mean ± standard deviation).
| Delivery
parameters | IMRT | 1ARC | 2ARC |
P-valuea |
P-valueb |
P-valuec |
|---|
| Monitor units |
1051±106 |
539±88 |
608±94 | 0.005 | 0.005 | 0.005 |
| Beam-on time,
sec |
285±19 |
51±5 |
125±7 | 0.005 | 0.043 | 0.043 |
| Treatment time,
sec |
440±56 |
59±12 |
129±34 | 0.005 | 0.028 | 0.028 |
| Total treatment
time, sec |
620±62 |
180±16 |
300±38 | 0.005 | 0.005 | 0.028 |
OARs
Spinal cord
All three techniques reached the planning objective
of Dmax<10 Gy for the PRV of the spinal cord. The
1ARC and 2ARC VMAT plans led to a significant decrease in the
Dmax of the spinal cord (P<0.05) compared with IMRT.
No significant dose difference was found between the 2ARC and 1ARC
VMAT plans.
Heart
For the 24 cases of post-mastectomy regional
irradiation, the three techniques yielded low doses to the heart
(Fig. 2B). The 1ARC and 2ARC VMAT
plans resulted in a significantly lower heart dose than IMRT
(P<0.05). No significant difference in the dose was found in the
2ARC and 1ARC VMAT plans.
Contralateral breast
The 1ARC and 2ARC plans exhibited lower volume
percentages for the contralateral breast that received 10 Gy
compared with the IMRT plan (P<0.05). Furthermore, there was a
lower dose for the contralateral breast that covered 15% of the
volume compared with that detected by the IMRT plan (P<0.05)
(Table I). No significant difference
existed between 1ARC and 2ARC plans in terms of the volume
percentage of the contralateral breast that received 10 Gy
(P>0.05) or the dose of the contralateral breast that covered
15% of the volume (P>0.05).
Lung
The volume to the lung was evaluated, including
ipsilateral and double lungs, and the specific dose limits were 5,
20 and 30 Gy. It was evident that 1ARC and 2ARC VMAT resulted in a
lower volume at an ipsilateral lung dose measuring 5, 20 and 30 Gy
compared with IMRT (64.0 and 65.2 vs. 83.0%, 15.5 and 17.7 vs.
22.0%, and 8.6 and 8.2 vs. 10.3%, respectively) (Table I). The volume differences were
significant at 20 and 30 Gy (P<0.05), but not at 5 Gy
(P>0.05). Double lungs produced similar results to the
ipsilateral lung. All the values are listed in Table I.
Planning and delivery efficiency
The mean values of MUs per fraction were 1,051 in
IMRT, 539 in 1ARC VMAT and 608 in 2ARC VMAT (Table II). The 1ARC and 2ARC VMAT plans
resulted in a 49 and 42% reduction in MUs per fraction consumed.
The mean planning time was 6.9, 23.4 and 32.5 min for IMRT, 1ARC
and 2ARC, respectively. The mean time to prepare a VMAT plan was
found to be approximately four times that required to prepare a
fixed-field IMRT plan, which was attributed to the fundamental
difference in the method for dosimetric optimization between the
two techniques. The 1ARC and 2ARC plans exhibited a shorter
treatment time, with a mean beam-on time of 51 and 125 sec,
respectively, and the mean treatment time was 59, 129 and 440 sec
for 1ARC, 2ARC and IMRT, respectively. When considering the time
for setup and position correction by image-guided radiotherapy, it
was estimated that the TTT for each patient per fraction was ~180,
300 and 620 sec for 1ARC, 2ARC and IMRT, respectively (P<0.05)
(Table II). The 1ARC and 2ARC VMAT
techniques reduced treatment time by ~87 and 40%, respectively. As
expected, 1ARC VMAT MU and TTT were less than those for 2ARC VMAT
(P<0.05) due to the gantry rotation.
Discussion
Post-mastectomy regional irradiation improves
disease management, while reducing patient toxicity. Improving the
homogeneity of irradiation following mastectomy reduces the acute
complication rate, as well as long-term fibrosis (26). The boosting of radiation to enhance
the local control rate in high-risk women has previously been
studied (27–29), and in consideration of this, reducing
the excess irradiation to the contralateral breast is important, as
it may decrease unnecessary cardiac and pulmonary irradiation.
The present study compared 1ARC, 2ARC and IMRT
radiation plans in 24 cases of post-mastectomy regional
irradiation. As three-dimensional conformal radiotherapy has not
been demonstrated to be better than IMRT, the CI, HI and OAR dose
were evaluated in IMRT, and 1ARC and 2ARC VMAT plans in the current
study. Since treatment planning depended on variations in TPS,
calculation algorithm, therapy equipment and most importantly, the
skill level of the planner, the present study aimed to normalize
the process of the three radiotherapy plans. For each patient,
1ARC, 2ARC and IMRT plans were generated under identical constraint
conditions. Each plan was designed by three different radiotherapy
physicists and confirmed by three different radiotherapy
physicians. Thus, the interpersonal deviation was minimized
The results of the present study demonstrated that
1ARC or 2ARC VMAT significantly spared the OARs, without
compromising target coverage when compared to the IMRT technique.
Although the mean time to prepare a VMAT plan was roughly four
times that of preparing a fixed-field IMRT plan, this plan
displayed several inherent advantages, including a reduced
treatment time and a decreased number of MUs. The greatest
advantage of using VMAT in the current study was the shorter
treatment time, which improved the comfort and satisfaction of the
patients, while reducing the chance of movement due to discomfort
and random errors introduced by intrafraction tumor motion.
In addition to the aforementioned application of
VMAT, the present study compared the 1ARC and 2ARC technique in
post-mastectomy regional irradiation. The advantages of using 2ARC
were an increase in the modulation factor during optimization and
the provision of more MLC control points than 1ARC, achieving
better dose distribution. However, in the current study, 2ARC did
not exhibit significant advantages over 1ARC. The most notable and
perhaps pertinent result was the further improvement in conformity
and homogeneity indexes when using 2ARC VMAT. Treatment volume in
the 2ARC plan could be much lower than that used in IMRT or 1ARC.
Thus, 2ARC would direct less radiation to the OARs. The results of
the present study are consistent with a previous study on
nasopharyngeal carcinoma (14), in
which 2ARC led to superior results in terms of dose coverage and
spared OARs when compared with single arc VMAT, without sacrificing
the delivery efficiency. Therefore, 2ARC VMAT may be an alternative
to 1ARC, allowing more optimal HI and CI values to be obtained,
since 2ARC VMAT created a wide range of beam incidents that allowed
a larger degree of freedom in the inverse optimizing process, and a
greater capability for modulating the gantry speed, MLC shape and
dose rate.
In conclusion, the advantage of delivering better
dose distribution in a shorter treatment time (14–19),
afforded by 1ARC and 2ARC VMAT, allowed these therapies to serve as
more efficient methods of delivering post-mastectomy irradiation
than the fixed-field IMRT technique. Long-term follow-up could
provide actual toxicity profiles and a clear assessment of VMAT
treatment efficacy. Furthermore, the present study did not include
patients who underwent breast-conserving radiotherapy, and further
studies could focus on these patients to provide a greater insight
into post-mastectomy irradiation. The 1ARC and 2ARC VMAT plans
produced superior dose distribution for post-mastectomy regional
irradiation with less dose exposure to critical healthy structures.
The plan quality and delivery efficiency made VMAT a reasonable
option for post-mastectomy regional irradiation, while the 2ARC
VMAT resulted in an improved HI and CI compared with the 1ARC
plan.
Acknowledgements
The authors are grateful for the support of the
National Natural Science Foundation of China (grant no. 81272910)
and the Clinical Foundation of the Third Military Medical
University, Chongqing, China (grant no. 2011XLC46).
References
|
1
|
Hijal T, Fournier-Bidoz N, Castro-Pena P,
Kirova YM, Zefkili S, Bollet MA, Dendale R, Campana F and Fourquet
A: Simultaneous integrated boost in breast conserving treatment of
breast cancer: A dosimetric comparison of helical tomotherapy and
three-dimensional conformal radiotherapy. Radiother Oncol.
94:300–306. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Clarke M, Collins R, Darby S, Davies C,
Elphinstone P, Evans V, Godwin J, Gray R, Hicks C, James S, et al:
Early Breast Cancer Trialists' Collaborative Group: Effects of
radiotherapy and of differences in the extent of surgery for early
breast cancer on local recurrence and 15-year survival: An overview
of the randomised trials. Lancet. 366:2087–2106. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fisher B, Anderson S, Bryant J, Margolese
RG, Deutsch M, Fisher ER, Jeong JH and Wolmark N: Twenty-year
follow-up of a randomized trial comparing total mastectomy,
lumpectomy, and lumpectomy plus irradiation for the treatment of
invasive breast cancer. N Engl J Med. 347:1233–1241. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kong FM, Klein EE, Bradley JD, Mansur DB,
Taylor ME, Perez CA, Myerson RJ and Harms WB: The impact of central
lung distance, maximal heart distance, and radiation technique on
the volumetric dose of the lung and heart for intact breast
radiation. Int J Radiat Oncol Biol Phys. 54:963–971. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kirova YM, Fournier-Bidoz N, Servois V,
Laki F, Pollet GA, Salmon R, Thomas A, Dendale R, Bollet MA,
Campana F, et al: How to boost the breast tumor bed? A
multidisciplinary approach in eight steps. Int J Radiat Oncol Biol
Phys. 72:494–500. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gray JR, McCormick B, Cox L and Yahalom J:
Primary breast irradiation in large-breasted or heavy women:
Analysis of cosmetic outcome. Int J Radiat Oncol Biol Phys.
21:347–354. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Neal AJ, Mayles WP and Yarnold JR: Invited
review: Tangential breast irradiation-rationale and methods for
improving dosimetry. Br J Radiol. 67:1149–1154. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Moody AM, Mayles WP, Bliss JM, A'Hern RP,
Owen JR, Regan J, Broad B and Yarnold JR: The influence of breast
size on late radiation effects and association with radiotherapy
dose inhomogeneity. Radiother Oncol. 33:106–112. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Neal AJ, Torr M, Helyer S and Yarnold JR:
Correlation of breast dose heterogeneity with breast size using 3D
CT planning and dose-volume histograms. Radiother Oncol.
34:210–218. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kestin LL, Sharpe MB, Frazier RC, Vicini
FA, Yan D, Matter RC, Martinez AA and Wong JW: Intensity modulation
to improve dose uniformity with tangential breast radiotherapy:
Initial clinical experience. Int J Radiat Oncol Biol Phys.
48:1559–1568. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vicini FA, Sharpe M, Kestin L, Martinez A,
Mitchell CK, Wallace MF, Matter R and Wong J: Optimizing breast
cancer treatment efficacy with intensity-modulated radiotherapy. Int
J Radiat Oncol Biol Phys. 54:1336–1344. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lo YC, Yasuda G, Fitzgerald TJ and Urie
MM: Intensity modulation for breast treatment using static
multi-leaf collimators. Int J Radiat Oncol Biol Phys. 46:187–194.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Palma DA, Verbakel WF, Otto K and Senan S:
New developments in arc radiation therapy: A review. Cancer Treat
Rev. 36:393–399. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lee TF, Ting HM, Chao PJ and Fang FM: Dual
arc volumetric-modulated arc radiotherapy (VMAT) of nasopharyngeal
carcinomas: A simultaneous integrated boost treatment plan
comparison with intensity-modulated radiotherapies and single arc
VMAT. Clin Oncol (R Coll Radiol). 24:196–207. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bertelsen A, Hansen CR, Johansen J and
Brink C: Single arc volumetric modulated arc therapy of head and
neck cancer. Radiother Oncol. 95:142–148. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chan OS, Lee MC, Hung AW, Chang AT, Yeung
RM and Lee AW: The superiority of hybrid-volumetric arc therapy
(VMAT) technique over double arcs VMAT and 3D-conformal technique
in the treatment of locally advanced non-small cell lung cancer - a
planning study. Radiother Oncol. 101:298–302. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Quan EM, Li X, Li Y, Wang X, Kudchadker
RJ, Johnson JL, Kuban DA, Lee AK and Zhang X: A comprehensive
comparison of IMRT and VMAT plan quality for prostate cancer
treatment. Int J Radiat Oncol Biol Phys. 83:1169–1178. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kopp RW, Duff M, Catalfamo F, Shah D,
Rajecki M and Ahmad K: VMAT vs. 7-field-IMRT: Assessing the
dosimetric parameters of prostate cancer treatment with a
292-patient sample. Med Dosim. 36:365–372. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Guckenberger M, Richter A, Krieger T,
Wilbert J, Baier K and Flentje M: Is a single arc sufficient in
volumetric-modulated arc therapy (VMAT) for complex-shaped target
volumes? Radiother Oncol. 93:259–265. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bzdusek K, Friberger H, Eriksson K,
Hårdemark B, Robinson D and Kaus M: Development and evaluation of
an efficient approach to volumetric arc therapy planning. Med Phys.
36:2328–2339. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Solin LJ, Gray R, Goldstein LJ, Recht A,
Baehner FL, Shak S, Badve S, Perez EA, Shulman LN, Martino S, et
al: Prognostic value of biologic subtype and the 21-gene recurrence
score relative to local recurrence after breast conservation
treatment with radiation for early stage breast carcinoma: Results
from the Eastern Cooperative Oncology Group E2197 study. Breast
Cancer Res Treat. 134:683–692. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zagouri F, Liakou P, Bartsch R, Peccatori
FA, Tsigginou A, Dimitrakakis C, Zografos GC, Dimopoulos MA and
Azim HA Jr: Discrepancies between ESMO and NCCN breast cancer
guidelines: An appraisal. Breast. 24:513–523. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wong EK, Truong PT, Kader HA, Nichol AM,
Salter L, Petersen R, Wai ES, Weir L and Olivotto IA: Consistency
in seroma contouring for partial breast radiotherapy: Impact of
guidelines. Int J Radiat Oncol Biol Phys. 66:372–376. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Feuvret L, Noël G, Mazeron JJ and Bey P:
Conformity index: A review. Int J Radiat Oncol Biol Phys.
64:333–342. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ayata HB, Güden M, Ceylan C, Kücük N and
Engin K: Comparison of dose distributions and organs at risk (OAR)
doses in conventional tangential technique (CTT) and IMRT plans
with different numbers of beam in left-sided breast cancer. Rep
Pract Oncol Radiother. 16:95–102. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Jones R, Yang W, Read P and Sheng K:
Radiation therapy of post-mastectomy patients with positive nodes
using fixed beam tomotherapy. Radiother Oncol. 100:247–252. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hurkmans CW, Meijer GJ, van
Vliet-Vroegindeweij C, van der Sangen MJ and Cassee J: High dose
simultaneously integrated breast boost using intensity modulated
radiotherapy and inverse optimization. Int J Radiat Oncol Biol
Phys. 66:923–930. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
van der Laan HP, Dolsma WV, Maduro JH,
Korevaar EW, Hollander M and Langendijk JA: Three-dimensional
conformal simultaneously integrated boost technique for breast
conserving radiotherapy. Int J Radiat Oncol Biol Phys.
68:1018–1023. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Singla R, King S, Albuquerque K, Creech S
and Dogan N: Simultaneous integrated boost intensity modulated
radiation therapy (SIB-IMRT) in the treatment of early stage left
sided breast carcinoma. Med Dosim. 31:190–196. 2006. View Article : Google Scholar : PubMed/NCBI
|