Introduction
Brunner's glands are submucosal mucin-secreting
glands that were first characterized by Brunner in 1688. The glands
have been observed between the pylorus and the jejunum (1), mainly in the first and second regions of
the duodenum, usually in individuals aged 40–60 years (2).
Brunner's gland cysts are rare, benign polypoid,
nodular mass lesions arising from Brunner's glands, with no
associated underlying malignancy (3–5). Only 13
cases have been reported in the literature (6,7). Certain
cases appear to present as a cystic dilatation of the Brunner's
gland ducts in association with hamartoma (8). Brunner's gland cysts are detected
incidentally and are usually asymptomatic (9,10).
Brunner's gland cyst of the duodenum may be removed by endoscopy,
and is one of the most cost-effective approaches of resection
(11). Furthermore, surgical
resection via a laparoscopic approach or laparotomy is required for
complete resection in cases where the tumor is too large to be
resected by endoscopy or if malignancy is suspected (12).
Gastrointestinal stromal tumor (GIST) is a rare
stromal tumor that accounts for 0.1–3.0% of all gastrointestinal
tumors arising from the interstitial cells of Cajal or the common
intestinal mesenchymal precursor cells (13). GISTs are observed in adults >40
years old (range, 55–60 years), but rarely in children. The
majority of GISTs are located in the stomach (55.6%) and small
intestine (31.8%), and 1 in 5 GISTs are detected incidentally
(14,15). The most common symptoms of the disease
are abdominal pain, gastrointestinal bleeding and obstruction,
together with other non-specific presentation (14). The treatment of GIST includes
molecularly targeted therapy and surgery. Although immunotherapy
has had profound effects on the management of these type of tumors,
surgery remains the optimal treatment approach for GIST based on
expert consensus, with optimistic outcomes following surgery
(16–19).
The present study reports the case of a patient with
Brunner's gland cyst in combination with a GIST and reviews the
clinical presentations, pathological features and therapy.
Case report
A 58-year-old female was admitted to Tianchang
Hospital of Traditional Chinese Medicine (Tianchang, China) on 19
July, 2014, with a one-month history of epigastric abdominal
discomfort, diarrhea and recurrent vomiting following the intake of
food. The feces of the patient occasionally appeared similar to
yellow jelly. A review of the body's systems and past medical
history of the patient, and the findings of physical examination
and routine laboratory tests performed were not notable. The body
temperature of the patient was 37.2°C (normal range, 36–37°C),
blood pressure was 130/77 mmHg (normal range, 90–140/60–90 mmHg)
and radial pulse rate was 70 beats/min and regular (normal range,
60–100 beats/min). A complete blood count revealed a red blood cell
count of 321×104 cells/µl (normal range,
350–500×104 cells/µl), hemoglobin concentration of 9.1
g/dl (normal range, 13.5–17.6 g/dl), and mean corpuscular volume of
87 fl (normal range, 80–100 fl).
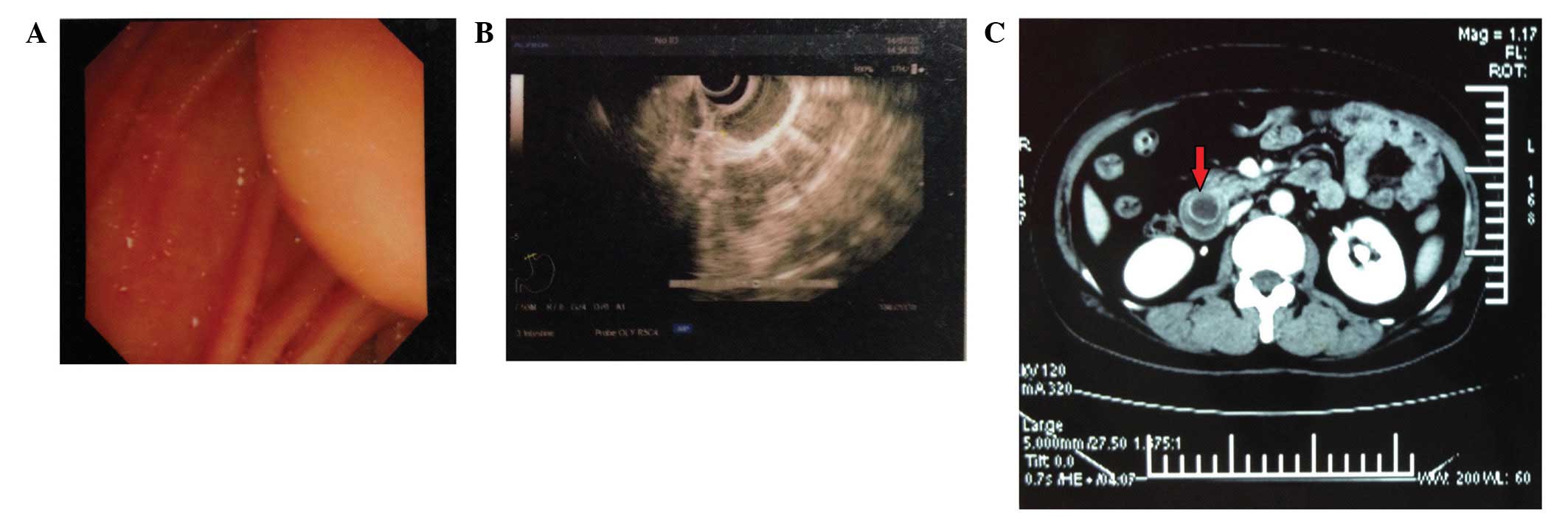
Upper gastrointestinal endoscopy was performed on 19
July 2014 and revealed the presence of a cap mass at the descending
region of the duodenum (Fig. 1A). A
computed tomography (CT) scan revealed a round, cystic-like lesion
with low internal density located within the duodenum (Fig. 1C). The patient underwent treatment
with norfloxacin (0.3 g, administered orally 2 times a day for 3
days) and support treatment (500 ml of 5% glucose normal saline,
500 ml Sodium Lactate Ringer's Injection, 30 ml of 10% KCl and 20
ml of 10% NaCl mixed into a single infusion bag, and administered
every day for 2 days by intravenous infusion). Following
administration, the diarrhea, nausea and vomiting stopped, but the
abdominal pain remained. The patient underwent endoscopic
ultrasound, which revealed the presence of a half-globular,
submucosal, low-echo cystic conglomeration in the wall of the
duodenum, near the duodenal bulb (Fig.
1B). The cyst originated from the muscle layer and its
cross-sectional size was 2.37×1.20 cm. A differential diagnosis of
GIST was provided, and the patient was admitted to the First
Affiliated Hospital of Nanjing Medical University (Nanjing,
Jiangsu, China) on 12 August, 2014, to confirm the diagnosis and
receive treatment. Considering the size and position of the mass,
the patient underwent surgical exploration and tumor resection
instead of endoscopic management. The surgery was performed on 14
August 2014. During surgery, a submucosal cyst was identified and
transduodenal local resection was performed. The specimen was
histopathologically examined.
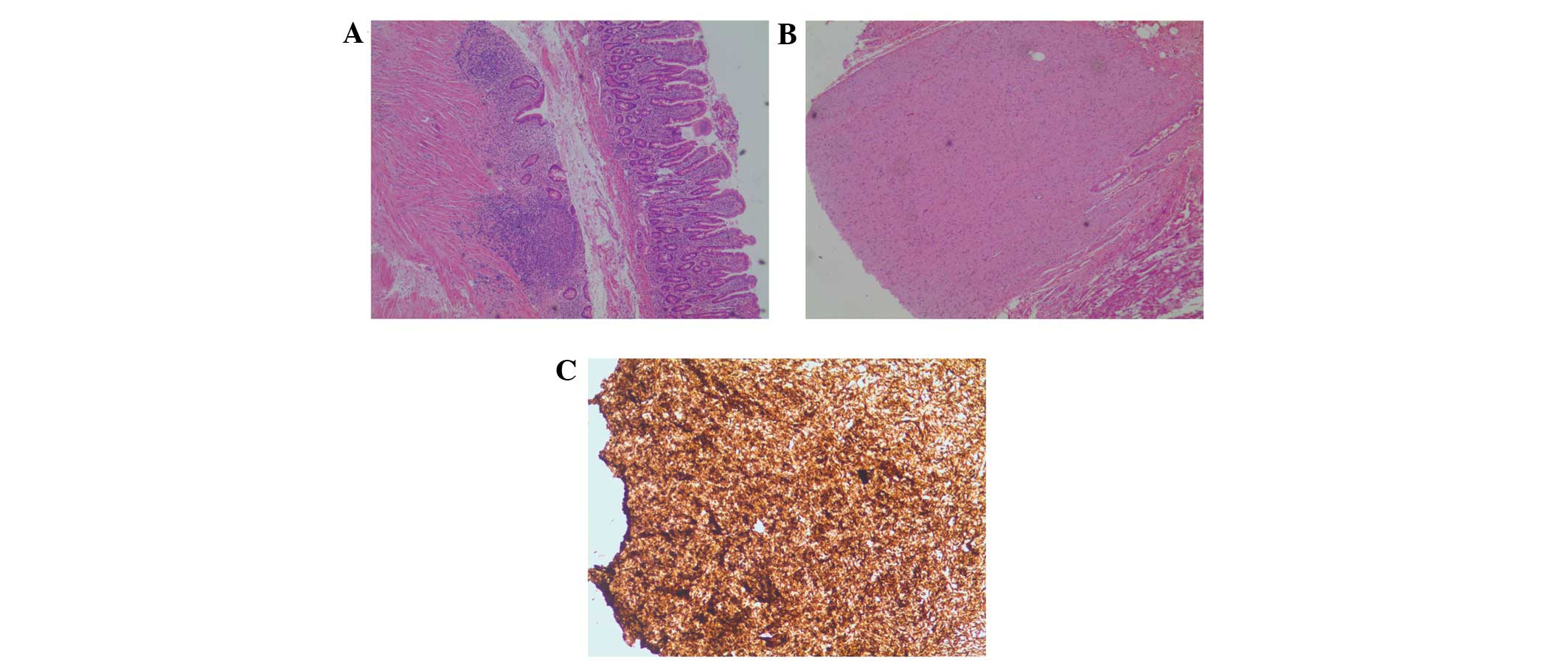
The mass was surgically resected and the specimen
was histopathologically examined using a OLYMPUS BX43 microscope
(Olympus Corporation, Tokyo, Japan) subsequent to staining with
hematoxylin and eosin (Fuzhou Maixin Biotech Co., Ltd., Fuzhou,
China). The typical appearance of the mass was a soft, submucosal
cyst measuring 3.0×2.0×2.0 cm in size that ruptured during biopsy.
The mass was full of fluid and flocculent precipitate. Microscopy
revealed that the tumor was composed of Brunner's glands. The
surface epithelium of the duodenum was normal. Chronic duodenal
mucosal inflammation with lymphoid tissue hyperplasia was observed
in the mass, but no dysplasia or malignancy was observed.
Adenomatous hyperplasia of the spindle cells was
identified inside a small nidus, which was extremely close to the
cyst and measured ~0.3 cm in diameter. The small nidus was resected
with the cyst during surgery. Additional immunohistochemistry was
performed using the following antibodies: Monoclonal rabbit cluster
of differentiation (CD)117 (catalog no., RMA-0632), mouse CD34
(catalog no., Kit-0004), rabbit discovered on GIST-1 (DOG-1;
catalog no., Kit-0035), mouse S-100 (catalog no., Kit-0007), mouse
desmin (catalog no., Kit-0023), mouse α-smooth muscle actin (SMA;
catalog no., Kit-0006), and mouse Ki-67 (catalog no., Kit-0005),
which were all purchased from Fuzhou Maixin Biotech Co., Ltd.. All
antibodies were ready-to-use products and did not require further
dilution. Succinate dehydrogenase complex iron-sulfur subunit B
(SDHB) was used for immunostaining. The mass clearly expressed CD34
(Fig. 2C), while DOG-1, S-100, desmin
and SMA were not expressed. A final diagnosis of extremely low-risk
type GIST was provided, which was based on the mitotic index, tumor
size, location and peritoneal deposits. The mitotic index was
calculated according to a mitosis count of 50 high-power field
(HPF) (20). The mitosis count of the
current patient was 2–3/50 HPFs, indicating a low risk of
aggressive behavior. Therefore, the lesion was diagnosed as a
Brunner's gland adenoma in combination with a GIST. The patient
received norfloxacin as an anti-infective therapy, and was
administered glucose and sodium chloride solution with electrolytes
as a support treatment (using same dose and duration as initial
treatment). The patient was discharged 2 weeks post-surgery, and
during the 12 month follow-up period, the outcome was good.
Discussion
Brunner's glands were first characterized by Brunner
in 1688, and are alkaline-secreting glands located in the
submucosal layer of the duodenum (21). The glands have been observed in
ectopic locations, such as the pylorus and jejunum, but the
majority of Brunner's glands are located in the first region of the
duodenum (1). Brunner's gland cysts
have also been termed cyst of Brunner's glands (22), Brunner's gland cystadenoma (23), Brunner's cyst (24), cystic hamartoma of Brunner's glands
(25), mucocele of Brunner's glands
(26) and cystic Brunner's gland
hamartoma (27).
Brunner's gland cysts are usually detected
incidentally (2,28), including in the case reported in the
present study. The etiology of Brunner's gland cyst has not been
fully elucidated; however, the cysts are hypothesized to arise as a
result of obstruction to a major Brunner's gland duct (29). In Brunner's gland cysts, Brunner's
glands may be mildly dilated, but predominantly the cysts consist
of hyperplastic lobules of Brunner's gland acini, without
cystically dilated spaces. By contrast, hyperplasia of the
Brunner's glands is not often observed in Brunner's gland cysts
(30,31). The cysts typically appear as soft,
submucosal lesions that rupture during biopsy (32). These cysts are not composed of solid
aggregates of Brunner's glands, and are occasionally mixed with
fibromuscular, adipose and lymphoid tissues, unlike classic
Brunner's gland hamartoma (6,33). Brunner's gland cysts are benign, with
no associated underlying malignancy, and may be excised
endoscopically or surgically, depending on the size and location of
the cyst (11,12). Although Brunner's gland cysts are
often identified incidentally, in symptomatic patients the most
common symptoms are gastrointestinal hemorrhage and obstructive
symptoms (6,32).
Diagnosing Brunner's gland cyst is challenging. It
should be distinguished from other duodenal lesions, including
Brunner's gland hamartoma, duplication cysts, pancreatic
pseudocysts, cystic dystrophy arising in heterotopic pancreatic
tissue, aberrant pancreatic tissue, leiomyoma, polypoid adenoma of
the superficial mucosal glands and malignant tumors (10,33–35). The
soft and submucosal appearance and the rupture or flattening of the
lesions following endoscopic biopsies may aid in diagnosing
Brunner's gland cyst. However, a final diagnosis of Brunner's gland
cyst is based on pathological findings of resected lesions obtained
by endoscopic mucosal resection, polypectomy or surgical treatment
(10,36). Pathologically, Brunner's gland cysts
are typically confined to the submucosa and consist of a single
layer of connective tissue and epithelial cells, which are composed
of columnar cells containing basal round nuclei and granular
cytoplasm (37). Cystic configuration
of a solitary duodenal mass should allow differentiation of
Brunner's gland cysts from other duodenal lesions (37).
Endoscopic or surgical removal of Brunner's gland
cyst may prevent the development of complications (38,39).
Endoscopic tumorectomy is the ideal surgical procedure for
Brunner's gland cyst and Brunner's gland adenoma resection,
depending on the region and size of the mass and the presence of a
peduncle (40). In the present study,
considering the size and distal location of the mass, a tumorectomy
was performed.
GISTs are rare stromal tumors that account for
0.1–3.0% of all gastrointestinal tumors, which are hypothesized to
arise from the interstitial cells of Cajal or the common intestinal
mesenchymal precursor cells (41).
In 95% of GISTs, positive immunohistochemical
staining is observed for CD117 and DOG-1, whilst 70% are positive
for CD34 (18,42). Patients with GISTs may present in
various forms and GISTs are often diagnosed incidentally.
Symptomatic patients tend to possess large tumors with a mean size
of 6.0 cm, compared with 2.0-cm masses in asymptomatic patients and
1.5-cm masses in patients that are diagnosed with GIST at autopsy
(43).
In conclusion, the present study reports a case of a
Brunner's gland cyst of the duodenum in combination with a GIST at
the same position, which, to the best of our knowledge, has not
previously been reported. Brunner's gland cyst should be considered
as a differential diagnosis of duodenal masses. The existence of
Brunner's gland cyst is not yet known to be associated with the
presence of GISTs. Consequently, considering the possible causes of
mucosal damage, including mechanical stimuli, Helicobacter
pylori infection and hyper acidic environment in the duodenum,
the mechanism and association of Brunner's gland cyst with GIST
require additional investigation.
References
|
1
|
Kaplan EL, Dyson WL and Fitts WT:
Hyperplasia of Brunner's glands of the duodenum. Surg Gynecol
Obstet. 127:371–375. 1968.
|
|
2
|
Sande-Lemos Azcue MP, Shaoul R, Cutz E and
Sherman PM: Nodular duodenum after pediatric renal transplant due
to Brunner's gland hyperplasia. J Pediatr Gastroenterol Nutr.
27:452–456. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Brookes MJ, Manjunatha S, Allen CA and Cox
M: Malignant potential in a Brunner's gland hamartoma. Postgrad Med
J. 79:416–417. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fujimaki E, Nakamura S, Sugai T and Takeda
Y: Brunner's gland adenoma with a focus of p53-positive atypical
glands. J Gastroenterol. 35:155–158. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Matsui T, Iida M, Fujischima M, Sakamoto K
and Watanabe H: Brunner's gland hamartoma associated with
microcarcinoids. Endoscopy. 21:37–38. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Powers M, Sayuk GS and Wang HL: Brunner
gland cyst: Report of three cases. Int J Clin Exp Pathol.
1:536–538. 2008.PubMed/NCBI
|
|
7
|
Park BJ, Kim MJ, Lee JH, Park SS, Sung DJ
and Cho SB: Cystic Brunner's gland hamartoma in the duodenum: A
case report. World J Gastroenterol. 15:4980–4983. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee J, Park CM, Kim KA, Lee CH, Choi JW,
Shin BK, Lee SJ, Choi D and Jang KT: Cystic lesions of the
gastrointestinal tract: Multimodality imaging with pathologic
correlations. Korean J Radiol. 11:4572010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Levine JA, Burgart LJ, Batts KP and Wang
KK: Brunner's gland hamartomas: Clinical presentation and
pathological features of 27 cases. Am J Gastroenterol. 90:290–294.
1995.PubMed/NCBI
|
|
10
|
Patel ND, Levy AD, Mehrotra AK and Sobin
LH: Brunner's gland hyperplasia and hamartoma: Imaging features
with clinicopathologic correlation. AJR Am J Roentgenol.
187:715–722. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gao YP, Zhu JS and Zheng WJ: Brunner's
gland adenoma of duodenum: A case report and literature review.
Word J Gastroenterol. 10:2616–2617. 2004. View Article : Google Scholar
|
|
12
|
Stewart ZA, Hruban RH, Fishman EF and
Wolfgang CL: Surgical management of giant Brunner's gland
hamartoma: Case report and literature review. World J Surg Oncol.
7:682009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Miettinen M and Lasota J: Gastrointestinal
stromal tumors - definition, clinical, histological,
immunohistochemical, and molecular genetic features and
differential diagnosis. Virchows Arch. 438:1–12. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Soreide K, Sandvik OM, Soreide JA, Giljaca
V, Jureckova A and Bulusu VR: Global epidemiology of
gastrointestinal stromal tumours (GIST): A systematic review of
population-based cohort studies. Cancer epidemiology. 40:39–46.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Watson GA, Kelly D, Melland-Smith M,
Gleeson J, McEntee G, Kelly CM and McCaffrey JA: Get the GIST? An
overview of gastrointestinal stromal tumours. Ir J Med Sci.
February 01–2016.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Demetri GD, von Mehren M, Antonescu CR, De
Matteo RP, Ganjoo KN, Maki RG, Pisters PW, Raut CP, Riedel RF,
Schuetze S, et al: NCCN Task Force report: Update on the management
of patients with gastrointestinal stromal tumors. J Natl Compr Canc
Netw. 8(Suppl 2): S1–41. 2010.PubMed/NCBI
|
|
17
|
ESMO/European Sarcoma Network Working
Group: Gastrointestinal stromal tumours: ESMO Clinical Practice
Guidelines for diagnosis, treatment and follow-up. Ann Oncol.
25(Suppl 3): iii21–iii26. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nishida T, Hirota S, Yanagisawa A, Sugino
Y, Minami M, Yamamura Y, Otani Y, Shimada Y, Takahashi F and Kubota
T: GIST Guideline Subcommittee: Clinical practice guidelines for
gastrointestinal stromal tumor (GIST) in Japan: English version.
Int J Clin Oncol. 13:416–430. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yeh CN, Hwang TL, Huang CS, Lee PH, Wu CW,
Chen-Guo K, Jan YY and Chen MF: Taiwan Surgical Society of
Gastroenterology: Clinical practice guidelines for patients with
gastrointestinal stromal tumor in Taiwan. World J Surg Oncol.
10:2462012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Joensuu H: Risk stratification of patients
diagnosed with gastrointestinal stromal tumor. Hum Pathol.
39:1411–1419. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Landboe-Christensen E: Staining of the
duodenal glands of Brunner in gross specimens of the duodenum in
man. Acta Pathologica Microbiologica Scandinavica. 21:374–379.
1944. View Article : Google Scholar
|
|
22
|
Hately W: Cyst of Brunner's glands. Br J
Radiol. 41:384–385. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wolk DP, Knapper WH and Farr GH: Brunner's
gland cystadenoma of the duodenum. Am J Surg. 126:439–440. 1973.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Taura M, Taura S, Kummerow FA, Noritomi S
and Iwanaga S: An ultrastructural study of the Brunner's cyst.
Gastroenterol Jpn. 12:241–244. 1977.PubMed/NCBI
|
|
25
|
Golan J, Dollberg L, Dollberg M, Farkash T
and Rivkin L: Cystic hamartoma of Brunner's glands. Int Surg.
63:173–175. 1978.PubMed/NCBI
|
|
26
|
Fisher JK: Mucocele of a Brunner gland.
Radiology. 136:3201980. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yamakawa M, Murata I, Yamao T, Kawai K and
Kohno S: Cystic Brunner's gland hamartoma. Gastrointest Endosc.
57:9192003. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Galiatsatos P: A case of mistaken lipoma.
Diagnosis: Brunner gland cyst. Gastroenterology. 141:1159–1160,
1533. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Varnholt H, Gang DL, Desilets DJ and
Pantanowitz L: Brunner gland cyst. Int J Surg Pathol. 15:64–65.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zanetti G and Casadei G: Brunner's gland
hamartoma with incipient ductal malignancy. Report of a case.
Tumori. 67:75–78. 1981.PubMed/NCBI
|
|
31
|
Kim K, Jang SJ, Song HJ and Yu E:
Clinicopathologic characteristics and mucin expression in Brunner's
gland proliferating lesions. Dig Dis Sci. 58:194–201. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chatelain D, Maillet E, Boyer L, Checkouri
G, Mourra N and Flejou JF: Brunner gland hamartoma with predominant
adipose tissue and ciliated cysts. Arch Pathol Lab Med.
126:734–735. 2002.PubMed/NCBI
|
|
33
|
Walden DT and Marcon NE: Endoscopic
injection and polypectomy for bleeding Brunner's gland hamartoma:
Case report and expanded literature review. Gastrointest Endosc.
47:403–407. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chattopadhyay P, Kundu AK, Bhattacharyya S
and Bandyopadhyay A: Diffuse nodular hyperplasia of Brunner's gland
presenting as upper gastrointestinal haemorrhage. Singapore Med J.
49:81–83. 2008.PubMed/NCBI
|
|
35
|
Schluger LK, Rotterdam H and Lebwohl O:
Gastrointestinal hemorrhage from a Brunner's gland hamartoma. Am J
Gastroenterol. 89:2088–2089. 1994.PubMed/NCBI
|
|
36
|
Krishnamurthy P, Junaid O, Moezzi J, Ali
SA and Gopalswamy N: Gastric outlet obstruction caused by Brunner's
gland hyperplasia: case report and review of literature.
Gastrointest Endosc. 64:464–467. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Nishida T, Blay JY, Hirota S, Kitagawa Y
and Kang YK: The standard diagnosis, treatment, and follow-up of
gastrointestinal stromal tumors based on guidelines. Gastric
Cancer. 19:3–14. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Coriat R, Mozer-Bernardeau M, Terris B,
Chryssostalis A, Prat F and Chaussade S: Endoscopic resection of a
large Brunner's gland hamartoma. Gastroenterologie Clinique et
Biologique. 32:11–14. 2008.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Janes SE, Zaitoun AM, Catton JA, Aithal GP
and Beckingham IJ: Brunner's gland hyperplasia at the ampulla of
Vater. J Postgrad Med. 52:38–40. 2006.PubMed/NCBI
|
|
40
|
Rocco A, Borriello P, Compare D, De
Colibus P, Pica L, Iacono A and Nardone G: Large Brunner's gland
adenoma: Case report and literature review. World J Gastroenterol.
12:1966–1968. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Kindblom LG, Remotti HE, Aldenborg F and
Meis-Kindblom JM: Gastrointestinal pacemaker cell tumor (GIPACT):
Gastrointestinal stromal tumors show phenotypic characteristics of
the interstitial cells of Cajal. Am J Pathol. 152:1259–1269.
1998.PubMed/NCBI
|
|
42
|
Miettinen M, Wang ZF, Sarlomo-Rikala M,
Osuch C, Rutkowski P and Lasota J: Succinate
dehydrogenase-deficient GISTs: A clinicopathologic,
immunohistochemical, and molecular genetic study of 66 gastric
GISTs with predilection to young age. Am J Surg Pathol.
35:1712–1721. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kindblom LG: Gastrointestinal stromal
tumors: Diagnosis, epidemiology and prognosis. ASCO Annual Meeting
(Chicago). May 31;-June 3. 2003.
|