Introduction
Follicular thyroid carcinoma (FC) is the second most
common malignancy of the thyroid, and accounts for ~10% of all
thyroid malignancies (1). FC
predominantly affects elderly females (2). Follicular adenomas are more common than
follicular carcinomas (3,4). In contrast to adenomas, carcinomas
exhibit microscopic vascular or capsular invasion (5). Follicular carcinoma patients with
extensive vascular invasion exhibit a poorer prognosis, and distant
metastases are occasionally present (5–8).
Hematogenous metastasis is most commonly observed, via the systemic
circulation or the paravertebral plexus. Lymphatic spread, which is
less common, is also possible. Distant metastases are more common
in FC than in papillary thyroid carcinoma (PC) (9). Furthermore, distant metastasis occurs in
>20% of FC cases and lung and bone metastases are common
(10–12). However, FC metastasis to the kidney is
rare (1). Ultrasound is useful for
the evaluation of thyroid nodules due to its high resolution, lack
of radiation exposure, portability and ease of use (13,14). A
number of retrospective studies have investigated the features of
follicular carcinomas exhibited on ultrasound. Calcifications are
common features of thyroid malignancies. Previously, eggshell
calcifications were considered an indicator of benign tumors
(15). However, cases of PC
associated with this type of calcification have been reported
(16,17). To the best of our knowledge, only a
small number of cases of follicular carcinoma with an eggshell
calcification have been reported in the literature (18). The present study reports a case of FC
with metastasis to the kidney in a patient exhibiting widespread
dissemination of the disease.
Case report
In July 2010, a 67-year-old woman was referred to
the Department of Urinary Surgery, West China Hospital of Sichuan
University (Chengdu, China) upon being diagnosed with a solitary
tumor in the left kidney at Chengdu No. 1 People's Hospital
(Chengdu, China). The present study was performed in accordance
with the Declaration of Helsinki, and was approved by the Ethics
Committee of Sichuan University. Written informed consent was
obtained from the patient. Physical examination and laboratory
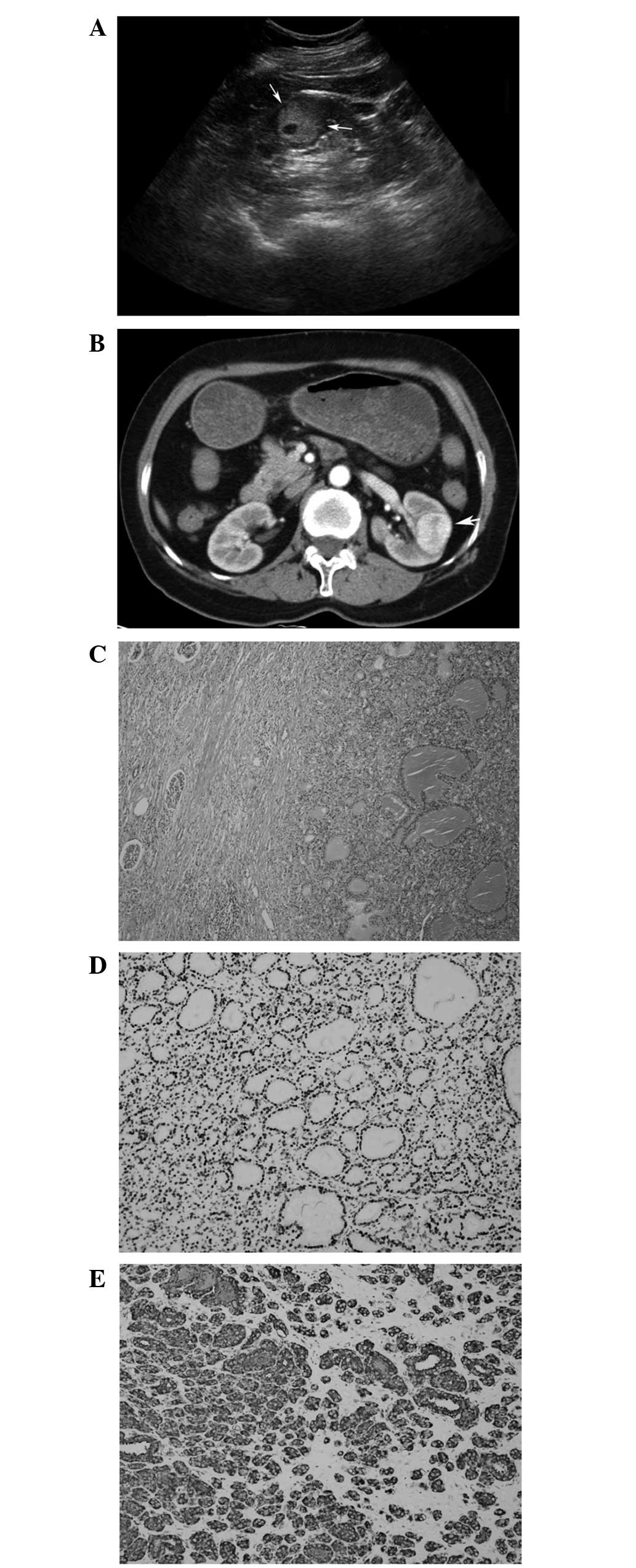
tests were normal. Ultrasound (US; iU22; C5–2 MHz convex transduced
and L12–5 MHz linear probe; Philips Healthcare, Bothell, WA, USA)
examination revealed a solitary heterogeneous hyperechoic mass with
an interior irregular anechoic area located in the mid pole of the
left kidney (Fig. 1A). The shape of
the tumor was regular and the margin was circumscribed. The size of
the tumor was 2.8×2.3×2.5 cm, and there were no internal color
Doppler signals. The patient was additionally examined by
contrast-enhanced computed tomography (CECT; Philips Brilliance;
Philips Medical Systems, Cleveland, OH, USA), and the preoperative
diagnosis was suspected to be primary malignancy of the left kidney
(Fig. 1B). Therefore, the patient
underwent a left radical nephrectomy. Hematoxylin and eosin stained
sections of the dissected surface of the resected mass were
evaluated using a BX51 Olympus microscope (Olympus Corporation,
Tokoyo, Japan), which revealed a distinct puce color and focal
hemorrhagic necrotic contents. The postoperative pathological
diagnosis was metastatic FC (Fig.
1C–E). Six months later, the patient was readmitted to the West
China Hospital of Sichuan University for thyroid surgery.
The patient's initial clinical manifestation of the
disease was a sensation of cold or occasional heat, with no dyspnea
or dysphagia. On palpation, a moderately tender mass with an
irregular and rough surface was identified in the right lobe of the
thyroid, which was observed to move during deglutition. No regional
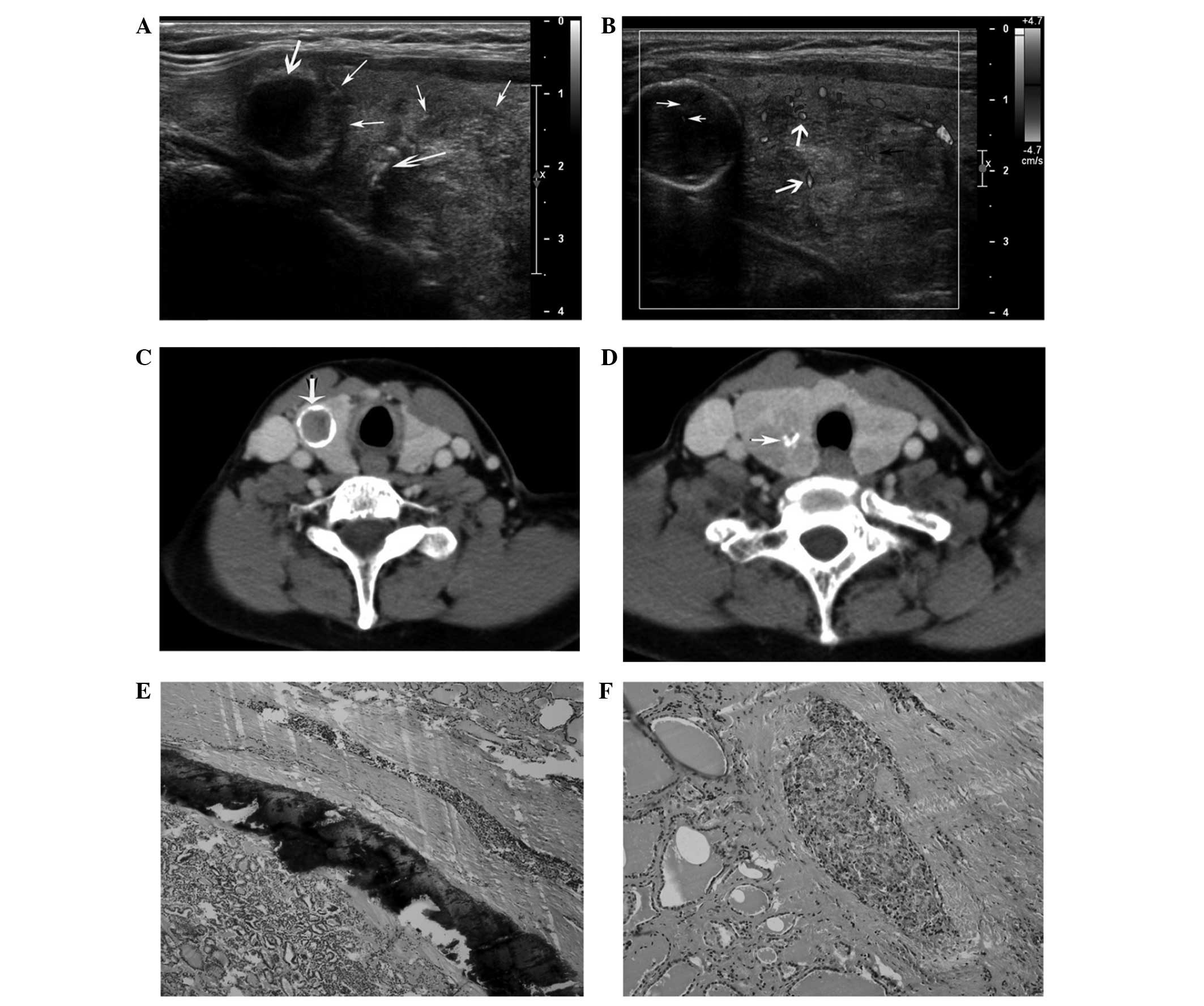
lymphadenopathy was noted. US examination with a high-frequency
linear probe transducer (12.5 MHz) revealed a hypoechoic lesion
with eggshell calcification and incomplete halo in the upper pole
of the right lobe of the thyroid gland. Simultaneously, a
hyperechoic lesion with heterogeneous enhancement was noted in the
mid pole of the thyroid, which presented macrocalcifications and an
incomplete halo. The size of the lesion located in the upper pole
of the thyroid was 2.5×2.3×2.5 cm, and the size of the lesion in
the mid pole was 2.9×2.5×3.4 cm. The shape of the upper lesion was
regular and its margin was circumscribed, while the shape of the
lower lesion was irregular and its margin was ill-defined. The
eggshell calcification was continuous, with marked echo attenuation
at the back of the upper lesion (Fig.
2A). Doppler study revealed the presence of a punctiform and an
irregular-distribution blood flow signal in the upper and lower
lesion, respectively (Fig. 2B).
Doppler-like blood flow was noted inside the lesion, with a high
resistance index of Doppler waveform. CECT of the neck revealed an
upper lesion exhibiting low density in the right lobe of the
thyroid, with a high density of calcification in the margins, and
an additional lower lesion with low density, macrocalcifications,
circumscribed margin and incomplete halo (Fig. 2C and D). Thyroid profile demonstrated
levels of thyroid stimulating hormone (TSH), 0.74 mU/l (normal,
0.27–4.20 mU/l); free triiodothyronine, 6.40 pmol/l (normal,
3.60–7.50 pmol/l); free thyroxine, 16.08 pmol/l (normal,
12.00–22.00 pmol/l); human thyroglobulin (hTG), 52.48 µg/l (normal,
1.40–78.00 µg/l); anti-TG antibody (TgAb), 15.89 IU/ml (normal,
<115.00 IU/ml); and anti-thyroid peroxidase (TPO)Ab, 12.84 IU/ml
(normal, <34.00 IU/ml). The patient's levels of serum bone
alkaline phosphatase were markedly increased (38.78 µg/l; normal,
11.40–24.60 µg/l). The patient underwent total thyroidectomy and
subsequent excision of the cervical lymph node of the central zone
of the thyroid.
During surgery, the thyroid was observed to be
markedly hyperemic, with abundant vasa vasorum. The dissected
surface of the two lesions in the right lobe of the thyroid
exhibited distinct white contents, without haemorrhagia or
necrosis. Two lymph nodes of ~0.5 cm in diameter located behind the
trachea were also excised. The postoperative pathological results
of the two lesions confirmed the diagnosis of FC, while the
resected lymph nodes did not display infiltration (Fig. 2E and F). Postoperative laboratory
tests revealed serum levels of TSH, 3.19 pmol/l; calcium, 1.90
mmol/l (normal, 2.10–2.70 mmol/l); magnesium, 0.77 mmol/l (normal,
0.67–1.04 mmol/l); inorganic phosphorus, 0.74 mmol/l (normal,
0.81–1.45 mmol/l); and calcitonin, 1.40 pg/ml (normal, 0.07–12.97
pg/ml). The patient experienced a favorable postoperative recovery,
and was readmitted to the West China Hospital of Sichuan University
for radionuclide therapy two months later. Radioactive
131I (Chengdu Gaotong Isotope Co., Ltd., Chengdu, China)
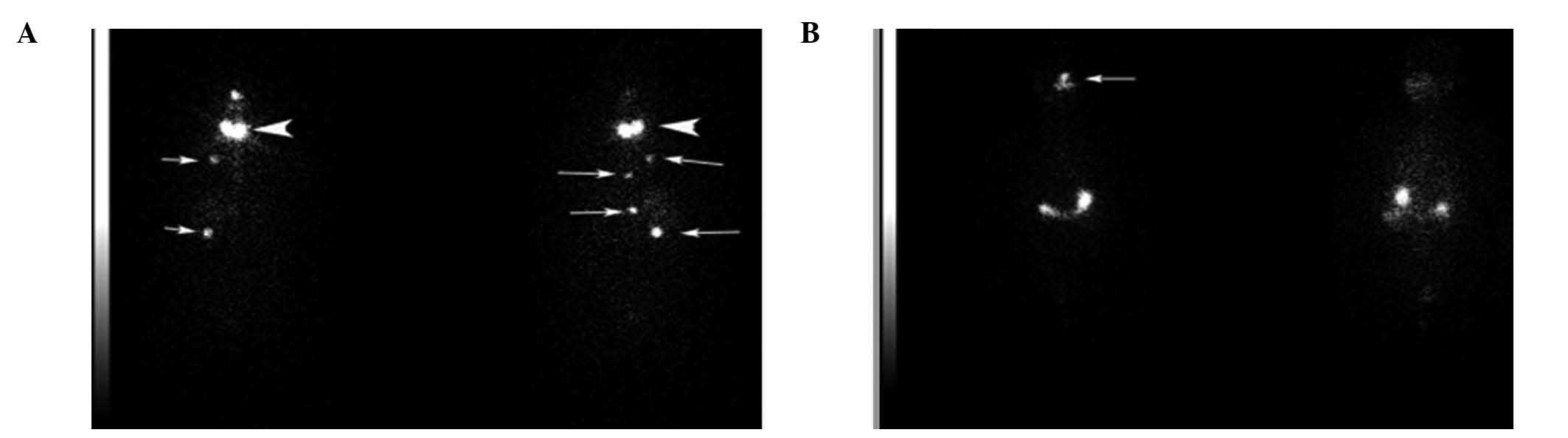
uptake by the thyroid was determined to be 3.7% in 24 h using a
Precedence SPECT/CT Imaging System (Philips Healthcare). A small
number of parenchyma cells corresponding to remnants of the thyroid
were identified in the thyroid region. Following administration of
an oral therapeutic dose of 100 mCi 131I, functional
imaging of the parenchyma remnants in the thyroid and cervical
region revealed the presence of multifocal metastases in the chest
and abdomen (Fig. 3A). Further
treatment with thyroid suppression therapy using oral
Euthyrox® (100 µg; Merck KGaA, Darmstadt, Germany) was
administered daily. The patient underwent functional imaging
therapy with oral 131I six months later, which
demonstrated the disappearance of the multifocal metastases
(Fig. 3B). The thyroid profile
results demonstrated revealed levels of TSH, 79.06 mU/l; TgAb,
19.90 IU/ml; TPOAb, 19.47 IU/ml; and hTG, 0.74 µg/l.
The patient was last observed during follow-up in
July 2013, and the patient was alive and well. Following this the
patient was lost to follow-up.
Discussion
FC is usually more aggressive and metastasizes more
frequently than PC (10). Metastasis
of FC to the bones and lungs are common, while metastasis to other
tissues and organs, including the kidney, skin and skull base, is
rare (19–22). FC differs from PC in its main route of
metastasis, since FC primarily metastasizes via the blood, whereas
PC primarily metastasizes via the lymphatic system (23), which explains why the incidence of
cervical lymphadenopathy in FC is lower than in PC (24). In the present case, the cervical lymph
nodes were not infiltrated, as confirmed by postoperative
pathological examination.
High-frequency US is an important method for
examining thyroid nodules (25). FC
is frequently misdiagnosed as follicular thyroid adenoma (FTA), due
to the similar characteristics displayed by FTA and FC in US
imaging (9). Particularly, the
presence of cervical lymphadenopathy is an indirect sign of
carcinoma in US diagnosis (23).
Metastasis is often the initial symptom of FC, since patients
usually remain asymptomatic in regards to thyroid function
(1). This leads to metastases
frequently being misdiagnosed as primary tumors until the
postoperative pathological examination confirms the primary lesion
to be FC (19), as occurred in the
present case.
The presence of two FC lesions located in the same
lobe of the thyroid, with multiple foci and low occurrence rate,
has been previously reported in the literature (26), in contrast to the frequent
multicentricity observed in PC (27).
In the present case, one lesion displayed continuous peripheral
eggshell calcification, while the other lesion exhibited
macrocalcifications. It is well known that calcification may occur
in benign and malignant thyroid lesions (28). To date, three distinct representations
of intrathyroidal calcification have been described: Eggshell,
dystrophic and fine stippled psammomatous calcification (29). Psammomatous calcification is typically
suggestive of PC (30,31), while eggshell calcification, including
Hürthle cell carcinoma, is rare and usually considered benign
(32). However, Yaturu and Rainer
(33) have reported that eggshell
calcification does not exclude the presence of cancer. Furthermore,
previous studies have confirmed the occurrence of eggshell
calcification in FC (34–36). Therefore, the presence of eggshell
calcification is not a specific method to distinguish between
benignancy and malignancy (15). Seo
et al (37) reported that
margin calcification is more common in FC than in FTA. In the
present case, the lesion exhibiting eggshell calcification also
displayed punctiform blood flow signals, in agreement with previous
findings by Lee and Rho (35). In
previous studies, a lesion with characteristics of FC, including
solid echogenicity, ill-defined margins, incomplete halo and
macrocalcifications, was identified by US (32,35,38,39).
In addition, the mass displayed a hyperechoic appearance, which is
common in FC (27,37). Previous studies have confirmed that
the internal signal displayed by FC lesions in color Doppler flow
imaging is a risk factor for the diagnosis of FC by US (37,40–42).
Additionally, the patient's gender and age have also been
associated with an increased risk of being diagnosed with FC
(37,43,44).
Fine-needle aspiration (FNA) biopsy has provided a
cost-effective and minimally invasive method of determining the
presence of malignancy in thyroid nodules, or the risk of
developing it (45). Unlike PC, which
may be accurately diagnosed by US using FNA biopsy, a diagnosis of
FC typically requires an assessment of vascular or capsular
invasion, which must be confirmed by histological evaluation
(46). Consequently, a diagnosis of
FC may only be suspected from FNA biopsies (46). Due to the clinical features of FC, it
is important to improve the accuracy of the diagnosis of FC by US,
which is currently the main method used to detect thyroid nodules
(46). Thus, improved detection
methods may reduce misdiagnosis rates of primary FC of thyroid
nodules or metastasis to other tissues and organs.
In conclusion, FC often presents at a higher tumor
stage, with distant metastases in 25–30% of cases, which is most
commonly observed in the lung and bone. However, other metastatic
sites have also been reported. Given the rarity of FC metastasis to
the kidney, the present case was diagnostically challenging, since
the identification of distant metastases may represent initial
symptoms of the disease. A renal solitary malignancy should be
considered with metastasis pre-surgery and a general check is
required, which was observed in the present patient; there was
widespread dissemination of FC metastasis pre-surgery. Radioiodine
and chronic thyroid-stimulating hormone suppression are effective
treatments for widespread metastases, and US is the most important
imaging tool for diagnosing thyroid disease. US imaging
characteristics of FC may appear atypical during thyroid
examination. Therefore, various risk factors should be considered
when diagnosing thyroid nodules, including the patient's gender and
age.
References
|
1
|
Sampson E, Brierley JD, Le LW, Rotstein L
and Tsang RW: Clinical management and outcome of papillary and
follicular (differentiated) thyroid cancer presenting with distant
metastasis at diagnosis. Cancer. 110:1451–1456. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Xu H, Zeng W and Tang Y: Metastatic
thyroid follicular carcinoma presenting as a primary renal tumor.
Intern Med. 51:2193–2196. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Carpi A, Nicolini A, Gross MD, Fig LM,
Shapiro B, Fanti S, Rampin L, Polico C and Rubello D: Controversies
in diagnostic approaches to the indeterminate follicular thyroid
nodule. Biomed Pharmacother. 59:517–520. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Goldstein RE, Netterville JL, Burkey B and
Johnson JE: Implications of follicular neoplasms, atypia, and
lesions suspicious for malignancy diagnosed by fine-needle
aspiration of thyroid nodules. Ann Surg. 235:656–662. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sobrinho-Simões M, Eloy C, Magalhães J,
Lobo C and Amaro T: Follicular thyroid carcinoma. Mod Pathol.
24(Suppl 2): S10–S18. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Benbassat CA, Mechlis-Frish S and Hirsch
D: Clinicopathological characteristics and long-term outcome in
patients with distant metastases from differentiated thyroid
cancer. World J Surg. 30:1088–1095. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Angeles-Angeles A, Chable-Montero F,
Martinez-Benitez B and Albores-Saavedra J: Unusual metastases of
papillary thyroid carcinoma: Report of 2 cases. Ann Diagn Pathol.
13:189–196. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tanriverdi O, Avci A, Yugunt I and Polat
M: A case report of breast and liver metastases of thyroid
follicular carcinoma. J Can Res Ther. 11:6522015. View Article : Google Scholar
|
|
9
|
Grebe SK and Hay ID: Follicular thyroid
cancer. Endocrinol Metab Clin North Am. 24:761–801. 1995.PubMed/NCBI
|
|
10
|
D'Avanzo A, Treseler P, Ituarte PH, Wong
M, Streja L, Greenspan FS, Siperstein AE, Duh QY and Clark OH:
Follicular thyroid carcinoma: Histology and prognosis. Cancer.
100:1123–1129. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Iwai H, Ohno Y, Ito H, Kiyokawa T and Aoki
N: Renal rupture associated with a poorly differentiated follicular
thyroid carcinoma metastasizing to the thigh muscle, lung and
kidney. Intern Med. 44:848–852. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cochetti G, Puxeddu P, Del Zingaro MD,
D'Amico F, Cottini E, Barillaro F and Mearini E: Laparoscopic
partial nephrectomy of thyroid cancer metastasis: Case report and
review of the literature. Onco Targets Ther. 6:355–360. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Remonti LR, Kramer CK, Leitão CB, Pinto LC
and Gross JL: Thyroid ultrasound features and risk of carcinoma: A
systematic review and meta-analysis of observational studies.
Thyroid. 25:538–550. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Coquia SF, Chu LC and Hamper UM: The role
of sonography in thyroid cancer. Radiol Clin North Am.
52:1283–1294. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Taki S, Terahata S, Yamashita R, Kinuya K,
Nobata K, Kakuda K, Kodama Y and Yamamoto I: Thyroid
calcifications: Sonographic patterns and incidence of cancer. Clin
Imaging. 28:368–371. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kim BM, Kim MJ, Kim EK, Kwak JY, Hong SW,
Son EJ and Kim KH: Sonographic differentiation of thyroid nodules
with eggshell calcifications. J Ultrasound Med. 27:1425–1430.
2008.PubMed/NCBI
|
|
17
|
Yoon DY, Lee JW, Chang SK, Choi CS, Yun
EJ, Seo YL, Kim KH and Hwang HS: Peripheral calcification in
thyroid nodules: Ultrasonographic features and prediction of
malignancy. J Ultrasound Med. 26:1349–1355. 2007.PubMed/NCBI
|
|
18
|
Vescini F, Di Gaetano P, Vigna E, Pascoli
A and Cacciari M: Anaplastic thyroid carcinoma in a 49 year-old
woman with a long-standing goiter: A case report. Minerva
Endocrinol. 25:81–83. 2000.PubMed/NCBI
|
|
19
|
Song HJ, Xue YL, Xu YH, Qiu ZL and Luo QY:
Rare metastases of differentiated thyroid carcinoma: Pictorial
review. Endocr Relat Cancer. 18:R165–R174. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Garcia-Sanchis L, Lopez-Aznar D, Oltra A,
Rivas A, Alonso J, Montalar J and Mateo A: Metastatic follicular
thyroid carcinoma to the kidney: A case report. Clin Nucl Med.
24:48–50. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Matsuno A, Katakami H, Okazaki R, Yamada
S, Sasaki M, Nakaguchi H, Yamada SM, Hoya K, Murakami M, Yamazaki
K, et al: Skull base metastasis from follicular thyroid carcinoma -
two case reports -. Neurol Med Chir (Tokyo). 50:421–425. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Camacho V, Rodríguez-Revuelto A, Flotats
A, Duch J, Artigas C, Carrió I and Estorch M: Skin metastasis of
follicular thyroid carcinoma. Eur J Nucl Med Mol Imaging.
37:12372010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lin X, Zhu B, Liu Y and Silverman JF:
Follicular thyroid carcinoma invades venous rather than lymphatic
vessels. Diagn Pathol. 5:82010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ito Y, Hirokawa M, Masuoka H, Yabuta T,
Kihara M, Higashiyama T, Takamura Y, Kobayashi K, Miya A and
Miyauchi A: Prognostic factors of minimally invasive follicular
thyroid carcinoma: Extensive vascular invasion significantly
affects patient prognosis. Endocr J. 60:637–642. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Grani G, D'Alessandri M, Carbotta G, Nesca
A, Del Sordo M, Alessandrini S, Coccaro C, Redina R, Bianchini M,
Prinzi N and Fumarola A: Grey-scale analysis improves the
ultrasonographic evaluation of thyroid nodules. Medicine
(Baltimore). 94:e11292015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Brennan MD, Bergstralh EJ, van Heerden JA
and McConahey WM: Follicular thyroid cancer treated at the Mayo
Clinic, 1946 through 1970: Initial manifestations, pathologic
findings, therapy, and outcome. Mayo Clin Proc. 66:11–22. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sillery JC, Reading CC, Charboneau JW,
Henrichsen TL, Hay ID and Mandrekar JN: Thyroid follicular
carcinoma: Sonographic features of 50 cases. AJR Am J Roentgenol.
194:44–54. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jiang J, Shang X, Wang H, Xu YB, Gao Y and
Zhou Q: Diagnostic value of contrast-enhanced ultrasound in thyroid
nodules with calcification. Kaohsiung J Med Sci. 31:138–144. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Khoo ML, Asa SL, Witterick IJ and Freeman
JL: Thyroid calcification and its association with thyroid
carcinoma. Head Neck. 24:651–655. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sun Y, Fang S, Dong H, Zhao C, Yang Z, Li
P and Wang J: Correlation between osteopontin messenger RNA
expression and microcalcification shown on sonography in papillary
thyroid carcinoma. J Ultrasound Med. 30:765–771. 2011.PubMed/NCBI
|
|
31
|
Kwak JY, Kim EK, Son EJ, Kim MJ, Oh KK,
Kim JY and Kim KI: Papillary thyroid carcinoma manifested solely as
microcalcifications on sonography. AJR Am J Roentgenol.
189:227–231. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lee SK: Hürthle cell thyroid adenoma with
an eggshell calcification: Sonographic-pathologic correlation. J
Clin Ultrasound. 42:172–175. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yaturu S and Rainer L: Thyroid nodule with
eggshell calcification and oncocytic thyroid cancer. Med Sci Monit.
16:CS25–CS28. 2010.PubMed/NCBI
|
|
34
|
Cheng SP, Lee JJ, Lin J and Liu CL:
Eggshell calcification in follicular thyroid carcinoma. Eur Radiol.
15:1773–1774. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lee SK and Rho BH: Follicular thyroid
carcinoma with an eggshell calcification: Report of 3 cases. J
Ultrasound Med. 28:801–806. 2009.PubMed/NCBI
|
|
36
|
Lee SK and Rho BH: Follicular thyroid
adenoma with eggshell calcification presenting as an intensely
hypermetabolic lesion on 18F-FDG PET/CT. J Clin Ultrasound.
38:107–110. 2010.PubMed/NCBI
|
|
37
|
Seo HS, Lee DH, Park SH, Min HS and Na DG:
Thyroid follicular neoplasms: Can sonography distinguish between
adenomas and carcinomas? J Clin Ultrasound. 37:493–500. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Yoon JH, Kim EK, Youk JH, Moon HJ and Kwak
JY: Better understanding in the differentiation of thyroid
follicular adenoma, follicular carcinoma, and follicular variant of
papillary carcinoma: A retrospective study. Int J Endocrinol.
2014:3215952014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Cordes M, Kondrat P, Uder M, Kuwert T and
Sasiadek M: Differential diagnostic ultrasound criteria of
papillary and follicular carcinomas: A multivariate analysis. Rofo.
186:489–495. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Rosario PW: Thyroid nodules with atypia or
follicular lesions of undetermined significance (Bethesda Category
III): importance of ultrasonography and cytological subcategory.
Thyroid. 24:1115–1120. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zhang JZ and Hu B: Sonographic features of
thyroid follicular carcinoma in comparison with thyroid follicular
adenoma. J Ultrasound Med. 33:221–227. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
McHenry CR and Phitayakorn R: Follicular
adenoma and carcinoma of the thyroid gland. Oncologist. 16:585–593.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Iared W, Shigueoka DC, Cristófoli JC,
Andriolo R, Atallah AN, Ajzen SA and Valente O: Use of color
Doppler ultrasonography for the prediction of malignancy in
follicular thyroid neoplasms: Systematic review and meta-analysis.
J Ultrasound Med. 29:419–425. 2010.PubMed/NCBI
|
|
44
|
Vasko VV, Gaudart J, Allasia C, Savchenko
V, Di Cristofaro J, Saji M, Ringel MD and De Micco C: Thyroid
follicular adenomas may display features of follicular carcinoma
and follicular variant of papillary carcinoma. Eur J Endocrinol.
151:779–786. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Balentine CJ, Domingo RP, Patel R,
Laucirica R and Suliburk JW: Thyroid lobectomy for indeterminate
FNA: Not without consequences. J Surg Res. 184:189–192. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Sakorafas GH: Thyroid nodules;
interpretation and importance of fine-needle aspiration (FNA) for
the clinician - practical considerations. Surg Oncol. 19:e130–e139.
2010. View Article : Google Scholar : PubMed/NCBI
|