Introduction
Breast cancer treatment has evolved in the last 20
years thanks to the better understanding of molecular mechanisms
and the identification of numerous genomic alterations involved in
the carcinogenesis process. This knowledge also allowed the
identification of novel therapeutic targets and the development of
numerous drugs specifically directed against these targets, called
targeted therapies. The human epidermal growth factor 2 (HER2)
oncoprotein is one of the first therapeutic targets identified for
breast carcinoma treatment. This protein is a class 1 transmembrane
receptor with tyrosine kinase activity and is involved in the
oncogenic activation of numerous signaling pathways, including the
mitogen-activated protein kinase (MAPK) and phosphoinositide
3-kinase (PI3K) pathways (1,2). These pathways are important for cellular
homeostasis and regulating the mechanisms of growth,
differentiation, cell proliferation and apoptosis (3). The two pathways are frequently
dysregulated in breast cancers due to mutations, deletions or
rearrangements on the signaling proteins encoding genes (4).
The MAPK and PI3K pathways are kinase dependent.
Activation of these kinases leads to the formation of their active
phosphorylated states (5). The
upregulation of signaling pathways and an increase in the
phosphorylation of proteins that are involved in these pathways has
been demonstrated in numerous cancers; this was particularly the
case for phosphorylated-protein kinase B (p-AKT) in lung cancer,
myeloid leukemia, prostate and breast cancers (6–8).
Consequently, protein phosphorylation may be an indicator of
signaling activity in tumors, and can be used to assess the
activity of intracellular signaling pathways (9). Levels of phosphorylated forms of cells
signaling proteins may be a prognostic biomarker and may predict
the tumors sensitivity to treatment (10–12).
HER2 receptors are involved in tumor development and
proliferation (13). Activating
mutations on gene loci encoding the tyrosine kinase domain, or the
overexpression of HER2 receptors, can lead to the upregulation or
dysregulation of downstream signaling pathways (13). HER2 is overexpressed in 15–20% of
breast carcinomas (1,14).
The overexpression of HER2 was previously associated
with a poor prognosis until the development of the first anti-HER2
therapy, trastuzumab, which drastically improves the
progression-free and overall survival times of patients with
HER2-overexpressing breast cancers (15).
Trastuzumab is an immunoglobulin G1 (IgG1)-type
humanized recombining monoclonal antibody (mAb) directed against
the extracellular domain of HER2 tyrosine kinase receptor (16,17). This
mAb specifically binds the subdomain IV of HER2 extracellular
domain, and through this molecular mechanism, trastuzumab activity
is awaited by blocking HER2 downstream cell signaling (17–19). Due
to the IgG1 backbone, trastuzumab also acts through
antibody-dependent cell-mediated cytotoxicity (ADCC). The
interaction of the Fc domain with Fc γ receptor of immune cells,
including natural killer cells and macrophages, leads to the
activation of these cells and thus the lysis of cancer cells
(1,2,16,20–24).
Several studies have proposed that the behavior and
mechanism of action of trastuzumab may be drastically altered in
vitro and in vivo (19,21), and
that the relative involvement of signaling inhibition vs. ADCC
could be an important determinant of the activity of trastuzumab
(25).
The aim of the present study was to assess the
ability of trastuzumab to inhibit the phosphorylation of the major
proteins of the PI3K/AKT/mechanistic target of rapamycin (mTOR) and
Ras/Raf/MAPK signaling pathways signaling pathways in vitro,
in breast cancer cell lines and in tumor biopsies obtained from
patients treated with preoperative trastuzumab monotherapy as part
of the RADHER clinical trial.
Materials and methods
Cell lines
HER2-positive SKBR3 [American Type Culture
Collection (ATCC)® HTB-30™; ATCC, Manassas, VA, USA],
and HER2 negative MCF-7 (ATCC® HTB-22™; ATCC), cell
lines were maintained in phenol red-free RPMI-1640 culture medium
supplemented by 10% fetal calf serum (FCS; Dutscher, Brumath,
France) in a 5% CO2 atmosphere. The two cell lines were
exposed to trastuzumab (5.10−6 mol/l) for 72 h in
FCS-free medium.
Patients
All patients (n=41) had non-metastatic early or
locally-advanced HER2 breast carcinomas (T1-3, N0-2, M0) according
to the TNM staging (6th edition, 2002) (26) and received trastuzumab as short-term
preoperative monotherapy as part of the Unicancer GEP04 RADHER
phase II clinical trial (European Clinical Trials Database no.,
2007-004098-24). Trastuzumab was administered intravenously
following a weekly schedule with a loading dose of 4 mg/kg at day 1
then 2 mg/kg/week for 6 weeks. Surgery was performed subsequent to
the completion of the sixth cycle. All patients provided written
consent, and the study was approved by the Comité de Protection des
Personnes Ouest IV (Nantes, France). All patients had baseline
18G-needle biopsies prior to the initiation of the treatment. A
second biopsy was performed at surgery. Samples were snap-frozen in
liquid nitrogen at −80°C to avoid the degradation of
phosphoproteins. Prior to being submitted to total protein
extraction, all biopsies were validated by a senior pathologist
from the Department of Biopathology of the Institut de Cancérologie
de Lorraine (Vandœuvre-lès-Nancy, France) using a hematoxylin-eosin
frozen section examination to ensure that the minimal tumor cell
content was >50%.
In total, 19 pairs of baseline/surgery biopsies were
eligible for protein extraction and comparative phosphoprotein
expression analysis prior to and subsequent to treatment.
Phosphoprotein expression analysis
using a multiplex bead immunoassay
The expression levels of p-AKT,
phosphorylated-ribosomal protein S6 kinase B1 (p-P70S6K),
phosphorylated-mitogen-activated protein kinase kinase 1 (p-MEK1)
and phosphorylated-extracellular signal regulated kinase 1/2
(p-ERK1/2) were quantitatively assessed using a multiplex bead
immunoassay, as previously described (27). Briefly, proteins were extracted from
cell cultures and tumor specimens using cell lysis kit (Bio-Rad
Laboratories, Inc., Hercules, CA, USA), according to the
manufacturer's instructions. Cell pellets (1×106 cells),
or tumor specimens (15–20 mg) were first disrupted for 15 min by
use a steel-bead tissue lyser (Qiagen GmbH, Hilden, Germany).
Disrupted tissues were then exposed for 10 sec to the lysis
solution containing phenylmethylsulfonylfluoride antiprotease.
Protein extracts were finally stored at −80°C until analyzed.
Proteins extracts were transferred into 96-well
plates and diluted with 25 µl buffered solution. Multiplexing
Bio-Plex phosphoprotein singleplex assay kits (Bio-Rad Laboratories
Inc.) for p-AKT (Ser473; catalog no. 171-V1075), p-P70S6K
(Thr421/Ser424; catalog no. 171-V24155), p-MEK1 (Ser217/Ser221;
catalog no. 171-V25340) and p-ERK1/2 (Thr202/Tyr204, Thr185/Tyr187;
catalog no. 171-V22238) monoclonal antibodies was performed
according to the manufacturer's instructions. First, beads bearing
antibodies directed against the phosphoproteins of interest were
added to each well and incubated overnight at 37°C. Biotinylated
antibodies and streptavidin phycoerythrin solution were then added.
Phosphoprotein expression was then assessed using
BioPlex® (Bio-Rad Laboratories, Inc.), in accordance
with the manufacturer's instructions. Frozen protein extracts from
the MCF-7 cell line exposed to epidermal growth factor (EGF) were
used as positive controls. The results were recorded as mean
fluorescence intensities, expressed as arbitrary units and
considered significant when exceeding a signal:noise ratio of 3.
Results were normalized to the data measured in the positive
controls.
Statistical analysis
Results were recorded as the mean fluorescence
intensity of triplicate experiments (cell lines) or duplicate
measurements (patients) and expressed as arbitrary units.
Parameters were rescaled by dividing by the mean of the parameter
prior to exposure to trastuzumab. Hence, all parameters prior to
exposure to trastuzumab had a mean that was equal to 1, and the
size of the effect was not affected by this transformation.
Comparisons of the parameters between the two times
(baseline and surgery) were made with a paired Student's
t-test. Statistical analyses were performed using SAS
software version 9.2 (SAS Institute Inc., Cary, NC, USA). A P-value
of 0.05 was considered to indicate a statistically significant
difference.
Results
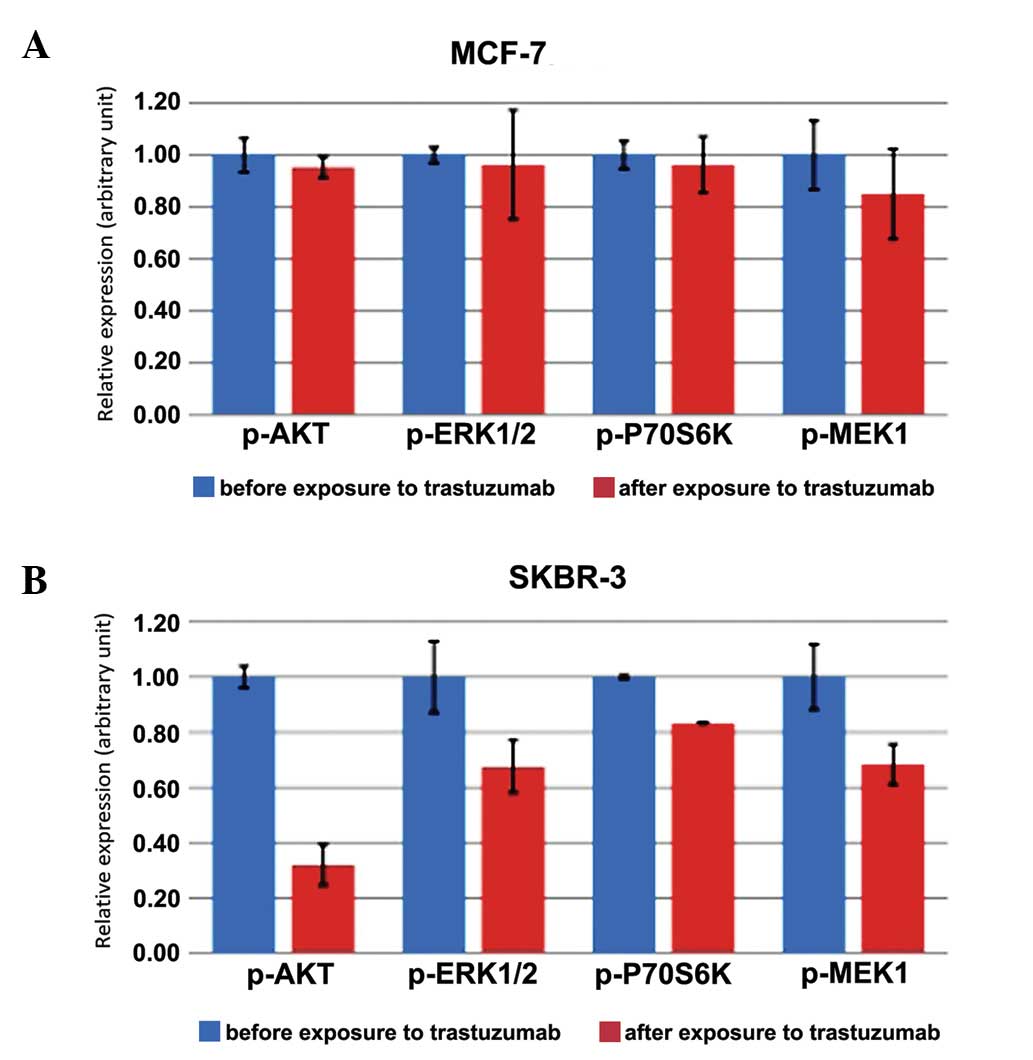
In the MCF-7 cell line, the mean expression levels
for phosphoproteins following exposure to 5×10−6 mol/l
trastuzumab were 0.95 [standard deviation (SD), 0.04], 0.96 (SD,
0.21), 0.96 (SD, 0.11) and 0.85 (SD, 0.17) for p-AKT, p-ERK1/2,
P-70S6K and p-MEK1, respectively. No statistically significant
difference in the expression level of phosphoproteins prior to and
subsequent to exposure to trastuzumab for p-AKT, p-ERK1/2, p-S70S6K
and p-MEK1 (P=0.36, P=0.78, P=0.63 and P=0.30, respectively) was
detected in MCF-7 cells (Table I;
Fig. 1A).
 | Table I.Expression level of phosphoproteins in
HER2-positive SKBR3 and HER2-negative MCF-7 cell lines. |
Table I.
Expression level of phosphoproteins in
HER2-positive SKBR3 and HER2-negative MCF-7 cell lines.
|
| Expression level |
|
|---|
|
|
|
|
|---|
| Phosphoprotein | 0×10−6
mol/l trastuzumab | 5×10−6
mol/l trastuzumab | P-value |
|---|
| MCF-7 |
|
|
|
|
p-AKT | 1.00 (0.06) | 0.95 (0.04) |
0.36 |
|
p-ERK1/2 | 1.00 (0.03) | 0.96 (0.21) |
0.78 |
|
p-P70S6K | 1.00 (0.05) | 0.96 (0.11) |
0.63 |
|
p-MEK1 | 1.00 (0.13) | 0.85 (0.17) |
0.30 |
| SKBR-3 |
|
|
|
|
p-AKT | 1.00 (0.04) | 0.32 (0.07) | <0.01 |
|
p-ERK1/2 | 1.00 (0.13) | 0.68 (0.09) |
0.02 |
|
p-P70S6K | 1.00 (0.01) | 0.83 (0.00) | <0.01 |
|
p-MEK1 | 1.00 (0.12) | 0.68 (0.07) |
0.02 |
In the SKBR-3 cell line, the mean expression levels
for phosphoproteins following exposure to 5.10−6 mol/l
trastuzumab were 0.32 (SD, 0.07), 0.68 (SD, 0.09), 0.83 (SD, 0.00)
and 0.68 (SD, 0.07) for p-AKT, p-ERK1/2, P-70S6K and p-MEK1,
respectively. A statistically significant decrease in the
expression level of p-AKT (P<0.01), p-ERK 1/2 (P=0.02), P-70S6K
(P<0.01) and p-MEK1 (P=0.02) was observed following exposure to
trastuzumab in SKBR-3 cells (Table I;
Fig. 1B).
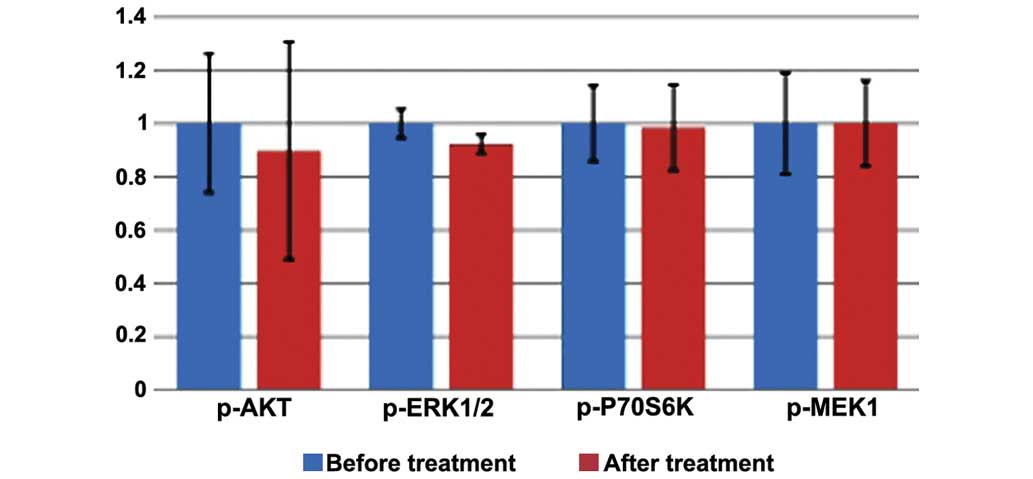
In patients, the mean expression levels of
phosphoproteins in the biopsies obtained subsequent to treatment
were 0.89 (SD, 1.77), 0.92 (SD, 0.15), 0.98 (SD, 0.70) and 1.00
(SD, 0.69) for p-AKT, p-P70S6K, p-MEK1 and p-ERK1/2, respectively.
No statistically significant difference in the expression of the
p-AKT (P=0.77), p-P70S6K (P=0.16), p-MEK1 (P=0.92) and p-ERK1/2
(P=0.99) signaling phosphoproteins was observed subsequent to
treatment (Table II; Fig. 2).
 | Table II.Expression level of phosphoproteins
in patients prior to and subsequent to treatment with
trastuzumab. |
Table II.
Expression level of phosphoproteins
in patients prior to and subsequent to treatment with
trastuzumab.
|
| Expression
level |
|
|---|
|
|
|
|
|---|
| Phosphoprotein | Pre-treatment | Post-treatment | P-value |
|---|
| p-AKT | 1.00 (1.13) | 0.89 (1.77) | 0.77 |
| p-P70S6K | 1.00 (0.24) | 0.92 (0.15) | 0.16 |
| p-MEK1 | 1.00 (0.62) | 0.98 (0.70) | 0.92 |
| p-ERK1/2 | 1.00 (0.83) | 1.00 (0.69) | 0.99 |
Discussion
Trastuzumab undoubtedly provides a major advancement
in the treatment of breast cancer in metastatic or adjuvant
settings and alone or in combination with chemotherapy.
Trastuzumab, a mAb, dramatically improves the response rate and
progression-free and overall survival of patients with metastatic
disease (15). However, the exact
mode of action of trastuzumab remains partly elucidated, and
several studies have suggested that the inhibition of oncogenic
signaling may not be the main mode of action (21,22), in
particular when trastuzumab is administered alone for
chemotherapy-naïve patients (25,28).
In the present study, the expression level of
phosphoproteins present in the PI3K/AKT/mTOR and RAS/RAF/MAPK
signaling pathways was analyzed prior to and subsequent to exposure
to trastuzumab.
The impact of trastuzumab was assessed in cell lines
and tumor specimens, which were obtained from patients with
HER2-overexpressing early breast cancer that had received
trastuzumab as a preoperative monotherapy as part of the RADHER
clinical trial.
The present study showed that trastuzumab has a
varied impact on the signaling pathways of the MCF-7 and SKBR-3
cell lines. Following exposure to trastuzumab, a statistically
significant decrease in the expression levels of p-AKT, p-P70S6K,
p-MEK1 and p-ERK1/2 was found in the SKBR-3 cell line, but not in
MCF-7 cells. This result was predictable, and may be explained by
the fact that SKBR-3 cell line overexpress HER-2, in contrast to
the MCF-7 cell line. Notably, no decrease in the expression level
of phosphoproteins was observed following treatment with
trastuzumab monotherapy in HER2-positive breast cancer patients,
which suggests that other mechanisms may interfere with the
expression.
Previous studies have demonstrated that trastuzumab
has several modes of action, implying that various mechanisms for
antitumor activity are present in vitro and in vivo
(18,21,22). The
modulation of signaling pathways was also shown to be a major
mechanism when cell lines were treated with trastuzumab, whereas
ADCC was the leading mechanism in small animals treated with the
same molecule (28,29). The mechanism of action involved was
also shown to vary depending on the neoadjuvant or adjuvant
setting, dose and administration schedule and the presence or
absence of co-administered drugs (28,30,31). In
2004, Gennari et al showed that trastuzumab employed the
preferential immunological mechanism of ADCC when used as a
monotherapy and in a preoperative setting (28). Therefore, the classification of the
tumor would not be the only parameter to consider when predicting
the response to treatment (31).
In the present study, trastuzumab was used in a
preoperative setting as a monotherapy; therefore, the lack of
downregulation of the PI3K and MAPK pathways could probably be
explained by the implementation of a predominant immunological
mechanism for a trastuzumab-associated ADCC, which is consistent
with previous studies (28).
Additional studies are required to elucidate the mechanisms
underlying ADCC.
Signaling pathways have been previously shown to be
highly interconnected, with multiple points of convergence, cross
talk and feedback loops, and these pathways can activate or inhibit
each other, depending on the context and on cellular conditions
(32–36). A compensatory mechanism, due to the
presence of other signaling pathways, could explain the absence of
or decrease in the expression of phosphoproteins. However, it
should be noted that the present study was performed on a small
population, which may have led to a bias in the results. These
results should be confirmed in a larger and more representative
effective.
Bio-Plex® phosphoprotein arrays do not
provide subcellular localization data or take into account the
heterogeneity of the tumor tissue (27). Tumor heterogeneity is a major source
of variability in results. Tumors can be polyclonal, and will
therefore not express homogeneous phosphoproteins. For this reason,
it is uncertain whether the samples analyzed were fully
representative of the whole tumor, as the stroma is present in
various proportions in the tumor tissue. This possibility may
explain the difference in the results observed with cell lines that
are not affected by the stroma or tumor heterogeneity.
Results can also be affected by parameters such as
the pre-analytical phase. The pre-analytical steps for sampling may
importantly affect the results, particularly with regards to
phosphoproteins (37).
Phosphoproteins are very sensitive to temperature and rapidly
degrade, which may have an impact on the results. Numerous
variables can affect the quality of sampling, particularly
intraoperative hypoxia and the cold ischemic time. A previously
study on uterus surgical specimens revealed that the time between
excision and analysis has an impact on the level of expression of
phosphoproteins (38).
The hot and cold ischemia time can affect the
quality of samples and induce variation in the expression of
phosphoproteins, as phosphoproteins are very sensitive to
phosphatase (38). Preventing the
dephosphorylation of the marker remains a challenge. In addition,
the degradation of phosphoproteins is preceded by an increase of
their concentration in the sample. All these parameters are
challenging to control. Rapid processing is essential for assessing
signaling activity in phosphoprotein studies. In the present study,
the processing time has not been traced, which may provide a
significant bias in the results. However, the excision and
snap-freezing procedure used in the present study ensures little
variation in the expression of phosphoproteins, by limiting
degradation.
In summary, the degradation of phosphoproteins can
vary according to the tissue, tumor type or the phosphoprotein
itself (37). Phosphoprotein
expression can also be affected by other cellular stressors prior
to tissue congelation (10).
Although trastuzumab is widely used for the
treatment of HER2-overexpressing breast cancers, the underlying
in vivo mechanism of action is not yet fully understood. The
present study showed that trastuzumab inhibits the MAPK and PI3K
pathways for cell lines overexpressing HER2, but not on
HER2-overexpressing tumors that have received preoperative
treatment as a monotherapy. According to the results, the
inhibition of oncogenic signaling pathways may not be the main mode
of action employed, when trastuzumab is administered alone in
chemotherapy naïve patients. Alternative molecular mechanisms, such
as the modulation of immune pathways, should be considered.
References
|
1
|
Hudis CA: Trastuzumab-mechanism of action
and use in clinical practice. N Engl J Med. 357:39–51. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Baselga J: Treatment of
HER2-overexpressing breast cancer. Ann Oncol. 21(Suppl 7):
vii36–vii40. 2010.PubMed/NCBI
|
|
3
|
Engelman JA, Luo J and Cantley LC: The
evolution of phosphatidylinositol 3-kinases as regulators of growth
and metabolism. Nat Rev Genet. 7:606–619. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Harlé A, Lion M, Lozano N, Husson M,
Harter V, Genin P and Merlin JL: Analysis of PIK3CA exon 9 and 20
mutations in breast cancers using PCR-HRM and PCR-ARMS: Correlation
with clinicopathological criteria. Oncol Rep. 29:1043–1052.
2013.PubMed/NCBI
|
|
5
|
Mendoza MC, Er EE and Blenis J: The
Ras-ERK and PI3K-mTOR pathways: Cross-talk and compensation. Trends
Biochem Sci. 36:320–328. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Martelli AM, Tabellini G, Bressanin D,
Ognibene A, Goto K, Cocco L and Evangelisti C: The emerging
multiple roles of nuclear Akt. Biochim Biophys Acta.
1823:2168–2178. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Park SS and Kim SW: Activated Akt
signaling pathway in invasive ductal carcinoma of the breast:
Correlation with HER2 overexpression. Oncol Rep. 18:139–143.
2007.PubMed/NCBI
|
|
8
|
Lin HJ, Hsieh FC, Song H and Lin J:
Elevated phosphorylation and activation of PDK-1/AKT pathway in
human breast cancer. Br J Cancer. 93:1372–1381. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Baker AF, Dragovich T, Ihle NT, Williams
R, Fenoglio-Preiser C and Powis G: Stability of phosphoprotein as a
biological marker of tumor signaling. Clin Cancer Res.
11:4338–4340. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
David KA and Juhl H: Immunohistochemical
detection of phosphoproteins and cancer pathways. Handbook of
Practical Immunohistochemistry. Lin F and Prichard J: Springer.
(New York, NY). 85–90. 2015.
|
|
11
|
Mandell JW: Phosphorylation state-specific
antibodies: Applications in investigative and diagnostic pathology.
Am J Pathol. 163:1687–1698. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mandell JW: Immunohistochemical assessment
of protein phosphorylation state: The dream and the reality.
Histochem Cell Biol. 130:465–471. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Menard S, Pupa SM, Campiglio M and
Tagliabue E: Biologic and therapeutic role of HER2 in cancer.
Oncogene. 22:6570–6578. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yersal O and Barutca S: Biological
subtypes of breast cancer: Prognostic and therapeutic implications.
World J Clin Oncol. 5:412–424. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Slamon DJ, Leyland-Jones B, Shak S, Fuchs
H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M,
et al: Use of chemotherapy plus a monoclonal antibody against HER2
for metastatic breast cancer that overexpresses HER2. N Engl J Med.
344:783–792. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Valabrega G, Montemurro F and Aglietta M:
Trastuzumab: Mechanism of action, resistance and future
perspectives in HER2-overexpressing breast cancer. Ann Oncol.
18:977–984. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gemmete JJ and Mukherji SK: Trastuzumab
(herceptin). AJNR Am J Neuroradiol. 32:1373–1374. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yakes FM, Chinratanalab W, Ritter CA, King
W, Seelig S and Arteaga CL: Herceptin-induced inhibition of
phosphatidylinositol-3 kinase and Akt Is required for
antibody-mediated effects on p27, cyclin D1, and antitumor action.
Cancer Res. 62:4132–4141. 2002.PubMed/NCBI
|
|
19
|
Mohsin SK, Weiss HL, Gutierrez MC,
Chamness GC, Schiff R, Digiovanna MP, Wang CX, Hilsenbeck SG,
Osborne CK, Allred DC, et al: Neoadjuvant trastuzumab induces
apoptosis in primary breast cancers. J Clin Oncol. 23:2460–2468.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nahta R, Yu D, Hung MC, Hortobagyi GN and
Esteva FJ: Mechanisms of disease: Understanding resistance to
HER2-targeted therapy in human breast cancer. Nat Clin Pract Oncol.
3:269–280. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Arnould L, Gelly M, Penault-Llorca F,
Benoit L, Bonnetain F, Migeon C, Cabaret V, Fermeaux V, Bertheau P,
Garnier J, et al: Trastuzumab-based treatment of HER2-positive
breast cancer: An antibody-dependent cellular cytotoxicity
mechanism? Br J Cancer. 94:259–267. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Clynes RA, Towers TL, Presta LG and
Ravetch JV: Inhibitory Fc receptors modulate in vivo cytotoxicity
against tumor targets. Nat Med. 6:443–446. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Spector NL and Blackwell KL: Understanding
the mechanisms behind trastuzumab therapy for human epidermal
growth factor receptor 2-positive breast cancer. J Clin Oncol.
27:5838–5847. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Molina MA, Codony-Servat J, Albanell J,
Rojo F, Arribas J and Baselga J: Trastuzumab (herceptin), a
humanized anti-Her2 receptor monoclonal antibody, inhibits basal
and activated Her2 ectodomain cleavage in breast cancer cells.
Cancer Res. 61:4744–4749. 2001.PubMed/NCBI
|
|
25
|
Andre F, Dieci MV, Dubsky P, Sotiriou C,
Curigliano G, Denkert C and Loi S: Molecular pathways: Involvement
of immune pathways in the therapeutic response and outcome in
breast cancer. Clin Cancer Res. 19:28–33. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sobin LH: TNM, sixth edition: New
developments in general concepts and rules. Semin Surg Oncol.
21:19–22. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chergui F, Chrétien AS, Bouali S, Ramacci
C, Rouyer M, Bastogne T, Genin P, Leroux A and Merlin JL:
Validation of a phosphoprotein array assay for characterization of
human tyrosine kinase receptor downstream signaling in breast
cancer. Clin Chem. 55:1327–1336. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Gennari R, Menard S, Fagnoni F, Ponchio L,
Scelsi M, Tagliabue E, Castiglioni F, Villani L, Magalotti C,
Gibelli N, et al: Pilot study of the mechanism of action of
preoperative trastuzumab in patients with primary operable breast
tumors overexpressing HER2. Clin Cancer Res. 10:5650–5655. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Therasse P: Measuring the clinical
response. What does it mean? Eur J Cancer. 38:1817–1823. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Petricevic B, Laengle J, Singer J, Sachet
M, Fazekas J, Steger G, Bartsch R, Jensen-Jarolim E and Bergmann M:
Trastuzumab mediates antibody-dependent cell-mediated cytotoxicity
and phagocytosis to the same extent in both adjuvant and metastatic
HER2/neu breast cancer patients. J Transl Med. 11:3072013.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Tagliabue E, Campiglio M, Pupa SM, Ménard
S and Balsari A: Activity and resistance of trastuzumab according
to different clinical settings. Cancer Treat Rev. 38:212–217. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Singh A, Nunes JJ and Ateeq B: Role and
therapeutic potential of G-protein coupled receptors in breast
cancer progression and metastases. Eur J Pharmacol. 763:178–183.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hollestelle A, Elstrodt F, Nagel JH,
Kallemeijn WW and Schutte M: Phosphatidylinositol-3-OH kinase or
RAS pathway mutations in human breast cancer cell lines. Mol Cancer
Res. 5:195–201. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Aksamitiene E, Kiyatkin A and Kholodenko
BN: Cross-talk between mitogenic Ras/MAPK and survival PI3K/Akt
pathways: A fine balance. Biochem Soc Trans. 40:139–146. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Saini KS, Loi S, de Azambuja E,
Metzger-Filho O, Saini ML, Ignatiadis M, Dancey JE and
Piccart-Gebhart MJ: Targeting the PI3K/AKT/mTOR and Raf/MEK/ERK
pathways in the treatment of breast cancer. Cancer Treat Rev.
39:935–946. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Carracedo A and Pandolfi PP: The PTEN-PI3K
pathway: Of feedbacks and cross-talks. Oncogene. 27:5527–5541.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Pinhel IF, Macneill FA, Hills MJ, Salter
J, Detre S, A'hern R, Nerurkar A, Osin P, Smith IE and Dowsett M:
Extreme loss of immunoreactive p-Akt and p-Erk1/2 during routine
fixation of primary breast cancer. Breast Cancer Res. 12:R762010.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Siddiqui S and Rimm DL: Pre-analytic
variables and phospho-specific antibodies: The Achilles heel of
immunohistochemistry. Breast Cancer Res. 12:1132010. View Article : Google Scholar : PubMed/NCBI
|