Introduction
Primary hyperparathyroidism (PHPT) is characterized
by hypercalcemia resulting from the overproduction of parathyroid
hormone (PTH) by one or multiple hyperfunctioning parathyroid
glands. It is the third most common endocrine disorder with a
reported incidence of ~0.25% in the general population (1). The incidence of PHPT increases with age,
and it occurs more frequently in females than in males (2). Research has confirmed that the majority
of patients with PHPT require surgery due to the risk of renal
stones, osteoporosis, cardiovascular disease, and in certain cases
silent complications of renal impairment (3). The majority of PHPT cases are caused by
a single parathyroid adenoma (75–85% of cases) (4). In 1928, Dr. Isaac Olch (5) performed the first successful
parathyroidectomy at Barnes Hospital in St. Louis, MO, USA, and
currently this operation remains one of the most effective
treatments, providing great potential for cure in patients with
PHPT. As the clinical features of PHPT are variable and lack
specificity, there is no clear consensus with regard to the most
effective treatment of patients with the condition. Therapeutic
strategies generally arise through clinical experiences. In this
study, we report our experience of dealing with 107 cases of PHPT
due to parathyroid tumor over the past 15 years, as well as our
experience in treatment of the condition with
parathyroidectomy.
Materials and methods
Patient data
In this retrospective study, we recruited 107
patients who were operated on for PHPT in our surgical department
between January 1998 and December 2013. Of the 107 patients, there
were 80 females and 27 males, with a median age of 57 years (range,
28–79 years). The disease duration ranged from 6 months to 15 years
(median, 25 months). Clinical information was derived from a
thorough review of the medical records and the institutional
patient database. Follow-up data were obtained through
correspondence and outpatient department visits, with the average
follow-up period being 5.7 years (range, 1–15 years).
Presentation and diagnosis
Forty-three patients exhibited an asymptomatic neck
mass. Metabolic bone disease was radiologically observed in 37
cases. Nineteen patients were asymptomatic despite hypercalcemia.
Eighteen were initially observed to have constitutional symptoms
including palpitations, nausea, fatigue, weight loss and memory
deficit. Twelve patients exhibited lithangiuria but had normal
renal function. Several patients suffered more than one
symptom.
To localize hyperfunctioning parathyroid glands, a
variety of imaging techniques were used, including neck
ultrasonography, Tc-99 m sestamibi scanning, computed tomography
(CT) and magnetic resonance imaging (MRI). All patients underwent
neck ultrasonography. The Tc-99 m sestamibi scan was performed in
83 cases (77.6%). In addition, 47 patients accepted CT or MRI
scanning.
Treatment
Under general anesthesia, all our cases underwent a
focused parathyroidectomy associated with a rapid intraoperative
PTH (IOPTH) assay monitoring. PTH levels were measured prior to
parathyroid tumor excision, and subsequent post-excision
measurements followed at 10 and 20 min, if a sufficient reduction
in PTH value was not observed. A 50% or greater drop in PTH values
from the pre-incision or pre-excision level was considered to
indicate a surgical success.
Ethics
Ethical approval was granted from the Zhengzhou
University Ethical Review Board.
Results
Pathological presentation
A total of 104 patients (97.2%) had benign lesions,
and 3 patients (2.8%) had parathyroid carcinoma. Of the 104
patients, there were 97 cases (90.7%) of single parathyroid
adenoma, 4 cases (3.7%) of multiple parathyroid adenoma or combined
parathyroid hyperplasia, and 3 cases (2.8%) of parathyroid
hyperplasia. Eighty-four cases (78.5%) were followed up. During the
follow-up period, 2 patients (2.4%) suffered parathyroid adenoma
recurrence, 2 patients (2.4%) succumbed to parathyroid carcinoma, 1
case of carcinoma survived for 34 months before succumbing to
postoperative lung and bone metastasis, and 1 succumbed to a
cardiovascular accident 21 months after surgery. The remaining
patients did not experience recurrence or metastasis.
Sensitivity and positive predictive
values
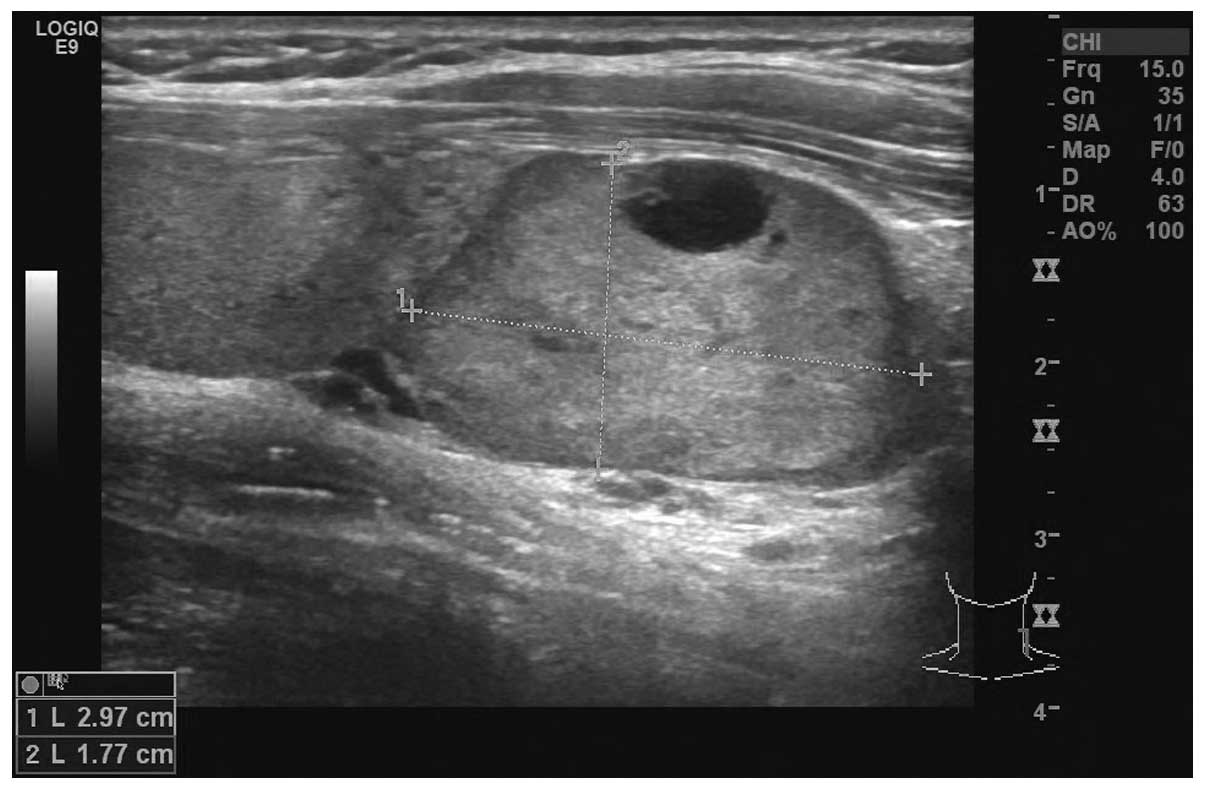
Ultrasonographic examination of the neck revealed 92
cases of occupied lesions in the parathyroid gland and 10 cases in
the thyroid gland (Fig. 1). The
remaining 5 cases had normal neck ultrasonography results. The
sensitivity and positive predictive values were 86.0% and 95.3%,
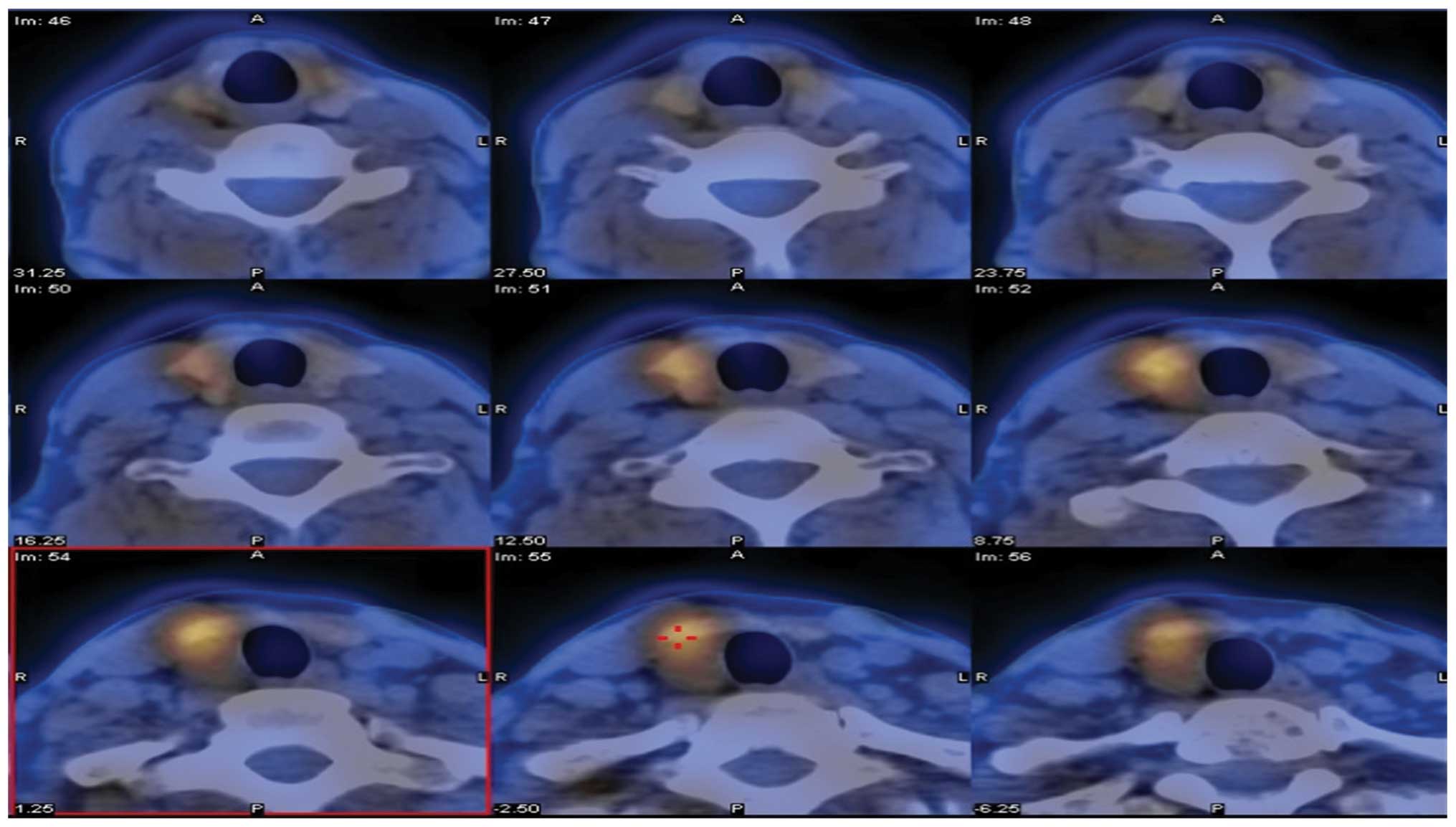
respectively. Eighty-three patients underwent Tc-99 m sestamibi
scanning. The accumulation of radioactivity was observed in 75 of
these patients (Fig. 2). The
sensitivity and positive predictive values were 90.4% and 94.1%.
The combination of an ultrasound and 99 m Tc-sestamibi scan
localized hyperfunctioning parathyroid in 76/82 patients (92.7%).
The sensitivity in identifying parathyroid tumors by CT and MRI was
80.8% and 79.6%, respectively (Table
I).
 | Table I.Sensitivity and positive predictive
values for various preoperative diagnostic modalities. |
Table I.
Sensitivity and positive predictive
values for various preoperative diagnostic modalities.
| Index | Ultrasound (%) | Sestamibi (%) | CT (%) | MRI (%) | Association of
ultrasound and sestamibi (%) |
|---|
| Sensitivity | 86.0 | 90.4 | 80.8 | 79.6 | 94.7 |
| Positive predictive
value | 95.3 | 94.1 | 83.6 | 85.0 | 100.0 |
PTH levels
Prior to surgery, elevated PTH levels were observed
in all patients. The preoperative serum calcium was abnormally
elevated in 86 patients (80.4%). The levels of serum calcium and
PTH in patients with parathyroid hyperplasia and carcinoma were
significantly higher than those in parathyroid adenoma patients
(Table II).
 | Table II.Comparison of observed indices among
various pathological parathyroid lesions. |
Table II.
Comparison of observed indices among
various pathological parathyroid lesions.
| Index | Parathyroid adenoma
(n=101) | Parathyroid
hyperplasia (n=3) | Parathyroid carcinoma
(n=3) |
|---|
| PTH before surgery
(pmol/l, mean ± SD) | 121.3±29.0 |
143.0±76.3a |
188.2±56.5b |
| Serum calcium before
surgery (mmol/l, mean ± SD) | 2.9±0.4 | 3.3±0.6c | 4.3±1.9d |
A 50% or greater drop in PTH levels within 10 min
compared with the highest PTH levels before surgery occurred in 86
patients (80.4%). In 9 cases the >50% drop in PTH levels was
attained after 20 min (8.4%). A >50% drop in PTH levels within
20 min was achieved by 95/107 patients (88.8%; Table III).
 | Table III.Decrease in PTH following surgery. |
Table III.
Decrease in PTH following surgery.
| Decrease in PTH | >50% decrease in
PTH within 10 min | >50% decrease in
PTH after 20 min |
|---|
| Patients | 86.0 | 9.0 |
| % | 80.4 | 8.4 |
Complications
Surgical complications were observed in nine
patients: three had wound infections, two had hematoma
necessitating re-operation and two had transient recurrent
laryngeal nerve paresis. Transient hypocalcemia occurred in 19
cases (17.8%). Symptoms ranged from face, hand and foot numbness to
limb twitching. All of these patients were treated with calcium and
vitamin D per os and intravenously with resolution within 1 month.
There were no cases of permanent hypocalcemia.
Statistical analysis
Results were recorded and are expressed as the means
± standard deviation. Statistical significance was determined using
the Chi-square test. All analyses were performed using the
Statistical Package for Social Science (SPSS) version 16.0 (SPSS
Inc., Chicago, IL, USA). P<0.05 was considered to indicate a
statistically significant difference.
Discussion
Ruda et al (6)
reviewed of the diagnosis and treatment of PHPT from 1995 to 2003
and concluded that single parathyroid adenoma accounts for ~90% of
benign tumors of the parathyroid. Our study revealed a similar
result: 90.7% of our cases had single-gland disease.
The diagnosis of PHPT is generally made
biochemically following the measurement of elevated serum calcium
and PTH levels (1,4). In this group, we did not observe any
significant differences between the parathyroid hyperplasia and the
parathyroid carcinoma groups with regard to the PTH and serum
calcium values before surgery. However, the levels of serum calcium
and PTH in patients with parathyroid hyperplasia and carcinoma were
significantly higher than those of parathyroid adenoma patients.
However, the small sample size of three cases means that the study
should be replicated with a larger sample.
There is wide variation in the anatomic location of
the parathyroid glands, and in certain patients hyperfunctioning
glands are hard to locate during surgery. In these cases, reliable
preoperative localization of abnormal parathyroid glands has become
invaluable. The two most common imaging modalities are sestamibi
scanning and neck ultrasonography. High-resolution ultrasound is a
effective examination to locate enlarged parathyroid glands in the
neck. One of the advanced features of neck ultrasound is the
ability to study the thyroid gland concurrently for any
abnormalities. In addition, neck ultrasound is also beneficial as
it is inexpensive, it does not use ionizing radiation, and it has
high sensitivity (7). The sensitivity
of ultrasonography for the localization of abnormal parathyroid
glands generally varies in the literature from 61% to 85% (8–11).
However, in the present study, we noted a higher sensitivity of
86.0%. The variation in these numbers could be due to the fact that
ultrasonography is operator-dependent. At our institution,
ultrasonography is performed by a professional neck ultrasound
doctor, and these individuals are likely to have the best
understanding of neck anatomy. Much like ultrasonography, sestamibi
also has a high sensitivity for the detection of abnormal
parathyroid glands, and is particularly useful in detecting small,
posterior adenomas (12). According
to our statistical results, when ultrasound and sestamibi scans are
used together, the sensitivity of preoperative localization of
parathyroid adenomas increases. These findings are consistent with
the majority of studies. The reported sensitivity ranges between
94% and 99% (13). CT and MRI are
less used but are useful in patients with failed parathyroidectomy
or persistent PHPT to identify ectopic glands (8).
In their study on the reassessment of PTH
monitoring, Gawande et al (14) noted that it is less necessary to
monitor the value of IOPTH when there are concordant imaging
studies. Conversely, other studies (15) advocate the use of IOPTH monitoring to
guide parathyroid excision in all patients with PHPT.
Sokoll (16) argued
that using IOPTH in conjunction with reliable preoperative
localization facilitates the ability to perform minimally invasive
surgery in an ambulatory surgery setting with improved success
intraoperatively, increased patient satisfaction postoperatively,
and decreased costs perioperatively. This argument has been a hot
debate in the literature in recent years and is likely to continue
to be a point of discussion in the foreseeable future. However,
from our point of view, surgical treatment without IOPTH assay may
be appropriate in certain institutions where financial or access
constraints prevent the use of IOPTH assay, and at this point, how
to correctly locate the abnormal parathyroid glands is particularly
significant.
At our institution, IOPTH assay is still widely
used. In particular, blood collection timing appears to be a
critical step (17). The widely used
Miami criterion (rapid IOPTH value drop >50% from the highest
levels either pre-incision or at 10 min after gland excision) is
reported to have a high overall accuracy. However, other authors
have reported error rates as high as 16% due to false-negative and
false-positive results (18). They
suggested that 20 min of PTH monitoring should be performed
(19). In this study, we performed
IOPTH monitoring after 10 min if a >50% drop of PTH levels was
not observed. In nine patients (6.4%), a >50% decrease of PTH
was observed only after 20 min, and an unnecessary bilateral
exploration was thus avoided.
Cure of PHPT may be defined as normocalcemia 6
months after surgery, irrespective of the level of PTH (20). According to Hessman et al, the
success rate of parathyroidectomy is greater than 95%, with low
complication rates in cases performed by experienced surgeons
(21). The results of the present
study are similar to those of Hessman et al (21).
Parathyroid carcinoma is an extremely rare
malignancy and is reported to occur in less than 0.1% to 5% of
patients with PHPT (22–24). The same result was demonstrated in the
current study. There were 3 cases of parathyroid carcinoma (2.8%)
among the 107 cases of PHPT due to parathyroid tumor in our study.
To date, the diagnostic criteria for parathyroid carcinoma has been
inconsistent. Parathyroid carcinoma may therefore be under- or
overdiagnosed. In our experience, the obscure boundary or/and
invasion of adjacent tissues is the key indicator of parathyroid
carcinoma. For parathyroid carcinoma, males and females are equally
affected, usually in the fourth or fifth decade of life. Short of a
major biological or molecular breakthrough, surgery remains the
most effective therapeutic and palliative option (25).
Considering the small number of parathyroid
carcinoma cases, our clinical diagnostic and treatment experience
is limited. Further research is required on this topic to confirm
our findings.
In conclusion, the symptoms of PHPT vary and lack
specificity. Parathyroidectomy provides the most effective
treatment for PHPT due to parathyroid tumor. The ultrasonography
and sestamibi scan is the most effective examination for
parathyroid tumor. The 20 min PTH measurement appears to be
extremely useful, and avoids unnecessary bilateral exploration and
the associated risk of complications with only a slight increase in
the duration of surgery and the cost.
Glossary
Abbreviations
Abbreviations:
|
PHPT
|
primary hyperparathyroidism
|
|
PTH
|
parathyroid hormone
|
|
CT
|
computed tomography
|
|
MRI
|
magnetic resonance imaging
|
|
IOPTH
|
intraoperative parathyroid hormone
|
References
|
1
|
Bilezikian JP and Silverberg SJ: Clinical
practice. Asymptomatic primary hyperparathyroidism. N Engl J Med.
350:1746–1751. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Udén P, Chan A, Duh QY, Siperstein A and
Clark OH: Primary hyperparathyroidism in younger and older
patients: Symptoms and outcome of surgery. World J Surg.
16:791–797; discussion 798. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Philips IJ, Kurzawinski TR and Honour JW:
Potential pitfalls in intraoperative parathyroid hormone
measurements during parathyroid surgery. Ann Clin Biochem.
42:453–458. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fraser WD: Hyperparathyroidism. Lancet.
374:145–158. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Meyer A, Brabant G and Behrend M: Surgical
treatment of primary hyperparathyroidism. Eur J Med Res.
29:287–291. 2005.
|
|
6
|
Ruda JM, Hollenbeak CS and Stack BC Jr: A
systematic review of the diagnosis and treatment of primary
hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg.
132:359–372. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Felger EA and Kandil E: Primary
hyperparathyroidism. Otolaryngol Clin North Am. 43:417–432. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Johnson NA, Tublin ME and Ogilvie JB:
Parathyroid imaging: technique and role in the preoperative
evaluation of primary hyperparathyroidism. AJR Am J Roentgenol.
188:1706–1715. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Meilstrup JW: Ultrasound examination of
the parathyroid glands. Otolaryngol Clin North Am. 37:763–778, ix.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Solorzano CC, Carneiro-Pla DM and Irvin GL
III: Surgeon-performed ultrasonography as the initial and only
localizing study in sporadic primary hyperparathyroidism. J Am Coll
Surg. 202:18–24. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ghaheri BA, Koslin DB, Wood AH and Cohen
JI: Preoperative ultrasound is worthwhile for reoperative
parathyroid surgery. Laryngoscope. 114:2168–2171. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Augustine MM, Bravo PE and Zeiger MA:
Surgical treatment of primary hyperparathyroidism. Endocr Pract.
17(Suppl 1): S75–S82. 2011. View Article : Google Scholar
|
|
13
|
Haber RS, Kim CK and Inabnet WB:
Ultrasonography for preoperative localization of enlarged
parathyroid glands in primary hyperparathyroidism: comparison with
(99m)technetium sestamibi scintigraphy. Clin Endocrinol (Ozf).
57:241–249. 2002. View Article : Google Scholar
|
|
14
|
Gawande AA, Monchik JM, Abbruzzese TA,
Iannuccilli JD, Ibrahim SI and Moore FD Jr: Reassessment of
parathyroid hormone monitoring during parathyroidectomy for primary
hyperparathyroidism after 2 preoperative localization studies. Arch
Surg. 141:381–384; discussion 384. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hanif F, Coffey JC, Romics L Jr,
O'Sullivan K, Aftab F and Redmond HP: Rapid intraoperative
parathyroid hormone assay - more than just a comfort measure. World
J Surg. 30:156–161. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sokoll LJ: Measurement of parathyroid
hormone and application of parathyroid hormone in intraoperative
monitoring. Clin Lab Med. 24:199–216. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Di Stasio E, Carrozza C, Lombardi Pio C,
Raffaelli M, Traini E, Bellantone R and Zuppi C: Parathyroidectomy
monitored by intra-operative PTH: the relevance of the 20 min
end-point. Clin Biochem. 40:595–603. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Calò PG, Pisano G, Tatti A, Medas F, Boi
F, Mariotti S and Nicolosi A: Intraoperative parathyroid hormone
assay during focused parathyroidectomy for primary
hyperparathyroidism: Is it really mandatory? Minerva Chir.
67:337–342. 2012.PubMed/NCBI
|
|
19
|
Lombardi CP, Raffaelli M, Traini E, Di
Stasio E, Carrozza C, De Crea C, Zuppi C and Bellantone R:
Intraoperative PTH monitoring during parathyroidectomy: the need
for stricter criteria to detect multiglandular disease. Langenbecks
Arch Surg. 393:639–645. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Suliburk JW and Perrier ND: Primary
hyperparathyroidism. Oncologist. 12:644–653. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hessman O, Stålberg P, Sundin A, Garske U,
Rudberg C, Eriksson LG, Hellman P and Akerström G: High success
rate of parathyroid reoperation may be achieved with improved
localization diagnosis. World J Surg. 32:774–781; discussion
782–783. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Obara T and Fujimoto Y: Diagnosis and
treatment of patients with parathyroid carcinoma: an update and
review. World J Surg. 15:738–744. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Favia G, Lumachi F, Polistina F and
D'Amico DF: Parathyroid carcinoma: sixteen new cases and
suggestions for correct management. World J Surg. 22:1225–1230.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Rodgers SE and Perrier ND: Parathyroid
carcinoma. Curr Opin Oncol. 18:16–22. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Givi B and Shah JP: Parathyroid carcinoma.
Clin Oncol (R Coll Radiol). 22:498–507. 2010. View Article : Google Scholar : PubMed/NCBI
|