Introduction
Branchiogenic carcinoma (BC) is an extremely rare
malignant neck tumor that usually appears as a mass lesion with a
prominent cystic component. Since oropharyngeal carcinoma (OPC)
metastasis in the lymph nodes also has a cystic appearance, it is
occasionally difficult to distinguish between BC and metastases in
the cervical lymph nodes from clinically silent OPC.
Martin et al (1) proposed the following criteria for the
diagnosis of BC, stating the fourth criterion as the most important
for confirming BC. First, the cervical tumor must occur at a point
along an imaginary line that extends between just anterior to the
tragus of the ear and downward along the anterior border of the
sternocleidomastoid (SCM) muscle to the clavicle. Second, the
histological appearance of the mass should be consistent with an
origin from tissue known to be present in the branchial vestigia.
Third, a survival period of at least 5 years, with periodic
examinations, must be recorded without the development of any other
lesion that could be the primary tumor. Fourth, histology should
demonstrate the presence of cancer in the wall of an epithelial
cyst situated in the lateral aspect of the neck. Khafif et
al disagreed with the third criterion, as patients may succumb
to unrelated causes prior to the 5-year milestone (2). In addition, a number of patients receive
post-operative irradiation, which may result in control of an
occult primary tumor. Therefore, Khafif et al (2) proposed replacement of this criterion
with two additional criteria: i) The absence of an identifiable
primary cancer in another location, as determined by a thorough
evaluation, including appropriate biopsies; and ii) the clear
histological identification of a cystic structure that is partially
lined by normal squamous or pseudostratified columnar epithelium,
with a gradual transition through intraepithelial carcinoma to
invasive squamous cell carcinoma. This proposal represents the most
recent criteria for the diagnosis of BC.
The present study describes a case of BC that
fulfilled the criteria of Khafif et al (2) and was possibly caused by high-risk-type
human papillomavirus (HPV) infection. Written informed consent was
obtained from the patient for publication of this case report and
any accompanying images. This report adhered to the tenets of the
Declaration of Helsinki.
Case report
Patient data
A 56-year-old man, who was a non-smoker with
diabetes mellitus, presented to a referral hospital in 2012 with a
4-month history of a non-pulsatile mass on the right side of the
neck. At that time, no sore throat, fever, weight loss, cough or
otalgia were reported. The patient's blood sugar level was well
controlled with medication and the family history was unremarkable.
A physical examination had revealed a 6-cm non-tender mass, and
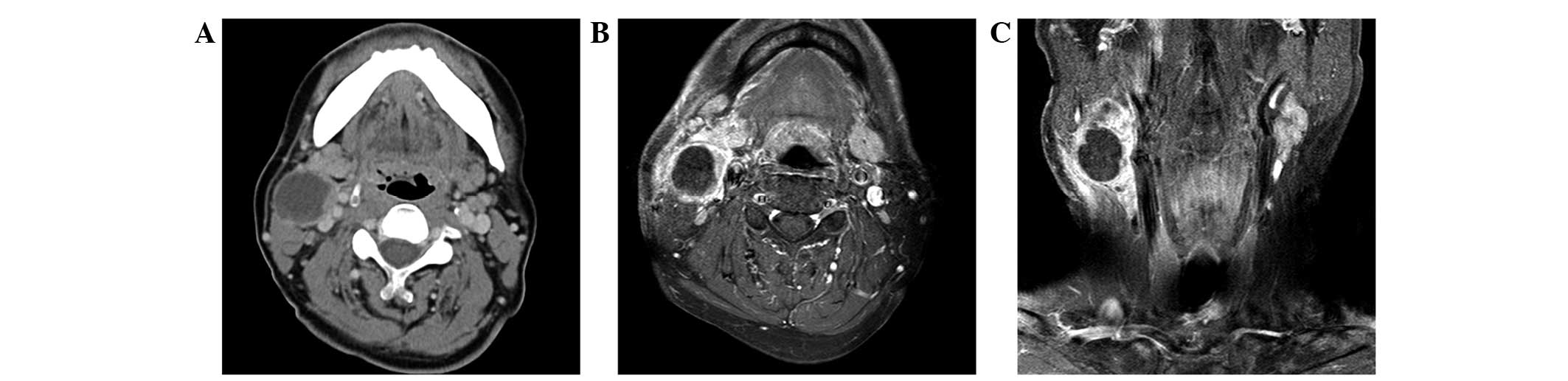
computed tomography (CT) and magnetic resonance imaging scans
showed a 3.6×5.0-cm, predominantly cystic mass, with a peripheral
solid component. The mass was located posterior to the
submandibular gland and anteromedial to the SCM muscle (Fig. 1). Several small lymph nodes in the
right neck were also detected on CT.
The patient was referred to the University Hospital,
University of the Ryukyus (Nishihara, Japan) for treatment of a
right neck lesion, 1 month subsequently to the intial visit to the
aforementioned hospital. Ultrasound-guided fine-needle aspiration
biopsy was reported as class V (squamous cell carcinoma). No tumor
was identified on endoscopic examination of the head and neck,
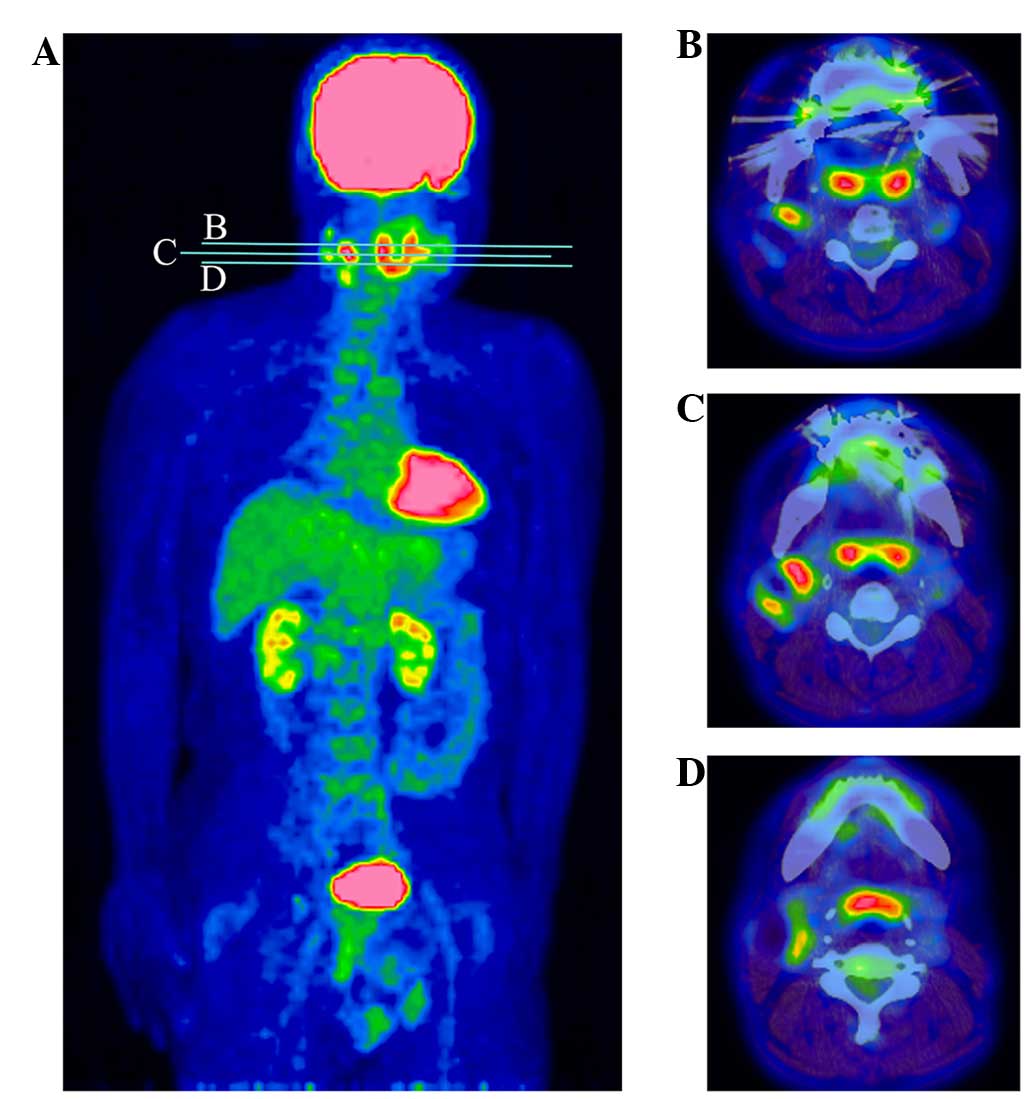
esophagus and stomach, or on thoracoabdominal CT. Positron emission
tomography/CT showed 18F-fluorodeoxyglucose (FDG) uptake
in the solid portion and cyst wall of the tumor (Fig. 2). Squamous cell carcinoma antigen in
the serum, a tumor marker for SCC, was slightly elevated at 1.9
ng/ml (normal, ≤1.5 ng/ml). No tumor was identified in random
biopsies of the nasopharynx, tongue base, bilateral palatine
tonsils, larynx and hypopharynx. A bilateral tonsillectomy was also
performed to exclude the possibility of lymph node metastasis from
an extremely small tonsillar carcinoma, but no cancerous lesion was
noted on examination of serial sections of the tonsils.
From the aforementioned history and findings, a
preliminary diagnosis of cervical lymph node metastasis with an
unknown primary site was formed, and a right neck dissection was
performed. Since the tumor adhered to the internal jugular vein and
SCM muscle, a radical neck dissection was performed.
Intraoperatively, several enlarged lymph nodes were noted around
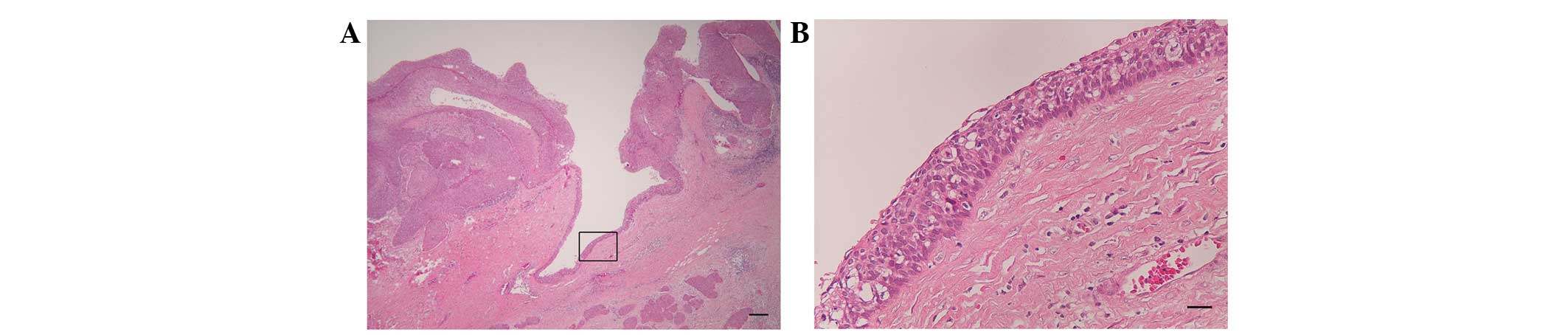
the tumor. Pathological examination revealed a cystic mass
containing poorly-differentiated, invasive squamous cell carcinoma
(Fig. 3A), with focal areas of normal
squamous epithelium and mild to severe dysplasia (Fig. 3B). In particular, there was transition
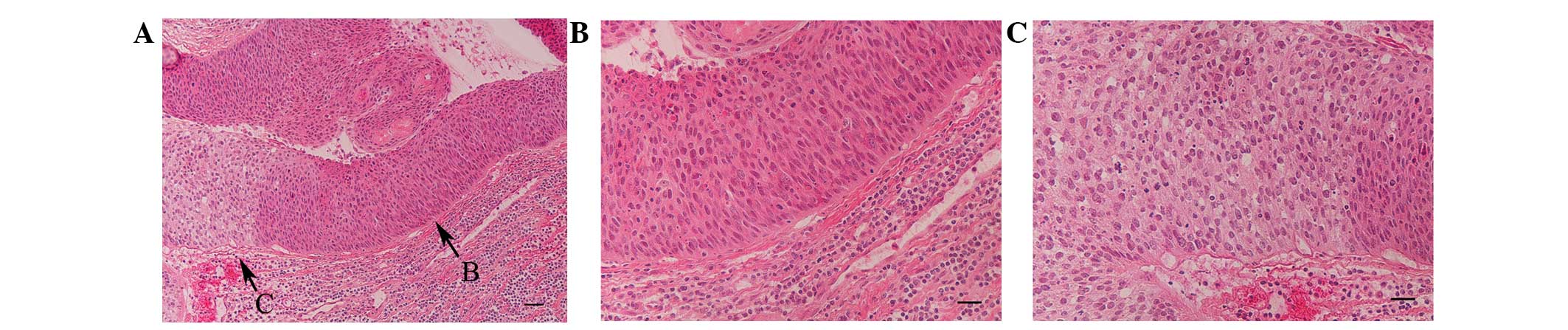
from dysplasia (Fig. 4A and B)
through intraepithelial carcinoma to invasive carcinoma with
pleomorphism and multiple mitoses (Fig.
4A and C). Koilocytosis was present in the areas of dysplasia
and carcinoma. An examination of the lymph nodes revealed 3 lymph
node metastases at level IIb, 5 at level III and 1 at level IV, and
none of the nodal metastases exhibited a cystic formation as was
observed in the main tumor. The surgical margins were negative.
Considering the clinical history, and the imaging
and histological findings, the tumor was diagnosed as BC,
fulfilling the diagnostic criteria proposed by Khafif et al
(2). Since lymph node metastases were
noted, concurrent chemoradiotherapy was administered with 50.4 Gy
irradiation to the entire neck, including the oropharynx, and two
cycles of nedaplatin plus 5-fluorouracil (3). Multiple lung metastases appeared at 6
months post-surgery, followed by the occurrence of brain
metastasis, despite several courses of docetaxel with nedaplatin
plus 5-fluorouracil (3). The patient
succumbed 1 year after surgery. No primary tumor or no lymph node
metastasis in the head and neck were noted at the time of
mortality.
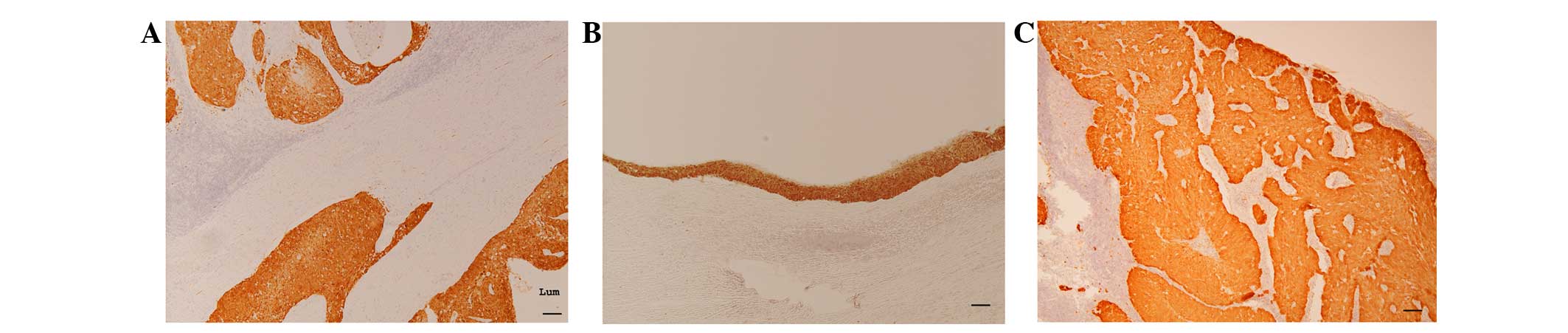
Immunohistochemical examination of
p16INK4a expression
The expression of p16INK4a was
investigated in the primary lesion, nodal metastases and bilateral
palatine tonsils, following the methods described in our previous
study (4). Strong p16INK4a
expression was observed in the squamous epithelium, dysplastic
epithelium and carcinoma within the BC (Fig. 5A and B). Notably, the nodal metastases
also exhibited strong p16INK4a expression (Fig. 5C). No expression was observed in
either palatine tonsil.
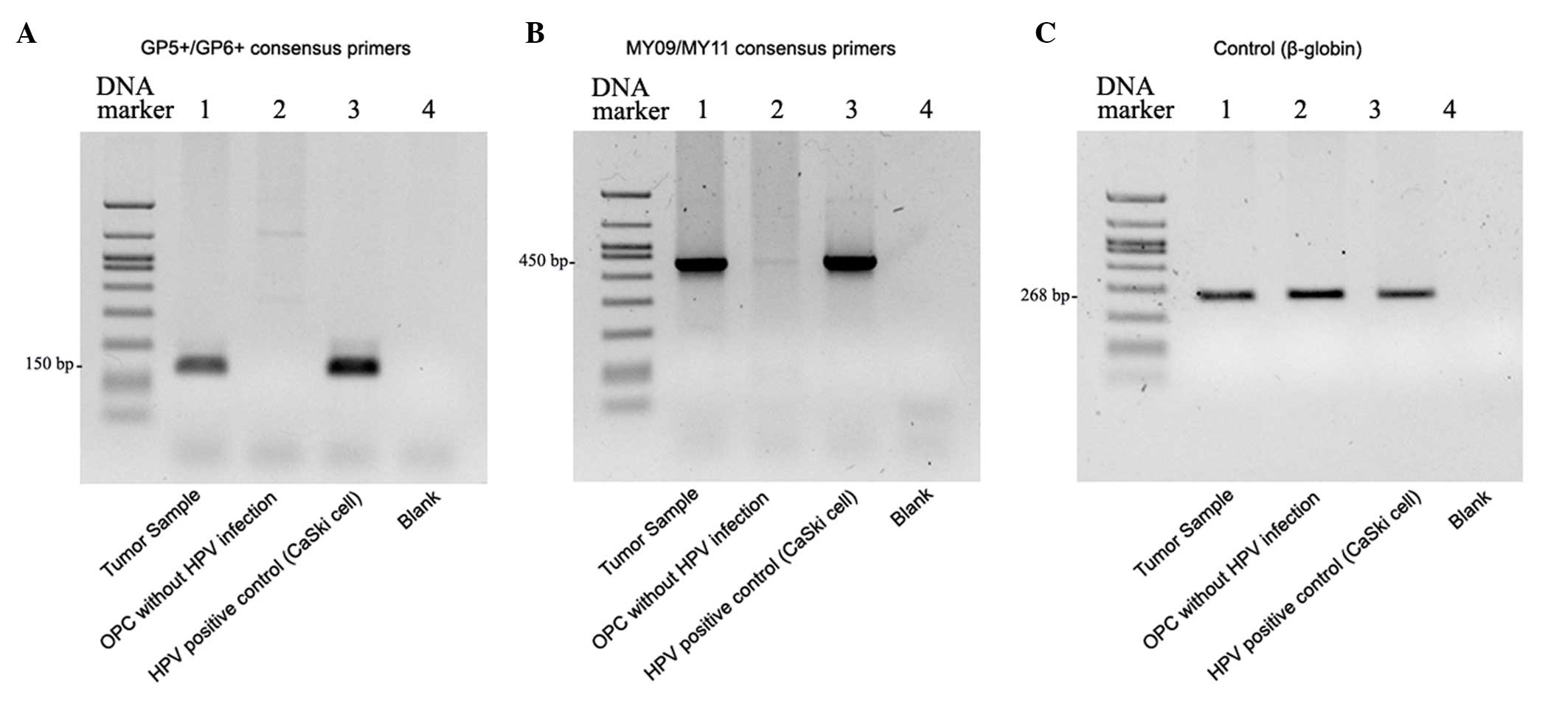
HPV infection, viral load and
integration status
A fresh specimen of BC was tested for the presence
of HPV, the viral load and the integration status, following the
methods described in our previous studies (5,6).
Polymerase chain reaction (PCR) for HPV using a consensus primer
was positive (Fig. 6). Direct
sequencing of the PCR product revealed the presence of HPV-16
infection. Quantitative PCR showed that the viral load of HPV-16
was 3.01×107/50 ng genomic DNA and that the E2/E6 ratio
was 0.13 (6); thus, the HPV-16
integration status was judged to be the mixed type.
Discussion
BC, an extremely rare primary tumor arising from the
remnant of the branchial pouches, is a rare tumor that was first
reported by Von Volkmann in 1882 (7).
However, BC has been considered a distinct entity only in the past
few decades. Since metastasis from OPC in the lymph nodes
frequently exhibits cystic formation, similar to that observed in
BC, recent reports have indicated that the majority of cystic
lesions previously diagnosed as squamous cell carcinoma were lymph
node metastases from OPC, particularly tonsillar carcinoma
(8–10). Yasui et al (10) reported that an occult HPV-positive
primary tumor will most likely occur in the oropharynx and that
determining the HPV status of fine-needle aspirates facilitates the
diagnosis of cystic node metastasis.
The present case matched the criteria proposed by
Khafif et al (2), but did not
match those proposed by Martin et al (1), as the patient succumbed to distant
metastasis within a 5-year period. Since normal squamous epithelium
at the cyst wall and transition from dysplasia to carcinoma were
observed, the case was judged to be a typical BC.
There was evidence of high-risk-type HPV infection
and integration in the tumor, with a high viral load. In a previous
study (6), the viral load in
tonsillar carcinoma with HPV-16 infection ranged from
1.54×102-1.34×107/50 ng genomic DNA (median,
4.13×105 ng). Compared with the viral load in tonsillar
carcinoma with HPV infection, the viral load in the present case
was quite high. To determine the physical status of HPV-16, the
present study applied quantitative PCR, as described in our
previous study (6). Tonsillar
carcinoma with high-risk-type HPV infection usually shows HPV
integration (6), which suggests that
malignant transformation of branchiogenic cyst may arise from
high-risk-type HPV infection and integration. To the best of our
knowledge, the present study is the first report in the English
literature to demonstrate a close association between BC and HPV
infection. The marked koilocytosis and p16INK4a
expression in the squamous epithelium, dysplastic epithelium and
cancerous areas support this assumption.
The prognosis of patients with OPC associated with
HPV infection is better than that for those individuals without HPV
infection (11). The treatment
regimen for OPC associated with HPV infection that was used in the
present results in a 5-year overall survival rate of >90%
(3,5).
Despite the presence of HPC infection, the present case had a
disease course that was different from OPC associated with HPV
infection. This suggests that BC associated with HPV infection may
have different clinical characteristics compared with OPC
associated with HPV infection.
It remains unclear why high-risk-type HPV infects
the branchiogenic cyst or carcinoma. One possible explanation is
that HPV infects the palatine tonsils and enters the branchial cyst
though the remnant or a patent communicating route. However, the
present study was unable to identify a communication between the
oropharyngeal cavity and BC, as a tonsillectomy was performed prior
to the neck dissection. The aforementioned experimental data
suggest that persistent HPV infection in the cyst causes HPV
integration and malignant transformation. However, further studies
are required to confirm this.
In conclusion, this is the first report of BC
associated with high-risk-type HPV infection. Although there may be
fewer BC than cystic lymph node metastases from OPC, a HPV-positive
neck mass is not necessarily associated with OPC, but can also
occur with BC that has a poor prognosis. This study provides
further evidence of the existence of BC and proposes that the cause
is HPV infection.
Acknowledgements
This study was supported by grants KAKENHI 23592534,
KAKENHI 26462610 and KAKENHI 26462611 awarded by the Japan Society
for the Promotion of Science. The authors would like to thank the
Ryukyu Society for the Promotion of Oto-Rhino-Laryngology for
proving editorial assistance and technical assistance.
Glossary
Abbreviations
Abbreviations:
|
BC
|
branchiogenic carcinoma
|
|
CT
|
computed tomography
|
|
FDG
|
18F-fluorodeoxyglucose
|
|
HPV
|
human papillomavirus
|
|
OPC
|
oropharyngeal carcinoma
|
|
PCR
|
polymerase chain reaction
|
|
SCM
|
sternocleidomastoid
|
References
|
1
|
Martin H, Morfit HM and Ehrlich H: The
case for branchiogenic cancer (malignant branchioma). Ann Surg.
132:867–887. 1950. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Khafif RA, Prichep R and Minkowitz S:
Primary branchiogenic carcinoma. Head Neck. 11:153–163. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hasegawa M, Maeda H, Deng Z, Kiyuna A,
Ganaha A, Yamashita Y, Matayoshi S, Agena S, Toita T, Uehara T and
Suzuki M: Prediction of concurrent chemoradiotherapy outcome in
advanced oropharyngeal cancer. Int J Oncol. 45:1017–1026.
2014.PubMed/NCBI
|
|
4
|
Deng Z, Hasegawa M, Aoki K, Matayoshi S,
Kiyuna A, Yamashita Y, Uehara T, Agena S, Maeda H, Xie M and Suzuki
M: A comprehensive evaluation of human papillomavirus positive
status and p16INK4a overexpression as a prognostic biomarker in
head and neck squamous cell carcinoma. Int J Oncol. 45:67–76.
2014.PubMed/NCBI
|
|
5
|
Deng Z, Hasegawa M, Yamashita Y, Matayoshi
S, Kiyuna A, Agena S, Uehara T, Maeda H and Suzuki M: Prognostic
value of human papillomavirus and squamous cell carcinoma antigen
in head and neck squamous cell carcinoma. Cancer Sci.
103:2127–2134. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Deng Z, Hasegawa M, Kiyuna A, Matayoshi S,
Uehara T, Agena S, Yamashita Y, Ogawa K, Maeda H and Suzuki M:
Viral load, physical status, and E6/E7 mRNA expression of human
papillomavirus in head and neck squamous cell carcinoma. Head Neck.
35:800–808. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Von Volkmann R: Deep branchiogenic neck
carcinoma. Zentralbl Chir. 9:49–63. 1882.(In German).
|
|
8
|
Thompson LD and Heffner DK: The clinical
importance of cystic squamous cell carcinomas in the neck: A study
of 136 cases. Cancer. 82:944–956. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Goldenberg D, Sciubba J and Koch WM:
Cystic metastasis from head and neck squamous cell cancer: A
distinct disease variant? Head Neck. 28:633–638. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yasui T, Morii E, Yamamoto Y, Yoshii T,
Takenaka Y, Nakahara S, Todo T and Inohara H: Human papillomavirus
and cystic node metastasis in oropharyngeal cancer and cancer of
unknown primary origin. PLoS One. 9:e953642014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ang KK, Harris J, Wheeler R, Weber R,
Rosenthal DI, Nguyen-Tân PF, Westra WH, Chung CH, Jordan RC, Lu C,
et al: Human papillomavirus and survival of patients with
oropharyngeal cancer. N Engl J Med. 363:24–35. 2010. View Article : Google Scholar : PubMed/NCBI
|