Introduction
Hemangioblastomas (HBMs) are highly vascular tumors
of the central nervous system, which represent 1.5–2.5% of all
intracranial tumors (1). HBMs may
occur sporadically in the central nervous system or in association
with von Hippel-Lindau disease (2).
Morphologically, HBMs appear as solid, solid-cystic or mainly
cystic with a small mural, vascularized nidus. Sporadic HBMs are
nearly always solitary, due to their highly vascular nature. The
characteristics of solid variants of HBMs, including a clear
vascular blush, multiple feeding vessels and draining veins on
digital subtraction angiography (DSA) (3), are similar to intracranial arteriovenous
malformations (AVMs) (4,5), and to the best of our knowledge, a case
of an HBM in the cerebellum mimicking an aneurysm have never been
reported in the literature. The present study reports a case of a
cerebellar HBM mimicking an aneurysm that was treated via surgical
resection. The patient provided written informed consent for
publication of this case report and any accompanying images.
Case report
A 52-year-old man presented with a 4-year history of
intermittent headaches at the Tsinghua University Yuquan Hospital
(Beijing, China) in January 2015. No other nervous system deficits
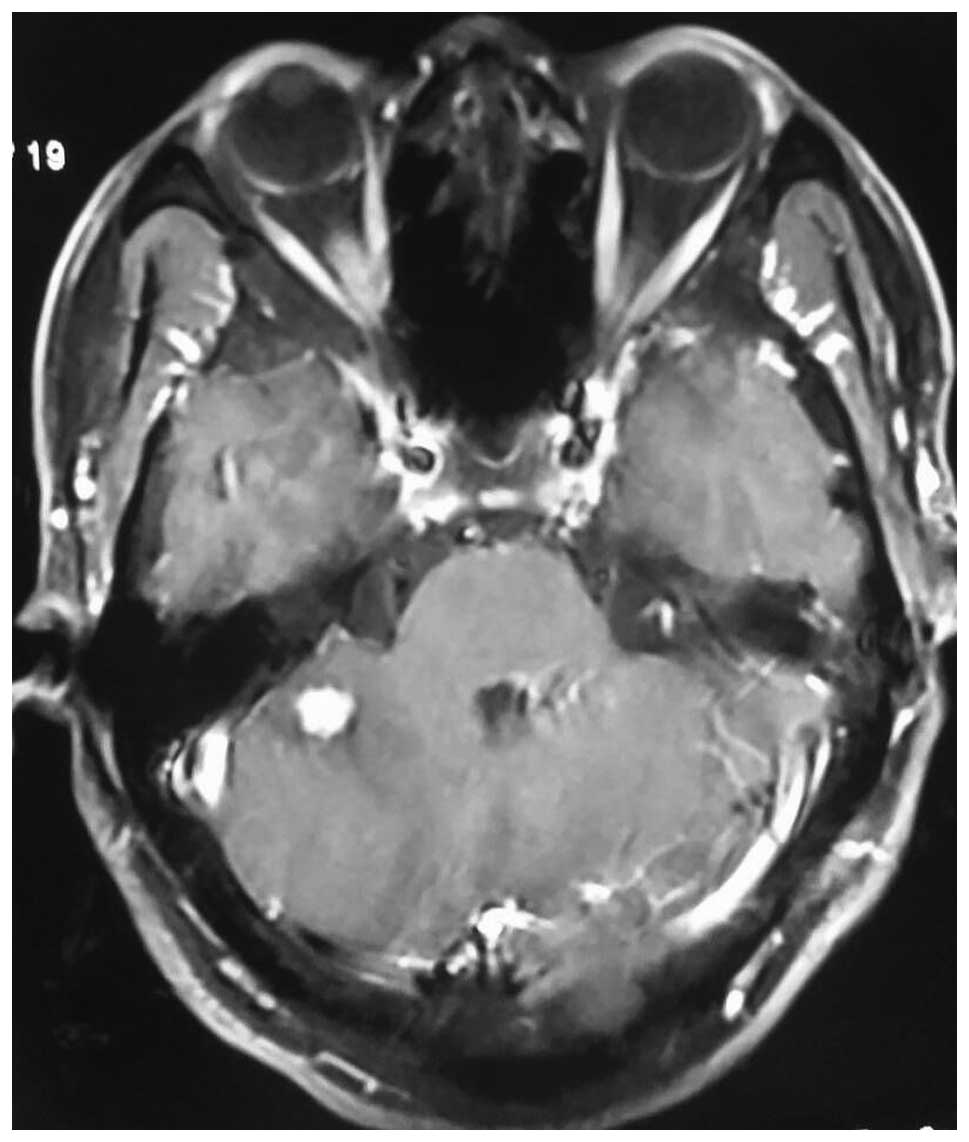
were found. Brain computed tomography (Fig. 1) and magnetic resonance imaging (MRI)
(Fig. 2) revealed a 0.9×0.9-cm mass
on the right cerebellar hemisphere and showed significant contrast
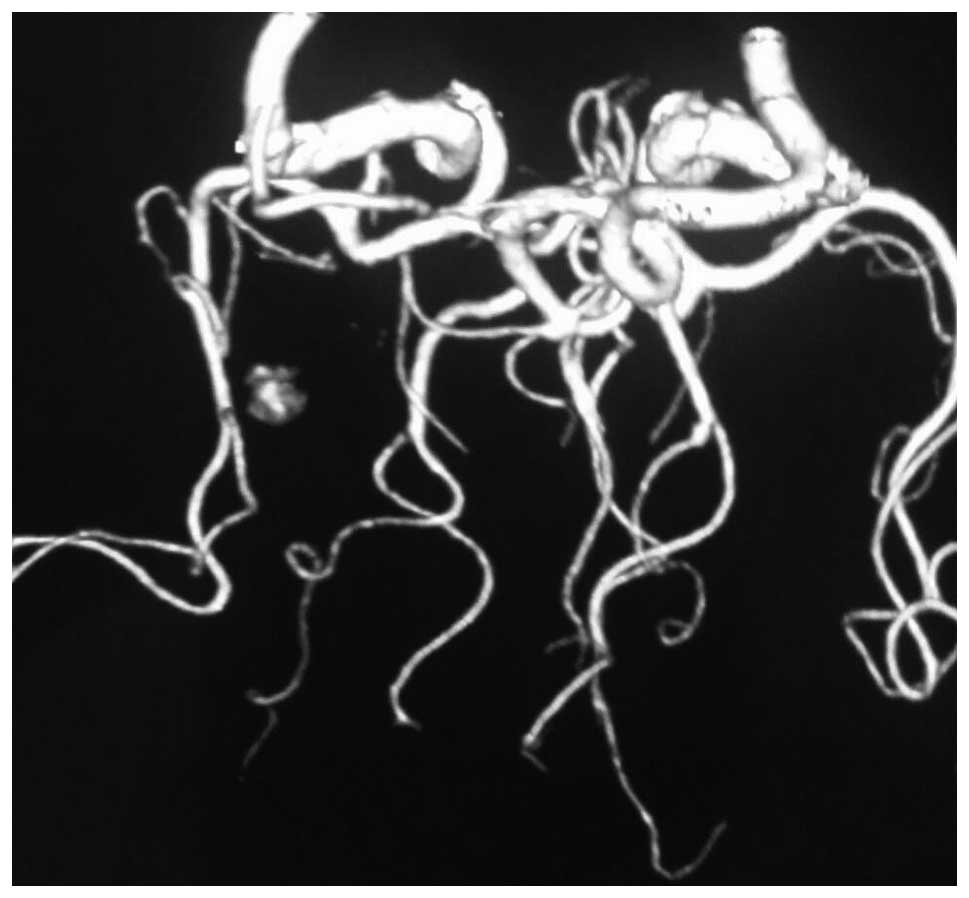
enhancement. MR angiography demonstrated a significant vascular
blush supplied from the right posterior inferior cerebellar artery
(PICA) (Fig. 3). All these results
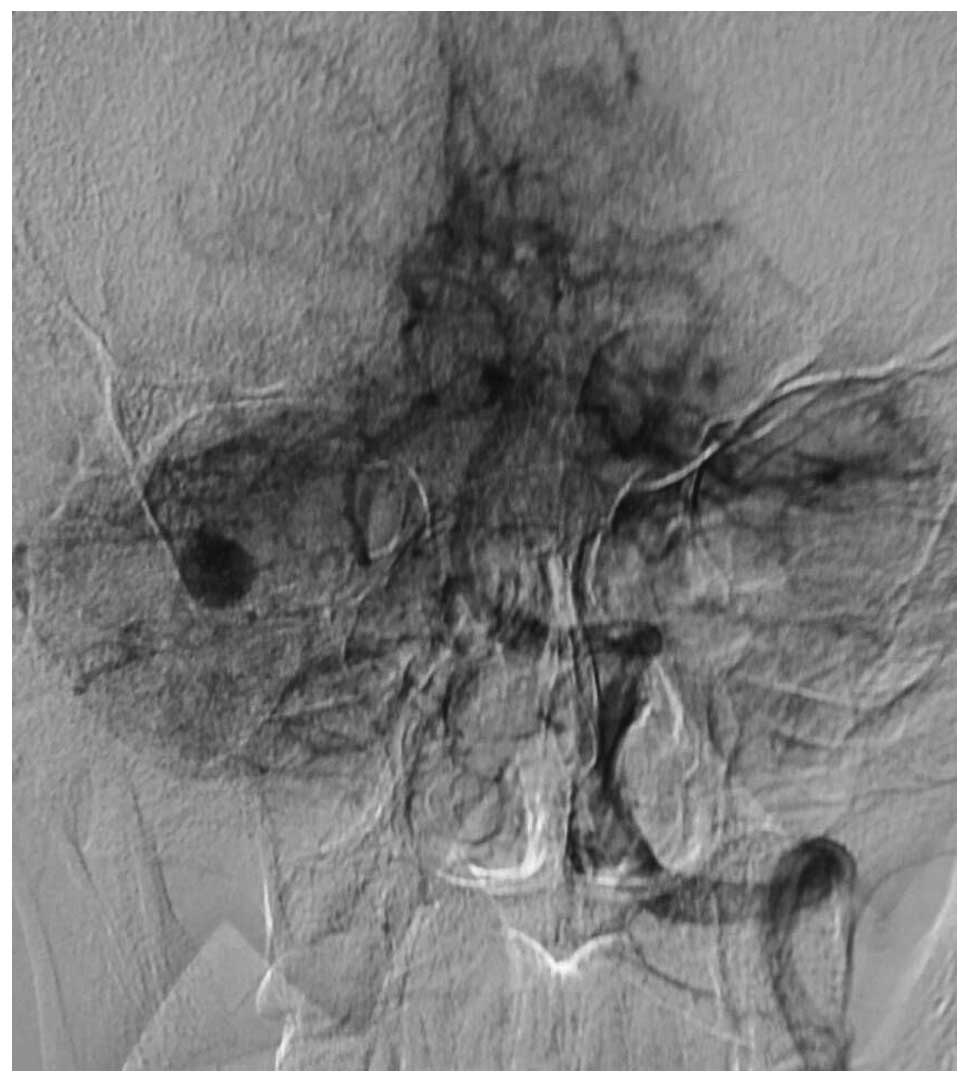
were consistent with an aneurysm. Lateral vertebral artery DSA then
showed a highly vascular tumor nodule supplied by the right PICA
(Fig. 4), so a diagnosis of an
aneurysm originating from the PICA was considered.
The patient was scheduled to undergo a suboccipital
retrosigmoid craniotomy, however, during the procedure the
suspected aneurysm was found to be an HBM and the surgical strategy
was changed. A total resection of the tumor was performed without
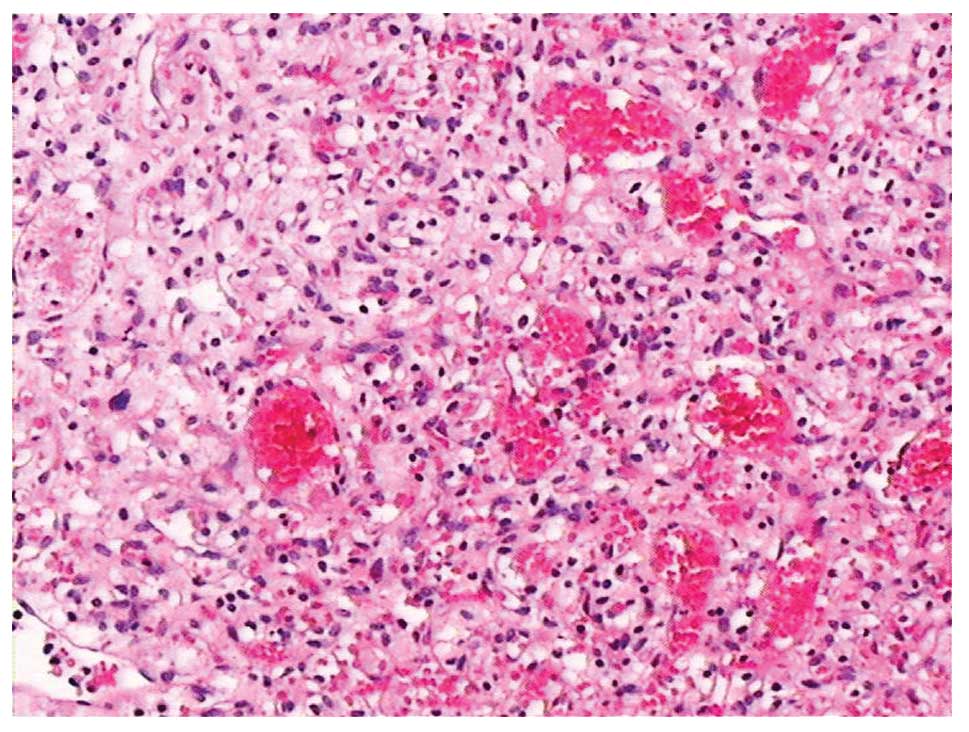
any complications. The tumor was pathologically confirmed as HBM
due to the results of a histological examination of the excised
mass. Briefly, resected tissues were fixed in formalin,
parrafin-embedded and cut into 4-µm sections, prior to staining
with hematoxylin and eosin and visualization under a light
microscope. The histopathological analysis revealed that the tumor
was composed of stromal cells and abundant vascular endothelial
cells (Fig. 5). Follow-up MRI
performed at 1 and 6 months post-surgery showed no evidence of
recurrence.
Discussion
According to the World Health Organization (6), HBMs are classified as grade I tumors,
with a highly vascularized solid tumor component. The tumors mainly
occur in the cerebellar hemisphere, spinal cord and brain stem
(7), but are rarely found in the
supratentorial region (8) due to its
high degree of vascularity. HBMs are easily misdiagnosed as AVMs or
intracranial aneurysms.
HBMs that appear as mainly cystic with a small
nodule are diagnosed easily due to their typical imaging
characteristic. However, solid HBMs present as round-shaped masses,
which are iso- or hypodense on T1-weighted images and hyperdense on
T2-weighted images, together with a significant contrast
enhancement pattern. Serpiginous flow voids are found on T1- and
T2-weighted images, which are characteristic of solid HBMs
(9). It is crucial to form a
differential diagnosis between solid HBM and vascular diseases
pre-operatively, particularly between AVM and aneurysm. An AVM
nidus presents as a dense vascular network similar to an HBM
nodule. However, HBMs may cause mass effects, which leads to
neurological symptoms. Moreover, HBMs present with a microvascular
structure that is similar to a normal capillary bed, whereas an AVM
nidus is formed from altered vessels with no actual capillary bed
(10). HBMs may coexist with
intracranial aneurysms due to hemodynamic stress mechanisms.
Therefore, an intracranial aneurysm should also be considered when
hemorrhage caused by HBM occurs (11). DSA is necessary for the differential
diagnosis of HBM, since it permits the identification of the
feeding artery and enlargement of draining veins (12). As was shown in the present case, the
characteristics on DSA are similar to an aneurysm originating from
the PICA, therefore, a tumor may wrongly be considered as an
aneurysm prior to surgery.
Surgical resection is the major treatment for HBMs
due to their benign features. However, surgical treatment is often
challenging, particularly for solid tumors with a highly
vascularized nature, and the mortality associated with the biopsy
or removal of a solid HBM is high. Therefore, internal
decompression and any attempt at biopsy or partial resection should
be avoided (13). With the
progression of microsurgical techniques, it is now feasible to
remove these tumors totally (3). The
successful resection of a solid HBM should follow the principles of
an AVM dissection. This means that feeding arteries should be
identified and blocked first, followed by tumor dissection and
occlusion of the draining veins. As the premature obliteration of
the venous drainage can result in terminal intraoperative swelling
and hemorrhage, a circumferential dissection with devascularization
and en bloc removal is favored whenever possible in solid tumors.
Importantly, all surgical instruments, including those for the
alternative procedure, should be made ready pre-operatively. The
surgical strategy should then be changed when the misdiagnosis is
identified intraoperatively.
Debate remains over whether the pre-operative
embolization of an HBM should be performed. It has been suggested
that the pre-operative embolization of an HBM can facilitate
surgical removal and allow complete tumor resection by
significantly reducing the tumor blood supply (14), controlling the inaccessible artery
supply and reducing the vascularity of the tumor (15). Occasionally, pre-operative
embolization may significantly avoid profuse intraoperative
bleeding. However, it has also been reported that pre-operative
embolization using particles has a high risk for acute tumor
bleeding and mortality (16). In our
opinion, the pre-operative embolization of HBM can reduce the risk
of intraoperative bleeding and shorten the surgical duration, which
may result in the improved success of a tumor resection and reduced
surgical complications.
The effectiveness of radiotherapy or chemotherapy in
HBM has been questioned (17–19). Although certain studies have
demonstrated that pre-operative radiotherapy can control local
tumor progression and finally facilitate complete and safe tumor
removal (4,20), the long-term results of radiosurgery
require confirmation (18).
Therefore, we believe that radiotherapy or chemotherapy should only
be used for residual or recurrent tumors post-operatively.
Solid HBMs are easily misdiagnosed as AVMs or
intracranial aneurysms due to their high degree of vascularity. DSA
is necessary to make the differential diagnosis and microsurgical
resection is the treatment of choice due to the benign features of
the disease. Pre-operative embolization can increase the surgical
effectiveness and reduce the complications. Assistant therapies
should only be used for residual or recurrent tumors after
microsurgery.
In conclusion, the present study described the case
of a 52-year-old male patient who presented with HBM mimicking an
aneurysm on DSA preoperatively, which was confirmed as HBM during
surgery via a histopathological analysis. The tumor was totally
resected according to the principles of an AVM dissection, and no
recurrence was found in follow-up MRI. This case demonstrates that
HBM may be easily misdiagnosed as an aneurysm.
References
|
1
|
Resche F, Moisan JP, Mantoura J, de
Kersaint-Gilly A, Andre MJ, Perrin-Resche I, Menegalli-Boggelli D,
Lajat Y and Richard S: Haemangioblastoma, haemangioblastomatosis,
and von Hippel-Lindau disease. Adv Tech Stand Neurosurg.
20:197–304. 1993.PubMed/NCBI
|
|
2
|
Conway JE, Chou D, Clatterbuck RE, Brem H,
Long DM and Rigamonti D: Hemangioblastomas of the central nervous
system in von Hippel-Lindau syndrome and sporadic disease.
Neurosurgery. 48:55–62; discussion 62-63. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Rachinger J, Buslei R, Prell J and Strauss
C: Solid haemangioblastomas of the CNS: A review of 17 consecutive
cases. Neurosurg Rev. 32:37–47. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kamitani H, Hirano N, Takigawa H, Yokota
M, Miyata H, Ohama E and Watanabe T: Attenuation of vascularity by
preoperative radiosurgery facilitates total removal of a
hypervascular hemangioblastoma at the cerebello-pontine angle: Case
report. Surg Neurol. 62:238–243; discussion 243-244. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dow GR, Sim DW and O'Sullivan MG: Excision
of large solid haemangioblastomas of the cerebellopontine angle by
a skull base approach. Br J Neurosurg. 16:168–171. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Louis DN, Ohgaki H, Wiestler OD, Cavenee
WK, Burger PC, Jouvet A, Scheithauer BW and Kleihues P: The 2007
WHO Classification of Tumours of the Central Nervous System. Acta
Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hussein MR: Central nervous system
capillary haemangioblastoma: The pathologist's viewpoint. Int J Exp
Pathol. 88:311–324. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim H, Park IS and Jo KW: Meningeal
supratentorial hemangioblastoma in a patient with von hippel-lindau
disease mimicking angioblastic menigioma. J Korean Neurosurg Soc.
54:415–419. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
González M Gelabert: Posterior fossa
hemangioblastomas. Neurologia. 22:853–859. 2007.(In Spanish).
PubMed/NCBI
|
|
10
|
de San Pedro JR, Rodríguez FA, Níguez BF,
Sánchez JF, López-Guerrero AL, Murcia MF and Vilar AM: Massive
hemorrhage in hemangioblastomas literature review. Neurosurg Rev.
33:11–26. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Suzuki M, Umeoka K, Kominami S and Morita
A: Successful treatment of a ruptured flow-related aneurysm in a
patient with hemangioblastoma: Case report and review of
literature. Surg Neurol Int. 5(Suppl 9): S430–S433. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Takeuchi S, Tanaka R, Fujii Y, Abe H and
Ito Y: Surgical treatment of hemangioblastomas with presurgical
endovascular embolization. Neurol Med Chir (Tokyo). 41:246–252.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Okawara SH: Solid cerebellar
hemangioblastoma. J Neurosurg. 39:514–518. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dabus G, Pryor J, Spilberg G, Samaniego EA
and Nogueira RG: Embolization of intra-axial hypervascular tumors
with Onyx: Report of three cases. J Neurointerv Surg. 5:177–180.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Standard SC, Ahuja A, Livingston K,
Guterman LR and Hopkins LN: Endovascular embolization and surgical
excision for the treatment of cerebellar and brain stem
hemangioblastomas. Surg Neurol. 41:405–410. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cornelius JF, Saint-Maurice JP, Bresson D,
George B and Houdart E: Hemorrhage after particle embolization of
hemangioblastomas: Comparison of outcomes in spinal and cerebellar
lesions. J Neurosurg. 106:994–998. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Capitanio JF, Mazza E, Motta M, Mortini P
and Reni M: Mechanisms, indications and results of salvage systemic
therapy for sporadic and von Hippel-Lindau related
hemangioblastomas of the central nervous system. Crit Rev Oncol
Hematol. 86:69–84. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Niemelä M, Lim YJ, Söderman M,
Jääskeläinen J and Lindquist C: Gamma knife radiosurgery in 11
hemangioblastomas. J Neurosurg. 85:591–596. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pan L, Wang EM, Wang BJ, Zhou LF, Zhang N,
Cai PW and Da JZ: Gamma knife radiosurgery for hemangioblastomas.
Stereotact Funct Neurosurg. 70(Suppl 1): S179–S186. 1998.
View Article : Google Scholar
|
|
20
|
Moss JM, Choi CY, Adler JJ Jr, Soltys SG,
Gibbs IC and Chang SD: Stereotactic radiosurgical treatment of
cranial and spinal hemangioblastomas. Neurosurgery. 65:79–85. 2009.
View Article : Google Scholar : PubMed/NCBI
|