Introduction
As a common tumour observed in urinary surgery, the
incidence rate of renal cell carcinoma accounts for 5% of carcinoma
cases in adults and is increasing by 4% per year. In addition, its
prevalence tends to be higher among young people relative to other
forms of carcinoma (1). With the
development of physical examination and imaging screening
technology, the rates of early detection, treatment, and recovery
of early stage renal cell carcinoma are improving. Surgical
operation is the main treatment method for early stage renal cell
carcinoma.
Retroperitoneoscopic radical operation of renal cell
carcinoma has been established among micro-invasive methods and its
resection rate, survival rate, incidence rate of complications and
recurrence rate are close to those of open operation (2,3). The
development of radiofrequency ablation (RFA) has improved
micro-invasive treatment techniques of small renal cell carcinoma.
With the guidance of CT, ultrasound, or MRI, and by laparoscopic or
open approach, RFA is performed by inserting monopolar or cluster
electrodes into tumour tissue. Heat generated from ions surrounding
the electrode needle are transferred to adjacent tissues around the
tumour to make tumour tissue dry and dehydrated, causing
coagulative necrosis. Therefore, rounded or spherical ablation
areas are formed as a means to kill tumour tissues (4,5). RFA has
shown good clinical outcomes for patients who are in middle and
late stage renal cell carcinoma and cannot receive open operations
or are limited to palliative treatment (6). Currently, there are few reports
regarding RFA treatment on early stage small renal cell carcinoma
and there has been no prospective study analysis.
Therefore, the aim of the present study was to
analyze the safety and effectiveness of percutaneous RFA, in
comparison to retroperitoneoscopic radical operation, in the
treatment of early stage renal cell carcinoma.
Patients and methods
Patient data
A total of 76 cases of early stage renal cell
carcinoma that were diagnosed in Yidu Central Hospital of Weifang
(Qingzhou, China) from January, 2011 to January, 2013 were selected
for the study. Diagnoses were clinically confirmed through
ultrasound, CT, intravenous urography and histopathology
examination. Inclusion criteria were: i) No renal vein, inferior
vena cava or renal pedicle lymph node involvement and no distant
metastasis of the tumour; ii) diameter of solidary tumour of
<4.0 cm; iii) clinical stage was classified as T1N0M0; iv) no
abdominal infection or surgical history; and v) important organs,
such as heart, lung and brain, were normal in routine examination
before operation. Exclusion criteria were: i) Abnormal coagulation
function; ii) abnormal contralateral renal function; and iii)
follow-up materials were incomplete.
After reviewing protocol and risks with patients and
their family members, we received informed and signed consent.
Patients were then randomly assigned into either the observation
group (41 cases) or the control group (35 cases). In the
observation group, there were 27 males and 14 females, ages 35–69
years, and with an average age of 53.5±12.3 years. Their average
tumour diameter was 2.73±0.85 cm. In the control group, there were
22 males and 13 females, aged 32–67 years, and with an average age
of 51.8±13.2 years. Their average tumour diameter was 2.54±0.80 cm.
There were no statistically significant differences in the above
factors between the two patient groups (P>0.05).
Study methods
Patients in the two groups were taken care of by the
same operation and nursing team and all procedures were conducted
based on standard medical procedures. For the observation group,
ultrasound was used to guide percutaneous RFA treatment as follows:
General anesthesia was administered with the patient in prone
position. A radiofrequency probe was inserted under the guidance of
ultrasound. RFA was then performed by passing the electrode through
the tumour tissue, with routine biopsy. An open cold circulating
pump and a radiofrequency generator were used to perform RFA for 1
cycle (12 min). The tissue temperature was set to remain elevated
>60°C after the treatment was stopped in order to ensure
termination of tumour cells. Repeated points and frequencies of RFA
were performed as necessary. For the control group,
retroperitoneoscopic radical operation of renal cell carcinoma was
performed, as follows: General anesthesia was administered with the
patient's healthy side in lateral position and the waist elevated.
The first puncturing hole was at the costal margin of posterior
axillary line. A self-made balloon dilator was put through the
incision to establish retroperitoneal space. The incision was
extended at the costal margin of posterior axillary line and then
the tumour was excised accordingly. Resected kidney samples were
put into self-made specimen bags to be sent for testing.
Observation methods
i) Operative conditions of the two groups were
recorded and compared, including operation time, blood loss during
operation, length of stay and incidence rate of complications after
the operation. ii) Collection and comparison of serum C-reactive
protein (CRP), interleukin (IL)-6 and T lymphocyte count changes
was done before the operation and 1, 2 and 3 days afterwards. iii)
Response evaluation criteria in solid tumours was used to compare
recent clinical effects between the two groups, including complete
remission, partial remission, stable, and progress. iv) Follow-up
was carried out on the two groups to compare tumour-free survival
time and survival rate.
Statistical analysis
SPSS 22.0 statistical software (IBM SPSS, Armonk,
NY, USA) was used for data processing and statistical analyses.
Data were presented as mean values with ± standard deviation.
Comparisons between groups were made using independent samples
t-tests and comparisons within one group at different time points
were done by analysis of variance for repeated measures.
Enumeration data were presented as cases or (%) and the comparison
between groups was made using Chi-square test. Comparison of ranked
data was made using the Mann-Whitney U test. The Kaplan-Meier model
was used to assess tumour-free survival time and log-rank test was
used to assess survival distribution. For all tests, P<0.05 was
considered to indicate a statistically significant difference.
Results
Comparison of operation
conditions
In the observation group, operation time, blood loss
during operation and length of stay were all lower than those in
control group, with the differences each statistically significant
(P<0.05, Table I).
 | Table I.Comparison of operation conditions
between patients of the observation group (n=41) and the control
group (n=35). |
Table I.
Comparison of operation conditions
between patients of the observation group (n=41) and the control
group (n=35).
| Groups | Operation time
(min) | Blood loss during
operation (ml) | Length of stay
(day) |
|---|
| Observation | 51.8±9.7 | 12.8±4.7 |
6.9±1.2 |
| Control | 101.3±14.7 | 117.5±32.8 | 10.7±3.3 |
| t-test |
8.598 | 18.329 | 5.544 |
| P-value | <0.001 | <0.001 | 0.036 |
Comparison of incidence rate of
operative complications
The incidence rate of operative complications in the
observation group was lower than that of the control group and the
difference was statistically significant (P<0.05, Table II).
 | Table II.Comparison of incidence rates of
operative complications [cases, (%)] |
Table II.
Comparison of incidence rates of
operative complications [cases, (%)]
| Groups | Cases | Acute renal
failure | Infection | Delayed bleeding | Seroperitoneum | Abdominal
adhesion | Total incidence
rate |
|---|
| Observation | 41 | 1 | 0 | 1 | 1 | 1 | 4 (9.8) |
| Control | 35 | 3 | 1 | 3 | 1 | 2 | 10 (28.6) |
| χ2 |
|
|
|
|
|
| 4.448 |
| P-value |
|
|
|
|
|
| 0.035 |
Comparison of serum CRP, IL-6 and T
lymphocyte counts
For both groups, serum CRP, IL-6 and T lymphocyte
counts on 1, 2 and 3 days after operation were all increased over
time (P<0.05). However, counts from the control group all showed
a greater increase for all time points, compared to the observation
group, and the differences were of statistical significance
(P<0.05, Table III).
 | Table III.Comparison of serum CRP, IL-6 and T
lymphocyte count between groups. |
Table III.
Comparison of serum CRP, IL-6 and T
lymphocyte count between groups.
| Groups | Time | CRP (mg/l) | IL-6 (ng/l) | Lymphocyte count
(×109/l) |
|---|
| Observation | Before operation | 2.55±0.81 | 1.83±0.25 | 2.16±0.64 |
|
| 1 day after
operation | 6.37±2.10 | 5.42±1.42 | 2.76±0.42 |
|
| 2 days after
operation | 7.49±2.06 | 6.67±1.85 | 2.68±0.25 |
|
| 3 days after
operation | 7.27±2.96 | 6.31±1.16 | 2.55±0.31 |
| Control | Before operation | 2.49±0.78 | 1.76±0.33 | 2.33±0.72 |
|
| 1 day after
operation | 7.73±2.29 | 6.30±1.48 | 2.88±1.06 |
|
| 2 days after
operation | 8.43±2.20 | 7.44±1.96 | 2.74±0.57 |
|
| 3 days after
operation | 8.35±2.67 | 7.22±1.84 | 2.60±0.61 |
Comparison of recent effects between
patients in the two groups
The differences in recent effects between patients
of the two groups were of no statistical significance (P>0.05,
Table IV).
 | Table IV.Comparison of recent effects between
patients in the two groups [cases, (%)]. |
Table IV.
Comparison of recent effects between
patients in the two groups [cases, (%)].
| Groups | Cases | CR | PR | SD | PD | Total effective
rate |
|---|
| Observation | 41 | 9
(22.0) | 21 (51.2) | 6 (14.6) | 5 (12.2) | 36 (87.8) |
| Control | 35 | 14 (40.0) | 10 (28.6) | 7 (20.0) | 4 (11.4) | 31 (88.6) |
| χ2 |
|
| 4.799 |
| 0.000 |
| P-value |
|
| 0.187 |
| 1.000 |
Comparison of tumour-free survival
time and survival rate during follow-up between the two groups
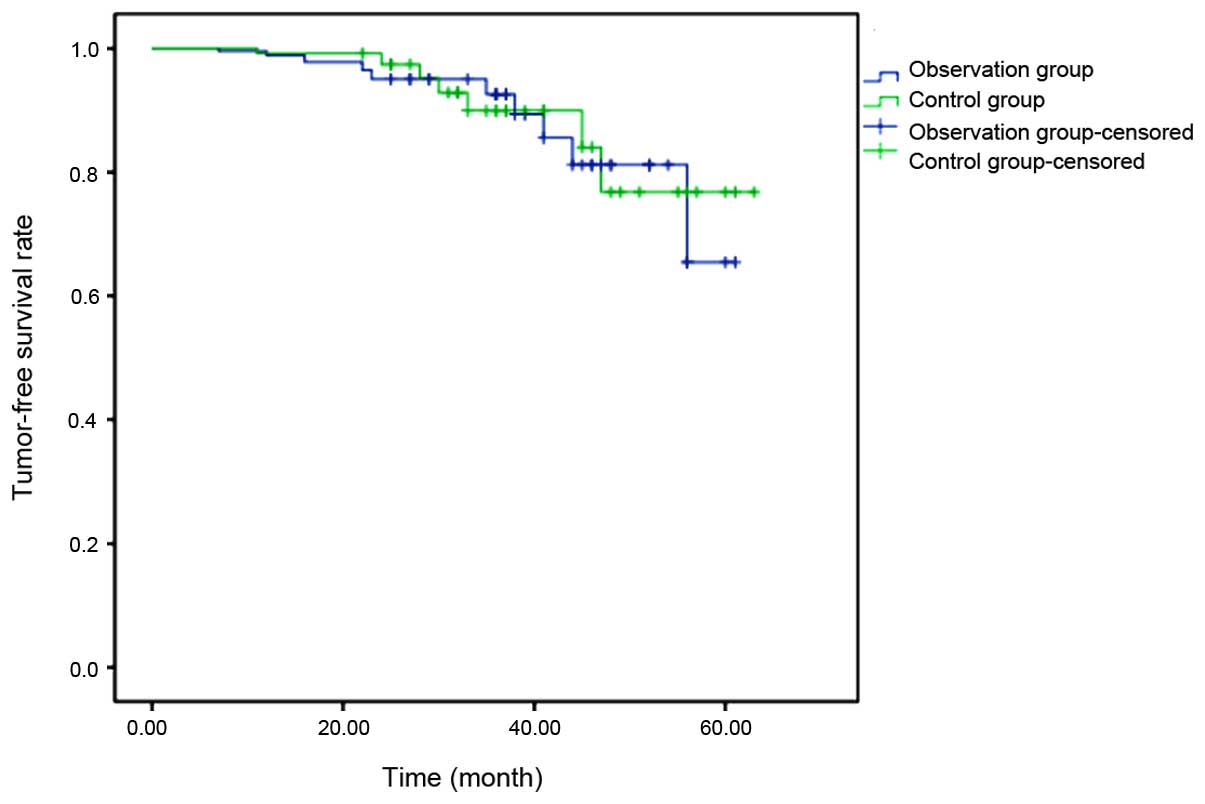
The median follow-up time after operation for the
two groups was 4.8 years and there were no statistically
significant differences in tumour-free survival time (43.6 vs. 45.7
months, χ2=2.021, P=0.125;) and survival rate (88.6
(31/35) vs. 85.4% (35/41); χ2=0.005, P=0.943) between
them (Fig. 1).
Discussion
It has been demonstrated by several studies
(7,8)
that RFA can be used as an effective alternative as a minimally
invasive treatment plan for localized tumours. It has been shown
through cell staining techniques that, after RFA treatment,
degenerative necrosis occurs to proteins of organelles in tumour
cells within a short period of time, even with no structural or
morphological changes of the tumour cells (9). Compared with partial nephrectomy, RFA
results in less hemorrhage during operation, reduced postoperative
convalescence, and expedited recovery time. Furthermore, RFA does
not require blockage of blood flow to the kidneys and there is no
warm ischemia period, thereby having less influence on renal
function and reduced risks of kidney loss (10,11). RFA
of renal cell carcinoma was first performed laparoscopically and,
with this as a basis, percutaneous RFA under ultrasound guidance is
now used in the Yidu Central Hospital of Weifang and its
application has achieved good clinical results. The result of the
present study have shown that, in patients treated by RFA,
operation time, blood loss during operation, length of stay and
incidence rate of complications are lower than patients treated by
established methods. For both groups of patients, serum CRP, IL-6
and T lymphocyte counts on 1, 2 and 3 days after operation were all
increaed over time. Furthermore, counts from the control group all
showed a greater increase for all the time points. For total
effective rates after operation, tumour-free survival times and
survival rates, differences between the two groups were of no
statistical significance.
Clinical indication for treatment with RFA is
diagnosis of a renal tumour with a diameter <4 cm (12). In this study, early stage renal cell
carcinoma patients with dorsolateral ultrasound of middle and lower
kidney showing a tumour with a diameter <4 cm were selected as
study objects. Research has shown that there are different effects
of RFA under different temperatures (13). The central part of the tumour is
always the focus of RFA and the temperature must be controlled to
>60°C to enable accurate ablation and to realize tumour
necrosis, and also to ensure that the physiological changes of the
malignant tissue are irreversible. Whereas, changes of neighboring
tissues are reversible when the temperature of healthy tissue is
controlled to <60°C. No adverse effects have been observed from
RFA, as the effects on healthy, neighboring tissue are too weak to
cause concern.
Currently, the intended target patient population
for RFA treatment is relatively small (14), which limits the ability to accurately
test for clinical effects of RFA. Limitations of this study are the
relatively small sample size of and the brief duration of follow-up
time. Therefore, further research should be conducted on the safety
and effectiveness of RFA to provide further clinical evidence.
Pathological reactions caused by a stress response
to surgical operations, such as immunosuppression and metabolic
disturbances, are related to tumour necrosis, nutritional status
and prognosis to some degree (15,16). It
has been widely shown that changes in serum CRP, IL-6 and T
lymphocyte counts in peripheral blood are indices of immune
response after tumour operation (17,18). The
results of this study have indicated that the above indices for the
two groups of patients have increased following the operation,
suggesting a stress response to the operative wound and tumour
necrosis. However, the serum levels of the indices at time points
following the operation in the control group were higher than those
in the observation group, indicating that RFA has specific effects
in alleviating postoperative inflammation and immune reaction.
Further research is required regarding the relationship between
treatment effects, tumour-free survival time and survival rate.
In conclusion, percutaneous RFA has advantages in
treating early stage renal cell carcinoma, such as a reduced
operative wound size, faster recovery times, and a reduced
inflammatory response. Furthermore, RFA achieves the same clinical
outcomes as the retroperitoneoscopic radical operation of renal
cell carcinoma. Therefore, results of this study support RFA being
recommended in clinical applications against early stage renal cell
carcinoma.
References
|
1
|
Yung KW, Yung TT, Chung CY, Tong GT, Liu
Y, Henderson J, Welbeck D and Oseni S: Principles of cancer
staging. Asian Pac J Surg Oncol. 1:1–16. 2015.
|
|
2
|
Nozaki T, Iida H, Morii A, Fujiuchi Y,
Komiya A and Fuse H: Use of the laparoscope holder for liver
retraction during urological laparoscopic surgery. Curr Urol.
6:99–101. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kamai T, Furuya N, Kambara T, Abe H, Honda
M, Shioyama Y, Kaji Y and Yoshida K: Single minimum incision
endoscopic radical nephrectomy for renal tumors with preoperative
virtual navigation using 3D-CT volume-rendering. BMC Urol.
10:72010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jun HY, Ryu JH, Byun SJ, Jeong CW, Kim TH,
Lee YH and Yoon KH: Combined radiofrequency ablation and double
anti-angiogenic protein therapy to increase coagulation efficacy:
An experimental study in a murine renal carcinoma model. Korean J
Radiol. 16:776–782. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Modabber M, Martin J and Athreya S:
Thermal versus impedance-based ablation of renal cell carcinoma: A
meta-analysis. Cardiovasc Intervent Radiol. 37:176–185. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kroeze SG, van Melick HH, Nijkamp MW,
Kruse FK, Kruijssen LW, van Diest PJ, Bosch JL and Jans JJ:
Incomplete thermal ablation stimulates proliferation of residual
renal carcinoma cells in a translational murine model. BJU Int.
110:(6 Pt B). E281–E286. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chan AA, Ahrar K and Matin SF: Ablative
therapies in renal cell carcinoma. Minerva Urol Nefrol. 63:237–250.
2011.PubMed/NCBI
|
|
8
|
Kong WT, Zhang WW, Guo HQ, Qiu JL, Tang M,
Jiang ZM, Shen Y, Li XG and Zhang SW: Application of
contrast-enhanced ultrasonography after radiofrequency ablation for
renal cell carcinoma: Is it sufficient for assessment of
therapeutic response? Abdom Imaging. 36:342–347. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Prokhorov DG, Shkol'nik MI, Shumskiĭ IA
and Belov AD: Application of radiofrequency ablation for treatment
of localized renal carcinoma. Vopr Onkol. 54:507–511. 2008.(In
Russian). PubMed/NCBI
|
|
10
|
Cahill T, Chen XL, Lee JW, Weiss M, Chang
VT and Cella D: Principles of radiofrequency ablation for cancer.
Asian Pac J Surg Oncol. 1:47–58. 2015.
|
|
11
|
Ramirez D, Akca O, Delluc A, Reaume N,
Haddock P and Chen XL: Staging of renal cell carcinoma. Asian Pac J
Surg Oncol. 2:281–290. 2016.
|
|
12
|
Powles T, Zhao S, Gorbonos A and Kapoor A:
Treatment strategies for renal cell carcinoma. Asian Pac J Surg
Oncol. 2:301–316. 2016.
|
|
13
|
Chang X, Liu T, Lin Y, Yu J and Liang P:
Radiofrequency ablation for renal cell carcinoma. Asian Pac J Surg
Oncol. 2:351–360. 2016.
|
|
14
|
Wendler JJ, Friebe B, Baumunk D, Blana A,
Franiel T, Ganzer R, Hadaschik B, Henkel T, Köhrmann KU, Köllermann
J, et al: Focal therapy for small renal masses: Observation,
ablation or surgery. Urologe A. 55:594–606. 2016.(In Russian).
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Reichle A, Grassinger J, Bross K, Wilke J,
Suedhoff T, Walter B, Wieland WF, Berand A and Andreesen R:
C-reactive Protein in patients with metastatic clear cell renal
carcinoma: An important biomarker for tumor-associated
inflammation. Biomark Insights. 1:87–98. 2007.PubMed/NCBI
|
|
16
|
Yang L, Wu X, Wang D, Luo C and Chen L:
Renal carcinoma cell-derived exosomes induce human immortalized
line of Jurkat T lymphocyte apoptosis in vitro. Urol Int.
91:363–369. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Figel AM, Brech D, Prinz PU, Lettenmeyer
UK, Eckl J, Turqueti-Neves A, Mysliwietz J, Anz D, Rieth N,
Muenchmeier N, et al: Human renal cell carcinoma induces a
dendritic cell subset that uses T-cell crosstalk for
tumor-permissive milieu alterations. Am J Pathol. 179:436–451.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Granov AM, Molchanov OE, Karelin MI,
Shkol'nik MI and Krotova OA: Influence of immunological parameters
on the effectiveness of systemic and loco-regional immunotherapy in
disseminated renal carcinoma. Vopr Onkol. 55:580–585. 2009.(In
Russian). PubMed/NCBI
|