Introduction
Malignant odontogenic tumors with the histological
features of ameloblastoma represent 1.6–2.2% of all odontogenic
tumors (1), and may be classified as
metastasizing ameloblastoma or ameloblastic carcinoma (AC); it is
generally agreed that the term ‘malignant ameloblastoma’ refers to
tumors exhibiting features of a benign ameloblastoma, while the
term ‘ameloblastic carcinoma’ indicates tumors that are still
recognizable as ameloblastoma but possess histological features of
malignancy. AC, which seems to be more frequent than malignant
ameloblastoma (2), is considered to
be a rare tumor, as few cases have been published. Although rare,
AC must be considered in the differential diagnosis of oral cavity
tumors. In 2004 Adebiyi et al (2) conducted a clinicopathological analysis
of 197 ectodermal odontogenic tumors and observed that AC was the
most frequent odontogenic malignant tumor (5.6%), followed by
primary intraosseous carcinoma (1.5%). AC exhibits a male
predominance, may arise de novo or from a pre-existing
odontogenic lesion (3), and affects a
wide range of ages. Two-thirds of these tumors arise from the
mandible, while one-third originate in the maxilla, and the
posterior portion of the jaws is more commonly involved (4).
Since few cases have been reported in the
literature, the incidence of the tumor, as well as the criteria for
classification, are not precisely define. Furthermore, treatment
modalities are still debated and there is lack of information
regarding certain characteristics of the disease (5). In the present study, a clinical case of
maxillary AC is presented and an up to date review of the published
cases is done.
Case report
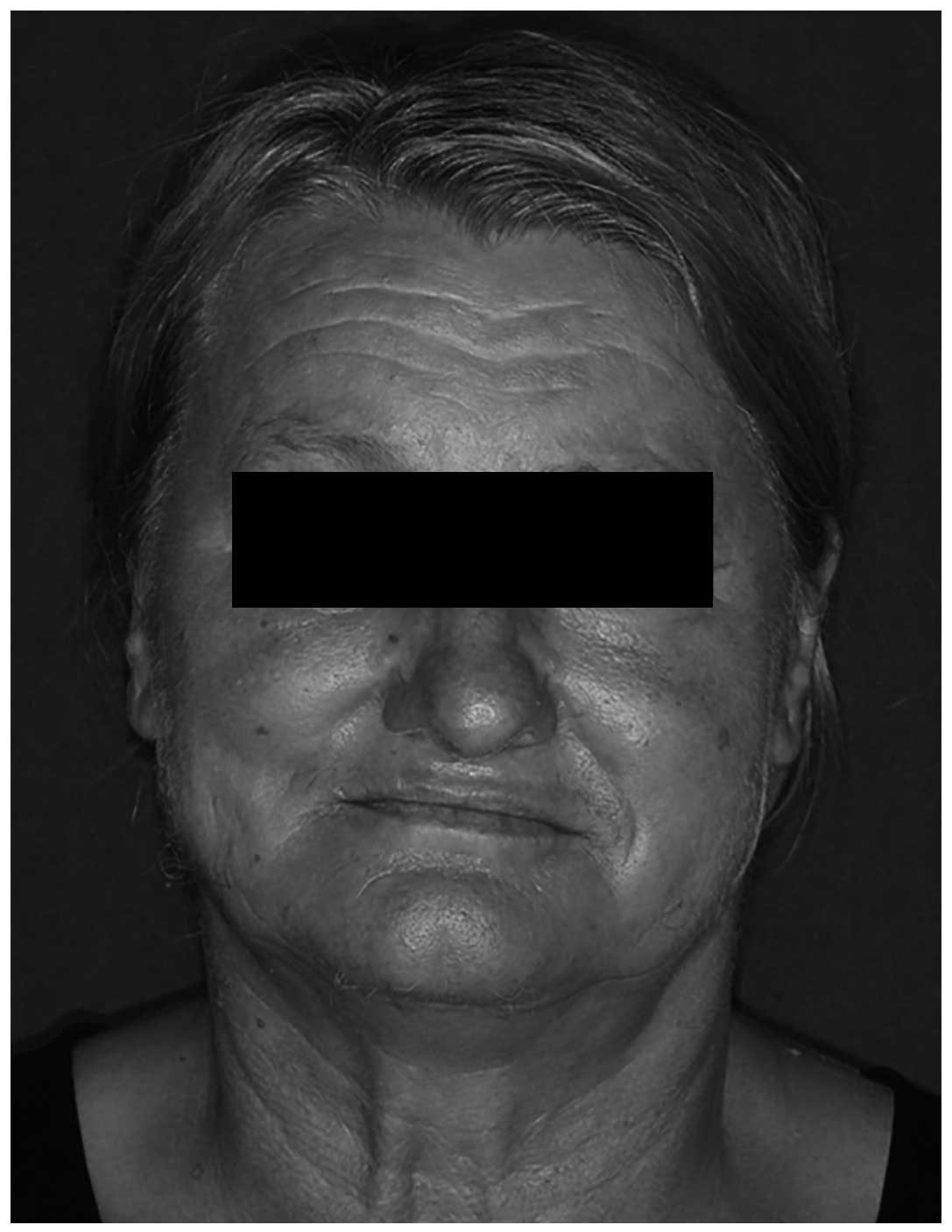
In August 2013, a 63-year-old female subject was
referred to the Maxillofacial Surgery Unit of Foligno Hospital
(Foligno, Italy) by her dentist, with a complaint of epistaxis and
painful swelling in the left upper jaw (Fig. 1). The initial symptom was epistaxis,
noted for the first time in February 2013; this was followed, in
April 2013, by an ulcerated, rapidly growing and painful swelling
localized in the upper maxillary fornix (Fig. 2). The patient was a non-smoker,
reported no alcohol consumption, and had no contributing medical
history. Extra-oral examination revealed facial asymmetry with
swelling of the left cheek; no neurological abnormalities were
noticed. Intra-oral examination revealed an ulcerated, swollen area
in the posterior left upper jaw, involving the soft palate, the
hard palate and the alveolar mucosa. Speech and feeding impairment
were reported by the patient.
An incisional biopsy was performed under local
anesthesia, and histological examination of paraffin-embedded
tissue sections with 10% neutral embedded-buffered formalin
established a provisional diagnosis of acanthomatous ameloblastoma.
Immunostaining was performed with antibodies against cytokeratin 5
[monoclonal antibody specific for human cytokeratin 5 intermediate
filament protein, used at pH 9.0 with Epitope Retrieval Solution 2
(Leica Biosystems Nussloch GmbH, Nußloch, Germany) as antigen
unmasker; Bond™ Ready-to-Use Primary Antibody Cytokeratin 5; clone
XM26; catalog no. PA0468; Leica Biosystems Nussloch GmbH),
cytokeratin 7 (mouse monoclonal antibody specific for human
cytokeratin 7 intermediate filament, used at a dilution 1:50 at pH
6.0 with Epitope Retrieval Solution 2 as antigen unmasker;
Novocastra™ Liquid Mouse Monoclonal Antibody Cytokeratin 7; clone
OV-TL 12/30; catalog no. NCL-L-CK7-OVTL; Leica Biosystems Nussloch
GmbH), p63 (monoclonal antibody used at pH 9.0 specific for human
p63 protein, used with Epitope Retrieval Solution 2 as antigen
unmasker; Bond™ Ready-to-Use Primary Antibody p63; clone: 7JUL;
catalog no. PA0103; Leica Biosystems Nussloch GmbH), thyroid
transcription factor-1 [TTF-1; mouse monoclonal antibody specific
for human TTF-1, used at a dilution 1:200 at pH 6.0 with Epitope
Retrieval Solution 1 (Leica Biosystems Nussloch GmbH) as antigen
unmasker; Novocastra™ Liquid Mouse Monoclonal, Antibody Thyroid
Transcription Factor-1; clone SPT24; catalog no. NCL-L-TTF-1; Leica
Biosystems Nussloch GmbH], cytokeratin 20 (mouse monoclonal
antibody specific for human cytokeratin 20 intermediate filament
protein, used at a dilution 1:50 at pH 6.0 with Epitope Retrieval
Solution 1 as antigen unmasker; Novocastra™ Liquid Mouse Monoclonal
Antibody Cytokeratin 20; clone Ks20.8; catalog no. NCL-L-CK20;
Leica Biosystems Nussloch GmbH), pan-cytokeratin (mouse monoclonal
antibody specific for human cytokeratins 5,6,8 and 18 intermediate
filament proteins, used at a dilution 1:80 with Enzyme 1 as antigen
unmasker; Novocastra™ Lyophilized Mouse Monoclonal Antibody
Cytokeratin (5/6/8/18); clones 5D3 and LP34; catalog no.
NCL-CK5/6/8/18; Leica Biosystems Nussloch GmbH) and Ki-67 [mouse
monoclonal antibody specific for human Ki-67 nuclear antigen (which
is expressed in all proliferating cells during the G1, S, M and G2
phases of the cell cycle), used a dilution 1:100 at citrate pH 6.0
as unmasking agent; Novocastra™ Liquid Mouse Monoclonal Antibody;
clone MM1; catalog no. NCL-L-Ki67-MM-1;Leica Biosystems Nussloch
GmbH].
A proliferation composed of solid epithelial cell
nests with peripheral palisading was present. Neoplastic cells were
focally atypical and scanty mitotic figures were evident. The Ki-67
proliferation index was 25%. The presence of a high mitotic index
and of focal nuclear atypia rendered necessary the study of further
material to more accurately define the exact nature of the lesion.
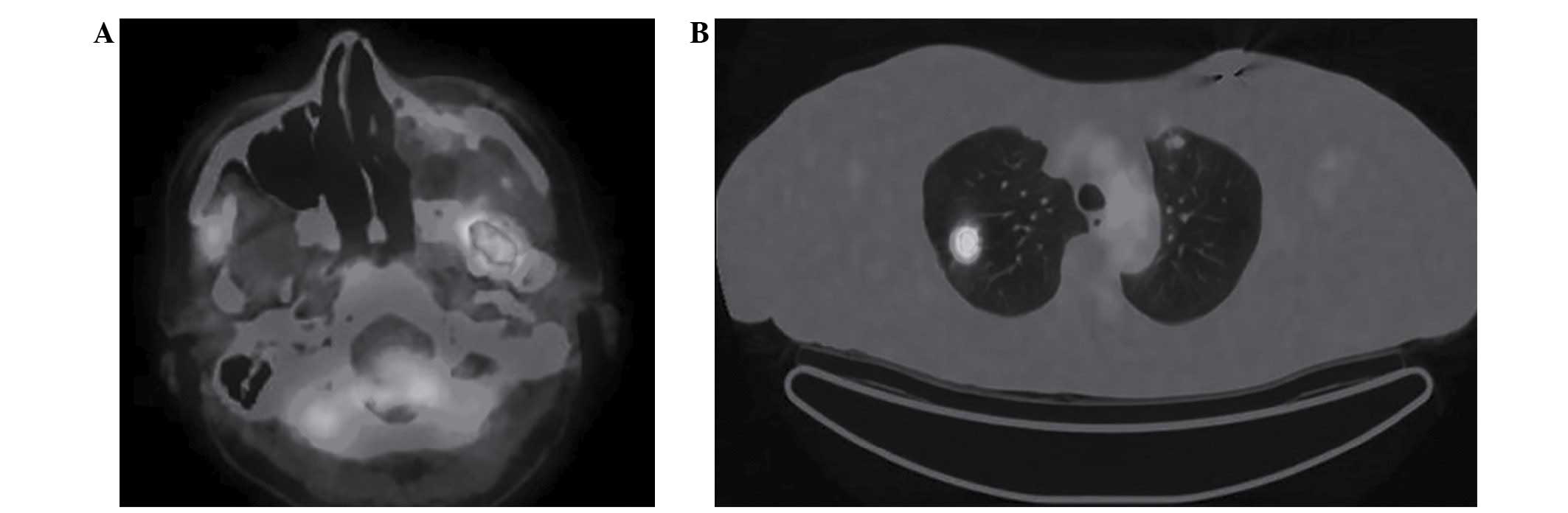
Computed tomography (CT) revealed an expansive lesion with erosion
of the left maxillary sinus, with extension to the infratemporal
fossa, nasopharynx, left nasal fossa, Eustachian tube and pterygoid
muscles. The lesion was ~58×40 mm, provoking left maxillary sinus
expansion, and erosion of its medial and posterior wall, orbital
floor and left pterygoid process (Fig.
3). Total body CT (TBCT) imaging revealed pathological
bilateral cervical lymph nodes. Two parenchymal lesions were
detected: One in the upper lobe of the left lung (6 mm), and one in
the upper lobe of the right lung (10 mm). According to the
histological results, the patient was diagnosed with an
acanthomatous ameloblastoma of the left maxilla. Due to the benign
character of the lesion, the pathological cervical lymph nodes and
the parenchymal lung lesions revealed on the TBCT could not be
considered as secondary tumors.
The patient underwent a left posterior maxillectomy
under general anaesthesia; the maxillectomy was extended to the
infratemporal and pterygopalatine fossa. An immediate
reconstruction was performed using a temporalis muscle flap. The
histopathological diagnosis of the surgical specimen was AC; a
proliferation made by an island of malignant epithelial cells
embedded in a fibrous stroma was evident. The mass was partly solid
and partly cystic. The basal cells of the islands appeared
columnar, hyperchromatic and were aligned in a palisaded fashion;
focally cell nuclei were displaced away from the basement membrane
and their cytoplasm was vacuolated.
On immunohistochemistry, neoplastic cells were
positive for cytokeratin 7 and negative for cytokeratin 20, and the
Ki-67 proliferation index was 30%. Following the surgical
treatment, the patient was treated with 3 sessions of chemotherapy
with cisplatin, 5-fluorouracil (5-FU) and cetuximab [1st session,
100 mg cisplatin intravenous (IV) and 440 mg cetuximab IV; 2nd and
3rd sessions, 150 mg cisplatin IV, 6,000 mg 5-FU IV and 700 mg
cetuximab IV], followed by 35 sessions of radiotherapy (70 Gy,
fractioned) to the primary site of the tumor and the neck. Head and
neck CT was performed to evaluate the presence of local recurrence
and the evolution of regional lymph nodes following therapies. CT
revealed small necrotic areas on the medial and posterior side of
the reconstructive flap, extending to the tonsillar region,
parapharyngeal space and masticatory space; a necrotic lymph node
was present in the right side (IIA area), measuring 16 mm in
diameter.
F-fluorodeoxyglucose-positron emission tomography
(FDG-PET)/CT was performed to confirm the presence and the
extension of the recurrence and of regional lymph node and distant
metastasis (Fig. 4). The FDG uptake
confirmed the presence of local recurrence; the maximum
standardized uptake value (SUVmax) was 10.4 on the left pterygoid
muscle, 4.3 on the right superior deep jugular lymph node (16 mm),
8.6 on the right lung lesion and 3.8 on the left lung lesion. No
uptake was documented on the left side of the neck. A core biopsy
of the right, necrotic, jugular node was performed, confirming the
presence of neck metastases of AC, which were positive for Bcl-2,
cytokeratin 7, cytokeratin 5 and p63, and negative for
carcinoembryonic antigen. A right neck dissection and removal of
the two lung nodes was performed, with histopathological findings
indicating positive reactivity to cytokeratin 7, cytokeratin 5 and
p63, and a diagnosis of AC metastases. The patient is currently
undergoing radiotherapy following the removal of lung metastases.
The patient signed an informed consent for publication of her
pictures for scientific purposes.
Discussion
A literature review was conducted by searching the
Pubmed (http://www.ncbi.nlm.nih.gov/pubmed), Scopus
(https://www.scopus.com/) and Scholar (https://scholar.google.it/) databases using the
keyword ‘ameloblastic carcinoma’. Articles from 2014 to 2016 were
selected among those published in English.
The statistics reported by Uzawa et al
(6), which can be considered our
starting point, have been updated, considering a total of 57 cases
of maxillary AC (56 cases in literature plus the present case). A
total of 14 cases not mentioned in previous reviews were
identified: 13 from the literature review and 1 treated in our
department (7–18). There were 2 cases reported in Uzawa's
study [Krempien (1979), and Kruse and Zwahlen (2003)] (6) that were excluded as they were malignant
ameloblastoma, which is not considered in the current review.
Of the reviewed patients, 44 were males and 13 were
females, corresponding to a male:female ratio of 3.38:1. The mean
age was 52.47, with a maximum of 90 and a minimum of 7 years. The
most common symptoms leading to presentation were swelling
(66.66%), pain (25.49%), ulcer (21.56%) and bleeding (9.8%).
A posterior location was reported in 61.40% (27
cases) of the cases, anterior location in 8.77% (4 cases), anterior
and posterior location in 17.54% (8 cases), and the maxillary sinus
was involved in 47.36% (21 cases) of the cases. In 7 patients, it
was not determinable whether the tumor was primary or secondary; in
the remaining 50 patients, 17 were secondary (34.0%) and 33 were
primary (66.0%).
With regard to the primary treatment, surgical
treatment was the modality of choice, and this was performed in 54
patients; in 35 patients, this was the only treatment modality,
while in 21 patients it was followed by radiotherapy, and in 3
cases a neck dissection was also performed.
Of the 57 total cases, 15 cases of recurrence were
recorded (26.3%): 11 recurrences (73.3%) occurred in males, and 4
in females (26,6%), with a male:female ratio of 2.75:1, an age
range of 7–77 years and a mean age of 51.1 years. Of the
recurrences, 12 occurred in cases with posteriorly located tumors
(80%), while 1 occurred in anterior, and 1 in anterior and
posterior tumors; in 1 case, location was not mentioned. The
predominance of posteriorly located tumors among recurrences was
likely due to the high prevalence of posterior (61.40%) or
anteroposterior tumors (17.54%) among all of the 57 included
patients, compared to the lower prevalence of anterior maxillary AC
(8.77%). Recurrences occurred predominantly in patients affected by
‘secondary AC’, and in 6 cases (40%) multiple recurrences were
observed (5 in secondary AC, 1 in primary AC). Of the cases of
multiple recurrences, 83.33% occurred in patients with secondary
AC. Additionally, 9 single recurrences were observed among the
patients (5 in secondary, 3 in primary, and 1 in an unknown type of
AC) (Table I).
 | Table I.Table of the series considered in this
study. |
Table I.
Table of the series considered in this
study.
| Case | First author, year
(ref.) | Gender | Age | Symptoms | Location | Tumor type | Primary
treatment | Time between
treatment and recurrence, months | Treatment for
recurrence | Time to metastasis,
months | Site of
metastasis | Follow-up,
months | Outcome |
|---|
| 1 | Grimes and
Stephens, 1948 (6) | F | 56 | Unknown | P | Sec. | S/R | – | – | 120 | Lung | 120 | NM |
| 2 | Eda et al,
1972 (6) | F | 44 | Painless | P | Sec. | Sa | 1st, 43 | Sa | 120 | Lymph nodes lung,
vertebra | 121 | Dc |
|
|
|
|
|
|
|
|
| 2nd, 32 | Sa |
|
|
|
|
|
|
|
|
|
|
|
|
| 3rd, 8 | Sa |
|
|
|
|
|
|
|
|
|
|
| 4th, 8 | Sa |
|
|
|
|
|
|
|
|
|
|
|
| 5th, 5 | R |
|
|
|
|
| 3 | Daramola et
al, 1980 (6) | M | 22 | Swelling | P | Sec. | Sa | 1st, 24 | Sa | 60 | Lung | NM | NM |
|
|
|
|
|
|
|
|
| 2nd, 36 | C/R |
|
|
|
|
| 4 | Madiedo et
al, 1981 (6) | M | 49 | Swelling | P | Sec. | Sa | 1st, 18 | S+ND/R | 36 | Lung | 60 | Dc |
|
|
|
|
|
|
|
|
| 2nd, 42 | C |
| 5 | Andersen and Bang,
1986 (26) | M | 77 | Bleeding | MS | Sec. | Sa | 1st, 36 | Sa | – | – | NM | NM |
| 6 | Nadimin et
al, 1986 (6) | F | 15 | Swelling | A/P | Prim. | Sa | – | – | – | – | NM | NM |
| 7 | Corio et al,
1987 (26) | M | 15 | Swelling | NM | U | Sa | – | – | – | – | NM | NM |
| 8 | Inoue et al,
1988 (6) | F | 51 | Swelling | P | Sec. | Sa | 1st, 137 | Sa | 145 | Lung | 186 | Dc |
| 9 | MacClatchey et
al, 1989 (6) | F | 77 | Concavity,
granulation | P | Prim. | Sa | – | – | – | – | 24 | Ao |
| 10 | Lee et al,
1990 (6) | M | 56 | Pain | P | Prim. | S/R | 1st, 3 | Untreated | 6 | Mandible | 7 | NM |
| 11 | Lolachi et
al, 1995 (4) | F | 82 | Trismus,
bleeding | MS | Prim. | Sa | – | – | – | – | NM | NM |
| 12 | Ingram et
al, 1996 (6) | M | 83 | Pain, erosion | P | Prim. | S/R | – | – | – | – | 24 | Ao |
| 13 | Infante-Cossio
et al, 1998 (6) | F | 69 | Painless, swelling,
anesthesia | A/P/MS | Prim. | S/R | – | – | – | – | 60 | Ao |
| 14 | Infante-Cossio
et al, 1998 (6) | M | 77 | Swelling, pain,
anesthesia | A/P/MS | Prim. | S/R | – | Untreated | – | – | 9 | Dc |
| 15 | Infante-Cossio
et al, 1998 (6) | M | 64 | Swelling,
fistula | P/MS | Prim. | S/R | – | – |
| – | 36 | Ao |
| 16 | Sastre et
al, 2002 (6) | M | 40 | Pain, Swelling | A | Prim. | S/S | – | – | – | – | 24 | Ao |
| 17 | Dhir et al,
2003 (24) | M | 72 | Unknown | P/MS | Prim. | S/R | – | – | – | – | 20 | Ao |
| 18 | Avon et al,
2003 (6) | M | 68 | Fistula | P/MS | Prim. | S/S | – | – | – | – | 24 | Ao |
| 19 | Oginni et
al, 2003 (6) | F | 61 | Bleeding | P | Prim. | Sa | 1st, 15 | Untreated | – | – | 15 | Ac |
| 20 | Goldenberg et
al, 2004 (6) | M | 72 | Unknown | NM | U | S/R | – | – | – | – | 36 | Ao |
| 21 | Philip et
al, 2005 (33) | M | 70 | Unknown | NM | Prim. | S/R | – | – | – | – | 40 | Ao |
| 22 | Philip et
al, 2005 (33) | M | 56 | Unknown | NM | Prim. | S/R | – | – | – | – | 8 | Ao |
| 23 | Hall et al,
2007 (6) | M | 15 | Swelling | A | Sec. | Sa | 1st, 10 | Sa | – | – | 196 | Ao |
|
|
|
|
|
|
|
|
| 2nd, 28 | Sa |
|
|
|
|
|
|
|
|
|
|
|
|
| 3rd, 2 | Sa |
|
|
|
|
| 24 | Hall et al
2007 (6) | M | 16 | Swelling | P/MS | Sec. | Sa | – | – | – | – | 288 | Ao |
| 25 | Hall et al
2007 (6) | M | 75 | Numbness, loose
tooth, nasal obstruction | P/MS | Sec. | Sa | 1st, 27 | Sa | – | – | 153 | Do |
| 26 | Hall et al
2007 (6) | F | 7 | Swelling | P | Sec. | Sa | 1st, 35 | Sa | – | – | 119 | Ao |
|
|
| 27 | Hall et al
2007 (6) | M | 63 | Swelling,
ulcer | P/MS | Sec. | Sa | 1st, 151 | Sa | – | – | 228 | Dc |
|
|
|
|
|
|
|
|
| 2nd, 13 | Sa |
|
|
|
|
|
|
|
|
|
|
|
|
| 3rd, 50 | Sa |
|
|
|
|
|
|
|
|
|
|
|
|
| 4th, 14 | Biopsy |
|
|
|
|
| 28 | Hall et al,
2007 (6) | M | 52 | Nasal congestion,
pain | P/MS | Sec. | Sa | 1st, 47 | C | 47 | Lung, liver | 51 | Ac |
| 29 | Ward et al,
2007 (6) | M | 64 | Swelling,
erythema | A | Prim. | Sa | – | – | – | – | 42 | Ao |
| 30 | Benlyazid et
al, 2007 (6) | M | 90 | Exophytic
ulcer | P | Prim. | Sa | – | – | – | – | 25 | Do |
| 31 | Naik and Kale, 2007
(6) | M | 70 | Swelling | A/P/MS | Prim. | Sa | – | – | – | – | 12 | Ao |
| 32 | Wu et al,
2007 (27) | M | 25 | Bleeding,
epistaxis, swelling, fistula | P/MS | Sec. | S/R | – | – | – | – | 30 | Ao |
| 33 | Koul et al,
2007 (7) | M | 73 | Exophytic
lesion | P/MS | Prim. | S+ND/R | – | – | – | – | 96 | Ao |
| 34 | Yazici et
al, 2008 (6) | M | 10 | Swelling | P/MS | Prim. | S/R | – | – | – | – | 6 | Ao |
| 35 | Angiero et
al, 2008 (28) | M | 68 | Bleeding | P/MS | Sec. | Sa | – | – | – | – | 6 | Ao |
| 36 | Yoon et al,
2009 (29) | M | 63 | Ulcer,
swelling | P | Prim. | S/R | 1st, unknown | Sa | – | – | 13 | Ao |
|
|
|
|
|
|
|
|
| 2nd, unknown | Sa |
|
|
|
|
| 37 | Yoon et al,
2009 (29) | F | 73 | Pain, swelling | P/MS | Prim. | Sa | – | – | – | – | 31 | Ao |
| 38 | Yoon et al,
2009 (29) | M | 61 | Pain, swelling,
trismus | P/MS | Prim. | Biopsy | – | – | – | – | NM | NM |
| 39 | Yoon et al,
2009 (29) | M | 58 | Pain, ulcer | P | Prim. | S+ND | – | – | – | – | 12 | Pain |
| 40 | Lucca et al,
2010 (6) | M | 73 | Swelling | A/P/MS | Prim. | Biopsy | – | – | – | – | 4 | Dc |
| 41 | Lucca et al,
2010 (6) | M | 69 | Ulcer | P | Prim. | Sa | – | – | – | – | 11 | Ao |
| 42 | Matsuzaki et
al, 2011 (36) | F | 73 | Swelling | P/MS | Prim. | Sa | – | – | – | – | 12 | Ao |
| 43 | Nicolotti et
al, 2011 (6) | M | 77 | Swelling,
ulcer | A/P | Prim. | Sb | – | – | 0 | Lung, liver,
cerebral | 5 | Dc |
| 44 | Ramesh et
al, 2011 (8) | M | 25 | Swelling,
ulcer | P | U | Sa | – | – | – | – | – | – |
| 45 | Karthikshree et
al, 2011 (9) | M | 55 | Rapid growth, pain,
ulcer | P | U | Sa | 1st, 2 | Sa | – | – | – | Ao |
| 46 | Perumal et
al, 2012 (10) | F | 74 | Swelling, nasal
obstruction | A/P/MS | U | S/R | – | – | – | – | – | Ao |
| 47 | França et
al, 2012 (6) | M | 59 | Swelling, pain | A/P/MS | U | S/R | – | – | – | – | 24 | Ao |
| 48 | Kar et al,
2012 (11) | M | 21 | Pain, swelling,
epistaxis | A/P | Prim. | S/R | – | – | – | – | 15 | Ao |
| 49 | Bedi et al,
2012 (12) | M | 18 | Swelling,
ulcer | P/MS | Prim. | Biopsy surgery | – | – | – | – | – | NM |
| 50 | Uzawa et al,
2014 (6) | M | 22 | Swelling | P | Prim. | Sa | – | – | – | – | 13 | Ao |
| 51 | Chilamakuri, et
al 2014 (13) | M | 12 | Pain, swelling,
ulcer | P/MS | Prim. | S+ND | – | – | – | – | 6 | Ao |
| 52 | Li et al,
2014 (14) | M | 47 | Unknown | Unknown | Sec. | Sa | – | – | – | – | 108 | Ac |
| 53 | Sahoo et al,
2014 (15) | M | 26 | Swelling | P/MS | Prim. | S/R | – | – | – | – | 24 | Ao |
| 54 | Tempaku et
al, 2014 (16) | M | 58 | Headache | A/MS | Sec. | S/R | – | – | – | – | 32 | Ao |
|
| Takahashi et
al, 2015 (6) |
|
| Dizziness
involve-ment) | (cranial | – | – | – | – | – | – | – | – |
| 55 | Borojeni et
al, 2015 (17) | M | 46 | Rapid growth,
swelling | A/P/MS | U | S/R | – | – | – | – | 12 | Ao |
| 56 | Sozzi et al,
2015 (18) | M | 14 | Swelling, tooth
mobility | A/MS | Sec. | Sa | – | – | – | – | 24 | Ao |
| 57 | Present case | F | 63 | Swelling, pain
ulcer | P/MS | Prim. | S/R | – | S/R | Present at
diagnosis | Neck, lung | 24 | Ac |
In 1972, the World Health Organization (WHO)
published a classification which mentioned malignant ameloblastoma
(19). Subsequently, in 1982, Elzay
(20) suggested a ‘modification of
the WHO classification system to include ameloblastic carcinoma’
(Table II). In 1983, Shafer et
al used the term ‘ameloblastic carcinoma’ to describe an
ameloblastoma with features of malignancy in the primary or
recurrent tumor (21). Other
classifications have been proposed in order to distinguish AC from
malignant ameloblastoma, a neoplasm in which the primary
localization in the jaws shows features of a benign ameloblastoma,
and which is typically recognized as ‘malignant’ once the
metastases have been diagnosed. In 1984, Slootweg and Müller
(22) noted that the diagnosis of
malignant ameloblastoma was used in an indiscriminate way. For this
reason the authors advocated a modification of the WHO
classification in order to introduce a subgroup in which AC was
described as arising de novo, ex ameloblastoma, or ex
odontogenic cyst (Table III).
 | Table II.Elzay classification, 1982 (20). |
Table II.
Elzay classification, 1982 (20).
| Groups | Description |
|---|
| Arising from an
odontogenic cyst | – |
| Arising from an
ameloblastoma |
|
| 2a | Well differentiated
(malignant ameloblastoma) |
| 2b | Poorly
differentiated (ameloblastic carcinoma) |
| Arising de
novo |
|
| 3a |
Non-keratinizing |
| 3b | Keratinizing |
 | Table III.Slootweg and Müller classification,
1984 (22). |
Table III.
Slootweg and Müller classification,
1984 (22).
| Groups | Description |
|---|
| Primary
intraosseous carcinoma ex odontogenic cyst |
|
| 2a | Malignant
ameloblastoma |
| 2b | Ameloblastic
carcinoma, arising de novo, ex ameloblastoma or ex
odontogenic cyst |
| Primary
intraosseous carcinoma de novo |
|
| 3a |
Non-keratinizing |
| 3b | Keratinizing |
In the 2005 WHO classification (23), AC was defined as a rare odontogenic
malignancy that combines the histological features of ameloblastoma
with cytological atypia, even in the absence of metastases, and
this is divided into primary, secondary intraosseous and secondary
peripheral types (Table IV). The
primary type arises as primitive malignancy of the jaws, and the
secondary type is the malignant transformation of a pre-existing
intraosseous or peripheral ameloblastoma. In 2009, Kruse et
al (5) proposed a revision of the
classification of AC, based on a review of the literature and with
consideration of the origin and histopathological features of the
primary tumor and metastases (Table
V). Actually, the classifications of AC are still under
revision, giving attention to histological features and biological
behavior of the disease, which in the future may represent useful
criteria for classification.
 | Table IV.WHO classification, 2005 (23). |
Table IV.
WHO classification, 2005 (23).
| Type | Subgroups |
|---|
| Ameloblastic
carcinoma | Primary type |
|
| Secondary type
(dedifferentiated) intraosseous |
|
| Secondary type
(dedifferentiated), peripheral |
 | Table V.Kruse et al classification,
2009 (5). |
Table V.
Kruse et al classification,
2009 (5).
| Types of
metastases | Description |
|---|
| Malignant
ameloblastoma |
|
| a | Metastases with
features of an ameloblastoma (well-differentiated) |
| b | Metastases with
malignant features (poorly differentiated) |
| Ameloblastic
carcinoma arising from an ameloblastoma |
|
| a | Without metastases
(malignant ameloblastoma) |
| b | Metastases with
features of an ameloblastoma (well-differentiated) |
| c | Metastases with
malignant features (poorly differentiated) |
| Ameloblastic
carcinoma with unknown origin histology (de novo) |
|
|
|
| a | Without
metastases |
| b | Metastases with
features of an ameloblastoma (well-differentiated) |
| c | Metastases with
malignant features (poorly differentiated) |
It is well known that AC is a disease that
predominantly affects the adult population, with a predilection for
males, and which is more frequent at the mandibular level rather
than in the maxilla. Dhir et al (24) analyzed 17 cases of AC with a mean age
of 53.5 years and male:female ratio of 1.5:1. Akrish et al
(25) analyzed 37 cases of AC that
were reported between 1984 and 2007. In these patients, the
male:female ratio was 2:1, the mean age was 52 years (range, 15–84
years), and the maxillary:mandibular tumor ratio was 1:1.9
(25). Li et al described a
series of 12 patients treated at the West China Hospital of
Stomatology between 2000 and 2008. The male:female ratio was 5:1
and the mean age was 44 years (range, 30–75 years). Mandibular
localization was more frequent than maxillary tumors (ratio, 11:1),
and there were 8 primary and 4 secondary tumors (14). In a review of the literature, Kar
et al identified 92 cases reported between 1984 and 2012,
with an age at presentation ranging from 7 to 91 years, a
male:female ratio of 2.3:1, mandibular localization reported in 56
cases and maxillary localization in 35 cases (11). In a review on pediatric maxillary AC,
Chilamakuri et al found a total of 104 cases of AC of the
jaws reported between 1979 and August 2013; 18 cases were in
children and adolescents, including 10 tumors located in the
mandible and 8 in the maxilla. In the maxilla, these tumors
occurred predominantly in the posterior region, and the age range
of the patients was 5–18 years (13).
AC is considered a rare tumor, and maxillary AC is
even less frequent; thus, knowledge of the disease is incomplete
and general agreement regarding certain biological characteristics
and the treatment of the disease has not been reached. Due to the
lack of large clinical series and reports with long-term follow-up,
several authors have recently reviewed data within the literature
in order to collect information about the disease and verify the
treatment options. In 2009, Kruse et al (5)presented a review of the literature on AC
of the maxilla, including cases published between 1948 and 2008,
identifying 26 cases; the patients had an average age of 54.4
years, with a marked prevalence in the group aged between 41 and 80
years (69.2%), and a male:female ratio of 2.7:1. A similar review
of the English literature published between 1948 and 2012,
conducted by Uzawa et al (6),
revealed 45 cases of maxillary AC, with patients ranging in age
between 5 and 90 years (mean age, 55.2 years) and a male:female
ratio of 3:1 (6). Notably, following
the review by Kruse, Uzawa found 19 new cases of maxillary AC that
were published between 2008 and 2012, corresponding to an increase
of ~70% of reported cases over a period of 4 years. In the present
review, the total number of cases of maxillary AC was 57,
comprising patients with an average age of 52.4 years and a
male:female ratio of 3.38:1.
The common clinical manifestations of AC are a large
mass, which is often painless and rapidly growing, and which can be
associated with tooth mobility and bleeding if the oral mucosa is
ulcerated. In maxillary AC, the predominant complaint is swelling,
with gingival bleeding, trismus, dysphonia, paresthesia, epistaxis
and oroantral fistulae also reported (25,26,27).
According to the current review, the most prevalent complaints were
swelling (66.66%), pain (25.49%), and ulceration (21.56%). At
radiographic examination, a poorly defined radiolucency, often
multilocular and with focal radiopacities, may be observed
(19). Root resorption is also
frequently observed (28); in cases
of maxillary AC, this may be associated with sinus obliteration,
palatal and maxillary bone resorption and nasal airway obstruction.
A report by Angiero et al (28) highlighted that histological
characterization of AC is challenging, and there are several
differential diagnoses that must be excluded. The authors stated
that the histological features of AC are like those of an
ameloblastoma, showing foci with sheets, islands or trabeculae of
epithelium, absence or rare presence of stellate reticulum, and
round-to-spindle-shaped epithelial cells with little or no
differentiation toward the columnar cells of ameloblastoma.
Features that may be useful to differentiate AC from ameloblastoma
are hyperchromatism, large or atypical nuclei, increased mitotic
index, necrosis, calcification and, particularly, neural and
vascular invasion. The presence of calcifications, which is not
usual in ameloblastoma, and a proportion of clear cells >15%
suggest a diagnosis of AC. Angiero et al (28) also remarked that diagnosis can be
difficult due to the variability of histological features,
suggesting that aspects such as occasional mitoses, keratin
production, and the formation of hyaline material near the
epithelial portion of the tumor must be taken into consideration as
indicative of malignant lesion (28).
In order to assist in differentiating AC from
ameloblastoma, several immunohistochemical markers have been
tested. Yoon et al (29) found
that the expression of cytokeratin 18, parenchymal matrix
metalloproteinase (MMP)-2, stromal MMP-9 and Ki-67 differentiate AC
from ameloblastoma. Lei et al (30) recommend the inclusion of SOX2
immunohistochemical staining in conjunction with Ki-67 in
challenging cases with atypical features. Locally the tumor is
invasive, often showing a silent infiltrative growth (30).
In a review of 31 studies published between 2005 and
2011, Casaroto et al (31)
found a high incidence of primary AC in the maxilla, while
secondary AC was more frequent in the mandible. In the review,
secondary AC was associated with cases with recurrence or mortality
from the disease. The higher frequency of the primary type in the
maxilla and the more aggressive behavior of the secondary type are
confirmed by other studies (32,33). In
the present series of 57 maxillary AC, the tumor types of 7 cases
were not determined due to a lack of available information. In the
remaining 50 cases, there were 17 secondary (34%) and 33 primary
tumors (66%).
A general consensus on treatment modalities for AC
has still not been reached; however, surgical therapy is the most
widely used treatment option, while few data regarding chemotherapy
are available (34). The recurrence
rate following curettage of maxillary ameloblastoma is almost 100%
(25); Yoon et al (29) reported a recurrence rate of 92.3%
following curettage alone and 28.3% following partial resection,
and therefore a wide surgical resection, with clear margins free of
tumor, is recommended (5,28,34).
Taking into consideration the relatively lower malignancy of
primary AC, a more tissue sparing resection may be indicated for
primary tumors, while a wider resection is recommended in cases of
secondary AC (6,28). Radiotherapy is used in cases with
positive surgical margins, perineural infiltration or soft-tissue
invasion (33).
Stereotactic radiosurgery (SRS) in the treatment of
AC has been recently reported (34).
Takahashi et al (35)
presented a report of the efficacy of single-fraction helical
tomotherapy for the treatment of residual AC following surgical
resection, remarking that SRS may be an effective treatment, but
only for small volumes due to the high doses used in
radiosurgery.
AC is prone to metastasis, and the presence of
hematogenous spread (the most frequent mode of diffusion) or neck
node involvement must be verified. In the review by Uzawa et
al (6), regional metastases
occurred in 3 cases: 1 in the mandible and 2 in the lymph nodes of
the neck. The most common location of distant metastasis was the
lung, occurring in 9 cases. Distant metastases were also reported
in the liver in 2 cases, the bone in 2 cases, the brain in 1 case
and the myocardium in 1 case. In the review by Kruse et al
(5), pulmonary metastases were
identified in 34.6% of cases, and cervical lymph node metastasis
could be found in only 1 patient (5).
The present review of the existing literature found 2 cases of neck
node involvement and 9 of distant metastases, while the current
case treated at our hospital exhibited neck node involvement and
lung metastases at the time of diagnosis. Indications for neck
dissection remain unclear; however, the procedure is not
recommended if there is no evidence of lymph node involvement
(28,29).
Recurrence of AC is not infrequent and appears to be
associated with mortality. Yoon et al (29) reported a recurrence rate of 28.3% in
patients who underwent surgical resection, while Uzawa et al
(6) found a rate of recurrence of
38.4%, often involving multiple recurrences or associated with
metastases (6). The present review
identified 15 recurrences among 57 cases (26.6%); the majority of
recurrences were in cases of posterior tumor location (80%). This
is likely due to the higher prevalence of posterior (61.40%) or
anteroposterior (17.54%) tumors, compared to the low prevalence of
anterior maxillary AC (8.77%), in this review.
Infiltration of surgical margins, presence of
metastases and diagnostic delay are other factors associated with
poor prognosis (25). Uzawa et
al (6) recommended early,
aggressive and complete removal of the tumor as the best treatment
to improve the survival rate, and a more radical treatment modality
in cases with primary recurrence. For the same reason an early and
precise diagnosis is mandatory, and it has been suggested that
FDG-PET/CT should be routinely performed during the diagnostic
phase in order to reveal possible metastatic disease (6,36) or,
together with magnetic resonance imaging, to detect tumor margins
and plan surgical resection (36).
Postoperatively, 11C-methionine (MET)-PET can be useful
in order to detect residual disease or recurrence during follow-up
(27). Since lesional MET
accumulation has been observed to decrease concurrently with the
decreased tumor volume following treatment with single-fraction
radiotherapy, MET-PET may also be used in monitoring the response
of AC to radiotherapy (27).
As previously reported, the prognosis of AC is
heavily influenced by the persistence of the tumor, the presence of
metastases and recurrences. Primary AC shows a more favorable
prognosis than secondary AC, and young patients have a higher
survival rate compared with the older patients (27). In any case, lifetime follow-up is
recommended due to the possibility of late recurrence of the tumor
(5,6).
In summary, AC is considered a rare disease and the
present review of the literature demonstrates the lack of knowledge
regarding this tumor and the consequent ongoing debate regarding
certain aspects of this disease. In recent years, a substantial
number of new cases of AC have been published and the disease has
been investigated with greater attention. It is possible that these
new cases should be attributed to the higher level of awareness of
the disease and increased accuracy of diagnoses, rather than to a
true increase in the incidence of AC. If this is the case, this may
indicate that better knowledge of the disease accounts for an
increased diagnostic sensibility, and, thus, AC may not be as rare
as previously believed.
References
|
1
|
Rizzitelli A, Smoll NR, Chae MP, Rozen WM
and Hunter-Smith DJ: Incidence and overall survival of malignant
ameloblastoma. PLoS One. 10:e01177892015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Adebiyi KE, Odukoya O and Taiwo EO:
Ectodermal Odontogenic tumours: Analysis of 197 Nigerian cases. Int
J Oral Maxillofac Surg. 33:766–770. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cizmecý O, Aslan A, Onel D and Demiryont
M: Ameloblastic carcinoma ex ameloblastoma of the mandible: Case
report. Otolaryngol Head Neck Surg. 130:633–634. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lolachi CM, Madan SK and Jacobs JR:
Ameloblastic carcinoma of the maxilla. J Laryngol Otol.
109:1019–1022. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kruse AL, Zwahlen RA and Grätz KW: New
classification of maxillary ameloblastic carcinoma based on an
evidence-based literature review over the last 60 years. Head Neck
Oncol. 1:312009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Uzawa N, Suzuki M, Miura C, Tomomatsu N,
Izumo T and Harada K: Primary ameloblastic carcinoma of the
maxilla: A case report and literature review. Oncol Lett.
9:459–467. 2015.PubMed/NCBI
|
|
7
|
Koul R, Binahmed A, Dubey A, Nason R and
Cooke AL: Maxillary Ameloblastic Carcinoma. J HK Coll Radiol.
11:32–34. 2008.
|
|
8
|
Ramesh M, Sekar B, Murali S, Mathew S,
Chacko J and Paul G: Ameloblastic carcinoma - review and
histopathology of 5 cases. Oral Maxillofac Pathol J (OMPJ).
2:154–160. 2011.
|
|
9
|
Karthikshree V, Ramesh V Prashad,
Balamurali PD and Premalatha B: Ameloblastic Carcinoma - A case
report highlighting its variations in histology. J Int Oral Health.
3:37–42. 2011.
|
|
10
|
Perumal CJ: Ameloblastic carcinoma of the
maxilla with extension into the ethmoidal air cells and close
proximity to the anterior skull base: A rare case presentation.
Craniomaxillofac Trauma Reconstr. 5:169–174. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kar IB, Subramanyam RV, Mishra N and Singh
AK: Ameloblastic carcinoma: A clinicopathologic dilemma - Report of
two cases with total review of literature from 1984 to 2012. Ann
Maxillofac Surg. 4:70–77. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bedi RS, Chugh A and Pasricha N:
Ameloblastic carcinoma of maxilla. Natl J Maxillofac Surg. 3:70–74.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chilamakuri S, Murathati S, Nuvvula S,
Nirmala S, Devireddy SK and Kanubaddy SR: Pediatric maxillary
ameloblastic carcinoma. J Cranio Max Dis. 3:141–146. 2014.
View Article : Google Scholar
|
|
14
|
Li J, Du H, Li P, Zhang J, Tian W and Tang
W: Ameloblastic carcinoma: An analysis of 12 cases with a review of
the literature. Oncol Lett. 8:914–920. 2014.PubMed/NCBI
|
|
15
|
Sahoo TK, Samal S, Dhal I, Mishra C and
Kar A: Ameloblastic carcinoma of maxilla and its management: A case
report and review of literature. Int J Dent Med Res. 1:73–76.
2014.
|
|
16
|
Tempaku A, Takahashi Y, Ikeda H, Yamauchi
S, Gotoh T, Bandoh N, Makino S, Shimada T and Kamada H: Usefulness
of 11C-methionine positron emission tomography for detecting
intracranial ameloblastic carcinoma: A case report. Oncol Lett.
8:1509–1512. 2014.PubMed/NCBI
|
|
17
|
Borojeni MP and Etesami M: Ameloblastic
carcinoma of maxillary sinus. Int J Dent Med Res. 1:73–75.
2015.
|
|
18
|
Sozzi D, Morganti V, Valente GM, Moltrasio
F, Bozzetti A and Angiero F: Ameloblastic carcinoma in a young
patient. Oral Surg Oral Med Oral Pathol Oral Radiol. 117:e396–e402.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pindborg JJ, Kramer IRH and Torloni H:
Histological typing of odontogenic tumors, jaw cysts and allied
lesions. World Health Organisation; Geneva: pp. 35–36. 1972
|
|
20
|
Elzay RP: Primary intraosseous carcinoma
of the jaws. Review and update of odontogenic carcinomas. Oral Surg
Oral Med Oral Pathol. 54:299–303. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shafer WG, Hine MK and Levy BM: A Textbook
of Oral Pathology. 4th. WB Saunders; USA: pp. 251–258. 1983
|
|
22
|
Slootweg PJ and Müller H: Malignant
ameloblastoma or ameloblastic carcinoma. Oral Surg Oral Med Oral
Pathol. 57:168–176. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Barnes L, Eveson JW, Reichart P and
Sidransky D: World Health Organization Classification Of Tumours -
Pathology & Genetics: Head and Neck Tumours. IARC Press; Lyon,
France: 2005
|
|
24
|
Dhir K, Sciubba J and Tufano RP:
Ameloblastic carcinoma of the maxilla. Oral Oncol. 39:736–741.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Akrish S, Buchner A, Shoshani Y, Vered M
and Dayan D: Ameloblastic carcinoma: Report of a new case,
literature review, and comparison to ameloblastoma. J Oral
Maxillofac Surg. 65:777–783. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Corio RL, Goldblatt LI, Edwards PA and
Hartman KS: Ameloblastic carcinoma: a clinicopathologic study and
assessment of eight cases. Oral Surg Oral Med Oral Pathol.
64:570–576. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wu JY, Chi LH, Pemg BY and Lin YH:
Ameloblastic carcinoma of the maxilla - case report. J Dent Sci.
2:164–170. 2007.
|
|
28
|
Angiero F, Borloni R, Macchi M and Stefani
M: Ameloblastic carcinoma of the maxillary sinus. Anticancer Res.
28:3847–3854. 2008.PubMed/NCBI
|
|
29
|
Yoon HJ, Hong SP, Lee JI, Lee SS and Hong
SD: Ameloblastic carcinoma: An analysis of 6 cases with review of
the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
108:904–913. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lei Y, Jaradat JM, Owosho A, Adebiyi KE,
Lybrand KS, Neville BW, Müller S and Bilodeau EA: Evaluation of
SOX2 as a potential marker for ameloblastic carcinoma. Oral Surg
Oral Med Oral Pathol Oral Radiol. 117:608–616.e1. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Casaroto AR, Toledo GL, Filho JL, Soares
CT, Capelari MM and Lara VS: Ameloblastic carcinoma, primary type:
Case report, immunohistochemical analysis and literature review.
Anticancer Res. 32:1515–1525. 2012.PubMed/NCBI
|
|
32
|
Henderson JM, Sonnet JR, Schlesinger C and
Ord RA: Pulmonary metastasis of ameloblastoma: Case report and
review of the literature. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod. 88:170–176. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Philip M, Morris CG, Werning JW and
Mendenhall WM: Radiotherapy in the Treatment of Ameloblastoma and
Ameloblastic Carcinoma. J HK Coll Radiol. 8:157–161. 2005.
|
|
34
|
Perera E, Lindquist C, Hughes C and Thomas
S: The use of gamma knife stereotactic radiosurgery in the
treatment of ameloblastic carcinoma. Int J Oral Maxillofac Surg.
42:934–938. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Takahashi Y, Bandoh N, Miyamoto A and
Kamada H: Single-fraction helical tomotherapy for ameloblastic
carcinoma. J Oral Maxillofac Surg. 74:302–306. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Matsuzaki H, Katase N, Hara M, Asaumi J,
Yanagi Y, Unetsubo T, Hisatomi M, Konouchi H and Nagatsuka H:
Ameloblastic carcinoma: A case report with radiological features of
computed tomography and magnetic resonance imaging and positron
emission tomography. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 112:e40–e47. 2011. View Article : Google Scholar : PubMed/NCBI
|