Introduction
In recent years, with the popularization of the
concept of minimally invasive surgery and the application of
video-assisted thoracoscopic surgery (VATS) technology, thoracic
surgery has become a major surgical method in chest surgery. VATS
incision has many options, and the most frequently used option is
one observation hole and 2–3 operation holes. In recent years, with
the development of VATS, a number of investigators have attempted
to further reduce the operating hole on the basis of traditional
thoracic surgery, only using a 4.0–5.0-cm incision as an operation
(1). More minimally invasive
operation, more appealing incision scar, more light postoperative
pain, more rapid postoperative patient recovery are the prominent
advantages (2). At present, this more
minimally invasive surgery has been widely used in the treatment of
primary spontaneous pneumothorax, lung cancer, mediastinal tumors
and other diseases (3).
We performed a retrospective analysis of the
efficacy of single-hole video-assisted thoracoscope in 32 pulmonary
peripheral tumor patients that were treated at The Central Hospital
of Xuzhou (Jiangsu, China) from March, 2011 to March, 2015. Summary
studies are provided below.
Materials and methods
General materials
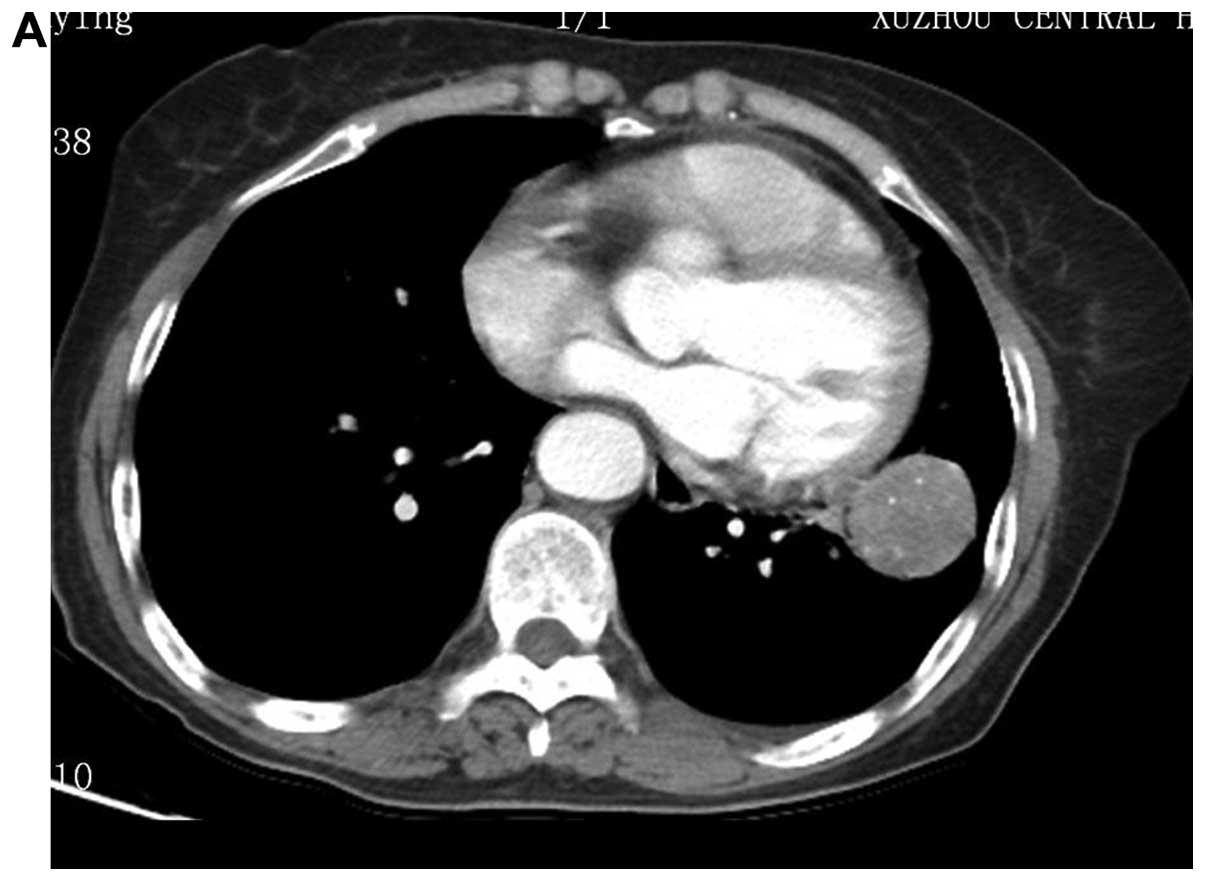
From March, 2011 to March, 2015, 32 patients, of
whom were 22 males and 10 females, age range, 34–81 years (average,
55 years) were enrolled in the present study. All the patients were
diagnosed with pulmonary peripheral tumor under CT examination.
Tumors in 8 patients was located in upper left pulmonary lobe, 9
cases in left lower pulmonary lobe, 5 cases in right upper
pulmonary lobe, and 2 cases in right middle pulmonary lobe, and 8
cases in right lower pulmonary lobe (Fig.
1). Eight patients were diagnosed with pulmonary malignant
tumor before operation, but could not tolerate lobectomy operation
due to pulmonary function impairment; 24 patients had no definite
pathological diagnosis before operation, and confirmed to be
pulmonary benign tumor after operation.
The present study was approved by the ethics
committee of The Central Hospital of Xuzhou. Signed written
informed consent was obtained from all the participants before the
study
Anesthesia method and position
The patients underwent double-lumen tube intubation,
intravenous combined anesthesia, and one-lung ventilation on
healthy side during operation. Patients were required to lie on
their healthy side and their upper arms in abduction position and
fixed onto the hand bracket.
Operation method
Patients diagnosed with malignant lung tumor were
confirmed to be unsuitable for lobectomy operation; thus, pulmonary
wedge resection was carried out directly. Those patients without
pathological diagnosis before operation received pulmonary wedge
resection and samples were sent for further pathological
examination. When the pathological results confirmed the presence
of benign pulmonary tumors, we terminated the operation. If
pathological result confirmed the presence of malignant pulmonary
tumors, we continued the pulmonary lobectomy and systematic lymph
node dissection (patients were excluded from this study).
We used 30° 10 mm thoracoscope and light source.
During operation, the operator stood on the patient's abdomen side
and the thoracoscope carrier was placed on the patient's back side.
Initially, we made a 1.5-cm incision on the seventh or eighth rib
in midaxillary line as the observation hole, inserted the
thoracoscope puncture trocar, and imbedded the thoracoscope to
detect the whole chest cavity. We observed the tumor's location and
condition of pleural adhesion. Subsequently we made a 4.0–5.0-cm
incision in the lateral margin of pectoralis major in the fourth or
fifth rib in midaxillary line as the operation hole and inserted an
incision protective casing into the operation hole.
We palpated the tumor by thoracoscope surgical
instruments or fingers to further determine the location and the
size of tumor and used sponge forceps or endoscopic grasping
forceps to pull the pulmonary lobe and exposed the surgery field.
When the location of tumor was determined, we put in an endoscopic
linear stapling device to make ‘V’ type cutting alongside the tumor
tissues and removed the tumor and partial lung tissues. While
cutting, the tumors inside the lung were required to be completely
enveloped within the normal lung tissues. Removed tumors were
placed in extracting bags or gloves. After completing the
resection, chest cavity was washed and examined for bleeding or
leakage on the pulmonary cutting surface. When necessary, we used a
4–0 single absorbable suture material to suture the cutting
surface. Meanwhile, our anesthesiologist made endotracheal
sputum-suction to confirm whether there was any bloody discharge
inside the patient's airway. As soon as the absence of bleeding or
leakage was confirmed, the operation was terminated. Before closing
the chest, we moved the thoracoscope into operation hole and under
direct vision of thoracoscope we placed an intrathoracic drain into
the observation hole. We sutured the operation hold by needle free
suture unit or intradermal suture.
Results
All the patients completed the tumor resection
smoothly under single-hole VATS. None of our patients required a
second operation hole or needed a transfer to thoracotomy.
Operation time was 40–100 min, with an average of 65.78±15.87 min.
Intraoperative blood loss was 20–100 ml, with an average of
47.19±26.91 ml. Post-operative chest drainage time was 3–6 days,
with an average of 4.22±0.87 days. Hospitalization time after
operation was 5–7 days, with an average of 5.97±0.82 days. No
patient received a second surgery for pulmonary leak or bleeding
and none had any complications. All the patients recovered very
well.
Discussion
Compared with traditional thoracotomy, VATS has many
advantages, such as less trauma, less bleeding, and rapid recovery
(4–6).
After many years of clinical practice, many scholars have
summarized the safety and reliability of complete VATS (7–9).
Conventional VATS surgery usually requires 3 incisions, i.e., an
observation hole in the 6th-8th rib in the midaxillary line, a main
operator hole in the 3rd-5th rib in the anterior axillary line, and
a deputy operation hole in the 6th-8th rib between the posterior
axillary line and the scapular line. Occasionally, a third
operation hole is required (10,11). These
three holes are distributed in a triangular shape (10,11). Under
2–3 operation holes, the surgical device could enter into the chest
cavity through different holes, which is convenient for the
operation and also conductive to hemostasis, adhesion isolation and
other operations. However, if surgical procedures could be improved
and the number or size of operation holes could be reduced, it
would be favorable for the optimization of VATS, making it less
invasive, and thereby minimize the patient's trauma.
In 2004, Rocco et al reported the single-hole
VATS wedge resection and confirmed that its operation results and
post-operative complications were similar to three-hole surgery,
but it could reduce the postoperative pain, shorten the duration of
hospitalization, and reduce the overall cost (12). Based on these facts, our team improved
the traditional VATS surgical incision design. By one operation
hole in the anterior axillary line, we achieved favorable operation
results. In the pressent study, all patients had completed the
tumor-reductive surgery under single-hole thoracoscope
successfully. None of the patients required a second operation hole
or needed a transfer to thoracotomy and all patients had a good
recovery. Chest back muscles have multiple layers, blood supply and
a vast nerve distribution with narrow space between ribs. These
characteristics make the incision in posterior axillary line more
prone to bleeding and have more difficult homeostasis, which can
translate to more pain for patients. Consequently clinicians
abandoned the incision in posterior axillary line and simply made
the operation hole in the anterior line axillary. Single-hole
surgery could be completed by one surgeon and one thoracoscope
assistant. Additionally, if during operation, patient needed a
transfer to thoracotomy, single-hole surgery could also avoid
excessive deputy operation holes, thereby reducing the scars.
Nevertheless, single-hole surgery also has some drawbacks. Since
the operation holes were reduced, the surgical instruments must
enter and exit through the same hole. When several instruments are
in use at the same time, they would interfere with each other.
However, an experienced surgeon can manage this situation (13).
For some patients we used lung wedge resection,
these included: i) patients with benign pulmonary tumors; ii)
patients with malignant pulmonary tumors unsuitable for lobectomy;
iii) patients with indefinite diagnosis; iv) with suspicious
pulmonary metastatic nodules; and v) patients with the focus
located in the periphery of the lung.
From our experience, we concluded the following
notes for attention while performing single-hole VATS:
i) The hole should be closely stuck to the incision
in upper edge of the rib and must be vertical. If the hole was
tilted and formed a subcutaneous tunnel, the entry and exit for
surgical instruments would be affected and also the operational
angle for instruments would be limited (14).
ii) The single operation hole location should be
determined by the site of the tumor and the size of incision should
be suitable for tumor removal.
iii) Instruments with different length could be used
to cooperate with the surgery. Moreover, we should make the most of
the radian of instruments, and must avoid the instruments to
interfere with each other (15).
iv) If necessary, the ‘observation hole’ and
‘operation hole’ could change their roles. Inserting an endoscopic
linear stapling device through the observation hole could make the
lung tissue resection more convenient.
v) Accurate localization of lung cancer was the key
for a successful operation. For accurate localization we used the
following methods: a) before surgery we injected methylene blue or
edical glue into the focus through chest CT, or placing fine needle
or steel wire to determine the position; and b) during operation we
observed the pleural indentation in visceral layer of lung surface
or navel signs; we made palpation by surgical instruments or single
finger or double fingers; we performed B-ultrasonic localization
during operation.
vi) We made a second operation hole or combine with
small incision operation if during the operation one of the
following circumstances occurred: a) the chest had extensive dense
adhesion; b) the amount of bleeding was too large to be stopped;
and c) air leakage from the lung was too serious and became
inconvenient for suture. For the safety of patients, we should take
other proper measures, instead of sticking to single hole
surgery.
In conclusion, for patients with pulmonary
peripheral tumor, single-hole video-assisted thoracoscope could
further reduce their surgical trauma. The operation is safe,
feasible and worthy of wide application.
References
|
1
|
Woo YJ and Reitz BA: One hundred years of
history at Stanford University: thoracic and cardiovascular
surgery. Semin Thorac Cardiovasc Surg. 27:388–397. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
He CX: Professor Eugenio Pompeo: the
present and future of minimally invasive thoracic surgery. Ann
Transl Med. 3:3442015.PubMed/NCBI
|
|
3
|
Bertoglio P, Davini F, Melfi FM and Mussi
A: eComment. Marking techniques can increase the use of minimally
invasive surgery for small and deep nodules of the lung. Interact
Cardiovasc Thorac Surg. 22:2072016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yun L, Sui XZ, Jiang GC, Li JF, Liu J and
Wang J: Experience of completely video-assisted thoracoscopic
lobectomy in non-small cell lung cancer: series of consecutive 500
patients in single-center. Chin J Cardiov Surg. 28:3–6. 2012.
|
|
5
|
Nuo X and Zhuo L: The clinical application
of video-assisted thoracoscopic lobectomy. Chinese J Lung Dis.
4:57–59. 2011.
|
|
6
|
Zhenyu S, Yong Z, Minwei G, Xiaofeng C, Qi
S and Weimin Z: Clinical study on the treatment of non-small cell
lung cancer by 3 kinds of surgical procedures. J Nanjing Med Univ.
31:427–430. 2011.
|
|
7
|
Xiandong T, Tiewen P and Bin W: Advantages
of VATS in the treatment of non small cell lung cancer. Chin J Lung
Dis. 4:33–37. 2011.
|
|
8
|
Guanchao J, Fan Y and Jun W: Progress of
thoracoscopic lobectomy in the treatment of non-small cell lung
cancer. Chin J Cardiovasc Surg. 26:291–293. 2010.
|
|
9
|
Li JF, Yang F, Li Y, Wang J, Liu J, Jiang
GC, Zhao H, Liu YG, Zhou ZL and Bu L: Clinical analysis of 100
consecutive completely thoracoscopic lobectomy. Chin J Clin Thorac
Cardiovasc Sur. 16:1–5. 2009.
|
|
10
|
Jianxing H: Minimally invasive thoratic
surgical procedures and atlas. Guangdong Sci Technol Press.
1:195–229. 2005.
|
|
11
|
Jun W: Chest disease VATS holo-authentic
atlas. Jiangsu Sci and Technol Press. 69–116. 2007.
|
|
12
|
Rocco G, Martin-Ucar A and Passera E:
Uniportal VATS wedge pulmonary resections. Ann Thorac Surg.
77:726–728. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Xin W, Lei W, Huayong W and Hao Z:
Clinical analysis of single-hole VATS in the treatment of non-small
cell lung cancer. Chin J Laparosc Surg. 6:26–29. 2013.
|
|
14
|
Che GW, Mei LY, Mei JD and Liu LX: Single
utility port video-asslsted thoracoscopic surgery for 158 patients
with pulmonary diseases. Chin J Clin Thorac Cardiovasc Surg.
19:116–119. 2012.
|
|
15
|
Xin W and Lei W: Treatment of single-hole
VATS in primary spontaneous pneumothorax. Chin J Laparosc Surg.
5:45–47. 2012.
|