Introduction
Primary anterior mediastinal tumors account for 50%
of mediastinal tumors, including thymic hyperplasia, thymoma,
thymic cysts, mature type and immature type teratomas, germ cell
tumors and lymphoma, however, thymoma is the most common primary
tumor of the anterior mediastinum (1–4). At
present, morphological examinations including computed tomography
(CT) and magnetic resonance imaging (MRI) are advantageous in that
they are able to identify the anatomical locations of tumors and
their relationships with adjacent tissues and organs. Although CT
is able to make relatively specific diagnoses for certain
mediastinal masses by identifying the fat, calcified or cystic
components, it is often difficult to distinguish benign and
malignant thymoma, and although benign and malignant thymic masses
demonstrate similar CT results their treatment programs differ
substantially (5). Therefore,
identifying the benign or malignant nature of these masses would
have great significance for assessing the condition of patients,
making treatment decisions and evaluating prognosis (5–8).
Biopsies provide strong evidence for differentiating
between benign and malignant tumors and their use has become more
common (9), but they remain an
invasive examination. Biopsies are likely to increase the risk of
disseminating the tumor cells along the needle tract, and patients
with thymoma and myasthenia gravis are more likely to enter
myasthenic crisis (10,11). Therefore, the development of a
non-invasive, simple and economical examination method would have
clinical significance. Positron emission tomography (PET)/CT has
previously been reported to exhibit certain value for grading the
malignancies of thymic tumors (12,13), but
this method would face difficulties spreading in developing
countries due to economic factors. Images of thymoma have also
previously been reported to be discovered in
99mTc-methoxyisobutylisonitrile (MIBI) myocardial
perfusion imaging by accident (14,15), which
provided certain guidance for the present study. A functional
imaging method, MIBI single-photon emission computed tomography
(SPECT), was able to reflect the metabolic activities of tumors,
thus helping to preliminarily determine the natures of the tumors.
This method is simple, economical, and readily accepted by
patients, so it is worthy of further research and application. In
the present study, postoperative pathologies were used as the basis
to investigate the application value of 99mTc-MIBI
imaging to differentiate between benign and malignant thymic
masses, thus providing the basis for clinical diagnosis and
treatment.
Materials and methods
Study subjects
A total of 32 patients diagnosed with mediastinal
space-occupying masses in the thymic region by CT or MRI between
February 2014 and December 2015 at The Affiliated Hospital of
Qingdao Medical University (Qingdao, China) were selected,
including 13 males and 19 females, aged 27 to 74 years, with a mean
of (50.6±11.1) years. The present study was conducted in accordance
with the declaration of Helsinki. The present study was conducted
with approval from the Ethics Committee of Qingdao Medical
University (Qingdao, China) and written, informed consent was
obtained from all participants. Following 99mTc-MIBI
radionuclide imaging, all patients underwent surgical removal of
the thymic masses, which were then used for postoperative biopsies.
According to the postoperative pathological results, these patients
were divided into three groups as follows: Those with benign thymic
masses (the BT group, including 9 cases of thymic hyperplasia, 1
case of mature cystic teratom, and 1 case of thymic cyst; n=11),
those with low-grade malignant thymoma (LRT group, including 1 case
of type A, and 9 cases of type AB, n=10), and those with
intermediate-grade malignant thymoma (IRT group, 2 cases of type
B1, 6 cases of type B2, and 3 cases of type B3; n=11) (16).
99mTc-MIBI-SPECT
Following intravenous injection of 740
megabecquerels of the imaging agent 99mTc-MIBI (provided
by Shihong Drug Development Center, Beijing Normal University,
Beijing, China, with a chemical purity of 95–98%), a Hawkeye
Millennium VG type SPECT device (GE Healthcare, Chicago, IL, USA)
was then used for imaging. This was accompanied by a low-energy,
high-resolution, parallel-hole collimator (GE Healthcare), with the
energy peak set as 140 KeV, window width as 20%, acquisition matrix
as 512×512 and magnification as 1.0, to perform planar and SPECT
imaging of local lesions. The planar images in the early phase (15
min following injection) and the delayed phase (2 h following
injection) were collected, as well as fusion imaging to assist
positioning if necessary.
Imaging interpretation
The equivalent irregular regions of interest
delineating the tumor and the background (lung) were manually drawn
by two experienced nuclear medicine physicians. For each lesion,
the uptake index was determined by dividing the average
counts/pixel within a lesion over the average counts/pixel in
normal tissues. Then the ratio of tumor to background (T/N) was
calculated. This generated T/N ratios for the early phase (e) and
the delayed phase (d). The 2-h washout index (WI) was calculated
according to the following formula: WI=[T/N (e)-T/N (d)]/T/N (e) ×
100%]. The 2-h retention index (RI) was calculated according to the
following formula: RI=[T/N(d)-T/N (e)]/T/N (e) × 100%]. The final
results were decided by the consensus of at least two nuclear
physicians.
Statistical analysis
The mean and standard deviation of the T/N ratio, RI
and WI were calculated. The intragroup comparisons between T/N(e)
and T/N(d) were performed using paired Student's t tests. Multiple
comparisons between the three groups was performed using one-way
analysis of variance. P<0.05 was considered to indicate a
statistically significant difference. SPSS 17.0 software (SPSS,
Inc., Chicago, IL, USA) was used for analysis.
Results
Comparison of MIBI uptake between
benign and malignant groups
Among the 12 patients of the BT group, the majority
of the masses revealed no significant radioactivity uptake in the
early and delayed phases, with the exception of a single case with
multilocular thymic cysts. Radioactivity uptake was similar to the
background radioactivity count. A representative case from the BT
group was depicted in Fig. 1. Among
the 21 patients included in the LRT and IRT groups, the majority
exhibited various degrees of radioactivity uptake, with the
exception of a single case of B3-type thymoma, with the sensitivity
as 95.24%, and the specificity as 90.91% (Table I). A representative case from the
malignant groups was depicted in Fig.
2.
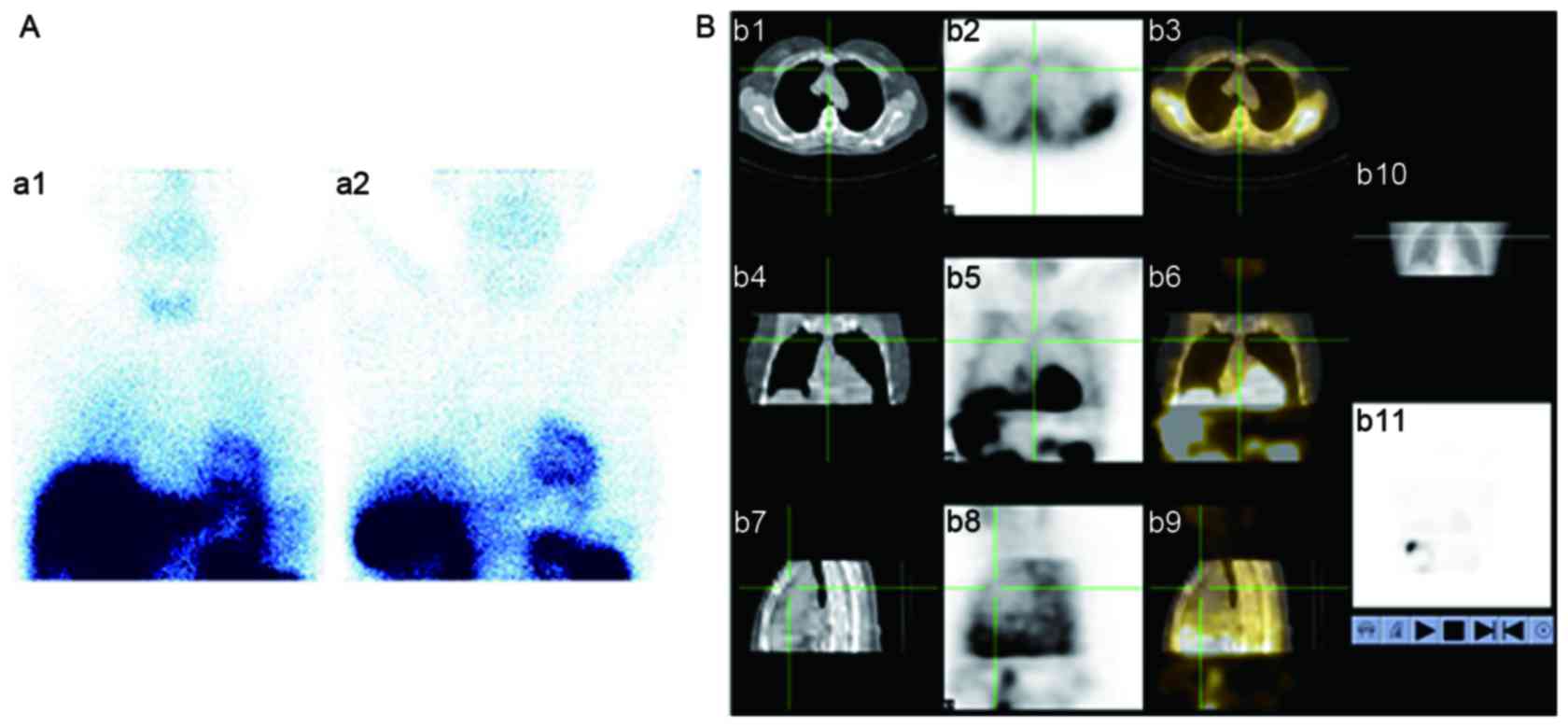
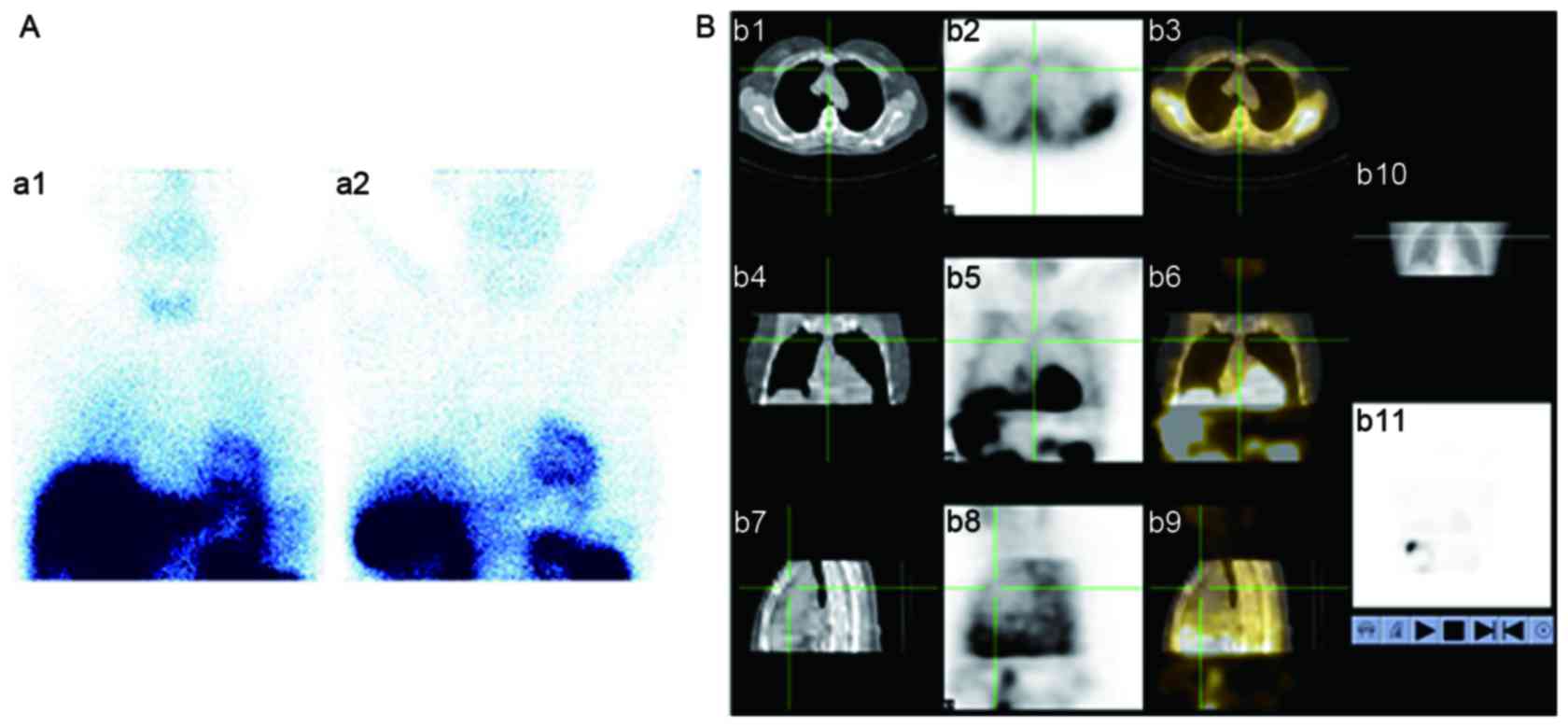 | Figure 1.A representative case from the benign
thymic mass group. The depicted patient is female (58 years old).
Physical examination revealed the presence of an anterior
mediastinal mass. (A) 99mTc-methoxyisobutylisonitrile
imaging. a1, early stage; a2, delayed stage. There was almost no
uptake in the two stages. (B) single-photon emission computed
tomography/computed tomography fusion imaging. b1-b3, transverse
view of CT, SPECT and fusion image, respectively. b4-b6, cronal
view of CT, SPECT and fusion image, respectively. b7-b9, sagittal
view of CT, SPECT and fusion image, respectively. b10, location
image. b11, 3D of SPECT image. SPECT, single-photon emission
computed tomography. |
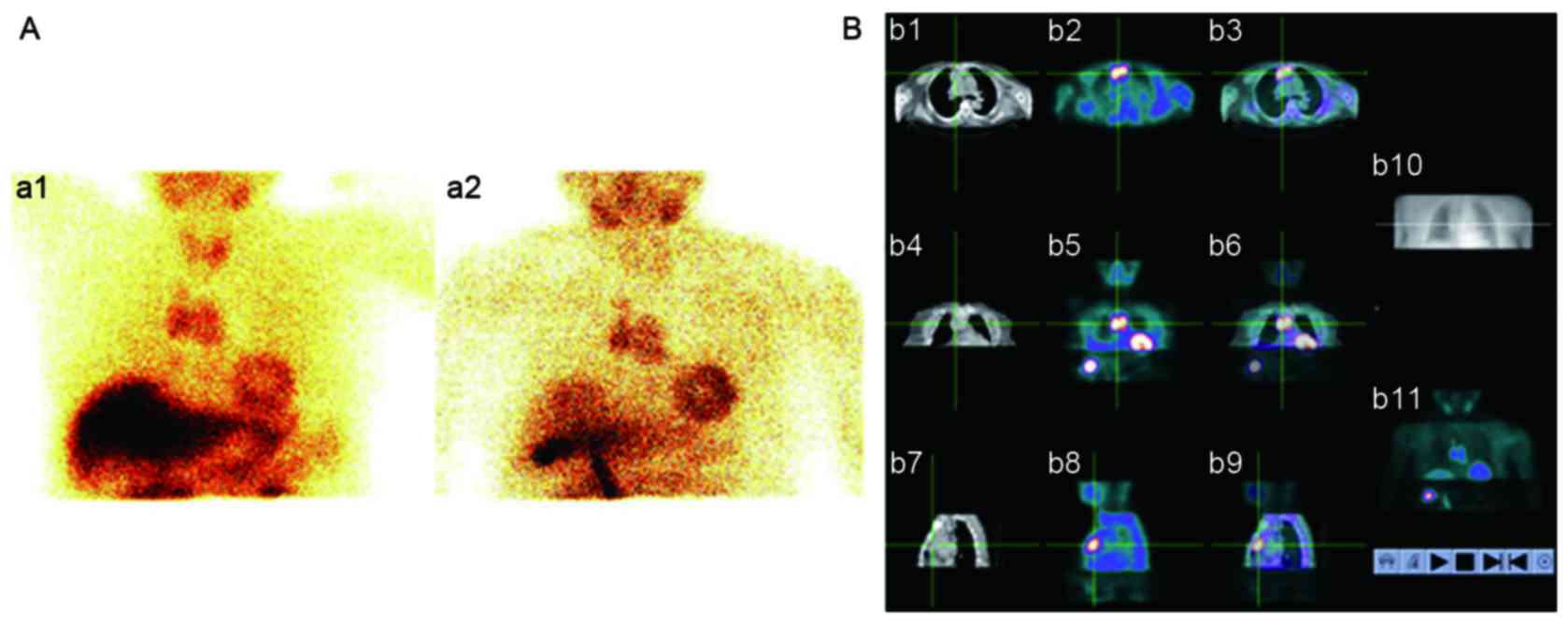
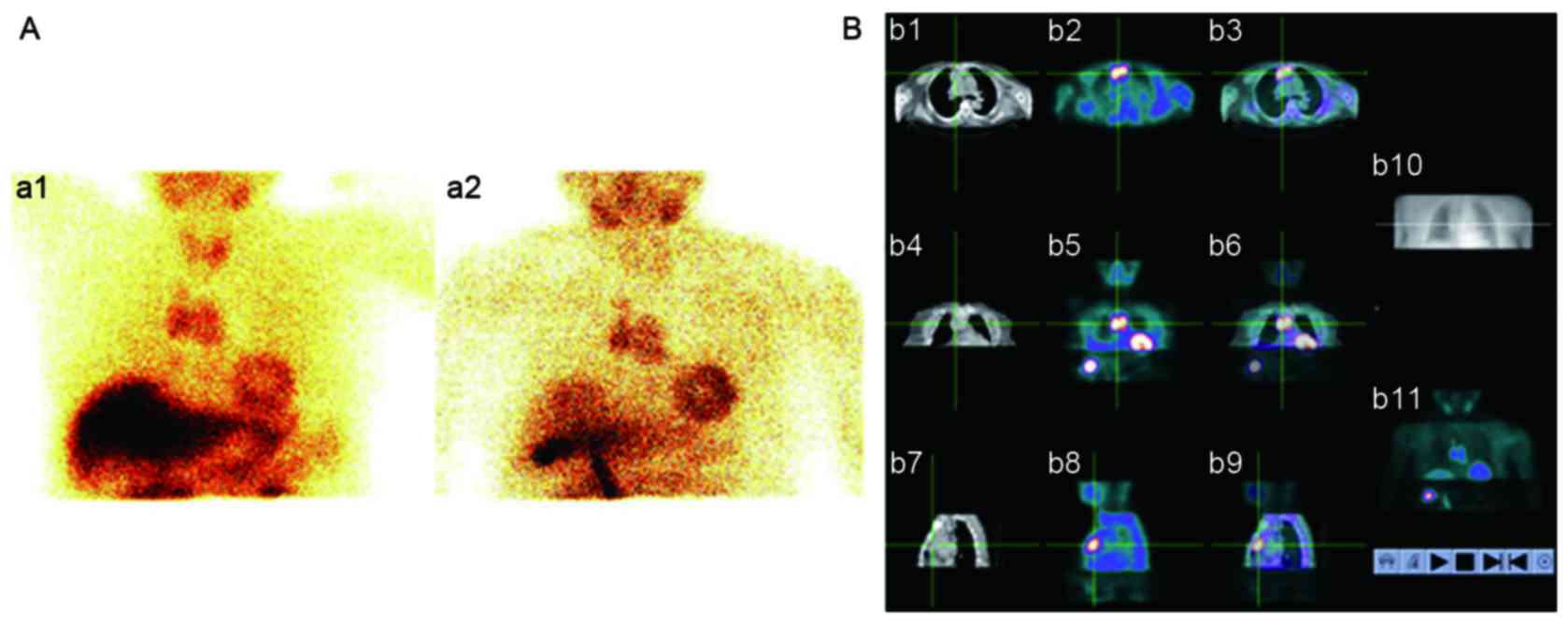 | Figure 2.A representative case from the
malignant groups. The depicted patient is female (63 years old).
Physical examination revealed the presence of a thymic mass. It was
confirmed to be thymoma (type AB) by postsurgical pathology. (A)
99mTc-methoxyisobutylisonitrile imaging. a1, early
stage; a2, delayed stage. (B) Single-photon emission computed
tomography/computed tomography fusion imaging. b1-b3, transverse
view of CT, SPECT and fusion image, respectively. b4-b6, cronal
view of CT, SPECT and fusion image. b7-b9, sagittal view of CT,
SPECT and fusion image. b10, location image. b11, 3D of SPECT
image. SPECT, single-photon emission computed tomography; CT,
computed tomography. |
 | Table I.
99mTc-methoxyisobutylisonitrile imaging results for the
benign and malignancy groups. |
Table I.
99mTc-methoxyisobutylisonitrile imaging results for the
benign and malignancy groups.
| Group | Positive | Negative |
|---|
| Benign group | 1 | 10 |
| Malignancy
groups | 20 | 1 |
Comparison of semi-quantitative
analysis of MIBI uptake among three groups
There was no statistically significant difference
between T/N(e) and T/N(d) in the BT group (P=0.253), but the
differences between T/N(e) and T/N(d) in the LRT and IRT groups
were statistically significant (P=0.045 and P=0.001,
respectively).
The comparison of T/N(e) between the three groups
revealed a statistically difference (P<0.001; Table II), among which the differences
between the BT and LRT groups, as well as between the LRT and IRT
groups, were statistically significant (P<0.001; Table II). However, the difference between
the BT and IRT groups was not significant (P=0.339; Table II). The comparison of T/N(d) between
the three groups revealed a statistically significant difference
(P<0.001; Table II), among which
the differences between the BT and LRT groups, as well as between
the LRT and IRT groups, were statistically significant (P<0.001;
Table II), while the difference
between the BT and IRT groups was not significant (P=0.08; Table II).
 | Table II.Comparison of semi-quantitative
indexes of radioactivity uptake among the three groups. |
Table II.
Comparison of semi-quantitative
indexes of radioactivity uptake among the three groups.
| Group | T/N (e) | T/N (d) | WI, % | RI, % |
|---|
| BT group | 1.033±0.163 |
1.011±0.143a |
|
|
| LRT group |
2.750±1.149b |
1.011±0.143c |
5.778±7.716 | −5.778±7.71 |
| IRT group |
1.317±0.182d |
1.482±0.155e | −13.315±9.410 | 13.315±9.410 |
The present study also revealed that T/N(e) and
T/N(d) of the patient with multilocular thymic cysts exhibited
apparent radioactivity uptake, so this case was seen as a false
positive and removed from the BT group when performing
semi-quantitative analysis. Another case with B3-type thymoma from
the IRT group revealed no significant radioactivity uptake in the
early or delayed phase, so it was seen as a false negative and
removed from the IRT group when performing semi-quantitative
analysis.
Fig. 1 depicted a
representative case from the BT group. The 10 min and 2 h
99mTc-MIBI images revealed no abnormal radioactivity
concentration shadow in the mediastinum (Fig. 1A). Fusion CT imaging revealed a soft
tissue mass in the anterior mediastinum, and SPECT/CT fusion
imaging revealed no significant radioactivity uptake in this soft
tissue mass (Fig. 1B). The diagnosis
was an anterior mediastinal mass, with a high probability of being
a benign lesion. Postoperative pathology revealed the presence of
thymic cysts and the cyst wall was primarily composed of
proliferated fibrous connective tissues, which contained more
lymphoid tissues, and was consistent with the diagnosis of
space-occupying thymic cysts. Fig. 2
depicted a representative case from the malignant groups. The 10
min 99mTc-MIBI image revealed an abnormal
dumbbell-shaped radioactivity uptake shadow in the mediastinum, and
the 2 h image revealed that the mass was still clear, without
significant regression (Fig. 2A).
Fusion CT imaging revealed that the thymus was irregularly
increased, and the abnormal dumbbell-shaped radioactivity uptake
shadow in the mediastinum was concentrated in the thymus (Fig. 2B). The diagnosis was a thymic mass,
with a 10-min T/N value 2.74, 2 h T/N value 2.88, and it was not
possible to rule out the probability of malignancy. Postoperative
pathology revealed the presence of thymoma (type AB).
Discussion
At present, 99mTc-MIBI imaging is the
most common non-specific imaging method for tumors in China, and it
has important application value for differentiating between benign
and malignant lesions in the chest, and while its applications for
the diagnosis of thymic masses are rarely reported it is more
commonly used for patients with breast cancer, lung cancer, thyroid
cancer, and malignant soft tissue metastases (14,15).
MIBI is positively charged, lipophilic molecule, so
its uptake by cells occurs through trans-membrane potential
difference, and may become concentrated inside the mitochondria and
cytoplasm. Malignant cells have a rich metabolism and abundant
mitochondria, so they have higher negative trans-membrane
potentials. Therefore, it may be possible to use this imaging
technique for differential diagnosis of benign and malignant tumors
(8,17). The results of the present study
revealed that the majority of thymic benign lesions demonstrated no
apparent MIBI uptake, while the thymoma groups demonstrated various
degrees of increased or concentrated MIBI uptake in the mass
regions, with the diagnostic sensitivity set as 95.24%, and the
specificity as 90.91%. This indicated that 99mTc-MIBI
imaging may also potentially be used to distinguish between benign
and malignant thymic masses.
Certain previous studies have confirmed that the
uptake of 99mTc-MIBI is not only associated with the
blood supply, capillary permeability and density of tumor cells,
but also with the vitality of mitochondria (13,14,17).
Patients with rapid tumor proliferation, high metabolism and low
tissue differentiation normally exhibited high uptake of
99mTc-MIBI in the early phase (18,19).
Fiorelli et al (17) reported
that the uptake of MIBI by thymoma was increased with the
increasing degree of malignancy of the tumor (the T/N values of
type A, B and C were 1.3±0.2,1.8±0.3 and 2.7±0.5, respectively).
The present study revealed that the uptake ratio in the early phase
of the thymoma group was not associated with the degree of
malignancy. It was not possible to diagnose mild uptake in the
early phase as benign, as certain highly malignant thymoma also
demonstrated mild uptake in the early phase, and patients with
higher degrees of malignancy demonstrated a gradual concentration
of radioactivity uptake within a certain period, namely higher RI.
The patients with low-grade malignancies demonstrated a greater
concentration of radioactivity uptake in the early phase, while the
uptake was reduced in the delayed phase, namely higher WI.
Therefore, low uptake with high retention of 99mTc-MIBI
in the early phase may indicate a higher degree of malignancy and
poor prognosis, so greater clinical attention should be paid and
the appropriate treatment programs should be selected. Conversely,
high uptake and high washout of 99mTc-MIBI in the early
phase may indicate a lower degree of malignancy and an improved
prognosis. Previous studies (18,20–23)
demonstrated that MIBI was the common transport substrate of
phosphoric acid glycoprotein (Pgp) and multidrug
resistance-associated protein (MRP), and were actively transported
out of the tumor cells by Pgp and MRP. Therefore, overexpression of
Pgp or MRP may decrease the concentration of MIBI uptake inside the
tumor cells. To determine whether Pgp or MRP were more highly
expressed in the group with high-grade malignant thymoma requires
additional large-sample studies at the molecular level.
There were certain limitations associated with the
present study. The cohort of patients included one case of
multilocular thymic cysts-which demonstrated apparent radioactivity
uptake in the early and delayed phases. This may be because the
cystic components altered the membrane permeability and the
potential difference on each side of the cell membrane (24). Another patient with B3-type thymoma
demonstrated no significant uptake of MIBI in the early or delayed
phase, and this may be due to the presence of an increased number
of necrotic components inside the tumor tissues. In addition, the
present study had a small sample size, and lacked the cases of
thymic cancer (C-type). However, MIBI imaging may still be a
potential method for the diagnosis of thymoma.
In short, 99mTc-MIBI imaging was able to
accurately discriminate between benign and malignant thymic masses,
and has the potential to be used to assess the malignancy of
thymoma at a preliminary stage. Thus, it may have significance for
the clinical treatment and evaluation of thymoma.
References
|
1
|
Suster S and Moran CA: Primary thymic
epithelial neoplasms showing combined features of thymoma and
thymic carcinoma. A clinicopathologic study of 22 cases. Am J Surg
Pathol. 20:1469–1480. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Priola AM, Priola SM, Cardinale L, Cataldi
A and Fava C: The anterior mediastinum: Diseases. Radiol Med.
111:312–342. 2006.(In English, Italian). View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Venuta F, Anile M, Diso D, Vitolo D,
Rendina EA, De Giacomo T, Francioni F and Coloni GF: Thymoma and
thymic carcinoma. Eur J Cardiothorac Surg. 37:13–25. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Aroor AR, Prakasha SR, Seshadri SST and
Raghuraj U: A study of clinical characteristics of mediastinal
mass. J Clin Diagn Res. 8:77–80. 2014.PubMed/NCBI
|
|
5
|
Tomiyama N, Honda O, Tsubamoto M, Inoue A,
Sumikawa H, Kuriyama K, Kusumoto M, Johkoh T and Nakamura H:
Anterior mediastinal tumors: Diagnostic accuracy of CT and MRI. Eur
J Radiol. 69:280–288. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Molina PL, Siegel MJ and Glazer HS: Thymic
masses on MR imaging. AJR Am J Roentgenol. 155:495–500. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
de Jong WK, Blaauwgeers JL, Schaapveld M,
Timens W, Klinkenberg TJ and Groen HJ: Thymic epithelial tumours: A
population-based study of the incidence, diagnostic procedure and
therapy. Eur J Cancer. 44:123–130. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hoerbelt R, Keunecke L, Grimm H, Schwemmle
K and Padberg W: The value of a noninvasive diagnostic approach to
mediastinal masses. Ann Thorac Surg. 75:1086–1090. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kesler KA, Wright CD and Loehrer PJ Sr:
Thymoma: Current medical and surgical management. Semin Neurol.
24:63–73. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Higuchi T, Taki J, Kinuya S, Yamada M,
Kawasuji M, Matsui O, Nonomura A, Bunko H and Tonami N: Thymic
lesions in patients with myasthenia gravis: Characterization with
thallium 201 scintigraphy. Radiology. 221:201–206. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Priola AM and Priola SM: Imaging of thymus
in myasthenia gravis: From thymic hyperplasia to thymic tumor. Clin
Radiol. 69:e230–e245. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Scagliori E, Evangelista L, Panunzio A,
Calabrese F, Nannini N, Polverosi R and Pomerri F: Conflicting or
complementary role of computed tomography (CT) and positron
emission tomography (PET)/CT in the assessment of thymic cancer and
thymoma: Our experience and literature review. Thorac Cancer.
6:433–442. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Treglia G, Sadeghi R, Giovanella L,
Cafarotti S, Filosso P and Lococo F: Is (18)F-FDG PET useful in
predicting the WHO grade of malignancy in thymic epithelial tumors?
A meta-analysis. Lung Cancer. 86:5–13. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Malek H, Ghaedian T, Yaghoobi N, Rastgou
F, Bitarafan-Rajabi A and Firoozabadi H: Focal breast uptake of
99mTc-sestamibi in a man with spindle cell lipoma. J Nucl Cardiol.
19:618–620. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gedik GK, Ergün EL, Aslan M and Caner B:
Unusual extracardiac findings detected on myocardial perfusion
single photon emission computed tomography studies with Tc-99m
sestamibi. Clin Nucl Med. 32:920–926. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rosai J: Histological typing of tumors of
the thymus. 2nd. World Health Organization International
Histological Classification of Tumors. Berlin, Springer-Verlag;
1999, View Article : Google Scholar
|
|
17
|
Fiorelli A, Vicidomini G, Laperuta P,
Rambaldi P, Mansi L, Rotondo A and Santini M: The role of
Tc-99m-2-Methoxy-Isobutyl-Isonitrile Single Photon Emission
Computed Tomography in visualizing anterior mediastinal tumor and
differentiating histologic type of thymoma. Eur J Cardiothorac
Surg. 40:136–142. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
García-Talavera P, Olmos R, Sainz-Esteban
A, Ruiz MÁ, González ML and Gamazo C: Evaluation by SPECT-CT of an
incidental finding of a thymoma and breast cancer in a myocardial
perfusion SPECT with 99mTc-MIBI. Rev Esp Med Nucl Imagen Mol.
32:260–262. 2013.PubMed/NCBI
|
|
19
|
Hashimoto T, Goto K, Hishinuma Y, Yachuda
K, Sugioka Y, Arai K, Harada S and Goto M: Uptake of
99mTc-tetrofosmin, 99mTc-MIBI and 201Tl in malignant thymoma. Ann
Nucl Med. 14:293–298. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sasajima T, Shimada N, Naitoh Y, Takahashi
M, Hu Y, Satoh T and Mizoi K: (99m)Tc-MIBI imaging for prediction
of therapeutic effects of second-generation MDR1 inhibitors in
malignant brain tumors. Int J Cancer. 121:2637–2645. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sun SS, Hsieh JF, Tsai SC, Ho YJ, Lee JK
and Kao CH: Expression of mediated P-glycoprotein multidrug
resistance related to Tc-99m MIBI scintimammography results. Cancer
Lett. 153:95–100. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kurata S, Ushijima K, Kawahara A, Kaida H,
Kawano K, Hirose Y, Kage M, Kamura T, Ishibashi M and Abe T:
Assessment of 99mTc-MIBI SPECT(/CT) to monitor multidrug
resistance-related proteins and apoptosis-related proteins in
patients with ovarian cancer: A preliminary study. Ann Nucl Med.
29:643–649. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Baumert C and Hilgeroth A: Recent advances
in the development of P-gp inhibitors. Anticancer Agents Med Chem.
9:415–436. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Araki T, Sholl LM, Gerbaudo VH, Hatabu H
and Nishino M: Intrathymic cyst: Clinical and radiological features
in surgically resected cases. Clin Radiol. 69:732–738. 2014.
View Article : Google Scholar : PubMed/NCBI
|