Introduction
Hemolymphangioma is a comparatively rare tumor
comprising newly-formed lymph spaces and blood vessels (1). The tumor can occur at any age and may
involve any part of the body (1–12).
Hemolymphangioma typically originates from congenital malformations
of the vascular and lymphatic system. Only a small number of cases
have been reported in the mediastinum (13–19),
spleen (4,6) and neck (20). In previously reported cases,
completely cystic and/or multifocal hemolymphangioma were extremely
rare. The correct preoperative diagnosis of hemolymphangioma
remains a challenge.
The present case report describes the diagnosis,
treatment and outcomes of 4 patients with hemolymphangioma that
were admitted to the Second Affiliated Hospital of Xi'an Jiaotong
University (Xi'an, China). All patients were female, with a mean
age of 44.7 years and a mean duration of symptoms prior to
diagnosis of 2.7 years. A total of 5 lesions were identified across
the four cases. One patient had multifocal hemolymphangioma in the
mediastinum and spleen. The other 3 patient's tumors were located
in the antero-superior mediastinum, neck and left forearm,
respectively. Owing to the rare nature of hemolymphangioma,
preoperative diagnosis is challenging. In the present case report,
the radiological findings of hemolymphangioma in 4 patients are
described, including the unusual imaging characteristics
observed.
Case report
Patient details
All patients were admitted to the Second Affiliated
Hospital of Xi'an Jiaotong University. Written informed consent was
obtained from all patients.
Case 1
A 43-year-old female patient was admitted with a
complaint of a mediastinal mass identified during a medical
examination ~1 year prior to admission. The patient did not
complain of any other discomfort. The patient had a history of
uterus teratoma detected 7 months prior to admission. No
abnormalities were detected by laboratory examinations (blood
routine examination and biochemical examination, including blood
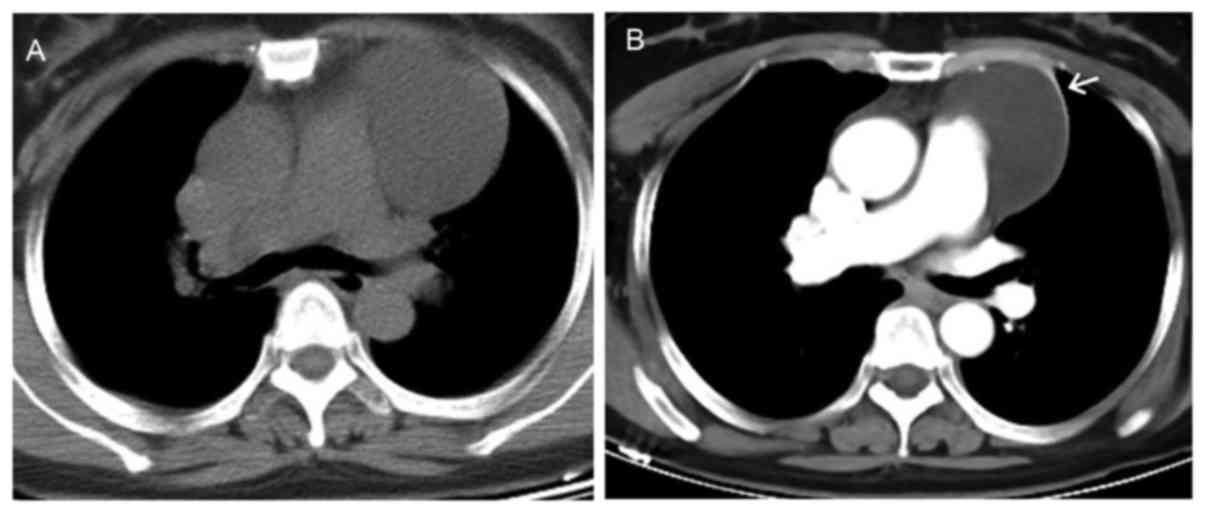
glucose analysis and triglyceride test). Computed tomography (CT)
demonstrated a well-defined cystic mass (5.4×6.9×6.6 cm) in the
left antero-superior mediastinum (Fig.
1A). The tumor was adjacent to the aortic arch and the
pulmonary trunk with a homogeneous density of 15 Hounsfield units
(HU) on plain CT images. Following contrast (iohexol, 350 mgI/ml,
4–5 ml/s) injection, the left and anterior parts of the wall of the
tumor exhibited significant enhancement, while the inside content
of the mass did not exhibit any enhancement compared with
pre-contrast images (Fig. 1B).
Neither calcification nor enlarged lymph nodes were observed. The
adjacent organs were slightly compressed and no bone destruction
was observed in the neighboring spine. Based on these findings, a
cystic hygroma was initially considered as the diagnosis.
The patient underwent a tumorectomy by thoracoscopy.
During the surgery, a well-defined cystic mass containing clear
liquid was identified in the left side of the antero-superior
mediastinum with a thin wall. Subsequently, the tumor was
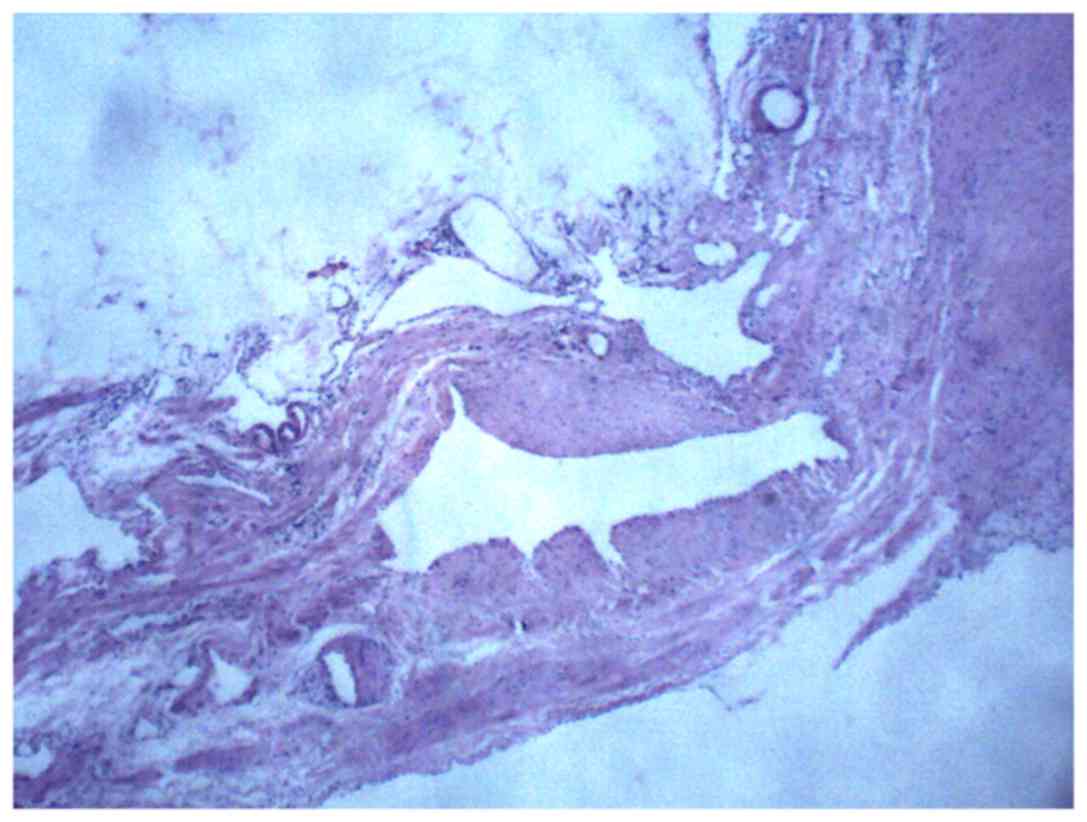
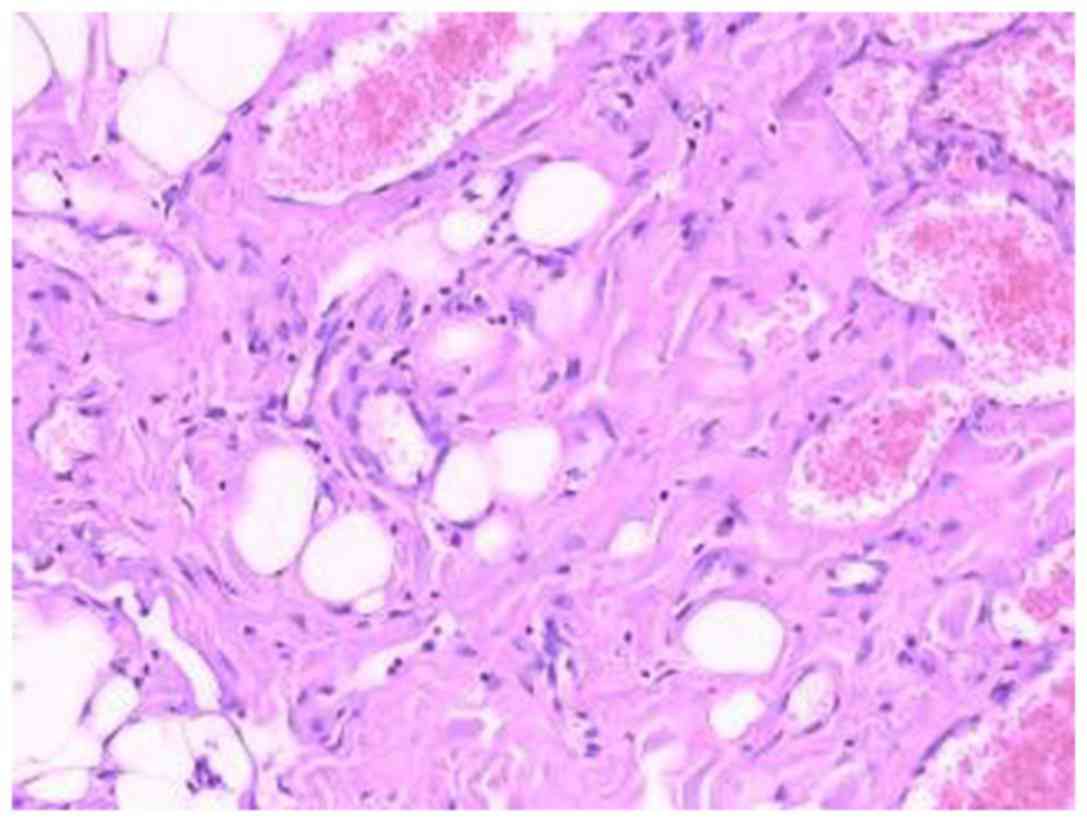
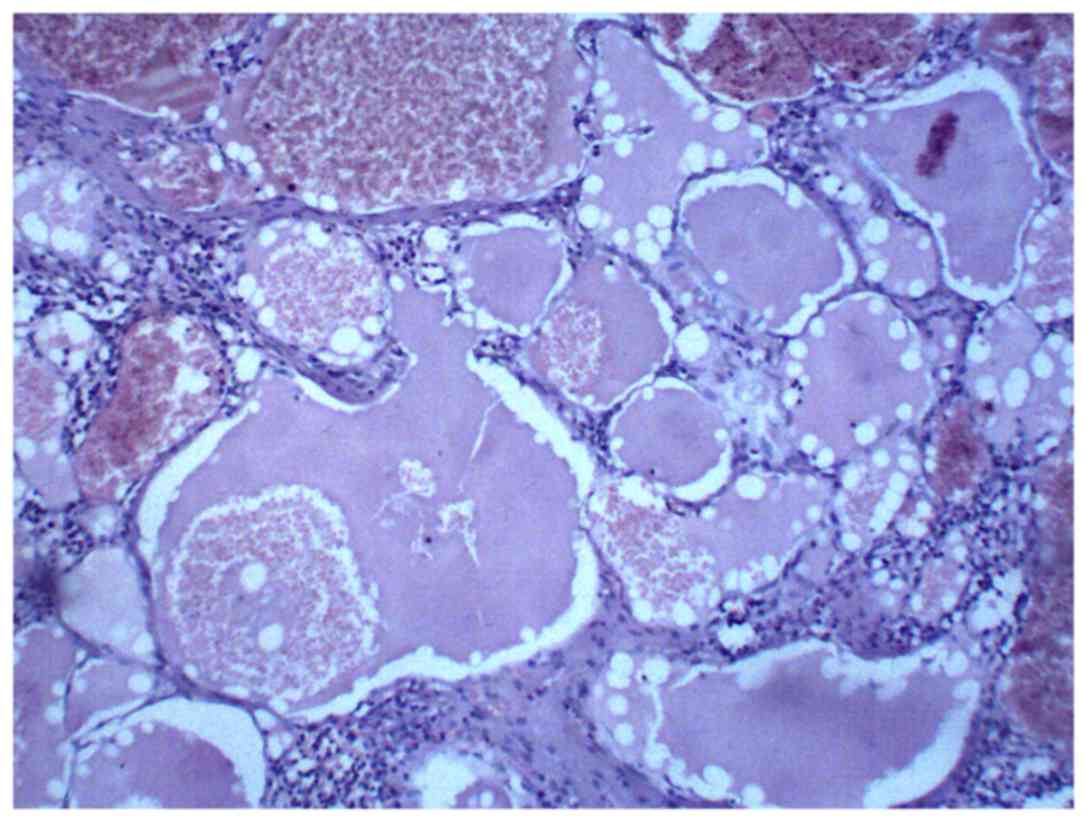
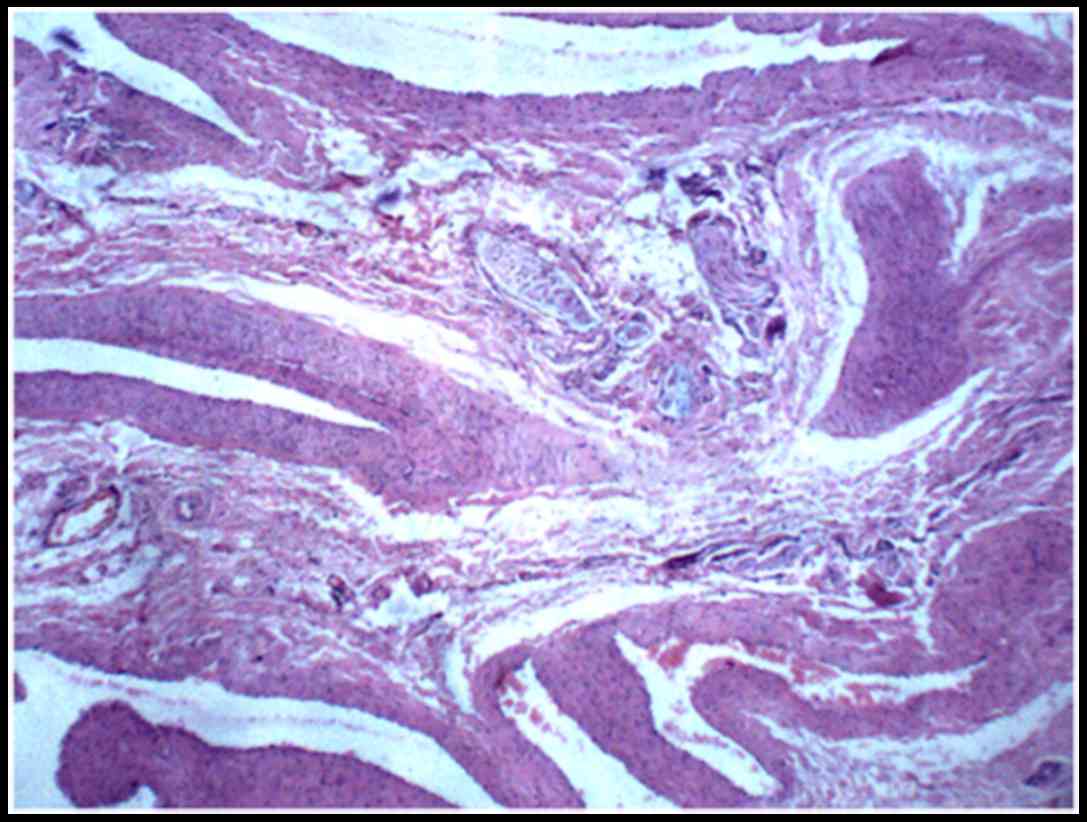
completely excised. Hematoxylin and eosin (H&E) staining of the
specimen was performed as previously described (5) and revealed dilated lymphatic vessels and
blood vessels in the tumor (Fig. 2).
A follow-up CT scan of chest revealed no recurrence ~9 months after
surgery.
Case 2
A 59-year-old female patient presented with a mass
on the right side of the neck. A total of ~9 months prior to
presentation at the hospital, the patient identified a walnut-like
mass on the right side of their neck. The mass grew gradually over
the following months. At first, the patient did not feel pain or a
burning sensation upon touching the mass and did not experience
weight loss. As the mass grew, the patient felt slight
pain/discomfort and exhibited limited cervical activity. The
patient had a high blood pressure (BP) that persisted for 5 years
(highest BP reading, 180/100 mmHg) prior to admission and was
prescribed oral medication (antihypertensive agents, taken daily)
to control their BP. A total of ~7 years prior to admission, the
patient underwent lobectomy of the left lobe of the thyroid for the
treatment of thyroid cancer). Following the surgery, the patient
took levothyroxine sodium regularly (50 µg/tablet, 1/4 tablet a
day).
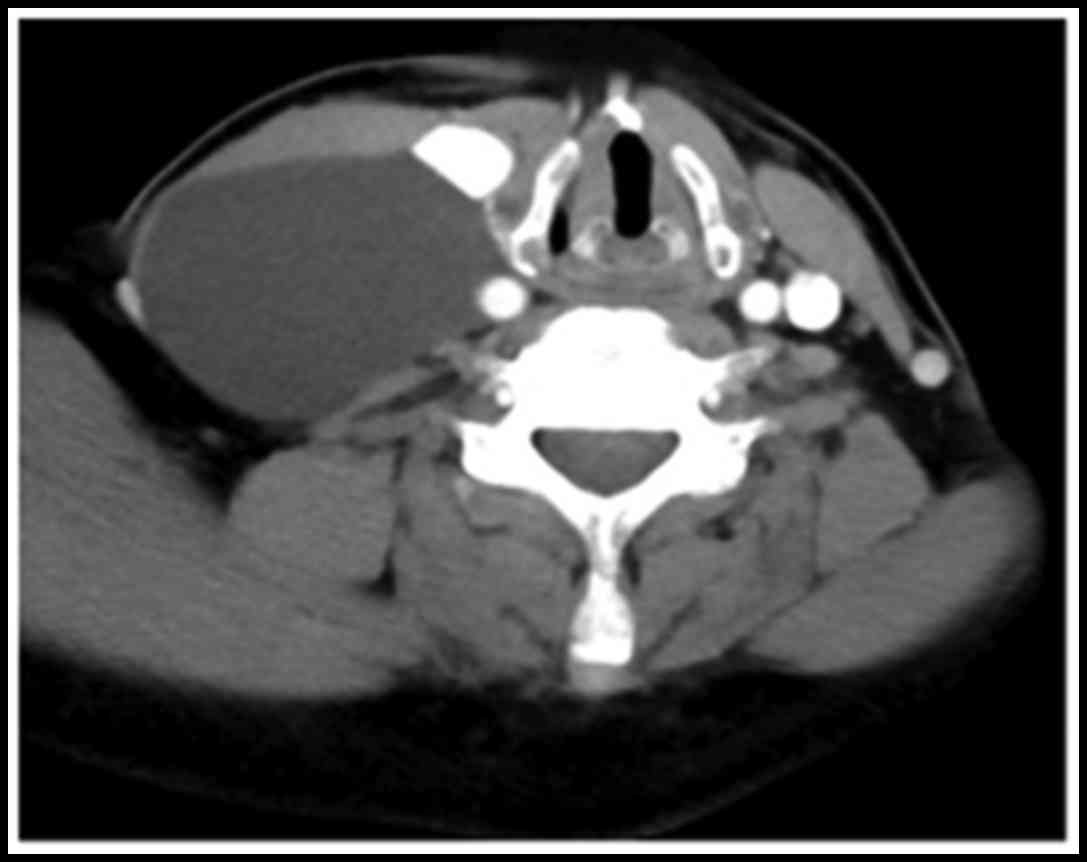
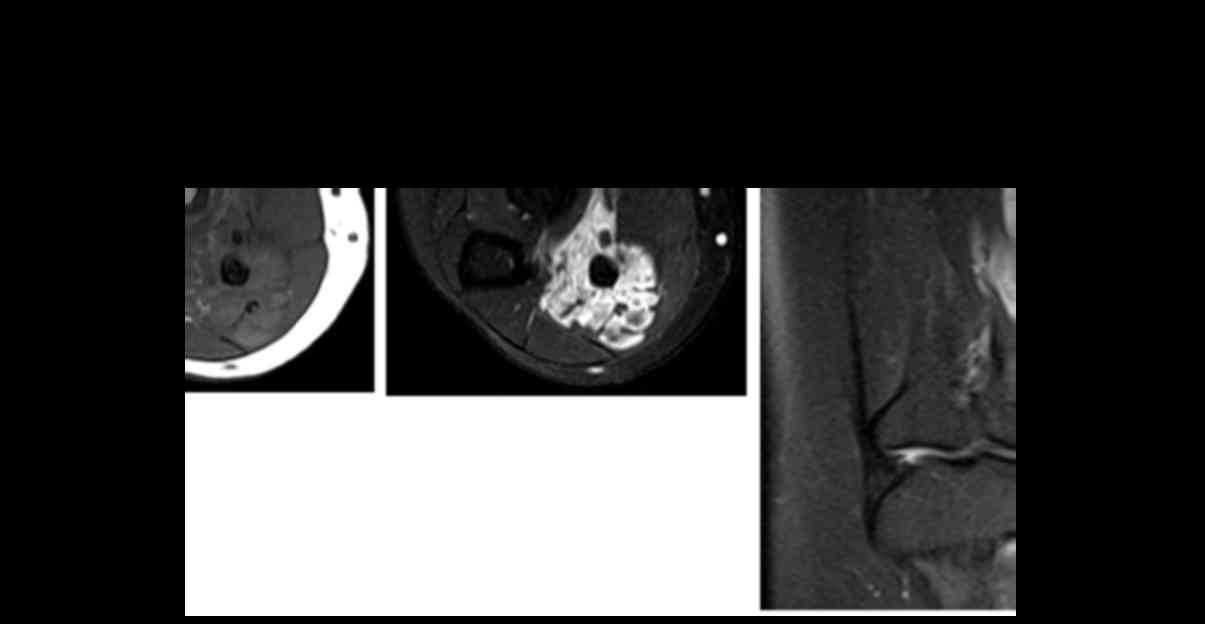
Post-contrast CT and pre-contrast magnetic resonance
imaging (MRI) were performed. The CT scan revealed a large cystic
mass (8×6×4 cm) occupying the right side of the neck (Fig. 3). The right carotid artery and jugular
vein were shifted to the left side, the right sternocleidomastoid
was pressed and shifted forward, and the trachea was slightly
shifted to the left. No bone destruction or enlarged lymph nodes
were observed.
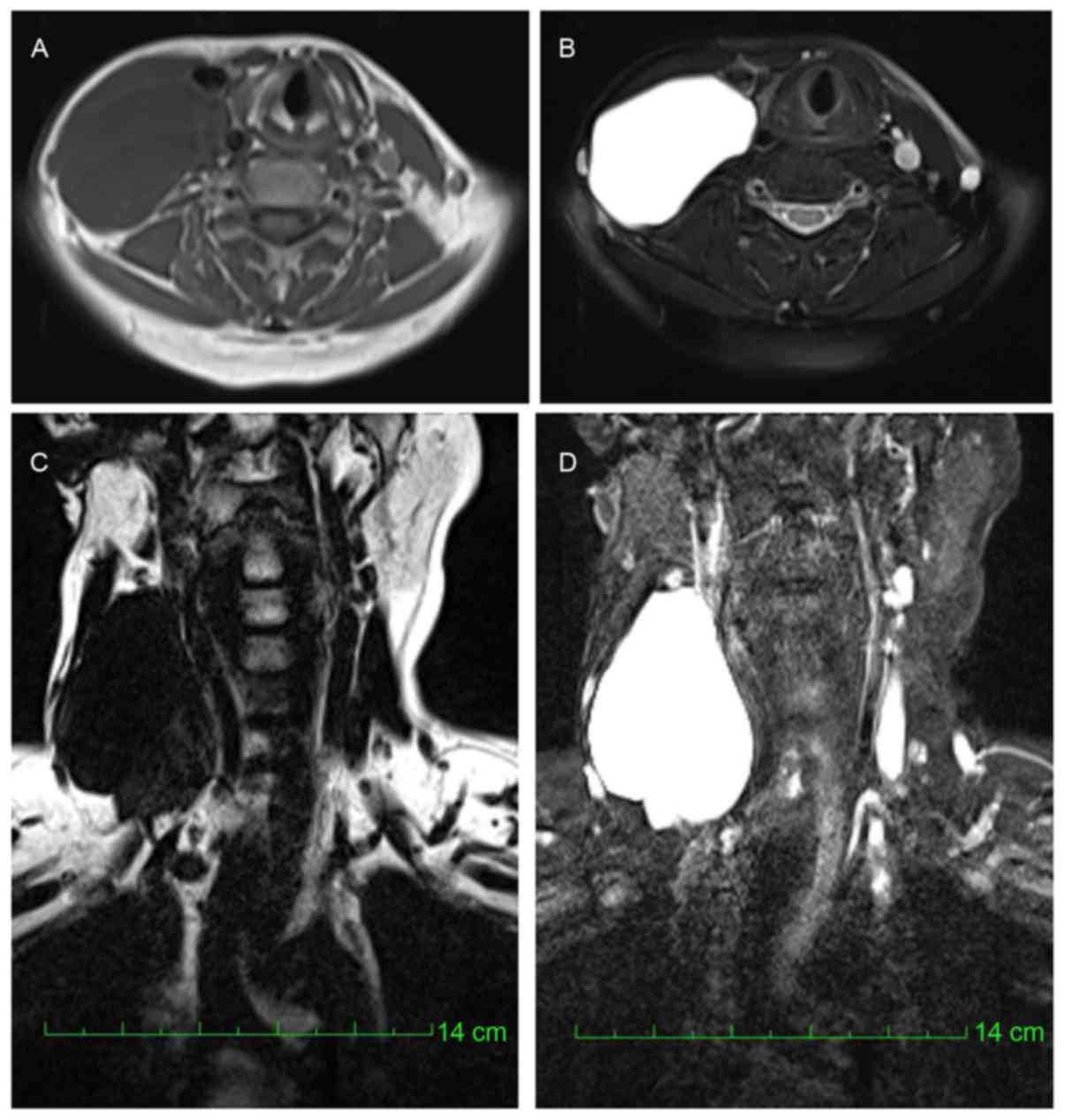
MRI revealed a mass lying on the right side of the
neck. The mass exhibited hypo-intensity on T1-weighted images
(T1WI; Fig. 4A), homogeneous
hyper-intensity on T2-weighted images (T2WI; Fig. 4B) and was well defined. The inferior
part of the mass was irregular (Fig.
4C). Water-fat separation MRI of the neck revealed a mass with
homogeneous hypointensity on the water-suppression images (Fig. 4C) and significant hyperintensity on
the fat-suppression images (Fig.
4D).
The patient underwent a surgical resection of the
tumor, during which a cystic mass was observed. The diolame
ruptured during surgery. The mass was completely excised and
histological analysis (H&E staining) supported a diagnosis of
hemolymphangioma (Fig. 5). The
patient was asymptomatic during a follow-up period of 10
months.
Case 3
A 48-year-old female patient with a known
mediastinal mass detected 1 year prior to presentation, was
referred for further examination and treatment due to a sporadic
cough and chest pain. The patient reported slight pain on the left
side of the chest which was accompanied by left shoulder pain and
back pain. In addition, the patient reported eyelid weakness that
became more severe when fatigued. The symptoms aggravated gradually
prior to the admission. The laboratory results (blood routine
examination and biochemical examination, including blood glucose
analysis and triglyceride test) were all within the normal
range.
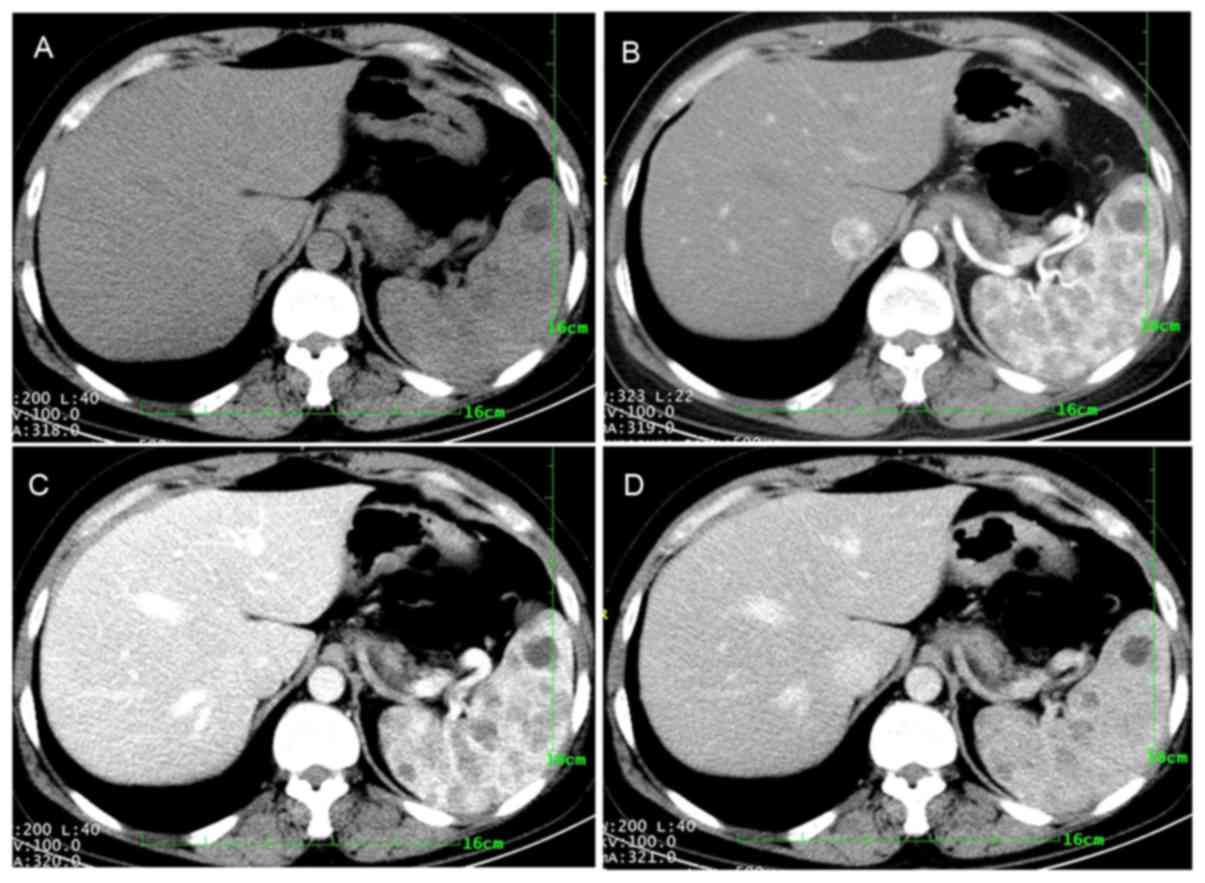
CT revealed a lobulated solid mass within the
mediastinum, with a size of 3×4×5 cm (Fig. 6A). The tumor was adjacent to the
aortic arch and left pulmonary artery. The mass showed iso-density
with internal scattered calcification inside on plain CT images and
progressive enhancement on post-contrast CT images (Fig. 6B and C).
Notably, the patient had a large spleen (size
determined by CT, 15×10×10 cm) and a myoma of the uterus. Multiple
nodules were observed in the spleen. Progressive enhancement was
observed for the majority of nodules on post-contrast (iohexol, 350
mgI/ml) CT images (Fig. 7). These
nodules were originally considered to be a hemangioma or
lymphangioma. In addition, there were a small number of nodules
that exhibited no enhancement, which were considered to be cysts.
The patient underwent resection of the mediastinal mass and a
splenectomy. The interval between the two surgeries was 9 months.
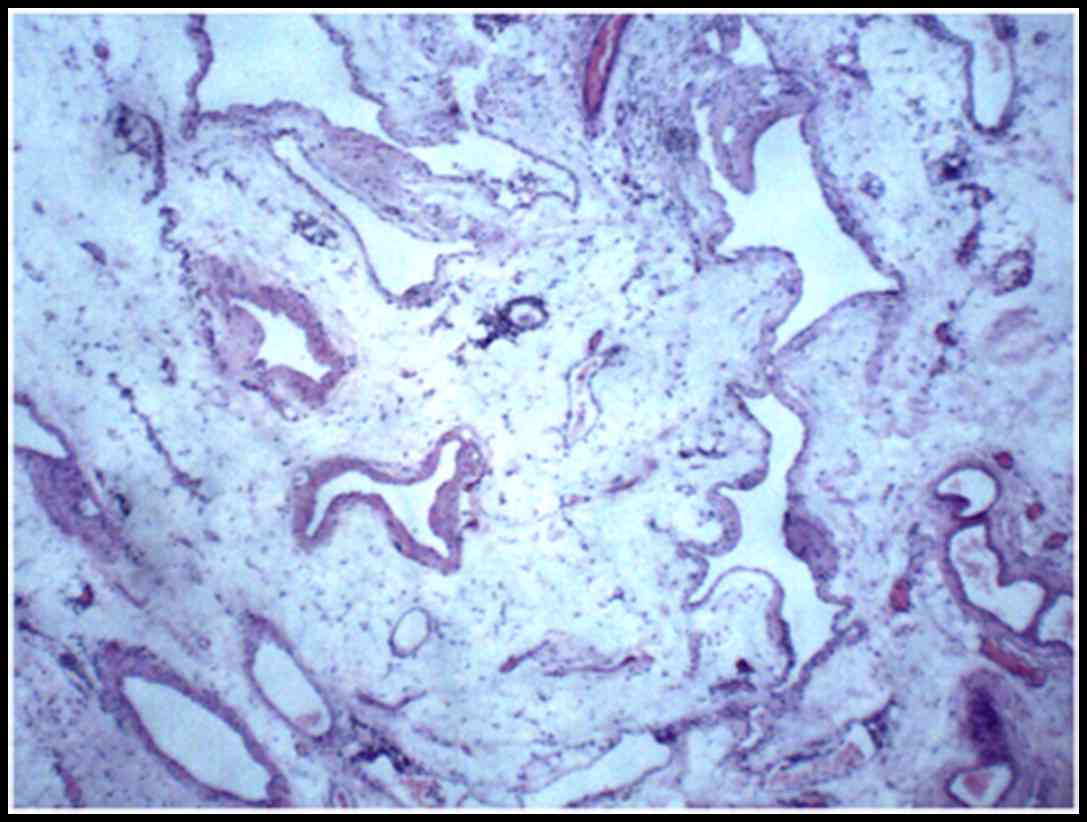
H&E staining of samples from the two surgeries revealed a
diagnosis of hemolymphangioma for the mediastinal mass (Fig. 8) and the spleen nodules (Fig. 9). There was no recurrence at the 15
month follow-up.
Case 4
A 29-year-old female patient was admitted to the
Second Affiliated Hospital of Xi'an Jiaotong University with a mass
on the left forearm that was identified ~8 years prior to
admission. Upon admission, the left forearm exhibited markedly more
swelling compared with its contra-lateral counterpart, with pain
upon pressing. The laboratory findings were normal (blood routine
examination and biochemical examination, including blood glucose
analysis and triglyceride test). An osteosarcoma was initially
considered as a diagnosis.
MRI revealed an irregular mass on the left forearm,
with heterogeneous intensities on T1WI (Fig. 10A) and hyper-intensity on T2WI
(Fig. 10B and C). On fat-suppression
T2WI, multiple small round-like hypo-intensity was observed inside
the tumor (Fig. 10B and C). A
diagnosis of a malignant osteosarcoma with infiltration of the left
ulna was initially considered. The mass was resected and a
grayish-yellow mass was identified in the lateral side of the
proximal left forearm with a size of 2×5×8 cm. Histopathological
features from H&E staining of the mass revealed a
hemolymphangioma (Fig. 11). The
postoperative course was uneventful. The patient was asymptomatic
during a follow-up period of 8 months.
Discussion
Hemolymphangioma is a rare tumor composed of
cystically dilated lymphatic and blood vessels (4). The pathogenesis of this disease remains
unclear. In the majority of cases, the tumor is considered to be a
congenital malformation of the vascular system. The obstruction of
the venolymphatic communication between dysembrioplastic vascular
tissue and the systemic circulation may contribute to the formation
of hemolymphangioma (21). Lymphatic
vessel injury as a result of trauma or surgery results in
inadequate lymph fluid drainage, which is regarded as another cause
of hemolymphangioma (8). In the
present study, five hemolymphangioma lesions across 4 patients are
reported. One of the patients had a history of thyroid surgery,
which may have contributed to the formation of the tumor. The
majority of patients with hemolymphangioma are asymptomatic for a
long period of time and the discomfort typically originates from
the tumor as it grows (22).
Hemolymphangioma can be located at any site of the
body, including the pancreas (1,7,10,21,23–28),
spleen (4,6), waist (5),
duodenum (29), small intestine
(30), rectum (8,12),
gastrointestinal system (31), chest
wall (9), mediastinum (13–18),
extremities (22,32,33), orbit
(34–36), esophagus (37), mouth (38,39), neck
(20), retroperitoneum (40), vertebrae (2), spermatic cord (41), knee (42), colon (43), vulva (44) and testis (45). Nevertheless, multi-focal
hemolymphangioma is rare. Only one previous study has reported on a
female patient with hemolymphangioma in the spleen and
retroperitoneum (3). Of the 4 cases
in the present case report, there was 1 patient who had multifocal
hemolymphangioma in the mediastinum and spleen. This made a
differential diagnosis challenging.
The clinical diagnosis of hemolymphangioma is not a
common occurrence, due to its rarity and the absence of distinctive
symptoms. CT and MRI are useful in defining the extent and the
invasion of the tumor, and planning the surgical strategy.
Hemolymphangioma typically presents as a cystic-solid or solid
tumor. The cystic part may be caused by the rupture and fusion of
the vascular cavity, and the solid part may represent the residual
and compressed vascular tissue (7).
The imaging characteristics depend on the composition of blood
vessels and any accompanying infection or bleeding.
Different sizes of blood vessels in the
hemolymphangioma may produce different enhanced characteristics
upon imaging (1). Significant and
persistent enhancement can be observed in tumors rich in blood
vessels and a septum may show marked enhancement. In the current
case report, the lesions in the mediastinum and spleen in case 3
exhibited progressive enhancement. The imaging findings were
similar to cavernous hemangioma. In case 1, the enhanced cyst wall
suggested that the tumor contained a significant blood vessel
component. Completely cystic hemolymphangioma has rarely been
reported previously (13,14,46). One
distinctive radiographic finding from the present case report is
that the tumors in the first two cases were similar, with cystic
characteristics. In particular, no enhancement was observed on
post-contrast CT images for case 2, which made the diagnosis more
challenging.
MRI can aid in determining the association between
hemolymphangioma and the surrounding tissues, and the extent of
invasion. The tumor in case 4 exhibited heterogeneous iso-intensity
on T1WI and hyper-intensity on T2WI, indicating the presence of a
lower number of tortuous blood vessels and water-based substances
in the lesions. CT and MRI can aid in the selection of surgical
strategy and follow-up treatment. However, a definitive diagnosis
should be based on histological evidence.
The cystic-solid and cystic lesions should be taken
into account during the differential diagnosis of hemolymphangioma,
including lymphangiomas and thymus cysts. Lymphangioma is a rare,
benign lesion derived from a malformation of the lymphatic system,
which is frequently identified in the head, neck and axilla.
Lymphangioma is commonly diagnosed in children <2 years old,
although it may occur at any age (15). Lymphangiomas are typically composed of
cystically dilated lymphatic vessels (47). It is challenging to differentiate
between cystic hemolymphangioma and cystic lymphangioma by imaging
alone, although enhanced CT may aid in distinguishing them. Cystic
lymphangioma is common and is typically observed in infants
(47,48). Combining imaging techniques with
clinical symptoms and pathologic findings may aid in determining
the correct diagnosis.
A cystic mediastinal hemolymphangioma should be
differentiated from a thymus cyst. A thymus cyst is typically
located in the neck and supra anterior mediastinum, and there are
typically no clinical symptoms. The flowing void effect of the
vessel component inside the cyst in case 3 from the present case
report may aid with the diagnosis of hemolymphangioma.
The majority of cases of hemolymphangioma are
diagnosed in female patients. A recent literature review reported
that >2/3 (15/22) reported cases of hemolymphangioma were in
female patients. In the present study, the patients were all
female. However, no direct evidence has been reported for the
gender-associated dominance of hemolymphangioma, to the best of our
knowledge.
Although hemolymphangioma is typically a benign
disease, the recurrence and invasion of adjacent organs has been
reported (24). Complete surgical
resection is considered to be the most effective treatment of the
hemophymphangioma (22,29); however, this needs to be performed
carefully in order to avoid possible haemorrhage due to the
vascular component of hemolymphangioma. Other treatment options
include sclerotherapy, electrocautery, radium implantation,
cyrosurgery and laser therapy. Angiography and embolization can
also be performed in cases of acute bleeding (30). The aim of treatment is to remove the
entire tumor. The majority of cases in the literature had
successful postoperative courses of treatment. Postoperative
follow-up is necessary due to the potential recurrence or
metastasis of the tumor (3). All
cases in the present case reports remained asymptomatic during
postoperative follow-up period.
In conclusion, the current case report describes
five hemolymphangioma lesions in 4 female patients. Completely
cystic and multifocal masses are rare. An accurate diagnosis cannot
typically be established preoperatively despite modern imaging
techniques. The possibility of a hemolymphangioma should be
considered when cystic and cystic-solid masses occur.
References
|
1
|
Pan L, Jian-bo G and Javier PT: CT
findings and clinical features of pancreatic hemolymphangioma: A
case report and review of the literature. Medicine. 94:e4372015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhang Y, Li B, Shi H, Cai L and Hou J:
Vertebral hemangiolymphangioma mimics bone metastases on 99mTc-MDP
SPECT/CT. Clin Nucl Med. 41:76–78. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang DY, Lu Z, Ma X, Wang QY, Sun WL, Wu
W and Cui PY: Multiple hemolymphangioma of the visceral organs: A
case report and review of the literature. Medicine. 94:e11262015.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mei Y, Peng CJ, Chen L, Li XX, Li WN, Shu
DJ and Xie WT: Hemolymphangioma of the spleen: A report of a rare
case. World J Gastroenterol. 21:5442–5444. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li Y, Pang X, Yang H, Gao C and Peng B:
Hemolymphangioma of the waist: A case report and review of the
literature. Oncol Lett. 9:2629–2632. 2015.PubMed/NCBI
|
|
6
|
Zhang Y, Chen XM, Sun DL and Yang C:
Treatment of hemolymphangioma of the spleen by laparoscopic partial
splenectomy: A case report. World J Surg Oncol. 12:602014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dong F, Zheng Y, Wu JJ, Fu YB, Jin K and
Chao M: Hemolymphangioma: A rare differential diagnosis of
cystic-solid or cystic tumors of the pancreas. World J
Gastroenterol. 19:3520–3523. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen G, Cui W, Ji XQ and Du JF: Diffuse
hemolymphangioma of the rectum: A report of a rare case. World J
Gastroenterol. 19:1494–1497. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhang X, Sheng X, Liu F, Jian R, Li L and
Luo R: Hemolymphangioma of the chest wall: A rare case report.
Oncol Lett. 3:816–818. 2012.PubMed/NCBI
|
|
10
|
Balderramo DC, Di Tada C, de Ditter AB and
Mondino JC: Hemolymphangioma of the pancreas: Case report and
review of the literature. Pancreas. 27:197–199. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pandey S, Fan M, Chang D, Zhu J, Zhu Y and
Li Z: Hemolymphangioma of greater omentum: A rare case report.
Medicine. 95:e35082016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pandey S, Fan M, Zhu J, Lu X, Chang D and
Li X: Unusual cause of 55 years of rectal bleeding:
Hemolymphangioma (a case report). Medicine. 96:e62642017.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zehani A, Ayadi-Kaddour A, Cherif J,
Marghli A, Beji M, Kilani T and El Mezni F: Cystic mediastinal
hemolymphangioma. Tunis Med. 90:754–755. 2012.(In French).
PubMed/NCBI
|
|
14
|
Bosdure E, Mates M, Mely L, Guys JM,
Devred P and Dubus JC: Cystic intrathoracic hemolymphangioma: A
rare differential diagnosis of acute bronchiolitis in an infant.
Arch Pediatr. 12:168–172. 2005.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Riquet M, Briere J, Le Pimpec-Barthes F,
Bely N, Dujon A, Velly JF, Brichon PY, Faillon JM, Mouroux J,
Jancovici R and Dahan M: Cystic lymphangioma of the neck and
mediastinum: Are there acquired forms? Report of 37 cases. Rev Mal
Respir. 16:71–79. 1999.PubMed/NCBI
|
|
16
|
Nataf P, Mestiri T, de Lasalle E Martin,
Benomar M, Gandjbakhch I and Cabrol C: Pericardial
hemolymphangioma. Apropos of a case. Arch Mal Coeur Vaiss.
81:1137–1140. 1988.(In French).
|
|
17
|
Contamin C, Denis B, Mallion JM, Rival MA,
Martin-Noel P, Latreille R and Barrie J: Heart hemolymphangioma.
Apropos of a case. Coeur Med Interne. 12:671–678. 1973.PubMed/NCBI
|
|
18
|
Bagolan P, Alati E and Fisicaro M: Some
defects of development of the mediastinum; three cases: One
cavernous hemolymphangioma and two cystic hygromas. Archivio Chir
Torace. 10:559–573. 1953.(In undetermined language). PubMed/NCBI
|
|
19
|
Wu J, Shangguan H, Zhou S and Dong L:
Hemolymphangioma in the posterior mediastinum: A case report and
literature review. Clin Respir J. Mar 7–2016.(Epub ahead of print).
View Article : Google Scholar
|
|
20
|
de Collogny L Gaillard and Delage J:
Cervical hemolymphangioma in a young patient. J Fr Otorhinolaryngol
Audiophonol Chir Maxillofac. 30:469–473. 1981.PubMed/NCBI
|
|
21
|
Figueroa RM, Lopez GJ, Servin TE, Esquinca
MH and Gómez-Pedraza A: Pancreatic hemolymphangioma. JOP.
15:399–402. 2014.PubMed/NCBI
|
|
22
|
Kosmidis I, Vlachou M, Koutroufinis A and
Filiopoulos K: Hemolymphangioma of the lower extremities in
children: Two case reports. J Orthop Surg Res. 5:562010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sun LF, Ye HL, Zhou QY, Ding KF, Qiu PL,
Deng YC, Zhang SZ and Zheng S: A giant hemolymphangioma of the
pancreas in a 20-year-old girl: A report of one case and review of
the literature. World J Surg Oncol. 7:312009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Toyoki Y, Hakamada K, Narumi S, Nara M,
Kudoh D, Ishido K and Sasaki M: A case of invasive hemolymphangioma
of the pancreas. World J Gastroenterol. 14:2932–2944. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Banchini E, Bonati L and Villani LG: A
case of hemolymphangioma of the pancreas. Minerva Chir. 42:807–813.
1987.(In Italian). PubMed/NCBI
|
|
26
|
Montete P, Marmuse JP, Claude R and
Charleux H: Hemolymphangioma of the pancreas. J Chir (Paris).
122:659–663. 1985.(In French). PubMed/NCBI
|
|
27
|
Couinaud C, Jouan Prot, Chalut Favre and
Schneiter: A rare tumor of the head of the pancreas.
(Hemolymphangioma weighing 1,500 kg.). Presse Med. 75:1955–1956.
1967.(In French). PubMed/NCBI
|
|
28
|
Couinaud Jouan, Prot Chalut and Schneiter:
Hemolymphangioma of the head of the pancreas. Mem Acad Chir
(Paris). 92:152–155. 1966.(In French). PubMed/NCBI
|
|
29
|
Antonino A, Gragnano E, Sangiuliano N,
Rosato A, Maglio M and De Palma M: A very rare case of duodenal
hemolymphangioma presenting with iron deficiency anemia. Int J Surg
Case Rep. 5:118–121. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Fang YF, Qiu LF, Du Y, Jiang ZN and Gao M:
Small intestinal hemolymphangioma with bleeding: A case report.
World J Gastroenterol. 18:2145–2146. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kim WT, Lee S and Lee JU: Bleeding gastric
hemolymphangioma: Endoscopic therapy is feasible. Dig Endosc.
25:553–554. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sideri V, Zavras N, Efi T, Niktari G,
Kyrkou I, Kanouras G, MexiBourna P and Fretzayas A: A
hemolymphangioma in the arm and the hand of a neonate. Early Human
Dev. 86:S104–S105. 2010. View Article : Google Scholar
|
|
33
|
Cole DJ, Sood SC and Broomhead IW:
Pulmonary embolism associated with hemolymphangioma of lower
extremity. Plast Reconstr Surg. 63:265–268. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chanfi M: Hemolymphangioma of the orbit in
a young girl: A clinical observation. J Fr Ophtalmol. 27:1047–1049.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ben Chehida F, Chahed N, Turki H, Jeddi A
Hammou, Zitouna MM, Bettaieb A and Gharbi HA: Hemolymphangioma of
the orbit in children. Apropos of a case. Ann Radiol (Paris).
28:626–628. 1985.PubMed/NCBI
|
|
36
|
Guillot M, Dufier JL, Pierre-Kahn A,
Nihoul-Fekete C, Lenoir G and Haye C: Hemolymphangioma of the orbit
in children. Arch Fr Pediatr. 40:401–403. 1983.(In French).
PubMed/NCBI
|
|
37
|
Canavese F, Cortese MG, Proietti L,
Costantino S, Rosina M, Nangeroni M, Defilippi C and Di Rosa GP:
Bulky-pedunculated hemolymphangioma of the esophagus: Rare case in
a two-years old girl. Eur J Pediatr Surg. 6:170–172. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Bureau Y, Delaire J, Barrière H, Litoux P
and Bureau B: Hemolymphangioma of the tongue. Results of surgical
treatment. Bull Soc Fr Dermatol Syphiligr. 73:422–423. 1966.(In
French).
|
|
39
|
Ullik R: On a hemolymphangioma of the
floor of the mouth. Wien Klin Wochenschr. 71:958–960. 1959.(In
German). PubMed/NCBI
|
|
40
|
Kanaitsuka T, Itani K, Shigeta H, Yamamura
Y, Kogawa T, Yoshikawa T, Sugino S, Kanatsuna T, Kondou M,
Takashina K, et al: A case report of giant retroperitoneal
hemolymphangioma. Nihon Naika Gakkai Zasshi. 76:1595–1603. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Rogel-Rodríguez JF, Gil-García JF,
Velasco-García P, Romero-Espinoza F, Zaragoza-Salas T and
Muñoz-Lumbreras G: Hemangiolymphangioma of the spermatic cord in a
17 year-old: A case report. Cir Cir. 84:164–168. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Parra BA, Valencia ZN, Espinal BD and Maya
AI: Low-flow synovial vascular malformation of the knee
(hemangiolymphangioma)-Case report. Rev Chil Pediatr. 86:43–46.
2015.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Castro-Poças F, Lobo L, Amaro T, Soares J
and Saraiva MM: Colon hemangiolymphangioma-a rare case of
subepithelial polyp. Int J Colorectal Dis. 30:989–990. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Sapountzis S, Singhal D and Chen HC:
Radical resection and reconstruction with bilateral gluteal fold
perforator flaps for vulvar hemangiolymphangioma. Int J Gynaecol
Obstet. 121:179–180. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Shin YS, Doo AR, Kim MK, Jeong YB and Kim
HJ: Cavernous hemangiolymphangioma of the testis without cutaneous
hemangiomatosis in an elderly patient. Korean J Urol. 53:810–812.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Gossot D, Decazes JM, Sarfati E and Dubost
C: Cystic hemolymphangioma of the adrenal gland. J Chir (Paris).
124:404–405. 1987.(In French). PubMed/NCBI
|
|
47
|
DI Marco M, Grassi E, Vecchiarelli S,
Durante S, Macchini M and Biasco G: Retroperitoneal lymphangioma: A
report of 2 cases and a review of the literature regarding the
differential diagnoses of retroperitoneal cystic masses. Oncol
Lett. 11:3161–3166. 2016.PubMed/NCBI
|
|
48
|
Yang B, Jiang C, Zhang B, Ren Q, Tang T,
Xu S, Xu H, Yao H, Han Y, Liu S, et al: Giant primary cystic
mediastinal lymphangioma: A case report. Oncol Lett. 8:1246–1248.
2014.PubMed/NCBI
|