Introduction
Bladder cancer (BCa) is the most common cancer of
the urinary tract in the United States (1,2). In China,
BCa is the malignant tumor of the urinary system with the highest
incidence and cancer-associated mortality rate and the incidence of
BCa has been increasing in previous years (3,4).
Approximately 90% of BCa cases are of bladder urothelial carcinoma
(BUC) (5). When initially diagnosed,
the majority of patients with BCa undergo transurethral resection
of the bladder tumor (TURBt) (6);
however, 50–70% of patients with non-muscle invasive BUC experience
disease recurrence following TURBt, 15–25% of whom experience
progression to higher disease grades and stages (7). Early disease diagnosis and surveillance
are necessary to attain better outcomes for patients with BUC
(8). Currently the standard
modalities for detecting BCa are cystoscopy and urine cytology
(8). Cystoscopy is an invasive
procedure with high specificity (8).
Although urine cytology is non-invasive and has high specificity
for detecting carcinoma cells, it lacks sensitivity, particularly
for low-grade tumors (8). Therefore,
it is necessary to find a non-invasive method with high specificity
and sensitivity to improve the diagnosis and surveillance of BUC
(9).
Liquid-based cytology (LBC) has been developed as an
alternative to conventional urine cytology. Previous comparative
studies have shown that LBC is superior to conventional cytology,
as it has a sensitivity and specificity >90% (10–12).
Additionally, complementary techniques, including DNA, RNA and
protein molecular analysis, can be applied to LBC samples, thus
allowing the effect of various cancer biomarkers to also be studied
(13,14).
In the ongoing search for novel bladder tumor
markers, numerous potential markers have been identified; however,
their sensitivity and specificity are not high enough to reduce the
application of cystoscopies for the detection of bladder carcinoma
(9,15). Survivin is a 16.5 kDa protein that
acts as a member of the inhibitor of apoptosis proteins (IAP)
family and is expressed during embryonic and fetal development
(16). Survivin is completely
undetectable in normal adult tissue, but is prominently expressed
in a variety of the most common human cancer types, including those
of the lung, colon, pancreas, prostate and breast (17,18). Owing
to its substantial upregulation in cancer tissue and its function
in carcinogenesis and tumor progression, Survivin is currently
proposed to be a possible tumor marker. In BCa, Survivin expression
has been observed by immunohistochemistry and may be associated
with accelerated incidence of disease recurrence (19). Survivin has been suggested to be a
promising diagnostic marker for BCa detection owing to its high
sensitivity for detection of carcinoma in situ, which is
frequently missed by cystoscopy and by the majority of other tests
(20). Smith et al (21) measured Survivin levels in a group of
138 patients with BCa and reported a sensitivity of 100% and a
specificity of 95%, where as Wang et al (22) reported a sensitivity of 80% and a
specificity of 100% in a group of 66 patients with BCa.
At the time of writing, to the best of our knowledge
no study has been conducted to investigate the diagnostic efficacy
of the combined using of urinary Survivin detection and LBC in the
same patients. This preliminary study was therefore undertaken to
evaluate the diagnostic values of this combined detection method
for BUC.
Patients and methods
Study subjects
Between January 2012 and December 2013, urine
samples from 36 patients with BUC were collected, which were
pathologically confirmed following surgery (27 males, 9 females;
age range, 41–79 years; mean age 57.34±22.20 years). In total, 26
patients had low-grade (grade I/II) disease and 10 had high-grade
(III grade) disease (according to the World Health Organisation
2004 criteria) (23). These patients
were divided into 19 cases of non-muscle-invasive tumor (Ta-T1) and
17 cases of muscle-invasive tumor (T2-T4) using the
Tumor-Node-Metastasis staging system (UICC 2009) (24). In the control group, 36 patients
diagnosed with non-cancerous urinary tract disease were selected
(28 males and 8 females, age range, 40–78 years; 13 cases of benign
prostate hyperplasia, 6 of chronic prostatitis, 8 of urinary tract
stones, 3 of urinary tract infection, 4 of glandular cystitis, 1 of
redundant prepuce and 1 of foreign body of bladder). Fasting
morning urine samples were obtained from all subjects. The present
study was approved by the ethics committee of Jinling Hospital and
each patient provided written informed consent.
Sample collection
Midstream urine samples (40–50 ml) were obtained
from all subjects and were concentrated immediately by
centrifugation at 400 × g for 5 min at room temperature (22±1°C).
The samples were then stored at −80°C until further processing.
ELISA
Survivin protein levels were measured in urine with
Human Survivin ELISA kit (D10564; Jingmei Biotech Co., Ltd.,
Shenzhen, China) according to the manufacturers protocol. The
absorbance was measured using a microplate reader at 570 nm (Model
680 Microplate Reader; Bio-Rad Laboratories, Inc., Hercules, CA,
USA) and the data were recorded. A Survivin concentration that was
2-fold higher than the mean levels of control groups were defined
as positive, as previously described (19).
LBC test
The LBC test was performed using an automated
liquid-based monolayer cell preparation system (ThinPrep 2000
system; Hologic, Inc., Marlborough, MA, USA). The samples were
immersed in Cytolyt (Hologic, Inc., Marlborough, MA, USA) and
transferred to a PreservCyt bowl. The cylinder with a filtration
membrane was then placed in PreservCyt bowl and was rotated to
ensure that the cells were homogeneously distributed. When a vacuum
was applied, the erythrocytes and mucus were removed by negative
pressure. Thus, only the cells left on the filtration membrane were
attached to the slide and then fixed in 95% ethyl alcohol at room
temperature. Following fixation for 30 min, smears of specimens
were cytologically stained using standard Papanicolaou staining as
previously described (25). All
slides were evaluated routinely by an experienced cytopathologist
without any prior knowledge of the immunohistochemical
findings.
Statistical analysis
The results are presented as proportion (%). The
sensitivity, specificity and accuracy were calculated for different
detection method. Comparison of the results were performed by the
χ2 test (SPSS 11.0 for Windows; SPSS, Inc., Chicago, IL,
USA). P<0.05 was considered to indicate a statistically
significant difference.
Results
Survivin level is elevated in the
urine of patients with BUC
The clinical utility of Survivin at discriminating
patients with BUC from individuals with non-cancerous urinary tract
disease was analyzed. Urine samples were categorized according to
histopathological results. Survivin concentrations in individual
urine samples were measured using a commercial ELISA kit. Survivin
levels in the urine of BUC and non-cancerous urinary tract disease
are demonstrated in Table I. Of the
36 BUC cases, 21 were Survivin-positive. In the non-cancerous
urinary tract disease group, only 2 cases were Survivin-positive.
The results revealed that urine Survivin concentrations are
extremely high in the BUC group compared with the controls. The
presence of Survivin was able to discriminate bladder cancer from
benign disease.
 | Table I.Combined sensitivity, specificity and
accuracy for Survivin and LBC in detection of bladder cancer. |
Table I.
Combined sensitivity, specificity and
accuracy for Survivin and LBC in detection of bladder cancer.
| Parameter(s) | Sensitivity, %
(n) | Specificity, %
(n) | Accuracy, % (n) |
|---|
| Survivin | 58.0
(21/36)a | 94.4 (34/36) | 76.4
(55/72)a |
| LBC | 77.8
(28/36)a | 97.2 (35/36) | 87.5
(63/72)a |
| Survivin and
LBC | 91.7
(33/36)a | 91.7 (33/36) | 91.7
(66/72)a |
Most of BUC cases test positive by
LBC
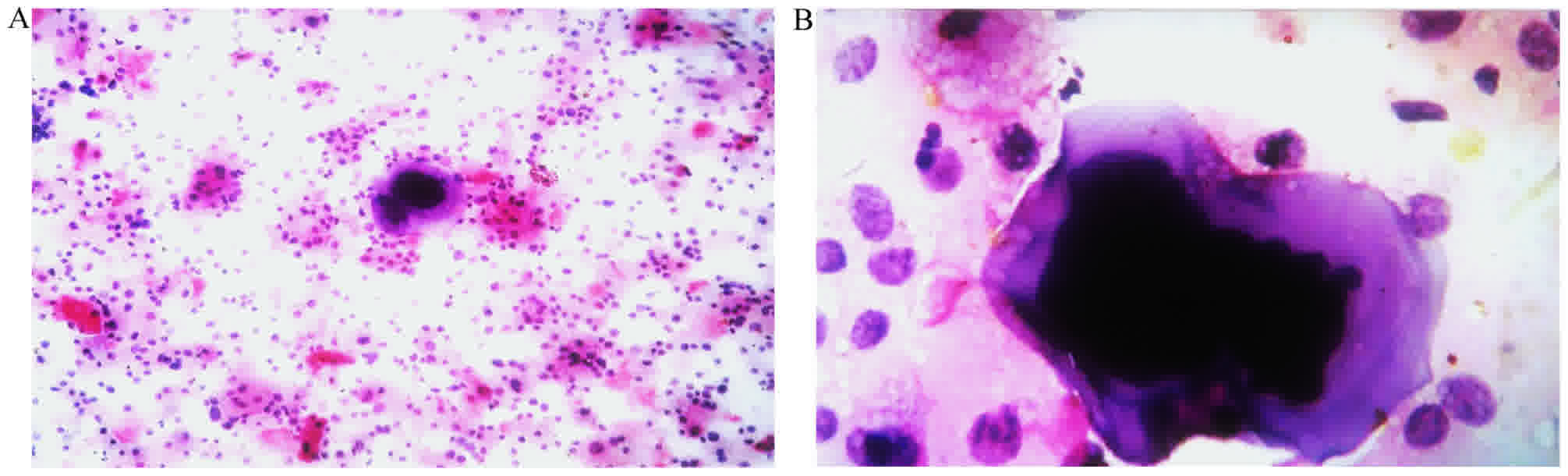
The LBC diagnoses for the 72 cytological samples are
summarized in Table I. The cells were
uniformly distributed on the glass slides in all cases. The LBC
technique provides a clean background with less obscuring
inflammatory cells and blood compared with urine cytology (Fig. 1). Of the 36 cancer cases, 28 were
found to be positive by LBC; of the 36 cases in control group, 1
was suspected to be positive.
The combined use of Survivin detection
and LBC has a significantly increased diagnostic sensitivity and
accuracy
The results for the combined use of Survivin
detection and LBC had also been indicated in the Table I. Of 36 cases in BUC group, 33 were
Survivin- and LBC-positive. Compared with Survivin detection or LBC
alone, the combined detection method had a slightly lower
specificity, but a significantly increased diagnostic sensitivity
and accuracy (P<0.05).
Discussion
An ideal test to monitor BCa should be objective,
non-invasive, easy to administer and interpret, and have high
sensitivity and specificity. An ideal tumor biomarker should be
highly sensitive, specific and accurate (26). Ease of performance and low cost are
also desirable. It has been reported that Survivin and LBC have
utility for the detection of BUC (11,12,16,20,22,26–36).
Urinary levels of Survivin expression at the protein
and mRNA levels are associated with BCa presence, higher tumor
grade, and advanced pathologic stage (16–28).
Survivin protein levels have been detected previously by nested
polymerase chain reaction (nested PCR), immunohistochemical
staining, western blot analysis and ELISA, with the nested PCR most
widely used (21,29,30). Smith
et al (21) were the first to
evaluate the diagnostic potential of Survivin expression in bladder
cancer, using protein and mRNA detection methods. The sensitivity
of Survivin as a biomarker was 100%, with a specificity of 95% in a
group of 138 patients (21). Zhao
et al (29) reported that
molecular beacons detected cancerous cells in 28 (80%) of the 35
patients with confirmed BCa. The Survivin mRNA assay for the
diagnosis of BCa had only 68.6% sensitivity; however, it did have
100% specificity. Chen et al (30) found that Immunohistochemical analysis
indicated high survivin expression was associated with tumor stage
and grade and may present a predictive marker of overall survival
in BUC. Zhao et al (29)
reported that Survivin protein expression was detected in 25
(71.4%) of the 35 patients studied. The sensitivity and specificity
of ELISA was 54.3 and 68.6%, respectively. In summary, Survivin has
been shown to be implicated in the detection of BUC (21,29,30). The
findings indicate that Survivin is a promising urinary molecular
marker for BCa early detection and prognosis prediction (21,29,30).
However, the assays above are non-standardized, as none of their
performances complied with validation criteria appropriate for
analytic techniques and the assays require further innovation and
standardization. Eissa et al (19) reported that qualitative reverse
transcription-PCR in 153 samples revealed that the mean rank levels
of survivin in the benign and malignant groups were significantly
increased by 1.1 and 2.23-fold, respectively, vs. the normal group
(P<0.0001). In the present study, Survivin levels over 2 times
of mean value in control group for the sample were defined as
positive. Applying this cutoff value, the sensitivity and
specificity of urinary survivin was 58.0 and 94.4%,
respectively.
Urine cytology, as a diagnosis method, has a
reasonable sensitivity for the detection of high-grade urothelial
carcinoma (UC); however, it is less sensitive for detecting
low-grade tumors (31).
LBC have been regarded as an alternative to
conventional cytology for the primary screening of BCa owing to its
practical advantages, with variable circumstances. The advantages
of LBC include: samples have a ‘cleaner’ background, devoid of
blood, mucus and inflammatory cells; LBC uses automated and
standardized processing techniques that produces the homogenous
distribution and efficient fixation of cells; and the residual
biological material can be used for immunohistochemical or other
special analyses (32–34). Several previous reports have
demonstrated that LBC is superior to conventional cytology for the
identification of BCa (11,35,36). LBC
has a sensitivity and specificity >90% in non-gynecological
specimens (12). The present study
revealed LBC had a sensitivity of 77.8% and specificity of
97.2%.
To the best of our knowledge, the present study is
the first to investigate the diagnostic activity of Survivin and
LBC in the same patients with BUC. The results indicated that
combined use of urine Survivin and LBC test could significantly
improve the diagnosis of BUC. In the present study, the efficacy of
this combined test was investigated, which exhibited a sensitivity
of 91.7%, specificity of 91.7% and accuracy of 91.7%. Compared with
the results of the individual tests, the specificity was decreased,
but the sensitivity and accuracy improved significantly. More
importantly, this method is non-invasive, economical, simple and
precise. Therefore, in future LBC could be used in combination with
Survivin detection for more accurate results in the diagnosis of
BUC. The research discussed in the current study is limited owing
to the small number of samples. Further investigation is therefore
required, with a study involving a large number of patients.
Acknowledgements
Not applicable.
Funding
This work was supported by the grants from the
National Natural Science Foundation of China (No. 81572526;
30901716).
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
WC had full access to all the data in the study and
takes responsibility for the integrity of the data and the accuracy
of the data analysis. Study concept and design: WC. Acquisition of
data: WC, XX, PL, DF, ZW and SX. Analysis and interpretation of
data: WC, XX, PL, ZYZ and JG. Drafting of the manuscript: XX.
Critical revision of the manuscript for important intellectual
content: WC, XX and PL. Statistical analysis: FX, FT. Supervision:
ZYZ and JG.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Jinling Hospital (Nanjing, China) and all patients
provided written informed consent.
Consent for publication
All patients provided written informed consent for
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jacobs BL, Lee CT and Montie JE: Bladder
cancer in 2010: How far have we come? CA Cancer J Clin. 60:244–272.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Parkin MD, Bray F, Ferlay J and Pisani P:
Global cancer statistics, 2002. CA Cancer J Clin. 55:74–108. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sujun H, Siwei Z, Wanqing C and Chang-Ling
L: Analysis of the status and trends of bladder cancer incidence in
China. Oncol Prog. 11:89–95. 2013.
|
|
5
|
Fleshner NE, Herr HW, Stewart AK, Murphy
GP, Mettlin C and Menck HR: The national cancer data base report on
bladder carcinoma. The American college of surgeons commission on
cancer and the american cancer society. Cancer. 78:1505–1513. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Richterstetter M, Wullich B, Amann K,
Haeberle L, Engehausen DG, Goebell PJ and Krause FS: The value of
extended transurethral resection of bladder tumour (TURBT) in the
treatment of bladder cancer. BJU Int. 110:E76–E79. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Brausi M, Collette L, Kurth K, van der
Meijden AP, Oosterlinck W, Witjes JA, Newling D, Bouffioux C and
Sylvester RJ: EORTC Genito-Urinary Tract Cancer Collaborative
Group: Variability in the recurrence rate at first follow-up
cystoscopy after TUR in stage Ta T1 transitional cell carcinoma of
the bladder: A combined analysis of seven EORTC studies. Eur Urol.
41:523–531. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schmitz-Dräger BJ, Droller M, Lokeshwar
VB, Lotan Y, Hudson MA, van Rhijn BW, Marberger MJ, Fradet Y,
Hemstreet GP, Malmstrom PU, et al: Molecular markers for bladder
cancer screening, early diagnosis and surveillance: The WHO/ICUD
consensus. Urol Int. 94:1–24. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Goebell PJ, Groshen SL and Schmitz-Dräger
BJ: Guidelines for development of diagnostic markers in bladder
cancer. World J Urol. 26:5–11. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nicol TL, Kelly D, Reynolds L and
Rosenthal DL: Comparison of TriPath thin-layer technology with
conventional methods on non-gynecologic specimens. Acta Cytol.
444:567–575. 2000. View Article : Google Scholar
|
|
11
|
Bishop JW, Bigner SH, Colgan TJ, Husain M,
Howell LP, McIntosh KM, Taylor DA and Sadeghi MH: Multicenter
masked evaluation of AutoCyte PREP thin layers with matched
conventional smears. Including initial biopsy results. Acta Cytol.
42:189–197. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nasuti JF, Tam D and Gupta PK: Diagnostic
value of liquid based (ThinPrep) preparation in non-gynecologic
cases. Diagn Cytopathol. 24:137–141. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tisserand P, Fouquet C, Marck V, Mallard
C, Fabre M, Vielh P and Soussi T: Thinprep-processed fine-needle
samples of breast are effective material for RNA- and DNA-based
molecular diagnosis. Application to p53 mutation analysis. Cancer.
99:223–232. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Linder J: Recent advances in thin-layer
cytology. Diagn Cytopathol. 18:24–32. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Weikert S, Christoph F, Schrader M, Krause
H, Miller K and Müller M: Quantitative analysis of survivin mRNA
expression in urine and tumour tissue of bladder cancer patients
and its potential relevance for disease detection and prognosis.
Int J Cancer. 116:100–104. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Horstmann M, Bontrup H, Hennenlotter J,
Taeger D, Weber A, Pesch B, Feil G, Patschan O, Johnen G, Stenzl A
and Brüning T: Clinical experience with survivin as a biomarker for
urothelial bladder cancer. World J Urol. 28:399–404. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Adida C, Crotty PL, McGrath J, Berrebi D,
Diebold J and Altieri DC: Developmentally regulated expression of
the novel cancer anti-apoptosis gene survivin in human and mouse
differentiation. Am J Pathol. 152:43–49. 1998.PubMed/NCBI
|
|
18
|
Tanaka K, Iwamoto S, Gon G, Nohara T,
Iwamoto M and Tanigawa N: Expression of survivin and its
relationship to loss of apoptosis in breast carcinomas. Clin Cancer
Res. 6:127–134. 2000.PubMed/NCBI
|
|
19
|
Eissa S, Swellam M, Shehata H, El-Khouly
IM, El-Zayat T and El-Ahmady O: Expression of HYAL1 and survivin
RNA as diagnostic molecular markers for bladder cancer. J Urol.
183:493–498. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ku JH, Godoy G, Amiel GE and Lerner SP:
Urine survivin as a diagnostic biomarker for bladder cancer: A
systematic review. BJU Int. 110:630–636. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Smith SD, Wheeler MA, Plescia J, Colberg
JW, Weiss RM and Altieri DC: Urine detection of survivin and
diagnosis of bladder cancer. JAMA. 285:324–328. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang H, Xi X, Kong X, Huang G and Ge G:
The expression and significance of survivin mRNA in urinary bladder
carcinomas. J Cancer Res Clin Oncol. 130:487–490. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Eble JN, Sauter G, Epstein JI and
Sesterhenn IA: World Health Organization Classification of
TumoursPathology and Genetics of Tumours of the Urinary System and
Male Genital Organs. IARC Press; Lyon: 2004
|
|
24
|
Sobin LH, Gospodariwicz M and Wittekind C:
International Union against Cancer: TNM classification of malignant
tumours2009, UICC international union against cancer. 7th edition.
Wiley-Blackwell; Hoboken, NJ: pp. 262–265. 2009
|
|
25
|
Gurley AM, Hidvegi DF, Bacus JW and Bacus
SS: Comparison of the papanicolaou and feulgen staining methods for
DNA quantification by image analysis. Cytometry. 11:468–474. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Goodison S, Rosser CJ and Urquidi V:
Bladder cancer detection and monitoring: Assessment of urine- and
blood-based marker tests. Mol Diagn Ther. 17:71–84. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Pina-Cabral L, Santos L, Mesquita B, Amaro
T, Magalhães S and Criado B: Detection of survivin mRNA in urine of
patients with superficial urothelial cell carcinomas. Clin Transl
Oncol. 9:731–736. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Srivastava AK, Singh PK, Srivastava K,
Singh D, Dalela D, Rath SK, Goel MM and Bhatt Brahma ML: Diagnostic
role of survivin in urinary bladder cancer. Asian Pac J Cancer
Prev. 14:81–85. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhao J, Wang ZQ, Wang XY, Yang XJ and He
D: Preliminary study of diagnostic utility of molecular beacons in
bladder cancer. Urology. 76:512.e8–e13. 2010. View Article : Google Scholar
|
|
30
|
Chen HA, Su CM, Hsieh HY, Tung CL, Hsu CD,
Wang YH and Shen CH: Clinical significance of survivin expression
in patients with urothelial carcinoma. Dis Markers.
2014:5749852014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wiener HG, Mian C, Hiatel A, Pycha A,
Schatzl G and Marberger M: Can urine bound diagnostic tests replace
cystoscopy in the management of bladder cancer? J Urol.
159:1876–1880. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lu DY, Nassar A and Siddiqui MT:
High-grade urothelial carcinoma: Comparison of SurePath
liquid-based processing with cytospin processing. Diagn Cytopathol.
37:16–20. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
33
|
Koo JH, Lee HC, Song HG, Han HS, Lee KH,
Choe KH, Lee KM and Lee OJ: Comparison of cytologic evaluation
between conventional method and Cellprep PLUS liquid-based cytology
in body fluid. Korean J Pathol. 43:448–452. 2009. View Article : Google Scholar
|
|
34
|
Son SM, Koo JH, Choi SY, Lee HC, Lee YM,
Song HG, Hwang HK, Han HS, Yun SJ, Kim WJ, et al: Evaluation of
urine cytology in urothelial carcinoma patients: A comparison of
cellprepPlus® Liquid-Based cytology and conventional
smear. Korean J Pathol. 46:68–74. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Nicol TL, Kelly D, Reynolds L and
Rosenthal DL: Comparison of TriPath thin-layer technology with
conventional methods on non-gynecologic specimens. Acta Cytol.
44:567–575. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Fischler DF and Toddy SM: Nongynecologic
cytology utilizing the Thin-Prep Processor. Acta Cytol. 40:669–675.
1996. View Article : Google Scholar : PubMed/NCBI
|