Introduction
Up to now, radiotherapy still the main treatment for
f patients with intermediate or advanced lung cancer or patient who
cannot tolerate surgical treatments (1). Vascular endothelial growth factor
(VEGF), as the strongest pro-angiogenic factor, can increase
vascular permeability, provide nutrients for growth of tumor cells
and promote development of tumor (2).
In the body, matrix metalloproteinases (MMPs) can degrade
extracellular matrix as well as major components of basement
membrane, and participate in inflammatory responses (2), atherosclerosis (3), tumor infiltration and metastasis
(4) and many other physiological and
pathological processes. In this study, enzyme-linked immunosorbent
assay (ELISA) was performed to detect VEGF and MMP-9 levels in
peripheral blood; reverse transcription-quantitative polymerase
chain reaction (RT-qPCR) was used to detect the expression of
related genes at messenger RNA (mRNA) level; gelatin zymography was
applied to measure the activity of serum MMP-9. Finally, the
feasibility of the application as indicators for the evaluation of
efficacy of radiotherapy in the treatment of intermediate and
advanced lung cancer were discussed.
Materials and methods
General information
A total of 77 patients who were diagnosed with
non-small cell lung cancer in the intermediate or advanced stage in
Tianjin Fifth Central Hospital (Tianjin, China) from February 2016
to February 2017 were selected as experimental group. The inclusion
criteria were: i) Patients with non-small cell lung cancer
confirmed with pathologic examination; ii) patients with measurable
tumor lesions and without surgery indications; iii) patients with
the disease in intermediate or advanced stage, namely, with a
tumor-node-metastasis (TNM) stage of III–IV; iv) patients with a
survival time >3 months; and v) patients without radiotherapy
contraindications as well as hematological system and autoimmune
diseases but were normal in blood routine tests and with normal
hepatic or renal functions. Among those patients, 53 were males and
24 were females, and the mean age was 55.24±8.83 years old. A total
of 19 healthy (12 males and 7 females) people were selected at the
same time to serve as control group, and the mean age was
56.15±6.94 years old. There were no significant differences in
gender, age and other basic data between controls and patients
(P>0.05). This experiment was approved by the Ethics Committee
of the Tianjin Fifth Central Hospital, and informed consent was
signed by all the patients and their families.
Experimental reagents and
instruments
ELISA kits for human VEGF and MMP-9 (Beijing KERUI
MEI Technology Co., Ltd., Beijing, China); gelatin zymography kits
(BestBio, Shanghai, China); RT kit (Shenzhen Abaier Biotech Co.,
Ltd., Shenzhen, China); gelatin zymography kits (Shanghai Xinfan
Biotech Co., Ltd., Shanghai, China); automatic microplate reader
(Shanghai Utrao Medical Instrument Co., Ltd., Shanghai, China);
centrifuge (Thermo Fisher Scientific, Inc., Waltham, MA, USA);
pipette (Eppendorf, Hamburg, Germany).
Experimental methods
Radiotherapy
Computed tomography (CT) simulation was applied to
measure gross tumor volume (GTV) and organs at risk; GTV was
equably expanded by 6–8 mm to obtain a clinical target volume which
was further expanded flatly by 5 mm and vertically by 10 mm to make
a planning target volume (PTV); then the expanded PTV was modified
appropriately if it included the spinal cord tissues.
Simultaneously integrated boost technology (SIB) was utilized, with
a prescribed dose of PTV (50–66 Gy), which was given at a dose of
1.8–2.0 Gy/day for 5 days/week and 25 times (a course of
treatment). All patients received a course of treatment with
radiotherapy.
Detection of expression levels of
serum VEGF and MMP-9
Peripheral blood samples were collected from each
patient at 1 day before and 1 day after treatment; expression
levels of serum VEGF and MMP-9 were detected according to the
instructions of the kit. Antigens were properly diluted with
coating buffer to make final concentration of 10 mg/ml; 100 µl
solution was added into each well and incubated at 37°C for 1 h;
then the plate was placed in a refrigerator at 4°C overnight. Then
liquid was removed and washing was performed 3 times using 200 µl
washing solution each time; finally, plate was inverted and the
liquid was removed using absorbent paper. Then, 200 µl blocking
buffer was added and placed at 37°C for 1 h. Serum samples to be
detected were diluted with a ratio of 1:1,000, 1:2,000, 1:4,000,
1:6,000, 1:8,000, 1:10,000, 1:20,000, 1:40,000 and 1:80,000,
respectively, and 100 µl of diluted serum sample was added into
each well. Meanwhile, control samples were also diluted, and
negative control was diluted with a ratio of t 1:1,000. After
incubation at 37°C for 2 h. 100 µl of horseradish
peroxidase-labeled goat-anti-mouse immunoglobulin G (IgG) was added
into each well, followed by incubation at 37°C for 1 h. After that,
washing was performed twice using double-distilled H2O
(ddH2O). Then 100 µl of 3,3′,5,5′-tetramethylbenzidine
(TMB) application solution was added into each well and kept in
dark for 10–20 min until blue staining appeared. Then, 50 µl of
stop buffer was added into each well and incubated for 3–5 min.
Enzyme-linked immunometric meter was used to measure the OD value
at the wavelength of 490 nm. Standard curves were constructed to
calculate the contents of serum VEGF and MMP-9.
Response evaluation and observation
indexes
CT was performed before and after radiotherapy to
evaluate the efficacies of the radiotherapy at 1, 3 and 5 weeks
after treatment; short-term efficacy on intermediate and advanced
lung cancer was evaluated according to Response Evaluation Criteria
in Solid Tumors (RECIST) (5), which
was characterized by the tumor size measured via double-path
product method. Changes in tumor size before and after the
treatment were compared. Efficacy was mainly divided into 4 levels,
namely, complete remission (CR), partial remission (PR), stable
disease (SD) and progressive disease (PD); CR+PR represented
effective treatment and SD+PD represented PD.
Detection of MMP-9 activity
In this study, gelatin zymography kit was utilized
to detect MMP-9 activity in peripheral blood serum. Frozen serum
was placed at room temperature for equilibrium; 20 µl serum was
mixed with 20 µl loading buffer through vortex oscillation. Then,
the mixture was subjected to 10% acrylamide gel electrophoresis.
After staining and washing, white bands appeared. Optical density
value of the white band indicated enzyme activity.
Detection of mRNA expressions via
RT-qPCR
Primers were synthesized by FamilyLab International
Biological Technology Institute Ltd. (Beijing, China), the primer
sequences were listed in Table I.
Total RNA in serum was extracted according to the instructions of
RNA extraction kit, and the complementary DNA (cDNA) was
synthesized using RT kit.
 | Table I.Primer sequences. |
Table I.
Primer sequences.
| Gene | Primer |
|---|
| MMP-9 | F:
5′-AAGGATGGTCTACTGGCAC-3′ |
|
| R:
5′-TCAGAACCGACCCTACAA-3′ |
| VEGF | F:
5′-TCGGGCCTCCGAAACCATGA-3′ |
|
| R:
5′-CCTGGAGAGAGATCTGGTTC-3′ |
| GAPDH | F:
5′-TGGGTGTGAACCACGAGAA-3′ |
|
| R:
5′-GGCATGGACTGTGGTCATGA-3′ |
20 µl RT system: 4 µl 5X PrimeScript Buffer, 1 µl
Random 6 mers (100 µM), 1 µl Oligo dT Primer (50 µM), 1 µl
PrimeScipt RT Enzyme Mix, 3 µl total RNA and 10 µl ribonuclease
(RNase) Free dH2O. Reaction conditions for RT: 37°C for
15 min and 85°C for 5 sec.
25 µl PCR system: 12.5 µl SYBR Premix Ex Taq™ II, 1
µl forward primer, 1 µl reverse primer, 2 µl cDNA and 8.5 µl
dH2O. Reaction conditions: pre-denaturation at 94°C for
3 min, followed by 40 cycles of denaturation at 94°C for 20 sec,
annealing at 58°C for 20 sec and extension at 72°C for 30 sec. With
GAPDH asendogenous control, relative expression levels of MMP-9 and
VEGF mRNAs were automatically calculated using by RT-qPCR
instrument.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
17.0 software (Beijing Xinmei Jiahong Technology Co., Ltd.,
Beijing, China) was used for all statistical analyses. Measurement
data were expressed as mean ± standard deviation; t-test was used
for comparisons between two groups, paired t-test was performed for
intragroup comparisons, and one-way analysis of variance (ANOVA)
was used for comparisons among multiple groups followed by the SNK
post hoc test. Count data were processed using χ2 test,
and α=0.05 was regarded as the statistical standard.
Results
Comparisons of serum level of VEGF and
MMP-9 between two groups
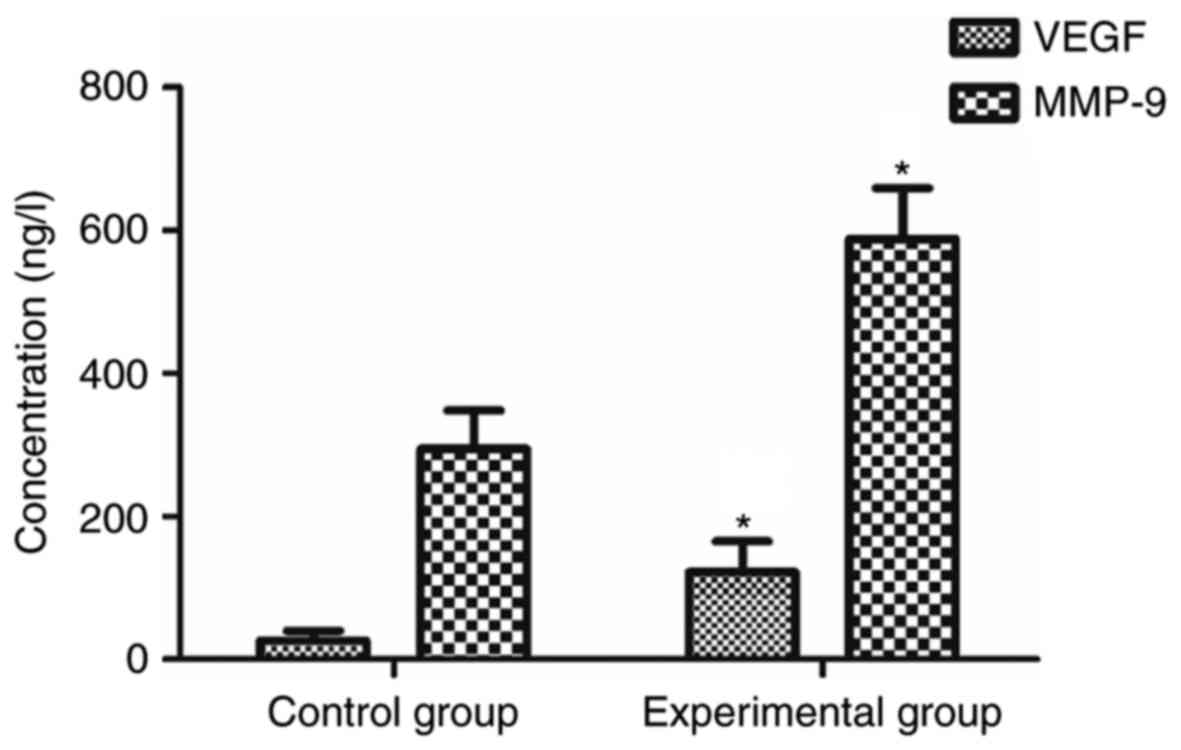
Results of ELISA showed that, compared with normal
control group, significantly higher levels of VEGF and MMP-9 were
found in experimental group (P<0.05; Fig. 1).
Correlation between serum level of
VEGF and MMP-9 and efficacy in experimental group
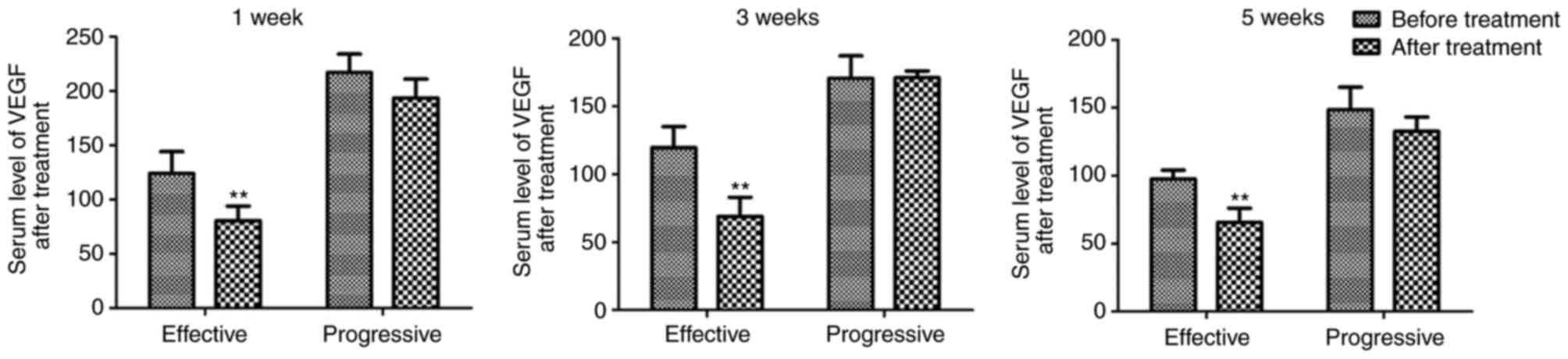
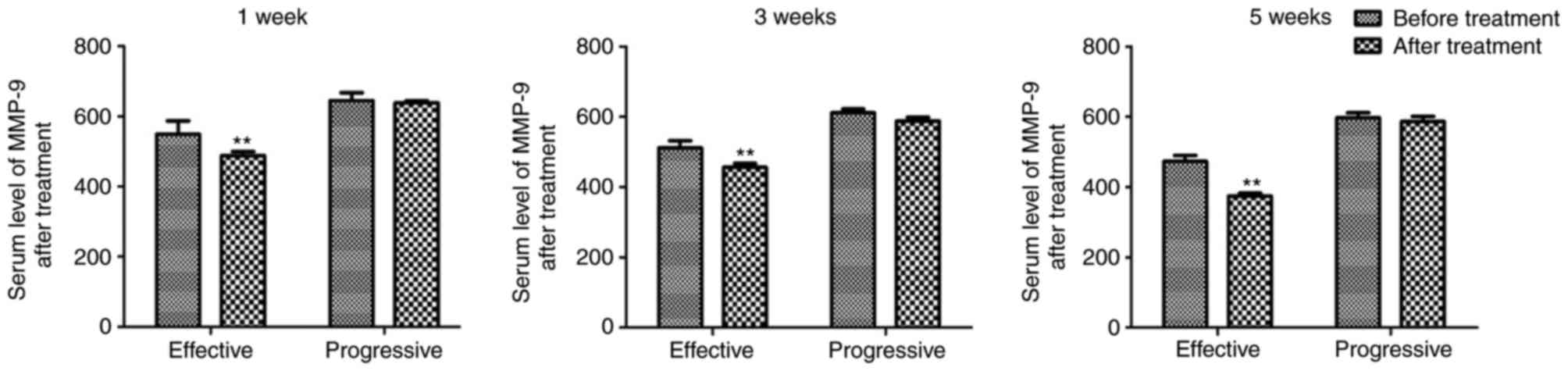
According to the efficacy evaluation after
treatment, there were 19 cases of CR, 35 cases of PR, 16 cases of
SD and 7 cases of PD; the effective rate of treatment (CR+PR) was
70.1%. Serum levels of VEGF and MMP-9 in patients of effective
treatment group were significantly lower than those before
treatment at 1, 3 and 5 weeks after treatment (P<0.05). For
patients with tumors in advanced stage, namely, patients in SD+PD
stage, there were no notable changes in the serum VEGF and MMP-9
levels after radiotherapy (Figs. 2
and 3).
Correlation of radiotherapy efficacy
with serum VEGF and MMP-9 before and after treatment
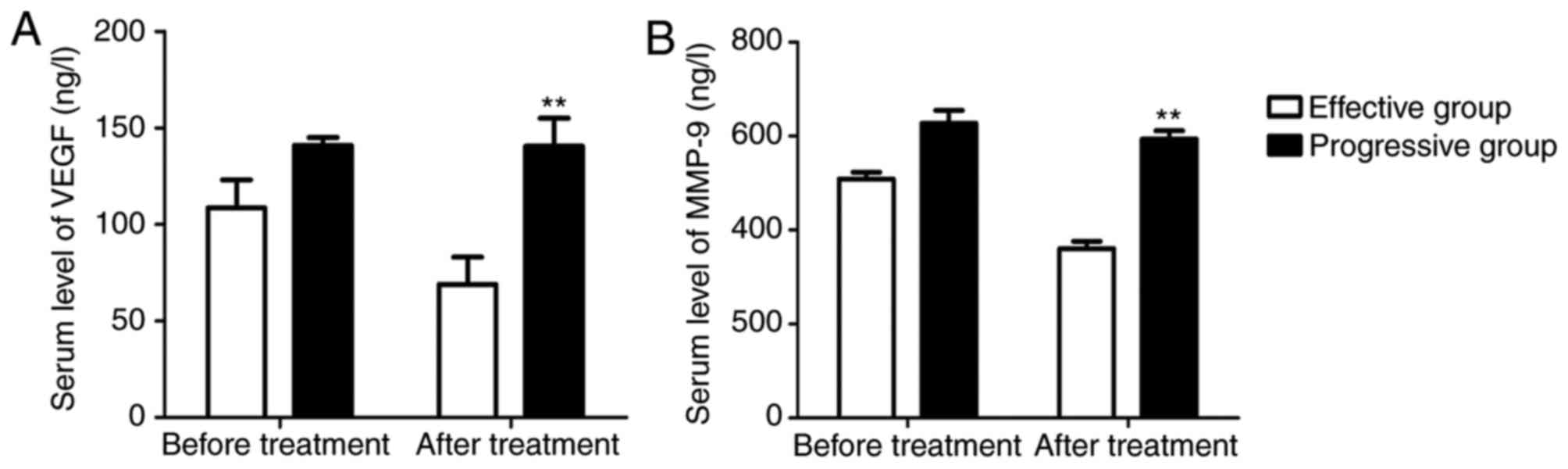
Before radiotherapy, serum VEGF level of the
patients in effective group was 94.13±38.35 ng/l, and that in
progressive group was 138.22±45.05 ng/l, there was no statistically
significant difference between those two groups (P>0.05). After
radiotherapy, serum VEGF level of the patients in effective group
was 50.28±33.17 ng/l, while that in progressive group was
127.36±52.84 ng/l, the difference between the two groups was
statistically significant (P<0.05; Fig. 4A).
Before radiotherapy, serum MMP-9 level of the
patients in effective group was 495.05±81.17 ng/l, and that in
progressive group was 601.53±70.05 ng/l, there was no statistically
significant difference between two groups (P>0.05). After
radiotherapy, serum MMP-9 level of the patients in effective group
was 340.25±68.93 ng/l, while that in progressive group was
579.95±82.24 ng/l, the difference between the two groups was
statistically significant (P<0.05; Fig. 4B).
MMP-9 activity in peripheral blood
serum
Compared with control group, significantly higher
MMP-9 activity was detected in patients both before and after
treatment (P<0.05). MMP-9 activity after treatment was
significantly lower than that before treatment (P<0.05; Table II).
 | Table II.Comparisons of MMP-9 activity in
peripheral blood serum (mean ± standard deviation). |
Table II.
Comparisons of MMP-9 activity in
peripheral blood serum (mean ± standard deviation).
|
|
| Net optical
density |
|
|
|---|
|
|
|
|
|
|
|---|
| Group | Case (n) | Effective | Progressive | t | P |
|---|
| Control group | 19 | 2.83±0.76 |
| −3.617 | <0.05 |
| Before treatment | 77 | 25.56±5.28 | 27.02±5.74 |
|
|
| After treatment | 77 | 14.92±3.88 | 24.03±4.95 |
|
|
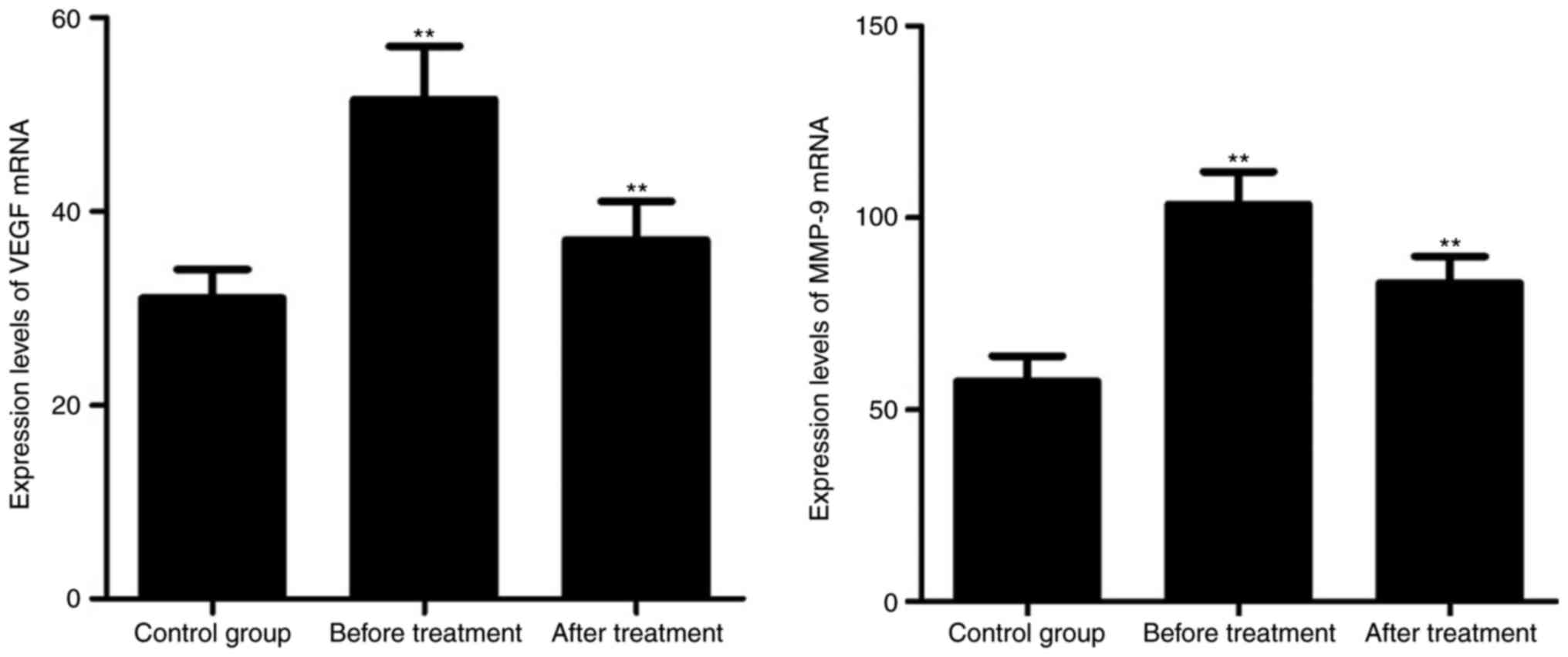
VEGF and MMP-9 mRNA expressions
Compared with control group, significantly higher
expression levels of VEGF and MMP-9 mRNAs were detected in patients
both before and after treatment (P<0.05). Expression levels of
VEGF and MMP-9 after treatment were significantly lower than those
before treatment (P<0.05; Fig.
5).
Discussion
With the increased severity of air pollution,
incidence rate of lung cancer is increasing year by year (6). More than 70% of the lung cancer patients
were diagnosed at intermediate and advanced stage (7). As one of the major methods in the
treatment of intermediate and advanced lung cancer, radiotherapy
can effectively kill tumor cells and prolong the patients' survival
time (8).
VEGF has multiple biological effects in the human
body. VEGF expression is significantly up-regulated in tumor cells,
and the expression level is closely related to the infiltration,
metastasis and prognosis of the tumor cells (9). Under hypoxia, VEGF expression is
up-regulated. After binding to its receptors, VEGF can accelerate
endothelial cell division, increase production of blood vessels and
lymphatic vessels, so as to promote growth, infiltration and
metastasis the tumor cells (10–12). In
recent years, VEGF has become a new target for the inhibition of
tumor vascularization (13). Some
studies have shown that expression levels of VEGF, carcinoembryonic
antigen (CEA) and neuron-specific enolase (NSE) in the serum were
positively correlated with cancer stage (14). MMP-9 is a member of the MMP family. It
was reported that MMP-9 and tissue inhibitor of metalloproteinases
1 (TIMP1) were highly expressed in serum of lung cancer patients
compared with normal healthy people (15). Expression levels of MMP-9 and TIMP1 in
stages III and IV were obviously higher than those in stages I and
II, indicating that expressions levels of TIMP1 and MMP-9 in the
serum were closely correlated with the occurrence and development
of lung cancer (16). Some studies
have revealed that MMP-9 plays an important role in the occurrence
and development of tumor infiltration and metastasis (17), possibly due to the positive
correlation between expression of VEGF and MMP-9 in tumor cells. In
addition, MMP-9 can interact with connective tissue growth factor
to inhibit its binding to VEGF receptors, as a result, more VEGF
will be released, and the formation of tumor neovascularization
will be promoted (18).
In this study, ELISA was used to detect the VEGF and
MMP-9 levels in the peripheral blood, enzyme activity test was
performed, and RT-qPCR method were applied to measure mRNA
expressions. Results showed that the overall response rate of
radiotherapy on intermediate and advanced lung cancer reached
70.1%. Levels of serum VEGF and MMP-9 in effective treatment group
were obviously lower than those before treatment (P<0.05);
meanwhile, expression levels of VEGF and MMP-9 in effective
radiotherapy group were obviously lower than those in progressive
group (P<0.05). MMP-9 activity before treatment was remarkably
higher than that after treatment (P<0.05). Expression levels of
VEGF and MMP-9 mRNA before treatment were evidently elevated
compared with those after treatment (P<0.05). Our finding were
consistent with the role of MMP-9 in lung cancer reported by
previous studies (19,20). Our study further proved that VEGF and
MMP-9 can be used as indicators for the evaluation of efficacy of
radiotherapy in the treatment of intermediate and advanced lung
cancer (21). However, our study is
still limited by the small sample size. Further studies with bigger
sample size are needed to confirm the conclusions in this
study.
In conclusion, VEGF and MMP-9 expression levels in
intermediate and advanced lung cancer decreased significantly after
radiotherapy. Detection of serum VEGF and MMP-9 expressions can be
used as novel indicators for the evaluation of efficacy of
radiotherapy in the treatment of intermediate and advanced lung
cancer.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GD and YL analyzed and interpreted the patient data.
GD wrote the manuscript. CL collected the patient data and revised
the manuscript for important intellectual content. GD and CL
contributed to the conception and design of the study. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the ethics committee of
the Tianjin Fifth Central Hospital. Patients who participated in
this research, signed the informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hayano K, Kulkarni NM, Duda DG, Heist RS
and Sahani DV: Exploration of imaging biomarkers for predicting
survival of patients with advanced non-small cell lung cancer
treated with antiangiogenic chemotherapy. AJR Am J Roentgenol.
206:987–993. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kim A, Im M, Yim NH and Ma JY: Reduction
of metastatic and angiogenic potency of malignant cancer by
Eupatorium fortunei via suppression of MMP-9 activity and VEGF
production. Sci Rep. 4:69942014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cai J, Li R, Xu X, Zhang L, Wu S, Yang T,
Fang L, Wu J, Zhu X, Li M and Huang Y: URGCP promotes non-small
cell lung cancer invasiveness by activating the NF-κB-MMP-9
pathway. Oncotarget. 6:36489–36504. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu F and Zhu L: Expression of adiponectin
in non-small cell lung cancer and its relationship with MMP-9 and
angiogenesis. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 40:579–584.
2015.(In Chinese). PubMed/NCBI
|
|
5
|
Lin X, Li HR, Lin XF, Yu ME, Tu XW, Hua
ZD, Lin M, Xu NL, Han LL and Chen YS: Silencing of Livin inhibits
tumorigenesis and metastasis via VEGF and MMPs pathway in lung
cancer. Int J Oncol. 47:657–667. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
El-Badrawy MK, Yousef AM, Shaalan D and
Elsamanoudy AZ: Matrix metalloproteinase-9 expression in lung
cancer patients and its relation to serum mmp-9 activity,
pathologic type, and prognosis. J Bronchology Interv Pulmonol.
21:327–334. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ramanujum R, Lin YL, Liu JK and He S:
Regulatory expression of MMP-8/MMP-9 and inhibition of
proliferation, migration and invasion in human lung cancer A549
cells in the presence of HGF variants. Kaohsiung J Med Sci.
29:530–539. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Matsumoto Y, Zhang Q, Akita K, Nakada H,
Hamamura K, Tsuchida A, Okajima T and Furukawa K, Urano T and
Furukawa K: Trimeric Tn antigen on syndecan 1 produced by
ppGalNAc-T13 enhances cancer metastasis via a complex formation
with integrin α5β1 and matrix metalloproteinase 9. J Biol Chem.
288:24264–24276. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Xu T, Xu Y, Huo J, Yang P, Gomez DR and
Liao Z: Incidental use of beta-blockers, serum VEGF, and their
association with disease outcome in patients with non-small-cell
lung cancer treated with definitive chemoradiation therapy. Int J
Radiat Oncol Biol Phys. 98:2452017. View Article : Google Scholar
|
|
10
|
Zhang H, Yun S, Batuwangala TD, Steward M,
Holmes SD, Pan L, Tighiouart M, Shin HJ, Koenig L, Park W, et al: A
dual-targeting antibody against EGFR-VEGF for lung and head and
neck cancer treatment. Int J Cancer. 131:956–969. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zheng H and Liu JF: Studies on the
relationship between P13K/AKT signal pathway-mediated MMP-9 gene
and lung cancer. Eur Rev Med Pharmacol Sci. 21:753–759.
2017.PubMed/NCBI
|
|
12
|
Farhat FS, Tfayli A, Fakhruddin N, Mahfouz
R, Otrock ZK, Alameddine RS, Awada AH and Shamseddine A:
Expression, prognostic and predictive impact of VEGF and bFGF in
non-small cell lung cancer. Crit Rev Oncol Hematol. 84:149–160.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kerenidi T, Kazakou AP, Lada M, Tsilioni
I, Daniil Z and Gourgoulianis KI: Clinical significance of
circulating osteopontin levels in patients with lung cancer and
correlation with VEGF and MMP-9. Cancer Invest. 34:385–392. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shiau MY, Fan LC, Yang SC, Tsao CH, Lee H,
Cheng YW, Lai LC and Chang YH: Human papillomavirus up-regulates
MMP-2 and MMP-9 expression and activity by inducing interleukin-8
in lung adenocarcinomas. PLoS One. 8:e544232013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yeo CD, Kim YA, Lee HY, Kim JW, Lee SH,
Kim SJ, Kwon SS, Kim YH and Kim SC: Inhibiting IGF-1R attenuates
cell proliferation and VEGF production in IGF-1R over-expressing
EGFR mutant non-small cell lung cancer cells. Exp Lung Res.
43:29–37. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Peng WJ, Zhang JQ, Wang BX, Pan HF, Lu MM
and Wang J: Prognostic value of matrix metalloproteinase 9
expression in patients with non-small cell lung cancer. Clin Chim
Acta. 413:1121–1126. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fan Z, Duan X, Cai H, Wang L, Li M, Qu J,
Li W, Wang Y and Wang J: Curcumin inhibits the invasion of lung
cancer cells by modulating the PKCα/Nox-2/ROS/ATF-2/MMP-9 signaling
pathway. Oncol Rep. 34:691–698. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ye HJ, Bai JJ, Guo PP, Wang W and Lin CS:
Propofol suppresses invasion of human lung cancer A549 cells by
down-regulating aquaporin-3 and matrix metalloproteinase-9. Nan
Fang Yi Ke Da Xue Xue Bao. 36:1286–1290. 2016.(In Chinese).
PubMed/NCBI
|
|
19
|
Xu L, Lina W and Xuejun Y: The diagnostic
value of serum CEA, NSE and MMP-9 for on-small cell lung cancer.
Open Med (Wars). 11:59–62. 2016.PubMed/NCBI
|
|
20
|
Lee CY, Shim HS, Lee S, Lee JG, Kim DJ and
Chung KY: Prognostic effect of matrix metalloproteinase-9 in
patients with resected Non-small cell lung cancer. J Cardiothorac
Surg. 10:442015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Balla MM, Desai S, Purwar P, Kumar A,
Bhandarkar P, Shejul YK, Pramesh CS, Laskar S and Pandey BN:
Differential diagnosis of lung cancer, its metastasis and chronic
obstructive pulmonary disease based on serum Vegf, Il-8 and MMP-9.
Sci Rep. 6:360652016. View Article : Google Scholar : PubMed/NCBI
|