Introduction
It has been reported that breast cancer is one of
the main causes of female mortality from cancer worldwide in 2017
(1). The incidence of human breast
cancer is associated with various factors, including lifestyle,
medical conditions, oncogenes and virus infection (2–7). It has
been reported that human papillomaviruses (HPVs), including high
risk-HPV (HR-HPV), may be responsible for the pathogenesis and
development of breast cancer. HPV16 is the most prevalent type of
HR-HPVs. The integration of the DNA of HPV16 into host cells
promotes a constitutive high expression of E7 oncoprotein, leading
to carcinogenesis in vivo (8).
A number of HPV vaccines have been developed to prevent
HPV16-mediated cancer progression (9,10).
However, these vaccines have been proven to be inefficient for the
treatment of HPV16-mediated cancer. Polymerase chain reaction (PCR)
has been employed for the diagnosis of HR-HPVs (11). However, the detection rate of HPV16 in
breast carcinoma may vary by region (12,13). As
~80% of all breast cancers are invasive ductal carcinoma, the
expression of HPV16 E7 was examined in samples from patients with
invasive breast ductal carcinoma from North China in the present
study (14). Additionally, novel
therapeutic targets for HPV16 E7-mediated cancer were
investigated.
Cyclooxygenase-2 (COX-2) is a rate-limiting
catalyzer in the conversion of arachidonic acid to prostaglandins
(15). Furthermore, COX-2 is highly
modulated in various malignancies, including breast carcinoma
(16,17). Several reports have demonstrated that
the suppression of COX-2 by selective inhibitors has antiviral
effects on viral agents, including herpes simplex virus, avian
influenza A (H5N1) and hepatitis C virus (18–20).
Celecoxib is a selective COX-2 inhibitor and has been reported to
be used for the treatment of various types of cancer (21–23).
Evidence suggests that COX-2 is overexpressed in various
HPV-induced lesions (24,25). However, it remains unknown whether the
upregulation of COX-2 results from HPV E7-mediated progression in
breast carcinoma.
In the present study, the expression of HPV16 E7 was
detected in samples from patients with invasive breast ductal
carcinomas from North China. Additionally, the molecular mechanisms
underlying the function of HPV16 E7 in the proliferation of breast
cancer cells were examined.
Materials and methods
Tissue specimens
A total of 59 cases of invasive breast ductal
carcinoma were collected from the patients who underwent resection
in the Department of Pathology, Third Affiliated Hospital of
Xinxiang Medical University (Henan, China) between January 2010 and
March 2012. All patients were females and did not receive
chemotherapy, radiotherapy or immunotherapy prior to surgery. All
specimens were subjected to haematoxylin and eosin staining and
diagnosed as invasive ductal breast carcinoma by two pathologists.
All participants provided written informed consent and the tissue
acquisition protocol was approved by the Institutional Board of
Xinxiang Medical University (Xinxiang, China).
DNA isolation and quantitative
(q)PCR
Invasive breast ductal carcinoma tissues were fixed
in neutral buffered formalin, embedded in paraffin and stored at
room temperature. Paraffin-embedded tissue samples were cut into 4
µm-thick sections. The sections were deparaffinized in xylene and
then were rehydrated in a descending ethanol series. The sections
were dried at room temperature and digested with Proteinase K
(Qiagen GmbH, Hilden, Germany) overnight at 56°C. The following
day, the samples were incubated for 1 h at 90°C to inactivate
Proteinase K and total DNA was extracted from paraffin-embedded
tissues using QIAamp DNA FFPE Tissue kit (Qiagen GmbH), according
to the manufacturer's protocol. The primers for HPV16 E7 and COX-2
are presented in the Table I. The
thermocycling conditions were as follows: Initial denaturation for
1 min at 95°C followed by 40 cycles of denaturation at 95°C for 30
sec, 50°C for 45 sec, 72°C for 30 sec and a final extension at 72°C
for 5 min. DNA content was measured using Applied Biosystems 7500
Sequence Detection system and SYBR Green I (Applied Biosystems;
Thermo Fisher Scientific, Inc., Waltham, MA, USA). The data were
normalized to the geometric mean of the housekeeping gene GAPDH and
quantified using the 2−ΔΔCq method (26).
 | Table I.Primer sequences. |
Table I.
Primer sequences.
| Gene | Forward primer | Reverse primer |
|---|
| HPV16E7 |
5′-GCATGGAGATACACCTACATTG-3′ |
5′-TGGTTTCTGAGAACAGATGG-3 |
| COX-2 |
5′-CGAGGTGTATGTATGAGTGT-3 |
5′-AGTGGGTAAGTATGTAGTGC-3 |
| GAPDH |
5′-GACTCATGACCACAGTCCATGC-3 |
5′-AGAGGCAGGGATGATGTTCTG-3 |
Immunohistochemistry
The expression of HPV16 E7 and COX-2 in invasive
breast ductal carcinoma tissues were detected using
immunohistochemistry streptavidin peroxidase (SP) method. IHC
SP-9000 kit which includes 3% H2O2, goat
serum, biotinylated second antibody and avidin-biotin complex
reagent. (SP-9000, Ready to use, ZSGB-BIO: OriGene Technologies,
Inc., Beijing, China). Paraffin-embedded tissue samples were cut
into 4 mm-thick sections and incubated at 60°C for 1 h. The
sections were deparaffinized in xylene and then were rehydrated in
a descending ethanol series. Endogenous peroxidase activity was
quenched by treatment with 3% hydrogen peroxide at room temperature
for 30 min. Antigens were retrieved with citrate buffer (0.01 M; pH
6). The tissue sections were blocked for 20 min with normal
non-immune serum and then incubated with mouse anti-HPV16 E7
(sc-51951; 1:50; Santa Cruz Biotechnology, Inc., Dallas, TX, USA)
or rabbit anti-COX-2 (12375-1-AP; 1:100; ProteinTech Group, Inc.,
Chicago, IL, USA) primary antibodies overnight at 4°C. Following
the primary incubation, the sections were incubated with
pre-diluted biotinylated second antibody and avidin-biotin complex
reagent according to the manufacturer's instructions at room
temperature for 20 min. The staining was visualized using
diaminobenzidine. In negative controls, the primary antibody was
replaced by PBS. The results of immunohistochemical staining were
evaluated by two independent pathologists blind to the clinical
findings. The staining intensity of COX2 was assessed with a
standard immunoreactive score (27).
Cell culture
MCF-7 cells stably expressing HPV16 E7 (MCF-7/HPV16
E7) or negative control (MCF-7/vector) were established previously
(28). Cells were maintained in
Dulbecco's modified Eagle's medium (Thermo Fisher Scientific, Inc.)
supplemented with 10% fetal bovine serum (FBS; Thermo Fisher
Scientific, Inc.) and 1% penicillin/streptomycin (Thermo Fisher
Scientific, Inc.) with the temperature of 37°C and 5%
CO2.
Western blot analysis
Total protein was extracted from cells with 1X
sample buffer (3.8 g Tris base, 2.5 ml 10% SDS, 50 ml Glycerin, 75
ml 20% SDS, then ddH2O2 added to a total volume of 500 ml). Protein
lysates obtained from the cells and protein determination was
measured by BCA protein assay kit (20201ES86; Shanghai Qcbio
Science and Technologies Co., Ltd, Shanghai, China). A total of 20
µl protein lysates was loaded per lane and then was separated by
SDS-PAGE (10.5% gels) and transferred onto a polyvinylidene
difluoride membrane (Nanjing KeyGen Biotech Co., Ltd., Nanjing,
China). The membranes were blocked in 5% non-fat milk, which was
suspended in tris-buffered saline with Tween 20 in room temperature
for 2 h and then were incubated with mouse anti-HPV16 E7 (1:200) or
rabbit anti-COX-2 (1:200) primary antibodies overnight at 4°C. The
membranes were incubated with the HRP-conjugated secondary antibody
(7076s; anti-mouse IgG; 1:2,000; 7074s; anti-rabbit IgG; 1:2,000;
CST Biological Reagent Co., Ltd., Shanghai, China) in room
temperature for 1 h. The protein bands were visualized by enhanced
chemiluminescence (Tanon Science and Technology Co., Ltd.,
Shanghai, China).
MTT assay
A total of 1×103 cells were seeded onto
96-well plates and cultured for 24 h. Then, 20 µl MTT solution
(Merck KGaA, Darmstadt, Germany) was added to each well prior to
incubation at 37°C for an additional 4 h. Following careful removal
of the medium, 150 µl dimethyl sulfoxide (Merck KGaA) was added to
the wells. The absorbance was measured at 450 nm using a microplate
autoreader (Bio-Rad Laboratories, Inc., Hercules, CA, USA). Three
individual experiments were performed.
Colony formation assay
Cells were trypsinized, plated on 6-well plates (200
cells/well) and cultured for 2 weeks. Subsequently, the cells were
fixed with 4% paraformaldehyde for 5 min and stained with
hematoxylin for 30 min. Visible colonies consisting of >50 cells
were counted. Three independent experiments were performed.
Soft agar assay
A total of 1×103 cells were resuspended
in 2 ml 0.3% low melting point agarose in DMEM/20% FBS and plated
on top of 1 ml 0.6% agarose in the same medium in 6-well culture
plates. The plates were incubated at 37°C in a humidified
atmosphere containing 5% CO2 for 2 weeks. The cell
colonies were photographed using light microscope (magnification,
×200).
In vivo proliferation assay
Female BALB/c nude mice aged 4–5 weeks (weight,
15–18 g) were obtained from the Center of Laboratory Animal Science
of Guangdong (Guangzhou, China). The mice were kept in the plastic
cage with sealed air filter at 27°C, in ad libitum feeding
and maintained 10 h of light and 14 h of dark daily. All animal
experiments were conducted in accordance with the China Guidelines
for Animal Care and Ethic for Animal Experiments. The study was
approved by the Institutional Animal Care and Use Committee of
Xinxiang Medical University (Henan, China). For the in vivo
proliferation assay, a total of 2×106 MCF-7/HPV16 E7 or
MCF-7/vector cells were injected subcutaneously into the hind limb
(n=6/group) of the mice. Tumor size was measured using a slide
caliper twice weekly (volume = length × width × height). After 3
weeks, mice were euthanized and tumors were excised, fixed in 10%
neutral buffered formalin and embedded in paraffin.
Paraffin-embedded tissue samples were cut into 4-µm thick sections.
Sections were deparaffinized, transferred to xylene, and rehydrated
in descending concentrations of ethanol (100, 100, 95, 95, 85, 70
and 0%). The sections were then stained with hematoxylin and eosin.
Additionally, the tissue sections were washed three times in PBS.
Citrate buffer (0.01 M, pH 6.0) was applied to the sections for 5
min under 95°C for antigen retrieval. Then IHC SP-9000 kit
(SP-9000, Ready to use, ZSGB-BIO: OriGene Technologies, Inc.) was
used in the detection of ki-67 expression according to the
manufacturer's protocol. Firstly, the sections were incubated in 3%
H2O2 and goat serum at room temperature for
30 min respectively and then were incubated in 4°C for 10 h with
primary antibody against mouse ki-67 (MX006; 1:100; Fuzhou Maixin
Biotech Co., Ltd., Fuzhou, China). Subsequently, the slides were
incubated with biotinylated second antibody and avidin-biotin
complex reagent (SP-9000 kit) at room temperature for 20 min.
Treatment with COX-2-specific small
interfering RNA (siRNA) and celecoxib
COX-2 siRNA (sequence, 5′-GCTCAGCCATACAGCAAAT-3′)
was purchased from Guangzhou RiboBio Co., Ltd. (Guangzhou, China).
Cells were transfected Lipofectamine® 2000 (Invitrogen;
Thermo Fisher Scientific, Inc.), according to the manufacturer's
protocol (siRNA, 100 nmol/l; 37°C for 24 h). The control siRNA was
provided by Guangzhou RiboBio Co., Ltd. (Guangzhou, China) which
was a random sequence of siRNA and incompatible with the target
gene. Cells were treated with celecoxib (Selleck Chemicals,
Houston, TX, USA) at the concentration of 1 mol/l (diluted in DMSO)
at 37°C for 48 h (DMSO without celecoxib as the control).
Statistical analysis
Data were analyzed using SPSS software (v20.0; IBM
Corp., Armonk, NY, USA). Data are expressed as the mean ± standard
deviation. Three individual experiments were performed. One-way
analysis of variance followed by least significant difference (LSD)
test was used to examine differences between more than two group
means. Mann-Whitney U-test was used to examine differences between
two groups medians. The association between HPV16 E7 and COX-2
expression was analyzed using Chi-square test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Expression of HPV16 E7 DNA in invasive
ductal breast cancer
The DNA of HPV16 E7 was detected in 18 out of 59
cases of paraffin-embedded invasive ductal breast carcinoma samples
by qPCR (Table II). Therefore, HPV16
E7 was positive for 30.5% cases of invasive ductal breast carcinoma
from North China.
 | Table II.Expression of HPV16 E7 and COX-2 in
invasive ductal breast cancer. |
Table II.
Expression of HPV16 E7 and COX-2 in
invasive ductal breast cancer.
| Sample | Sex | Ct GAPDH (mean ±
SD) | Ct of HPV16E7 (mean
± SD) | Ct of COX-2 (mean ±
SD) |
|---|
| 1 | Female | 25.15±0.07 | Undetermined | 27.56±0.43 |
| 2 | Female | 24.27±0.18 | 25.53±0.29 | 23.62±0.23 |
| 3 | Female | 25.51±0.32 | Undetermined | 27.68 ±0.39 |
| 4 | Female | 23.55±0.18 | 24.29±0.09 | 21.38±0.38 |
| 5 | Female | 26.42±0.23 | 27.58±0.31 | 25.36±0.24 |
| 6 | Female | 26.09±0.32 | Undetermined | 28.29±0.10 |
| 7 | Female | 28.07±0.07 | Undetermined | 27.18±0.11 |
| 8 | Female | 24.58±0.20 | 22.22±0.04 | 23.22±0.19 |
| 9 | Female | 26.94±0.05 | Undetermined | 29.52±0.18 |
| 10 | Female | 27.59±0.50 | Undetermined | 25.67±0.34 |
| 11 | Female | 25.07±0.27 | Undetermined | 27.77±0.35 |
| 12 | Female | 29.35±0.16 | Undetermined | 28.77±0.44 |
| 13 | Female | 25.06±0.12 | Undetermined | 27.53±0.41 |
| 14 | Female | 21.30±0.21 | Undetermined | 26.64±0.91 |
| 15 | Female | 25.44±0.26 | Undetermined | 27.56±0.29 |
| 16 | Female | 24.33±0.15 | 32.17±0.03 | 24.21±0.17 |
| 17 | Female | 26.49±0.30 | Undetermined | 28.32±0.21 |
| 18 | Female | 26.28±0.19 | 28.16±0.05 | 24.42±0.15 |
| 19 | Female | 28.28±0.22 | Undetermined | 27.30±0.10 |
| 20 | Female | 27.51±0.40 | Undetermined | 28.52±0.18 |
| 21 | Female | 26.62±0.20 | 33.21±0.05 | 26.44±0.20 |
| 22 | Female | 27.60±0.50 | Undetermined | 26.52±0.23 |
| 23 | Female | 24.57±0.23 | Undetermined | 27.58±0.21 |
| 24 | Female | 29.44±0.23 | Undetermined | 29.13±0.18 |
| 25 | Female | 25.67±0.17 | Undetermined | 24.55±0.37 |
| 26 | Female | 24.67±0.20 | 25.32±0.27 | 22.33±0.17 |
| 27 | Female | 27.36±0.15 | Undetermined | 27.52±0.37 |
| 28 | Female | 25.19±0.13 | 30.27±0.13 | 24.12±0.03 |
| 29 | Female | 29.34±0.27 | Undetermined | 27.19±0.29 |
| 30 | Female | 25.52±0.26 | 28.13±0.10 | 23.56±0.28 |
| 31 | Female | 24.81±0.15 | Undetermined | 24.15±0.09 |
| 32 | Female | 26.41±0.19 | Undetermined | 27.45±0.31 |
| 33 | Female | 23.28±0.10 | Undetermined | 21.67±0.10 |
| 34 | Female | 28.76±0.30 | Undetermined | 28.29±0.15 |
| 35 | Female | 24.54±0.28 | 24.18±0.03 | 22.59±0.13 |
| 36 | Female | 29.60±0.36 | Undetermined | 29.33±0.29 |
| 37 | Female | 27.57±0.31 | Undetermined | 26.47±0.15 |
| 38 | Female | 29.82±0.03 | Undetermined | 29.21±0.04 |
| 39 | Female | 24.70±0.18 | 33.20±0.08 | 22.49±0.35 |
| 40 | Female | 22.80±0.16 | 26.53±0.29 | 21.59±0.11 |
| 41 | Female | 26.29±0.18 | Undetermined | 25.67±0.10 |
| 42 | Female | 27.37±0.48 | Undetermined | 26.29±0.15 |
| 43 | Female | 27.95±0.02 | Undetermined | 26.59±0.13 |
| 44 | Female | 30.49±0.17 | Undetermined | 30.39±0.23 |
| 45 | Female | 26.27±0.42 | Undetermined | 24.74±0.55 |
| 46 | Female | 27.44±0.34 | Undetermined | 27.24±0.22 |
| 47 | Female | 29.74±0.16 | Undetermined | 29.38±0.24 |
| 48 | Female | 22.42±0.25 | 30.58±0.31 | 21.32±0.22 |
| 49 | Female | 23.71±0.20 | 35.29±0.09 | 23.45±0.22 |
| 50 | Female | 23.61±0.44 | 27.18±0.01 | 25.42±0.52 |
| 51 | Female | 25.12±0.05 | Undetermined | 25.39±0.10 |
| 52 | Female | 26.46±0.31 | Undetermined | 26.72±0.33 |
| 53 | Female | 27.41±0.25 | Undetermined | 27.65±0.28 |
| 54 | Female | 29.14±0.12 | Undetermined | 29.22±0.14 |
| 55 | Female | 22.97±0.03 | 23.37±0.23 | 21.61±0.12 |
| 56 | Female | 26.81±0.16 | 29.31±0.15 | 25.27±0.12 |
| 57 | Female | 28.49±0.22 | Undetermined | 30.46±0.46 |
| 58 | Female | 26.10±0.02 | Undetermined | 24.57±0.31 |
| 59 | Female | 25.44±0.43 | Undetermined | 26.15±0.18 |
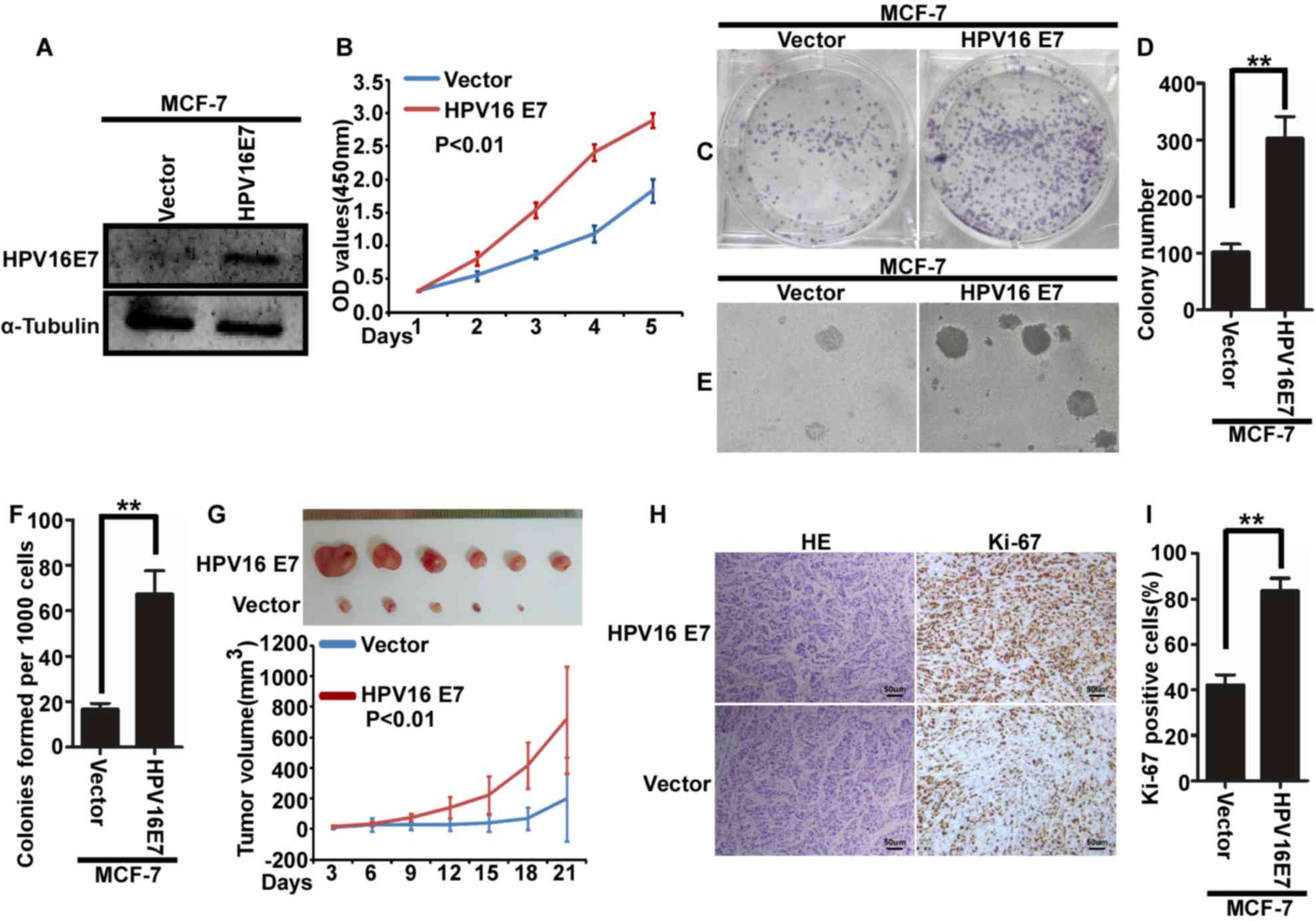
HPV16 E7 promotes the proliferation of
breast cancer cells in vitro and in vivo
To further explore the function of HPV16 E7 in
breast cancer, MCF-7 cells with stable expression of HPV16 E7 were
used. MCF-7/vector cells were used as a control (Fig. 1A). Cell proliferation was assessed
using a MTT (Fig. 1B), colony
formation (Fig. 1C and D) and soft
agar (Fig. 1E). The results
demonstrated that stable expression of HPV16 E7 in MCF-7 cells
promoted the proliferation of MCF-7 cells (Fig. 1B-F). Additionally, female BALB/c nude
mice injected with MCF7/HPV16 E7 cells exhibited an increased tumor
volume (Fig. 1G) and increased
cellular proliferation (Fig. 1H, I)
compared with control mice.
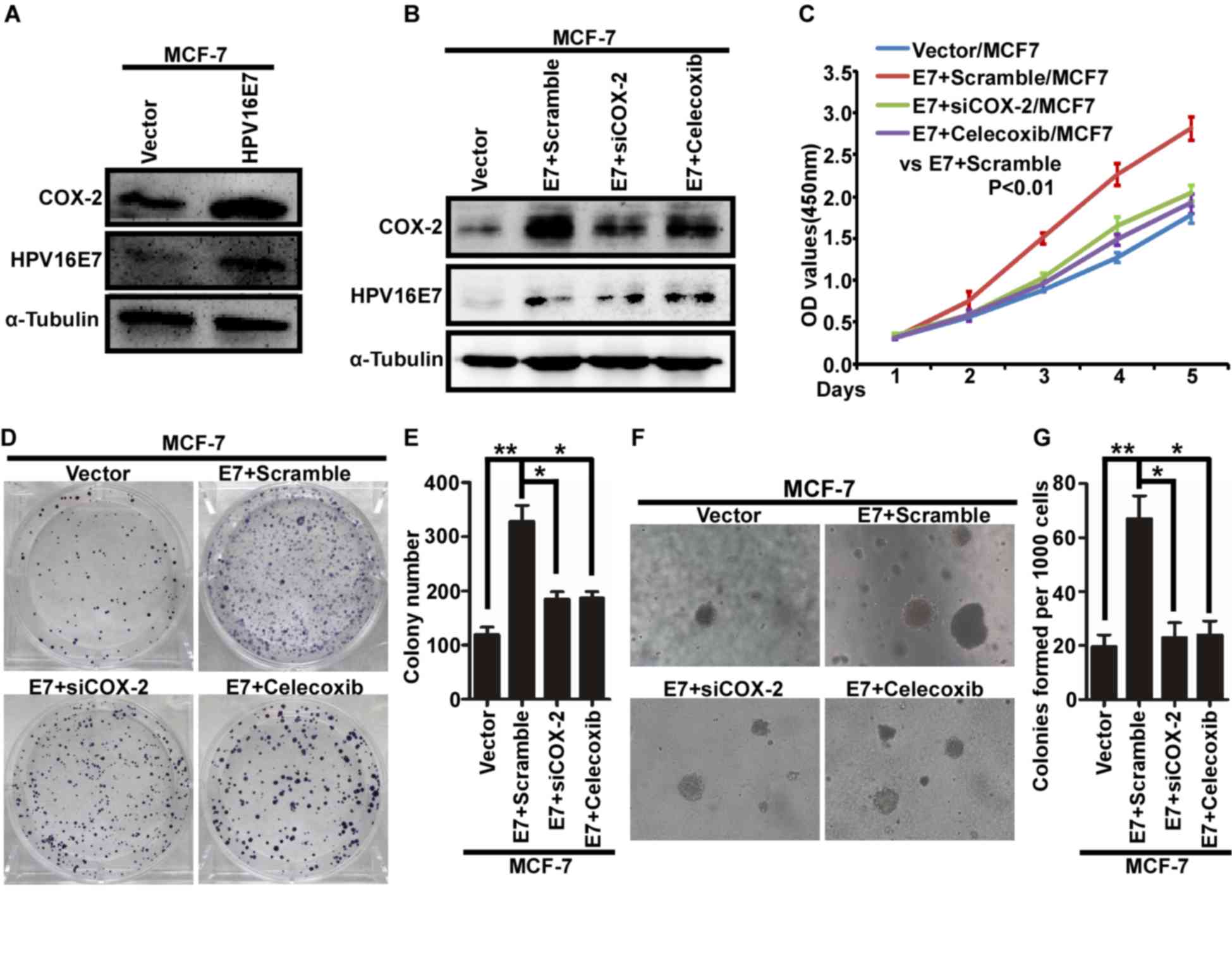
HPV16 E7 promotes the proliferation of
breast cancer cells by upregulating COX-2
Western blot analysis demonstrated that the
expression of COX-2 increased with stable expression of HPV16 E7 in
MCF-7 cells (Fig. 2A). Next,
MCF-7/HPV16 cells were treated with COX-2-specific siRNA (siCOX-2)
and celecoxib to inhibit the expression of COX-2 (Fig. 2B). Proliferation was assessed in
response to siCOX-2 and celecoxib treatment using a MTT (Fig. 2C), colony formation (Fig. 2D and E) and soft agar (Fig. 2F, G) and revealed that downregulation
of COX-2 significantly inhibited proliferation of MCF-7/HPV16 cells
(Fig. 2B-G). Therefore, these results
suggest that HPV16 E7 may promote the proliferation of breast
cancer cells by upregulating the expression of COX-2.
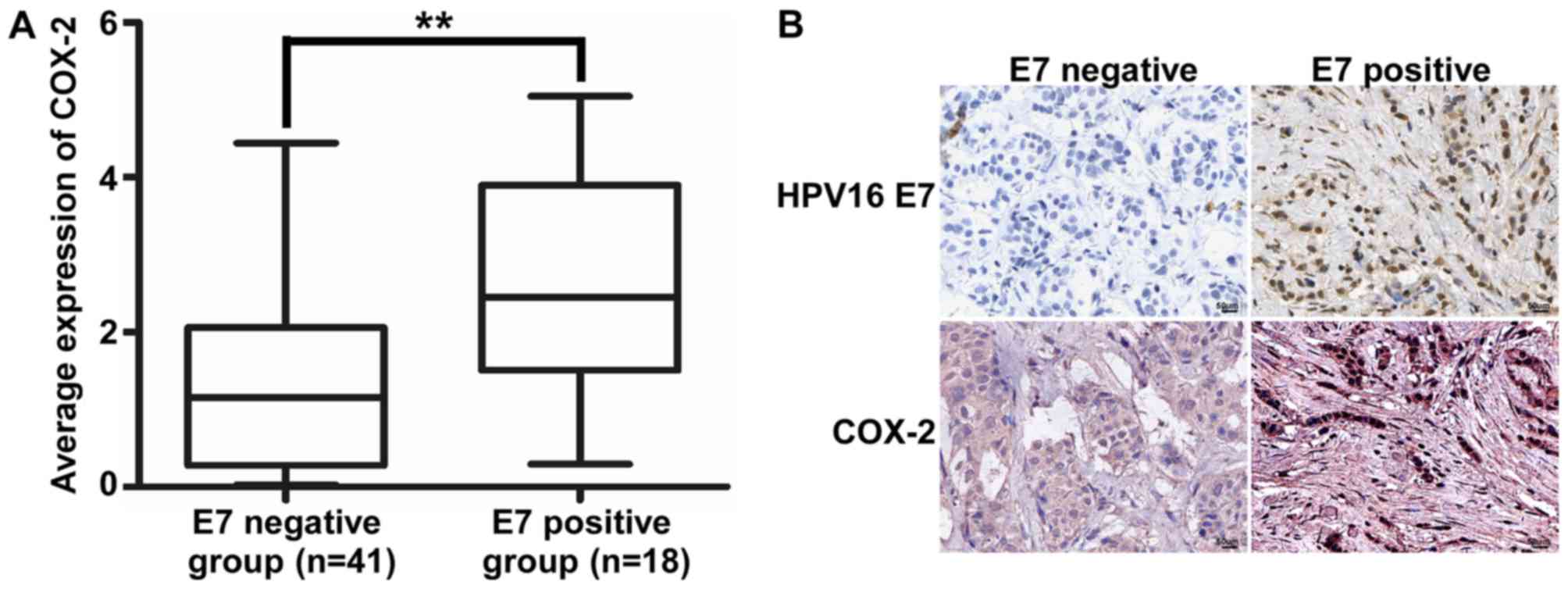
The association between the expression
of HPV16 E7 and COX- in invasive breast ductal carcinoma
According to the results of IHC, immunopositive
cells for HPV16 E7 were detected in the nucleus and the
immunopositive cells for COX-2 were detected in the cytoplasm. The
expression level of COX-2 DNA in HPV16 E7-positive samples was
significantly increased compared with that in HPV16 E7-negative
samples (Fig. 3A, Table II). Additionally, the expression of
HPV16 E7 and COX-2 was also detected using immunohistochemistry.
The results demonstrated that HPV16 E7 protein was expressed in 18
cases of invasive breast ductal carcinoma (Fig. 3B). Additionally, there was an
association between HPV16 E7 and COX-2 expression in invasive
breast ductal carcinoma (Table
III).
 | Table III.Association between the expression of
HPV16 E7 and COX-2 in invasive ductal breast cancer tissues by
immunohistochemistry. |
Table III.
Association between the expression of
HPV16 E7 and COX-2 in invasive ductal breast cancer tissues by
immunohistochemistry.
|
| COX-2
expression |
|
|
|---|
|
|
|
|
|
|---|
| HPV16 E7
expression | High | Low | χ2 value | P-value |
|---|
| Positive | 17 | 1 | 4.625 | 0.023 |
| Negative | 26 | 15 |
|
|
Discussion
Breast cancer remains the leading cause of mortality
in females worldwide. Breast cancer accounts for 1.7 million new
cases and 0.5 million cases of mortality worldwide in 2012
(29). Additionally, the incidence
and mortality rates of breast cancer have been increasing in the
developing countries (1). HPV is a
small, double-stranded and circular DNA virus that infects
epithelial cells. Accumulating evidence has indicated that various
HPVs, including HPV16, may be involved in the pathogenesis and
development of breast cancer (12,30).
However, the prevalence of HPV16 may vary widely. The detection
rate of HPV16 in breast carcinoma varies from 0–86%, indicating an
inconsistent association between HPV16 and the progression of
breast cancer. A recent meta-analysis suggested an increased risk
of breast cancer associated with HPV infection (31). HPV16 encodes a vital oncoprotein E7.
HPV16 E7 serves an important function in the viral life cycle by
regulating cellular proliferation and differentiation in the
epithelium, and thus causing the virus to replicate and be
constitutively expressed in differentiating epithelial cells
(32). Additionally, HPV16 E7 may be
a promising therapeutic target for cervical cancer (33).
In the present study, the expression of HPV16 E7 DNA
was detected in patients with invasive breast ductal carcinoma from
North China. The results demonstrated that HPV16 E7 DNA was
detected in 30.5% cases of invasive breast ductal carcinoma,
suggesting that HPV16 E7 may serve an important function in the
pathogenesis of breast cancer. Previous studies demonstrated that
infection with HPV16 E7 increased the proliferation of breast
cancer cells (34,35). The results of the present study
demonstrated that the expression of COX-2 in HPV16 E7-positive
samples was increased compared with that in HPV16 E7-negative
samples, suggesting that the expression of COX-2 may be upregulated
by the expression of HPV16 E7.
Recent studies have investigated the function of
COX-2 in tumorigenesis (36). COX-2
is an important COX inform, which is usually undetectable in normal
tissues. Various factors, including hormones, cytokines and
oncogenes may induce the expression of COX-2. It has been reported
that COX-2 serve important functions in carcinogenesis and
development of various tumors, including breast cancer (37,38). In
vivo, it has been demonstrated that increased expression of
COX-2 is associated with tumorigenesis (39). Recently, it has been demonstrated that
the combination of specific COX-2 inhibitors with conventional
chemotherapy may be used as a novel approach for the treatment of
breast cancer. Celecoxib is a selective COX-2 inhibitor that has
been used for the treatment of osteoarthritis and rheumatoid
arthritis. Recently, it has been demonstrated that celecoxib
prevented carcinogenesis, delayed cancer progression and enhanced
the efficacy of conventional cancer therapies, including
chemotherapy and radiation therapy (40–43).
Considering the lack of effective therapeutic treatments for
HPV-associated breast cancer, the use of celecoxib may be a
promising approach. In the present study, the effect of HPV16 E7 on
the expression of COX-2 was examined and it was demonstrated that
COX-2 may be regulated by HPV16 E7. Additionally, in vitro
experiments using COX-2 inhibitors demonstrated that HPV16 E7
promoted the proliferation of breast cancer cells by increasing the
expression of COX-2.
The expression of HPV16 E7 and COX-2 was detected in
59 cases of invasive breast ductal carcinoma from North China using
immunohistochemistry. The results revealed a positive association
between the expression of HPV16 E7 and COX-2. These results suggest
that COX-2 may be upregulated by HPV16 E7 and are in accordance
with previous studies (24,44). Currently, there is no effective
therapeutic approach for HPV-associated cancer (45). Thus, the development of therapeutic
strategies for the treatment of HPV-induced cancer is required. It
has been reported that celecoxib-treated HPV16+/- animals showed a
lower incidence of epidermal dysplasia compared with untreated mice
(46). Additionally, celecoxib was
reported to significantly decrease breast tumor volume in rats
(47). In conclusion, the use of
celecoxib may be an effective therapeutic approach for the
treatment of HPV-associated breast cancer.
In conclusion, the present study confirmed that
HPV16 E7 may be an important factor in the pathogenesis of breast
cancer in North China, and HPV16 E7 promoted the proliferation of
breast cancer cells by upregulating the expression of COX-2.
Additionally, the inhibition of COX-2 by siCOX-2 or celecoxib
attenuated the HPV16 E7-mediated proliferation of breast cancer
cells. Therefore, the present study may provide a potent
therapeutic target for HPV16 E7-associated breast cancer.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Science and
Technology Key Project of Henan Province Office Education of China
(grant no. 14A310004) and the Scientific Research Fund of Xinxiang
Medical University (grant nos. ZD200959, ZD2011-21 and
ZD2011-11).
Availability of data and materials
The data generated or analyzed during this study are
available from the corresponding author on reasonable request.
Author's contributions
XLQ and JC designed the experiments. YXW and ZYZ
conducted experiments and wrote the manuscript. JQW provided
research materials and methods and analyzed data.
Ethics approval and consent to
participate
All participants provided written informed consent
to participate and the tissue acquisition protocol was approved by
the Ethic Institutional Board of Xinxiang Medical University.
Consent for publication
The relevant patients were informed and agreed to
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Denny L, de Sanjose S, Mutebi M, Anderson
BO, Kim J, Jeronimo J, Herrero R, Yeates K, Ginsburg O and
Sankaranarayanan R: Interventions to close the divide for women
with breast and cervical cancer between low-income and
middle-income countries and high-income countries. Lancet.
389:861–870. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Brody JG, Rudel RA, Michels KB, Moysich
KB, Bernstein L, Attfield KR and Gray S: Environmental pollutants,
diet, physical activity, body size, and breast cancer: Where do we
stand in research to identify opportunities for prevention? Cancer.
109:2627–2634. 2017. View Article : Google Scholar
|
|
3
|
Kaiser J: Cholesterol forges link between
obesity and breast cancer. Science. 342:10282013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gage M, Wattendorf D and Henry LR:
Translational advances regarding hereditary breast cancer
syndromes. J Surg Oncol. 105:444–451. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Anothaisintawee T, Wiratkapun C,
Lerdsitthichai P, Kasamesup V, Wongwaisayawan S, Srinakarin J,
Hirunpat S, Woodtichartpreecha P, Boonlikit S, Teerawattananon Y
and Thakkinstian A: Risk factors of breast cancer: A systematic
review and meta-analysis. Asia Pac J Public Health. 25:368–387.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Glaser SL, Canchola AJ, Keegan TH, Clarke
CA, Longacre TA and Gulley ML: Variation in risk and outcomes of
Epstein-Barr virus-associated breast cancer by epidemiologic
characteristics and virus detection strategies: An exploratory
study. Cancer Causes Control. 28:273–287. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wu H, Zhao C, Adhikari VP, Lu L, Huang J,
Wei Y, Luo Q, Dai W, Wu Y, Li X, et al: The prevalence and
clinicopathological features of breast cancer patients with
hepatitis B virusinfection in China. Oncotarget. 8:18185–18190.
2017.PubMed/NCBI
|
|
8
|
White EA and Munger K: Crowd control: E7
conservation is the key to cancer. Cell. 170:1057–1059. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yin W, Duluc D, Joo H and Oh S: Dendritic
cell targeting vaccine for HPV-associated cancer. Cancer Cell
Microenviron. 3:e14822016.PubMed/NCBI
|
|
10
|
Torres-Rueda S, Rulisa S, Burchett HE,
Mivumbi NV and Mounier-Jack S: HPV vaccine introduction in Rwanda:
Impacts on the broader health system. Sex Reprod Healthc. 7:46–51.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Einstein MN, Smith KM, Davis TE, Schmeler
KM, Ferris DG, Savage AH, Gray JE, Stoler MH, Wright TC Jr,
Ferenczy A and Castle PE: Clinical evaluation of the
cartridge-based GeneXpert human papillomavirus assay in women
referred for colposcopy. J Clin Microbiol. 52:2089–2095. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ilahi NE, Anwar S, Noreen M, Hashmi SN and
Murad S: Detection of human papillomavirus-16 DNA in archived
clinical samples of breast and lung cancer patients from North
Pakistan. J Cancer Res Clin Oncol. 142:2497–2502. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Omura Y, Jones MK, Nihrane A, Duvvi H,
Shimotsuura Y and Ohki M: More than 97% of human papilloma virus
type 16 (HPV-16) was found with chrysotile asbestos &
relatively smooth round tumor outline, and less than 3% was found
with HPV-18 and tremolite asbestos & irregular
sawtooth-like zigzag outline in breast cancer tissues in over 500
mammograms of female patients: Their implications in diagnosis,
treatment, and prevention of breast cancer. Acupunct Electrother
Res. 38:211–230. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tavassoli FA and Devolee P: Worldhealth
organization classification of tumors, pathology and genetics of
the breast and female genital organs. IARC press; 2003
|
|
15
|
Wu KK: Cyclooxygenase 2 induction:
Molecular mechanism and pathophysiologic roles. J Lab Clin Med.
128:242–245. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Harris RE, Casto BC and Harris ZM:
Cyclooxygenase-2 and the inflammogenesis of breast cancer. World J
Clin Oncol. 5:677–692. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Liu B, Qu L and Yan S: Cyclooxygenase-2
promotes tumor growth and suppresses tumor immunity. Cancer Cell
Int. 15:1062015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gebhardt BM, Varnell ED and Kaufman HE:
Inhibition of cyclooxygenase 2 synthesis suppresses Herpes simplex
virus type 1 reactivation. J Ocul Pharmacol Ther. 21:114–120. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lee SM, Gai WW, Cheung TK and Peiris JS:
Antiviral effect of a selective COX-2 inhibitor on H5N1 infection
in vitro. Antiviral Res. 91:330–334. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lin CK, Tseng CK, Chen KH, Wu SH, Liaw CC
and Lee JC: Betulinic acid exerts anti-hepatitis C virus activity
via the suppression of NF-κB- and MAPK-ERK1/2-mediated COX-2
expression. Br J Pharmacol. 2015. View Article : Google Scholar
|
|
21
|
Zhao Q, Guo J, Wang G, Chu Y and HU X:
Suppression of immune regulatory cells with combined therapy of
celecoxib and sunitinib in renal cell carcinoma. Oncotarget.
8:1668–1677. 2017.PubMed/NCBI
|
|
22
|
Tury S, Becette V, Assayag F, Vacher S,
Benoist C, Kamal M, Marangoni E, Bièche I, Lerebours F and Callens
C: Combination of COX-2 expression and PIK3CA mutation as
prognostic and predictive markers forcelecoxib treatment in breast
cancer. Oncotarget. 7:85124–85141. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Riva B, De Dominici M, Gnemmi I, Mariani
SA, Minassi A, Minieri V, Salomoni P, Canonico PL, Genazzani AA,
Calabretta B and Condorelli F: Celecoxib inhibits proliferation and
survival of chronic myelogeous leukemia (CML) cells via
AMPK-dependent regulation of β-catenin and mTORC1/2. Oncotarget.
7:81555–81570. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Subbaramaiah K and Dannenberg AJ:
Cyclooxygenase-2 transcription is regulated by human papillomavirus
16 E6 and E7 oncoproteins: Evidence of a corepressor/coactivator
exchange. Cancer Res. 3976–3985. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhuang ZH, Tsao SW, Deng W, Wang JD, Xia
HH, He H, Feng HC, Wang LD, Gu Q, Lam SK, et al: Early upregulation
of cyclooxygenase-2 in human papillomavirus type 16 and
telomerase-induced immortalization of human esophageal epithelial
cells. J Gastroenterol Hepatol. 23:1613–1620. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-delta delta C(T))method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Friedrichs K, Gluba S, Eidtmann H and
Jonat W: Overexpression of p53 and prognosis in breast cancer.
Cancer. 72:3641–3647. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Li N, Ye YP, Zhu HF, et al: The effect and
mechanism of HPV16 E6 and E7 on the invasion of breast cancer.
Chongqing Yixue. 41:2572–2574. 2012.
|
|
29
|
Ferlay J, Soerjomataram I, Dikshit R, Eser
S, Mathers C, Rebelo M, Parkin DM, Forman D and Bray F: Cancer
incidence and mortality worldwide: Sources, methods and major
patterns in GLOBOCAN 2012. Int J Cancer. 136:E359–E386. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zhou Y, Li J, Ji Y, Ren M, Pang B, Chu M
and Wei L: Inconclusive role of human papillomavirus infection in
breast cancer. Infect Agent Cancer. 10:362016. View Article : Google Scholar
|
|
31
|
Bae JM and Kim EH: Human papillomavirus
infection and risk of breast cancer: A meta-analysis of case
control studies. Infect Agents Cancer. 11:142016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Münger K, Basile JR, Duensing S, Eichten
A, Gonzalez SL, Grace M and Zacny VL: Biological activities and
molecular targets of the human papillomavirus E7 oncoprotein.
Oncogene. 20:7888–7898. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Grabowska AK, Kaufmann AM and Riemer AB:
Identification of promiscuous HPV16-derived T helper cell epitopes
for therapeutic HPV vaccine design. Int J Cancer. 136:212–224.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Liu Y, Wang YN, Chen CQ, Zhang J, Qian W,
Dong Y, Liu Z, Zhang X, Wang X, Zhang Z, et al: LSD1 binds to HPV16
E7 and promotes the epithelial-mesenchymal transition in cervical
cancer by demethylating histones at the Vimentin promoter.
Oncotarget. 8:11329–11342. 2017.PubMed/NCBI
|
|
35
|
Organista-Nava J, Gómez-Gómez Y,
Ocadiz-Delgado R, García-Villa E, Bonilla-Delgado J,
Lagunas-Martínez A, Tapia JS, Lambert PF, García-Carrancá A and
Gariglio P: The HPV16 E7 oncoprotein increases the expression of
Oct3/4 and stemness-related genes and augments cell self-renewal.
Virology. 499:230–242. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Xu F, Li M, Zhang C, Cui J, Liu J, Li J
and Jiang H: Clinicopathological and prognostic significance of
COX-2 immunohistochemical expression in breast cancer: A
meta-analysis. Oncotarget. 8:6003–6012. 2017.PubMed/NCBI
|
|
37
|
Campillo N, Torres M, Vilaseca A, Nonaka
PN, Gozal D, Roca-Ferrer J, Picado C, Montserrat JM, Farré R,
Navajas D and Almendros I: Role of Cyclooxygenase-2 on intermittent
hypoxia-induced lung tumor Malignancy in a mouse model of sleep
apnea. Sci Rep. 7:446932017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Hsu HH, Chen MC, Day CH, Lin YM, Li SY, Tu
CC, Padma VV, Shih HN, Kuo WW and Huang CY: Thymoquinone suppresses
migration of LoVo human colon cancer cells by reducing
prostaglandin E2 induced COX-2 activation. World J Gastroenterol.
23:1171–1179. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Howe LR: Inflammation and breast cancer.
Cyclooxygenase/prostaglandin signaling and breast cancer. Breast
Cancer Res. 9:2102007. View
Article : Google Scholar : PubMed/NCBI
|
|
40
|
Shirali S, Barari A, Hosseini SA and
Khodadi E: Effects of six weeks endurance training and aloe vera
supplementation on COX-2 and VEGF levels in mice with breast
cancer. Asian Pac J Cancer Prev. 18:31–36. 2017.PubMed/NCBI
|
|
41
|
Sun J, Liu NB, Zhuang HQ, Zhao LJ, Yuan ZY
and Wang P: Celecoxib-erlotinib combination treatment enhances
radiosensitivity in A549 human lung cancer cell. Cancer Biomark.
19:45–50. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Pridgen WL, Duffy C, Gendreau JF and
Gendreau RM: A famciclovir + celecoxib combination treatment is
safe and efficacious in the treatment of fibromyalgia. J Pain Res.
10:451–460. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Liu B, Yan S, Qu L and Zhu J: Celecoxib
enhances anticancer effect of cisplatin and induces anoikis in
osteosarcoma via PI3K/Akt pathway. Cancer Cell Int. 17:12017.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Wu R, Abramson AL, Shikowitz M, Dannenberg
AJ and Steinberg BM: Epidermal growth factor-induced
cyclooxygenase-2 expression is mediated through
phosphatidylinositol-3 kinase, not mitogen-activated
protein/extracellular signal-regulated kinase kinase, in recurrent
respiratory papillomas. Clin Cancer Res. 11:6155–6161. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Yang A, Jeang J, Cheng K, Cheng T, Yang B,
Wu TC and Hung CF: Current state in the development of candidate
therapeutic HPV vaccines. Expert Rev Vaccines. 15:989–1007. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
DA Costa RMG, Araújo R, Santos JMO,
Fernandes M, Neto T, Sousa H, Ribeiro J, Bastos MMSM, Oliveira PA,
Carmo D, et al: Regulation of miRNA-146a and miRNA-150 levels by
celecoxib in premalignant lesions of K14-HPV16 Mice. Anticancer
Res. 37:2913–2918. 2017.PubMed/NCBI
|
|
47
|
Alshafie GA, Abou-Issa HM, Seibert K and
Harris RE: Chemotherapeutic evaluation of Celecoxib, a
cyclooxygenase-2 inhibitor, in a rat mammarytumor model. Oncol Rep.
7:1377–1381. 2000.PubMed/NCBI
|