Introduction
Sorafenib is a small-molecule multi-kinase inhibitor
approved by the US Food and Drug Administration as an oral agent
for the treatment of hepatocellular carcinoma (HCC) and renal cell
carcinoma. It is an inhibitor of Raf serine/threonine kinases,
c-Raf, wild type and mutant B-Raf, which are all essential
constituents of the Ras/Raf/mitogen-activated protein kinase (MAPK)
signaling pathway that is important for cancer cell proliferation,
and survival. Sorafenib also potently inhibits receptor tyrosine
kinases, including vascular endothelial growth factor receptor
(VEGFR)-2 and −3, and the platelet-derived growth factor
receptor-β. As these targets are involved in cancer growth and
angiogenesis, sorafenib has been demonstrated to exert anticancer
activity through inhibiting tumor cell proliferation, and tumor
angiogenesis (1,2). Two placebo-controlled phase III studies
have revealed that sorafenib treatment results in ~3-month
extension of survival in patients with advanced HCC (3,4). Another
phase III study on advanced HCC demonstrated a significant
improvement in progression-free survival relative to the placebo
group (167 vs. 84 days) (5). However,
similar to other kinase inhibitors, unresponsiveness and acquired
resistance are commonly observed in patients with HCC, which hinder
the clinical use of sorafenib (6,7). Although
the precise mechanism underlying sorafenib resistance remains
elusive, various efforts have been made to improve sorafenib
sensitivity, among which combination therapy is a promising
approach.
Luteolin, 3′,4′,5,7-tetrahydroxyflavone, is a
flavonoid identified in a variety of vegetables, including
broccoli, green peppers and celery. Flavonoids are common nutrients
that are antioxidants, estrogenic regulators and antimicrobial
agents. Numerous flavonoids may also serve as cancer preventive
agents (8). Likewise, luteolin has
been demonstrated to exhibit anticancer activities, including the
induction of apoptosis, cell cycle arrest and antiangiogenesis
(9–11). The pro-apoptotic property of luteolin
is associated with redox regulation, DNA damage and protein kinases
inhibition (12). Furthermore,
numerous studies have revealed that luteolin may sensitize cancer
cells to therapeutically induced cytotoxicity through suppressing
cell survival pathways and stimulating apoptosis pathways (13–15).
Luteolin are generally safe and associated with low toxicity,
making them ideal candidates for chemosensitizer. To the best of
our knowledge, the combination effect of luteolin and sorafenib in
cancer cell killing remains elucidated. In the present report,
whether the combination of sorafenib and luteolin was able to
increase anticancer activity in HCC cells was investigated, and the
underlying mechanism was addressed.
Materials and methods
Reagents
Sorafenib (Nexavar®) and luteolin were
purchased from Bayer AG (Leverkusen, Germany) and Sigma-Aldrich
(Merck KGaA, Darmstadt, Germany), respectively. Antibodies against
active caspase-3 and poly (ADP-ribose) polymerase (PARP) were from
BD Pharmingen (BD Biosciences, Franklin Lakes, NJ, USA).
Anti-phospho-c-Jun N-terminal kinase (JNK), -JNK1, and -β-actin
were from Cell Signaling Technology, Inc. (Danvers, MA, USA), Abcam
(Cambridge, UK), and Protein Tech Group, Inc. (Chicago, IL, USA),
respectively. The pan-caspase inhibitor zVAD-fmk, the JNK inhibitor
SP600125, the ERK inhibitor U0126, and the P38 inhibitor SB203580
were purchased from Calbiochem (Merck KGaA). Reactive oxygen
species (ROS) scavenger butylated hydroxyanisole (BHA) and
N-acetyl-L-cysteine (NAC) were from Sigma-Aldrich (Merck KGaA).
Cell lines and cell culture
Human hepatocellular carcinoma Hep3B and SMMC-7721
cell lines were purchased from the Type Culture Collection of
Chinese Academy of Sciences (Shanghai, China). The cells were
cultured in Dulbecco's modified Eagle's medium (Invitrogen; Thermo
Fisher Scientific, Inc., Waltham, MA, USA) supplemented with 10%
fetal bovine serum (Sigma-Aldrich; Merck KGaA), 100 U/ml
penicillin, and 100 µg/ml streptomycin under standard incubation
conditions (37°C, 5% CO2).
Cytotoxicity assay based on the
release of lactate dehydrogenase (LDH)
Following designated treatment, cell death was
quantitatively detected by a cytotoxicity assay based on the
release of lactate dehydrogenase using a cytotoxicity detection kit
(Promega Corporation, Madison, WI, USA) as described previously
(16). Briefly, 50 µl culture medium
from each well was collected and transferred to 96-well
flat-bottomed plates. LDH activity was determined by adding 50 µl
reaction mixture to each well. The absorbance of the samples was
measured at 490 nm using a plate reader. All the experiments were
repeated between three and five times, and data are expressed as
the mean ± standard deviation. Cell death was calculated using the
following formula: Cytotoxicity (%) = (Experimental
value-Spontaneous LDH release)/(Maximum LDH release-Spontaneous LDH
release) × 100.
Apoptosis analysis by flow
cytometry
Flow cytometry was applied to detect apoptosis in
cultured cells using an Annexin V-fluorescein isothiocyanate (FITC)
Apoptosis Detection kit purchased from Nanjing KeyGen Biotech Co.,
Ltd. (Nanjing, China). Following designated treatments, cells were
double stained with annexin V-FITC and propidium iodide (PI)
according to the manufacturer's protocol. Apoptosis was then
analyzed by flow cytometry (BD Biosciences). Early apoptosis was
defined as Annexin V+/PI− staining (B4) and
late apoptosis was defined as Annexin V+/PI+
staining (B2).
Western blot analysis
Cells treated as indicated in each figure legend
were lysed in M2 buffer (20 mmol/l Tris-HCl (pH 7.6), 0.5% NP40,
250 mmol/l NaCl, 3 mmol/l EDTA, 3 mmol/l EGTA, 2 mmol/l DTT, 0.5
mmol/l phenylmethylsulfonyl fluoride, 20 mmol/l β-glycerophosphate,
1 mmol/l sodium vanadate, and 1 µg/ml leupeptin). Protein
concentrations in the cell extracts were determined by using BCA
Protein Assay Kit. Cell extracts (~50 µg) were resolved in SDS-PAGE
(8% gel for detecting PARP, 10% gel for detecting p-JNK, JNK1 and
β-actin, and 15% gel for detecting active caspase 3), and then
transferred to polyvinylidene fluoride membrane. The membrane was
blocked with TBS containing 5% milk and 0.05% Tween-20 for 2 h at
37°C and detected with various antibodies: Anti-PARP (dilution
1:500; catalog no. 556494; BD Pharmingen; BD Biosciences; overnight
at 4°C); anti-p-JNK (dilution 1:1,500; catalog no. 9255; Cell
Signaling Technology, Inc., overnight at 4°C); anti-JNK1 (dilution
1:1,000; catalog no. 110724; Abcam, overnight at 4°C); anti-β-actin
(dilution 1:5,000, catalog no. 60008-1-Ig; Protein Tech Group,
Inc.; 1 h at room temperature); and anti-active-caspase 3 (dilution
1:500; catalog no. 559565; BD Pharmingen; BD Biosciences; overnight
at 4°C). Subsequently, the membrane was washed three times for 5
min each with TBS containing Tween-20. Next, peroxidase-conjugated
goat anti-mouse immunoglobulin (Ig)G (catalog no. ZB 2305; Beijing
Zhongshan Golden Bridge Biotechnology Co., Ltd., Beijing, China) or
peroxidase-conjugated goat anti-rabbit IgG (catalog no. ZB 2301;
Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd.) was added
at a 1:5,000 dilution and incubated with the membrane at room
temperature for 30 min. The specific proteins were visualized using
Immobilon Western Chemiluminescent HRP Substrate (catalog no.
WBKLS0500; EMD Millipore, Billerica, MA, USA) using a Bio-Rad Image
station (Bio-Rad Laboratories, Inc., Hercules, CA, USA). Each
experiment was repeated at least three times and representative
results were presented.
Statistical analysis
Data are expressed as the mean ± standard deviation
and were analyzed with one-way analysis of variance followed by
Dunnett's multiple comparison test. Statistical analysis was
performed using SPSS software (version 19.0; IBM Corp., Armonk, NY,
USA). P<0.05 was considered to indicate a statistically
significant difference.
Results
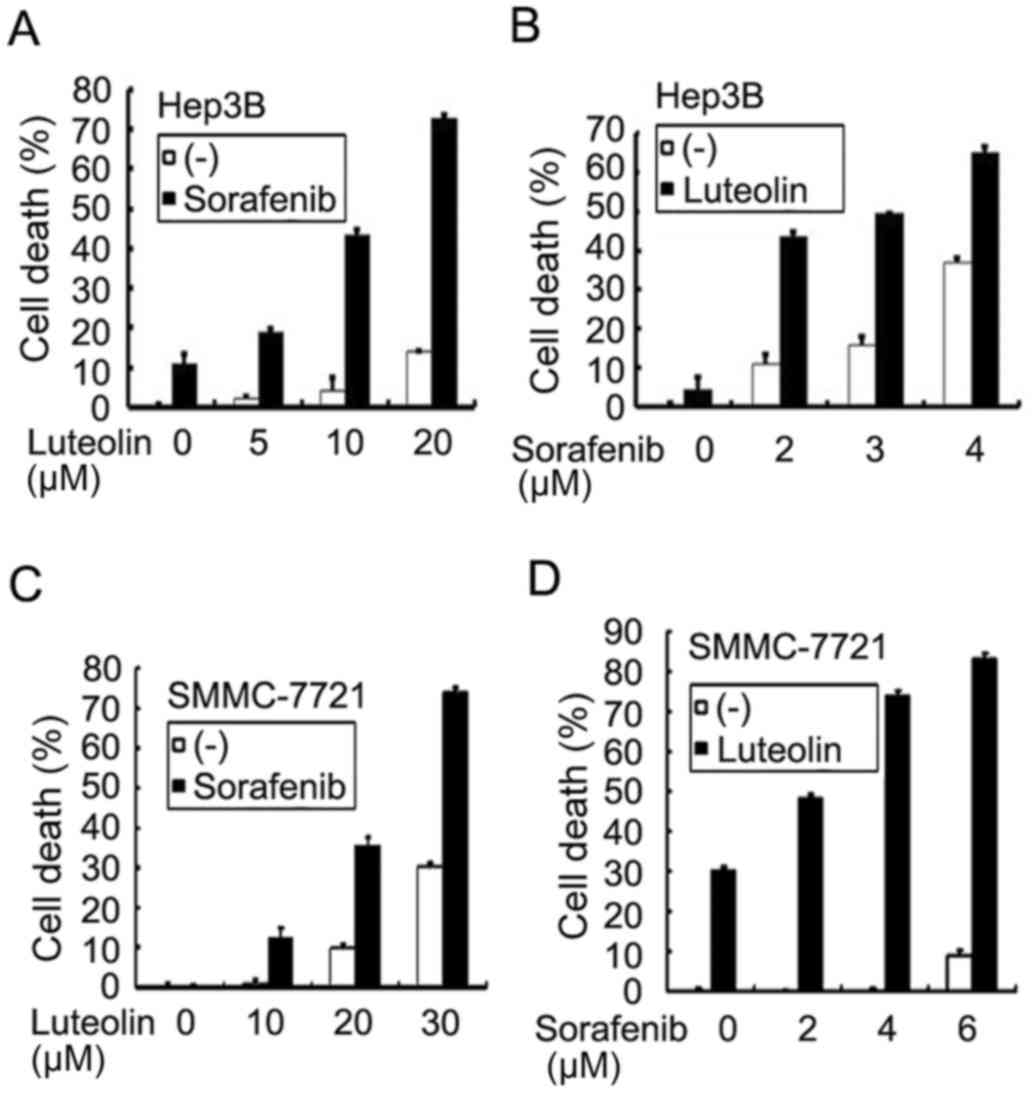
Sorafenib and luteolin combination
induces synergistic cytotoxicity in human hepatocellular carcinoma
cells
To investigate whether luteolin is able to enhance
the anticancer activity of sorafenib, Hep3B cells were treated with
increasing concentrations of luteolin (5–20 µM) and a fixed
concentration of sorafenib (2 µM) for 72 h. Cell death was measured
using an LDH-release cytotoxicity assay. The results revealed that
sorafenib at 2 µM alone caused ~10% cell death, and luteolin alone
had little cytotoxicity with <20% cell death even at the highest
evaluated dose of 20 µM. However, combining luteolin and sorafenib
increased cytotoxicity significantly in a dose-dependent manner
with increasing concentrations of luteolin (Fig. 1A). Conversely, a similar potentiation
of cytotoxicity was also identified with increasing concentrations
of sorafenib (2–4 µM) and a fixed luteolin dose (10 µM) (Fig. 1B). The combinatory cytotoxic effect of
luteolin and sorafenib was synergistic as evaluated using CI
analysis as described previously (17) (Table I).
In the human HCC cell line SMMC-7721, a similar dose-dependent
synergism with fixed concentrations of sorafenib or luteolin was
observed (Fig. 1C and D). These
results suggest that the combination of luteolin and sorafenib was
effective in sensitizing HCC cells to sorafenib-induced
cytotoxicity.
 | Table I.Synergistic interaction of sorafenib
and luteolin in human hepatocellular carcinoma Hep3B cells. |
Table I.
Synergistic interaction of sorafenib
and luteolin in human hepatocellular carcinoma Hep3B cells.
| Sorafenib
(µmol/l) | Luteolin
(µmol/l) | CI |
|---|
| 2 | 10 | 0.549 |
| 3 | 10 | 0.674 |
| 4 | 10 | 0.632 |
| 2 | 5 | 0.841 |
| 2 | 20 | 0.349 |
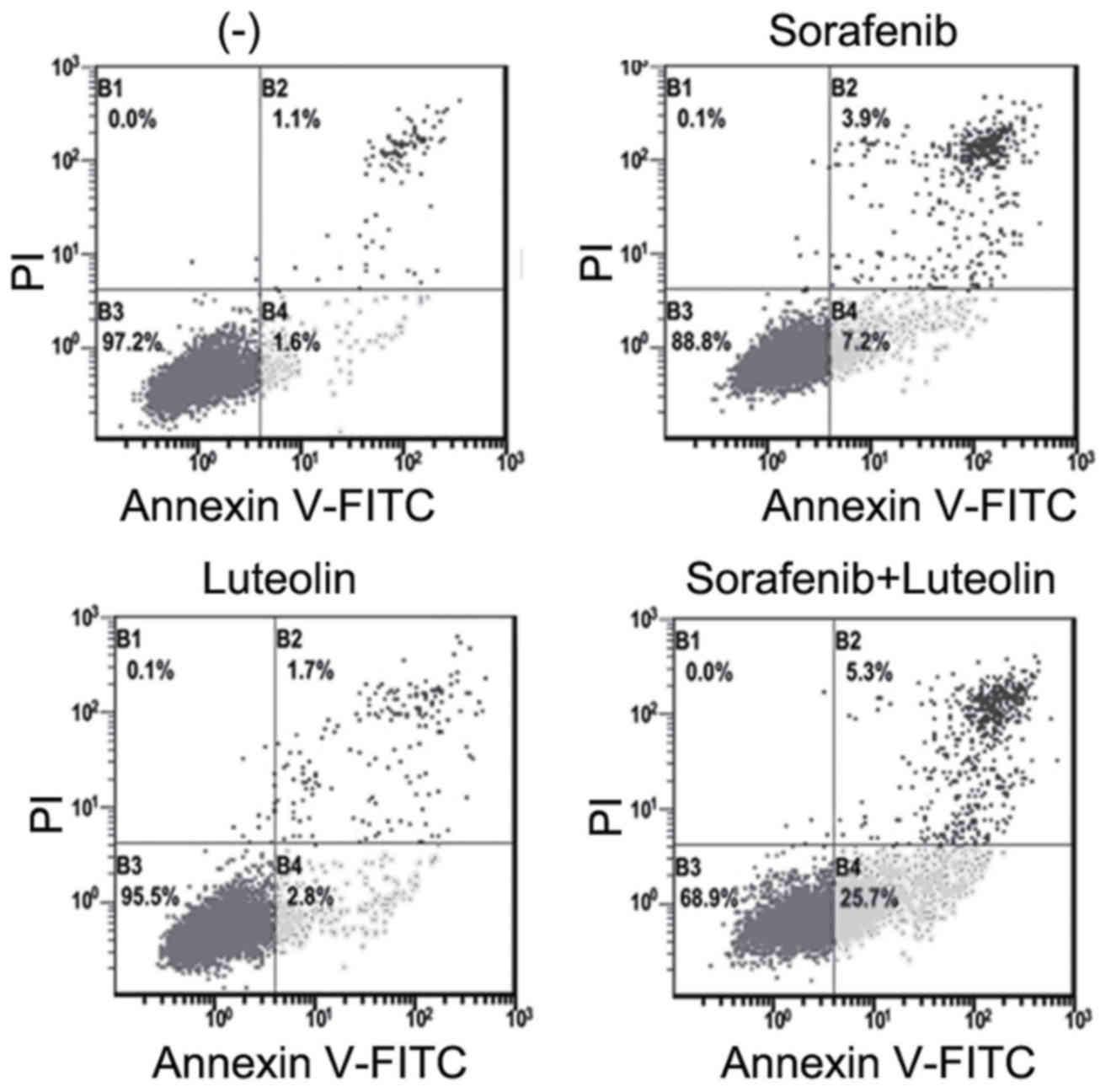
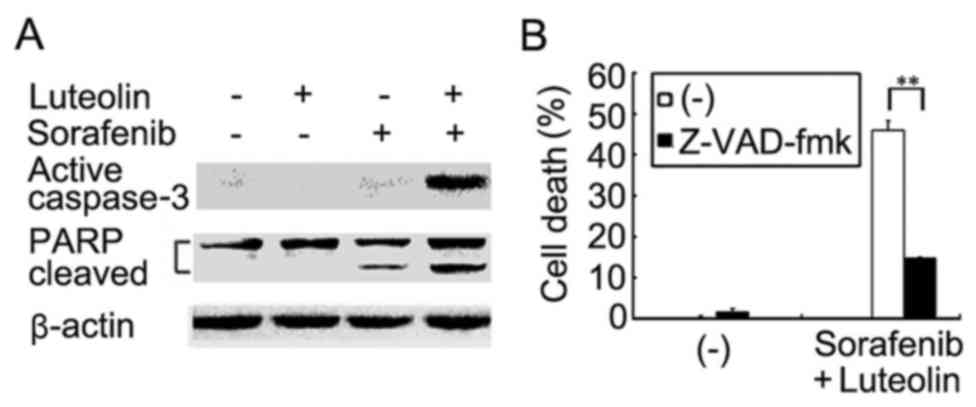
Potentiated cytotoxity induces by the
sorafenib and luteolin combination is achieved through apoptosis
potentiation
Luteolin and sorafenib are able to induce apoptosis
(18–21). Whether the enhanced cell death
observed in HCC cells co-treated with luteolin and sorafenib was
achieved through potentiation of apoptosis was then examined.
Apoptosis in Hep3B cells treated with sorafenib in the absence or
presence of luteolin was analyzed using flow cytometric assays.
Early (B4) and late (B2) apoptotic cells were markedly increased in
cells with sorafenib, and luteolin co-treatment compared with that
in the cells treated with either agent alone (Fig. 2). Furthermore, the results
demonstrated that activation of caspase 3 as demonstrated by the
detection of the active form of caspase 3 was markedly potentiated
in co-treated Hep3B cells (Fig. 3A).
Consistently, the cleavage of the caspase-3 substrate PARP in the
co-treated cells was also markedly enhanced (Fig. 3A). As expected, z-VAD-fmk
significantly suppressed the enhanced cytotoxicity in Hep3B cells
induced by co-treatment with sorafenib and luteolin (Fig. 3B). These results suggest that the
enhanced cytotoxicity induced by the sorafenib and luteolin
combination was due to the potentiation of apoptosis.
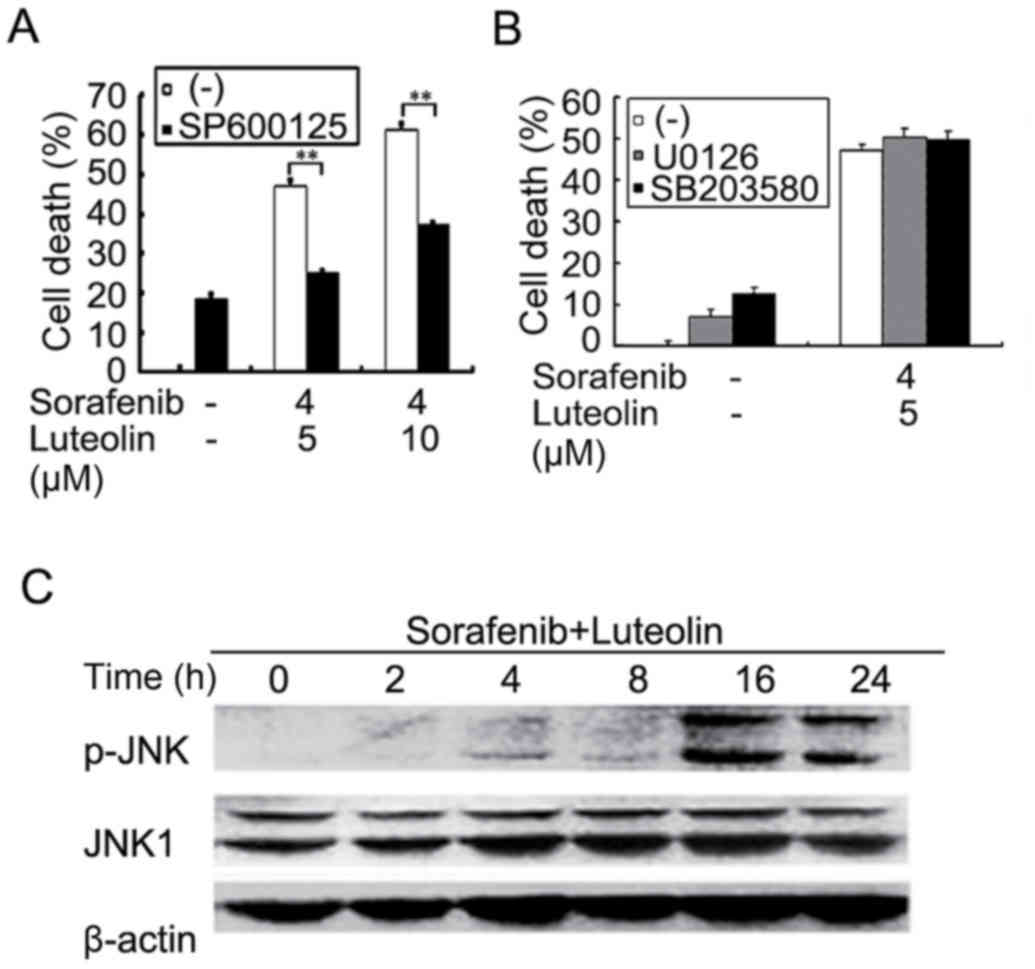
Sorafenib and luteolin co-treatment
potentiates the JNK activation pathway
The apoptotic cascade is tightly regulated in the
cell by multistep regulation mechanisms, including multiple
cellular signaling pathways. In order to dissect the mechanisms
underlying enhanced cytotoxicity induced by luteolin and sorafenib
combination, several inhibitors, including JNK inhibitor SP600125,
ERK inhibitor U0126, P38 inhibitor SB203580, and ROS scavengers BHA
and NAC were used to block corresponding pathways in sorafenib, and
luteolin co-treated Hep3B cells. The results demonstrated that only
SP600125 significantly inhibited the enhanced cytotoxicity induced
by sorafenib and luteolin co-treatment, indicating that activation
of JNK signaling pathway may be involved (Fig. 4A and B and data not shown). Indeed,
while sorafenib- or luteolin alone slightly activated JNK as
demonstrated, the sorafenib and luteolin co-treatment markedly
potentiated JNK activation (Fig. 4C
and data not shown). Altogether, these results suggest that the
cytotoxic synergy of sorafenib and luteolin combination is induced
by JNK-mediated apoptosis.
Discussion
In the present study, it was demonstrated that the
combination of sorafenib and luteolin synergistically induced
cytotoxicity in HCC cells. The enhanced cell death observed in
sorafenib and luteolin co-treated cells was accompanied by
potentiation of apoptosis. Furthermore, it was revealed that the
sorafenib and luteolin combination markedly activated JNK, and the
JNK inhibitor SP600125 significantly suppressed the synergistic
cytotoxicity. Thus, potentiation of JNK-mediated apoptosis
contributed to the enhancement of cancer cell death caused by
sorafenib and luteolin combination. To the best of our knowledge,
this is the first report to demonstrate that the combination of
sorafenib and luteolin is effective in killing human HCC cells.
As a candidate anticancer agent, luteolin has
presented apoptotic effects in various tumor cells including lung
cancer cells, hepatoma cells, pancreatic tumor cells, and leukemia
cells with no significant toxic effects in normal cells (12,22). The
combination of luteolin with numerous conventional
chemotherapeutics has been investigated in order to improve the
anticancer efficacy of treatments (15,19,20,23).
Thus, it was considered that luteolin may be combined with
targeted-therapy agent to provide efficacious treatment. To the
best of our knowledge, the present study demonstrated for the first
that the combination of luteolin and sorafenib kills human HCC
cells in a synergistic manner. The results indicate that luteolin
may be an ideal candidate for increasing the activity of sorafenib
in HCC therapy, which warrants further in vivo
investigation.
JNK is a main MAPK activated by extracellular
stimuli and intracellular stresses. JNK can be induced by the
MAP3K-MAP2K-JNK kinase signaling cascade or inactivated by a group
of MAPK phosphatases, of which protein-tyrosine-phosphatase MKP1
(MKP1) is a major JNK suppressor (24,25).
Depending on the intensity and duration of the damage signal, JNK
signaling may lead to either cell survival or cell death. JNK
activation is often the target for cell death signaling induced by
numerous chemotherapeutics, including lutoelin and sorafenib
(19,26,27). The
results of the present study revealed that JNK activation was
markedly potentiated in lutoelin and sorafenib co-treated cells,
and that the JNK inhibitor (SP600125) was able to protect cells
against cell death induced by the combination. Consistently, JNK
was reported to be required for the synergistic cytotoxicity
induced by the co-treatment of sorafenib and the proteasome
inhibitor bortezomib (28). Our
previous study demonstrated that luteolin triggers
superoxide-dependent rapid degradation of the JNK suppressor MKP1
thus activating JNK (19). The
mechanism underlying how the activation of JNK in lutoelin and
sorafenib co-treated cells is promoted warrants further
investigation.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (grant nos. 81172111 and
81372377) and the Science & Technology Department of Sichuan
Province, China (grant no. 2015JY0096).
References
|
1
|
Wilhelm S, Carter C, Lynch M, Lowinger T,
Dumas J, Smith RA, Schwartz B, Simantov R and Kelley S: Discovery
and development of sorafenib: A multikinase inhibitor for treating
cancer. Nat Rev Drug Discov. 5:835–844. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Liu L, Cao Y, Chen C, Zhang X, McNabola A,
Wilkie D, Wilhelm S, Lynch M and Carter C: Sorafenib blocks the
RAF/MEK/ERK pathway, inhibits tumor angiogenesis, and induces tumor
cell apoptosis in hepatocellular carcinoma model PLC/PRF/5. Cancer
Res. 66:11851–11858. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Llovet JM, Ricci S, Mazzaferro V, Hilgard
P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A,
et al: Sorafenib in advanced hepatocellular carcinoma. N Engl J
Med. 359:378–390. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S,
Kim JS, Luo R, Feng J, Ye S, Yang TS, et al: Efficacy and safety of
sorafenib in patients in the asia-pacific region with advanced
hepatocellular carcinoma: A phase iii randomised, double-blind,
placebo-controlled trial. Lancet Oncol. 10:25–34. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kane RC, Farrell AT, Saber H, Tang S,
Williams G, Jee JM, Liang C, Booth B, Chidambaram N, Morse D, et
al: Sorafenib for the treatment of advanced renal cell carcinoma.
Clin Cancer Res. 12:7271–7278. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Keating GM and Santoro A: Sorafenib: A
review of its use in advanced hepatocellular carcinoma. Drugs.
69:223–240. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gauthier A and Ho M: Role of sorafenib in
the treatment of advanced hepatocellular carcinoma: An update.
Hepatol Res. 43:147–154. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Birt DF, Hendrich S and Wang W: Dietary
agents in cancer prevention: Flavonoids and isoflavonoids.
Pharmacol Ther. 90:157–177. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Huang YT, Hwang JJ, Lee PP, Ke FC, Huang
JH, Huang CJ, Kandaswami C, Middleton E Jr and Lee MT: Effects of
luteolin and quercetin, inhibitors of tyrosine kinase, on cell
growth and metastasis-associated properties in A431 cells
overexpressing epidermal growth factor receptor. Br J Pharmacol.
128:999–1010. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Leung HW, Wu CH, Lin CH and Lee HZ:
Luteolin induced DNA damage leading to human lung squamous
carcinoma ch27 cell apoptosis. Eur J Pharmacol. 508:77–83. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bagli E, Stefaniotou M, Morbidelli L,
Ziche M, Psillas K, Murphy C and Fotsis T: Luteolin inhibits
vascular endothelial growth factor-induced angiogenesis; inhibition
of endothelial cell survival and proliferation by targeting
phosphatidylinositol 3′-kinase activity. Cancer Res. 64:7936–7946.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lin Y, Shi R, Wang X and Shen HM:
Luteolin, a flavonoid with potential for cancer prevention and
therapy. Curr Cancer Drug Targets. 8:634–646. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yan J, Wang Q, Zheng X, Sun H, Zhou Y, Li
D, Lin Y and Wang X: Luteolin enhances tnf-related
apoptosis-inducing ligand's anticancer activity in a lung cancer
xenograft mouse model. Biochem Biophys Res Commun. 417:842–846.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Reipas KM, Law JH, Couto N, Islam S, Li Y,
Li H, Cherkasov A, Jung K, Cheema AS, Jones SJ, et al: Luteolin is
a novel p90 ribosomal S6 kinase (RSK) inhibitor that suppresses
Notch4 signaling by blocking the activation of Y-box binding
protein-1 (YB-1). Oncotarget. 4:329–345. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yang MY, Wang CJ, Chen NF, Ho WH, Lu FJ
and Tseng TH: Luteolin enhances paclitaxel-induced apoptosis in
human breast cancer MDA-MB-231 cells by blocking STAT3. Chem Biol
Interact. 213:60–68. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang X, Ju W, Renouard J, Aden J, Belinsky
SA and Lin Y: 17-allylamino-17-demethoxygeldanamycin
synergistically potentiates tumor necrosis factor-induced lung
cancer cell death by blocking the nuclear factor-kappab pathway.
Cancer Res. 66:1089–1095. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhao L, Wientjes MG and Au JL: Evaluation
of combination chemotherapy: Integration of nonlinear regression,
curve shift, isobologram, and combination index analyses. Clin
Cancer Res. 10:7994–8004. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Broecker-Preuss M, Müller S, Britten M,
Worm K, Schmid KW, Mann K and Fuhrer D: Sorafenib inhibits
intracellular signaling pathways and induces cell cycle arrest and
cell death in thyroid carcinoma cells irrespective of histological
origin or braf mutational status. BMC Cancer. 15:1842015.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bai L, Xu X, Wang Q, Xu S, Ju W, Wang X,
Chen W, He W, Tang H and Lin Y: A superoxide-mediated
mitogen-activated protein kinase phosphatase-1 degradation and
c-Jun NH(2)-terminal kinase activation pathway for luteolin-induced
lung cancer cytotoxicity. Mol Pharmacol. 81:549–555. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ju W, Wang X, Shi H, Chen W, Belinsky SA
and Lin Y: A critical role of luteolin-induced reactive oxygen
species in blockage of tumor necrosis factor-activated nuclear
factor-kappaB pathway and sensitization of apoptosis in lung cancer
cells. Mol Pharmacol. 71:1381–1388. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kurosu T, Ohki M, Wu N, Kagechika H and
Miura O: Sorafenib induces apoptosis specifically in cells
expressing BCR/ABL by inhibiting its kinase activity to activate
the intrinsic mitochondrial pathway. Cancer Res. 69:3927–3936.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bai L, Chen W, Wang X, Ju W, Xu S and Lin
Y: Attenuating smac mimetic compound 3-induced NF-kappaB activation
by luteolin leads to synergistic cytotoxicity in cancer cells. J
Cell Biochem. 108:1125–1131. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Attoub S, Hassan AH, Vanhoecke B, Iratni
R, Takahashi T, Gaben AM, Bracke M, Awad S, John A, Kamalboor HA,
et al: Inhibition of cell survival, invasion, tumor growth and
histone deacetylase activity by the dietary flavonoid luteolin in
human epithelioid cancer cells. Eur J Pharmacol. 651:18–25. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wagner EF and Nebreda AR: Signal
integration by jnk and p38 mapk pathways in cancer development. Nat
Rev Cancer. 9:537–549. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
25
|
Haagenson K and Wu GS: Mitogen activated
protein kinase phosphatases and cancer. Cancer Biol Ther.
9:337–340. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Choi AY, Choi JH, Yoon H, Hwang KY, Noh
MH, Choe W, Yoon KS, Ha J, Yeo EJ and Kang I: Luteolin induces
apoptosis through endoplasmic reticulum stress and mitochondrial
dysfunction in Neuro-2a mouse neuroblastoma cells. Eur J Pharmacol.
668:115–126. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ou DL, Shen YC, Yu SL, Chen KF, Yeh PY,
Fan HH, Feng WC, Wang CT, Lin LI, Hsu C and Cheng AL: Induction of
DNA damage-inducible gene GADD45beta contributes to
sorafenib-induced apoptosis in hepatocellular carcinoma cells.
Cancer Res. 70:9309–9318. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yu C, Friday BB, Lai JP, Yang L, Sarkaria
J, Kay NE, Carter CA, Roberts LR, Kaufmann SH and Adjei AA:
Cytotoxic synergy between the multikinase inhibitor sorafenib and
the proteasome inhibitor bortezomib in vitro: Induction of
apoptosis through Akt and c-Jun NH2-terminal kinase pathways. Mol
Cancer Ther. 5:2378–2387. 2006. View Article : Google Scholar : PubMed/NCBI
|