Introduction
Intrauterine adhesions (IUA) refer to the
endometrial fibrosis caused by endometrial injury in operative
hysteroscopy (1). Endometrial
injuries may lead to recurrent miscarriages, infertility,
amenorrhea, abnormal placentation, dysmenorrhea and abnormal
uterine bleeding, thus being detrimental to the health of affected
women (2). Expression levels of
transforming growth factor (TGF)-β1, epidermal growth factor (EGF),
basic fibroblast growth factor and platelet-derived growth factor
(PDGF)-BB were found to be significantly increased in exudates in
patients with IUA following surgery (3,4), which in
turn promoted the growth of fibroblasts and the formation of
adhesions. Despite advances in intraoperative techniques, including
minimizing trauma of the healthy myometrium and endometrium, and
reducing the usage of electrosurgery (5), the incidence of IUA caused by surgery
remains high. Therefore, the development of novel approaches to
inhibit the formation of post-surgical IUA is required.
A variety of novel therapies for IUA have been
developed. Estrogen is the most important female sex hormone, which
serves pivotal functions in the regulation and development of the
reproductive system of females and the formation of secondary sex
characteristics. It has been reported that postoperative estrogen
therapy may be used to prevent recurrent adhesions (6). However, the recurrence rate of IUA
accounted for 62.5% in patients with severe IUAs (7). Transplantation of bone marrow
mesenchymal stem cells (MSCs) may promote the regeneration of the
injured uterus and abnormal endometrium (8–10). However, the
application of MSCs in the treatment of IUA is limited due to its
low efficiency in promoting endometrial repair and regeneration. It
has been reported that human endometrial stem cells (EnSCs) derived
from the endometrium may contribute to the repair of the injured
endometrium by inducing angiogenesis (11), highlighting the potential of using
ESCs for the treatment of IUA.
In the present study, a rat model of IUA was
established. Additionally, the effects of hESCs, estrogen and the
combination of estrogen plus hESCs in the treatment of IUA were
assessed.
Materials and methods
Patients
A total of 30 patients aged 25–35 years (mean age:
31) with moderate to severe IUA underwent IUA dissection in the
Affiliated Yantai Yuhuangding Hospital of Qingdao University
(Shandong, China) between January 2016 and December 2016 and were
enrolled in the present study. The criteria for patient inclusion
were as follows: Initial hysteroscopic adhesions score in line with
moderate to severe IUA [American Fertility Society score (12) ≥5]; age ≤40 years; hysteroscopic
examination following surgery; and a complete record of the medical
history. A total of 30 females aged 23–34 years (mean age: 28) with
normal endometrium who received hysteroscopic examination were
selected as controls. Endometrial tissue was collected by
curettage. All participants provided written informed consent and
the study was approved by the Ethics Committee of The Affiliated
Yantai Yuhuangding Hospital of Qingdao University.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Expression levels of EGF and PDGF-BB in endometrial
tissue were detected using RT-qPCR. Additionally, expression levels
of epithelial membrane antigen (EMA), Thy-1 membrane glycoprotein
(THY-1), cytokeratin (CK), collagen type 1 (Col I), integrin α-6
(CD49f), vimentin and 5B5 in ESCs were assessed using RT-qPCR.
Total RNA was extracted from endometrial tissue and ESCs using
TRIzol reagent (Thermo Fisher Scientific, Inc., Waltham, MA, USA).
The concentration and quality of RNA were assessed using the
260/280 nm absorbance ratio of 1.8–2.0. Total RNA was reverse
transcribed using a reverse transcription kit (Takara Bio, Inc.,
DRR047A) according to the manufacturer's protocol. RT-qPCR was
performed using LightCycler®480 SYBR Green Master mix
(Roche Diagnostics, Basel, Switzerland). Primers used for the PCR
are listed in Table I. All primers
were synthesized by Sangon Biotech Co., Ltd. (Shanghai, China).
GAPDH was used as an endogenous control. Thermocycling conditions
were as follows: 95°C for 30 sec, followed by 40 cycles of 95°C for
10 sec, 60°C for 15 sec and 72°C for 15 sec, and finally, 60°C for
15 sec. Relative expression levels were determined using the
2−ΔΔCq method (13).
 | Table I.Primers used in the study. |
Table I.
Primers used in the study.
| Gene name | Primers | Sequence (5′-3′) |
|---|
| EGF | Sense |
CAGGGAAGATGACCACCACT |
|
| Antisense |
CAGTTCCCACCACTTCAGGT |
| PDGF-BB | Sense |
CGCGGATCCACCATGAATCGCTGCTGG |
|
| Antisense |
CCGCTCGAGCTAGGCTCCAAGGGTCTC |
| EMA | Sense |
TGGATGTGCTTGATAAGCGG |
|
| Antisense |
ACCATGTCCTTTCCAGTGTGT |
| CK | Sense |
GGTCATGGCCGAGCAGAA |
|
| Antisense |
TTCAGTCCGGCTGGTGAAC |
| CD49f | Sense |
CCTGCTGCTGCTCCTCACA |
|
| Antisense |
GTAACAACTGTTGCGGGTTTAGG |
| THY-1 | Sense |
ATCGCTCTCCTGCTAACAGTC |
|
| Antisense |
CTCGTACTGGATGGGTGAACT |
| Col I | Sense |
AATCCTCTCGTCAAAACTGAAGG |
|
| Antisense |
CCATCTCGCTTATCCAACAATGA |
| 5B5 | Sense |
TGACAGCGACAAGAAGTG |
|
| Antisense |
CAGTGAAGCGGTACATAGG |
| Vimentin | Sense |
CCAAACTTTTCCTCCCTGAACC |
|
| Antisense |
GTGATGCTGAGAAGTTTCGTTGA |
| GAPDH | Sense |
GGCTCTCCAGAACATCATCC |
|
| Antisense |
TGTCATCATATTTGGCAGGT |
Western blot analysis
Total protein was extracted from the endometrial
tissues and EnSCs, and quantified using a bicinchoninic acid assay
(Pierce; Thermo Fisher Scientific, Inc.). A total of 30 µg
protein/lane was separated by SDS-PAGE (10% gels) and transferred
onto polyvinylidene difluoride membranes. The membranes were then
blocked with 5% non-fat milk. for 1 h at room temperature.
Following blocking, the membranes were incubated with the following
primary antibodies: Rabbit anti-human EGF antibody (cat. no.
DF2225, 1:2,000; Affinity Biosciences, Cincinnati, OH, USA), rabbit
anti-human PDGF-BB (cat. no. orb303833, 1:2,000; Biorbyt,
Cambridge, UK,), rabbit anti-human EMA antibody (cat. no. orb31710;
1:2,000; Biorbyt), rabbit anti-human CK antibody (cat. no. BF0141,
1:1,000; Affinity Biosciences), rabbit anti-human CD49f antibody
(cat. no. orb39949, 1:1,000; Biorbyt), rabbit anti-human THY-1
(cat. no. orb136416, 1:2,000; Biorbyt), rabbit anti-human Col I
antibody (cat. no. orb345868, 1:2,000; Biorbyt), rabbit anti-human
5B5 antibody (cat. no. orb241612, 1:1,000; Biorbyt), rabbit
anti-human vimentin antibody (cat. no. AF7013, 1:2,000; Affinity
Biosciences), rabbit anti-rat estrogen receptor (ESR1) (cat. no.
DF6094, 1:2,000; Affinity Biosciences) and rabbit anti-rat matrix
metalloproteinase (MPP)-9 (cat. no. orb100446, 1:1,000; Biorbyt)
overnight at 4°C. Membranes were washed three times with
Tris-buffered-saline with Tween-20 (TBST) for 10 min. Following the
primary incubation, membranes were incubated with horseradish
peroxidase-labeled goat anti-rabbit antibody (cat. no. orb345943,
1:1,500; Biorbyt) at room temperature for 1 h. Membranes were then
washed three times with TBST. Protein bands were visualized using
enhanced chemiluminescence (ECL; Merck KGaA). The densitometric
analysis for the quantification of the bands was performed using
ImageJ software (version 2.1; National Institutes of Health,
Bethesda, MD, USA). β-actin was used as an endogenous control.
Isolation and culture of human
EnSCs
Endometrial tissue was obtained from ovulating women
without endometrial disease. All participants provided written
informed consent and the study was approved by the Ethics Committee
of The Affiliated Yantai Yuhuangding Hospital of Qingdao
University. EnSCs were prepared as reported by Ebrahimi-Barough
et al (14,15). Endometrial tissue was rinsed with PBS
and cut into 1 mm3 pieces. Tissues were then incubated
with 5 ml digestion solution in a 25 cm2 cell culture
flask [0.25% trypsin (cat. no. T8150; Beijing Solarbio Science
& Technology Co, Ltd., Beijing, China) + 0.02%
ethylenediaminetetraacetic acid (cat. no. C1033; Beijing Solarbio
Science & Technology Co., Ltd.) + 300 µg/ml type II collagenase
(cat. no. C8150; Beijing Solarbio Science and Technology Co.,
Ltd.)] under agitation (80 rpm) for 45–60 min at 37°C. Samples were
filtered with 80 mesh screen and collect the filtrate. Red blood
cells were removed with red blood cell lysis buffer (cat. no.
ab204733; Abcam). When the cells were ~80% confluent, they were
used for subsequent experiments.
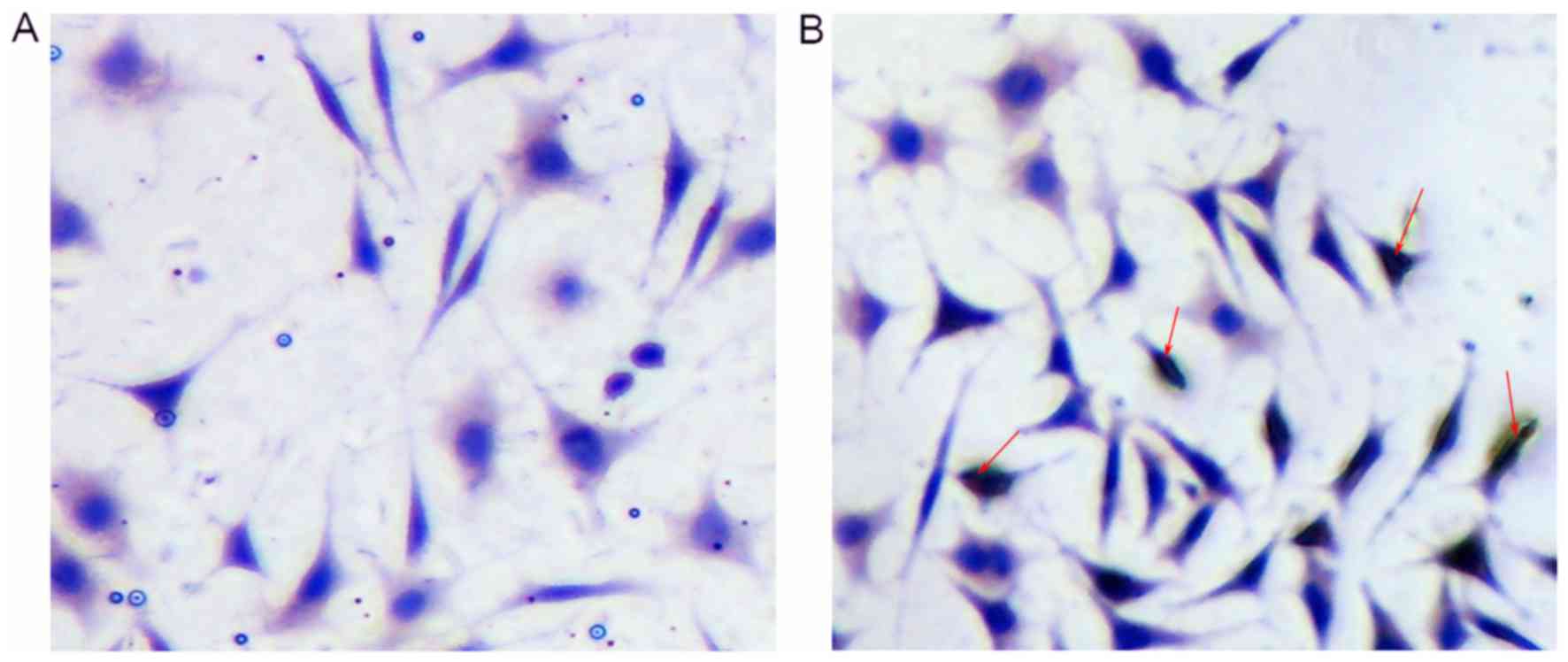
Immunocytochemistry
EnSCs were fixed with 4% paraformaldehyde at room
temperature for 20 min and permeabilised with 0.1% Triton in PBS at
room temperature for 20 min. The slides were then blocked using 5%
goat serum in TBS and incubated with primary antibody against CD90
(cat. no. ab106934, 1:200; Abcam) overnight at 4°C. Following the
primary incubation, cells were incubated with horseradish
peroxidase secondary antibody (cat. no. ab95376; rabbit anti-rat
immunoglobulin; 1:200; Abcam) at 37°C for 4 h. Cells were washed
with TBST for 10 min. The negative controls were incubated only
with the secondary antibody. The slides were stained with
3,3-diaminobenzidine tetrahydrochloride for 10 min, counterstained
with hematoxylin, subjected to gradient alcohol dehydration and
mounted with neutral gum. Cells were observed under an optical
microscope (×400 magnification).
Model establishment and treatment
A total of 50 specific pathogen-free (SPF) female
Sprague Dawley rats (weight, 200–220 g, 8 weeks old) were purchased
from the Shanghai Institutes for Biological Sciences, Chinese
Academy of Science (Shanghai, China). The animals were maintained
in a 12–12 h light-dark cycle at a temperature of 22±1°C with free
access to food and water in a specific pathogen-free environment. A
total of 50 rats were randomly divided into 5 groups with 10 rats
in each group. A rat model of IUA was established by scraping the
uterine horn to mimic the cause of IUA in humans. The model was
established using the methods described by Tang et al
(16). Rats in the control group were
subjected to a sham surgery. At day 7 following the establishment
of the model, rats in the EnSCs group were subcutaneously injected
with 1 ml EnSCs, rats in estrogen group were subjected to
subcutaneous injection of estradiol benzoate (0.5 mg/kg; Hangzhou
Animal Pharmaceutical Factory, China) in PBS according to previous
studies (17) and rats in the E+EnSCs
group received an injection of estradiol benzoate (0.5 mg/kg) and
EnSCs (1 ml). Rats (n=5/group) were sacrificed 1 week after IUA and
5 weeks following IUA. Uterine tissue was collected from both sides
of the uterus and 2 ml of blood was extracted. Blood samples were
centrifuged at 3,000 × g at 4°C for 10 min. Serum was stored at
−80°C. The study was approved by the Animal Ethics Committee of The
Affiliated Yantai Yuhuangding Hospital of Qingdao University.
Hematoxylin and eosin staining
Uterine tissue was fixed in 10% neutral formaldehyde
and embedded in paraffin. Paraffin-embedded tissue samples were cut
into 5-µm sections. The tissue sections were deparaffinized in
xylene at room tempetature and rehydrated in a descending ethanol
series (100% for 5 min, 95% for 1 min, 80% for 5 min and 75% for 5
min). Hematoxylin and eosin staining was performed using the
routine method (18). Following
dehydration, sections were treated with xylene for 2 times. Tissue
sections were mounted with neutral resin and observed under optical
microscopy (×200 magnification) (Olympus BX51; Olympus Corporation,
Tokyo, Japan).
ELISA
The total protein extracted from the blood samples
of the experimental rat groups was used to determin the serum
concentrations of β-estradiol (E2) (cat. no. KGE014), TGF-β1 (cat.
no. MB100B), EGF (cat. no. DY3214) and PDGF-BB (cat. no. MBB00), as
detected using ELISA kits (R&D Systems, Inc., Minneapolis, MN,
USA), according the manufacturer's protocol.
Statistical analysis
Data were analyzed using SPSS software (version
19.0; IBM Corp., Armonk, NY, USA). The relevant data are expressed
as the mean ± standard deviation. Results were analyzed using
Student's t-test when only two groups were compared. Multiple
comparisons between more than two groups were performed by one way
analysis of variance followed by least significant difference or
Kruskal-Wallis tests. P<0.05 was considered to indicate a
statistically significant difference.
Results
mRNA and protein expression levels of
EGF and PDGF-BB in IUA tissues
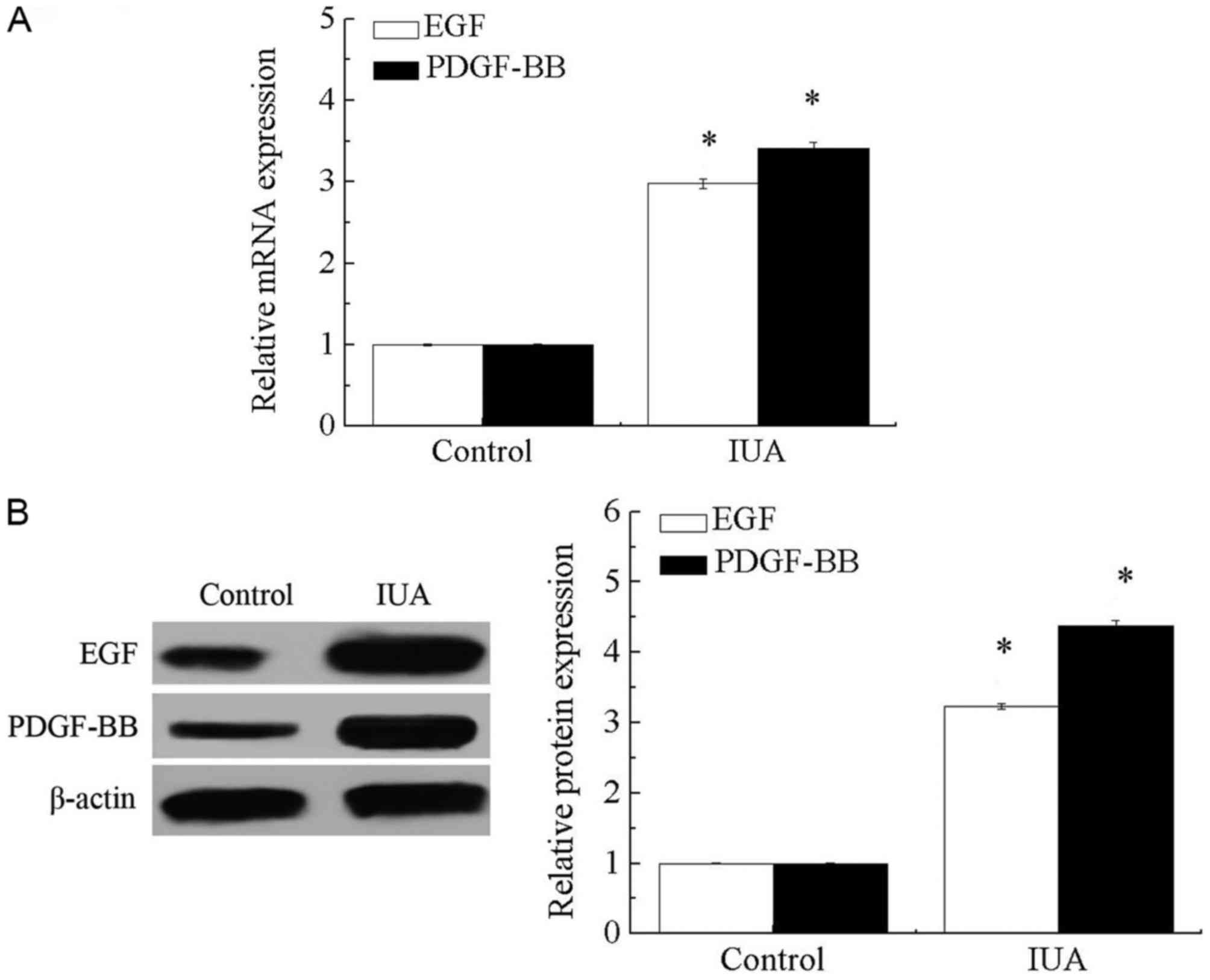
As presented in Fig. 1A
and B, mRNA and protein levels of EGF and PDGF-BB were
significantly increased in endometrial tissue derived from patients
with IUA compared with that in healthy individuals (P<0.05).
These results suggest that endometrial injury may significantly
increase the expression levels of EGF and PDGF-BB.
Expression levels of EMA, CK, CD49f,
THY-1, Col I, 5B5 and vimentin in EnSCs
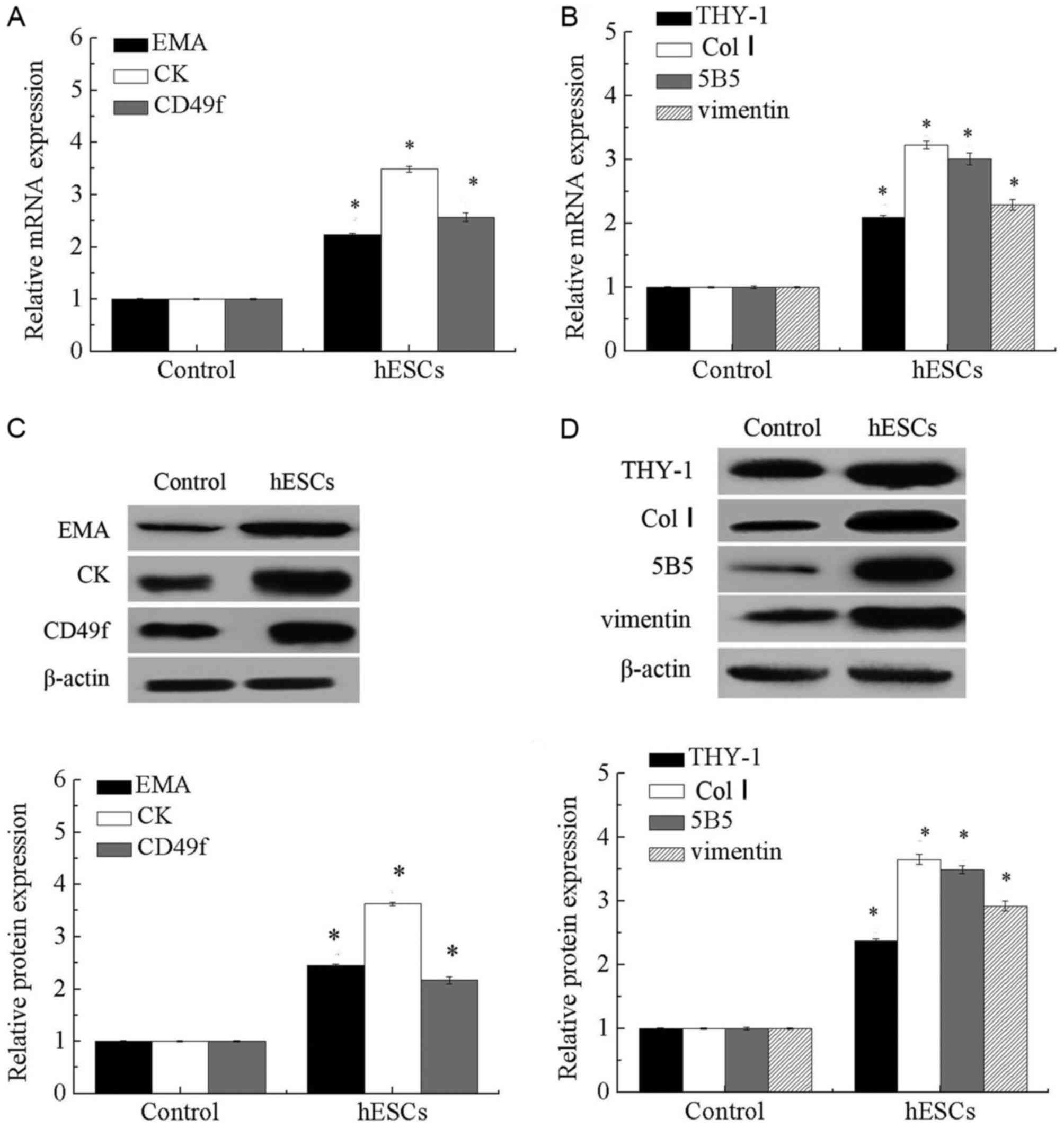
As presented in Fig.
2, expression levels of endometrial epithelial stem
cell-associated genes, including CK, EMA and CD49f, and endometrial
stromal cell-associated genes, including THY-1 (CD90), Col I, 5B5
and vimentin, were significantly increased in EnSCs compared with
that in the controls (P<0.05).
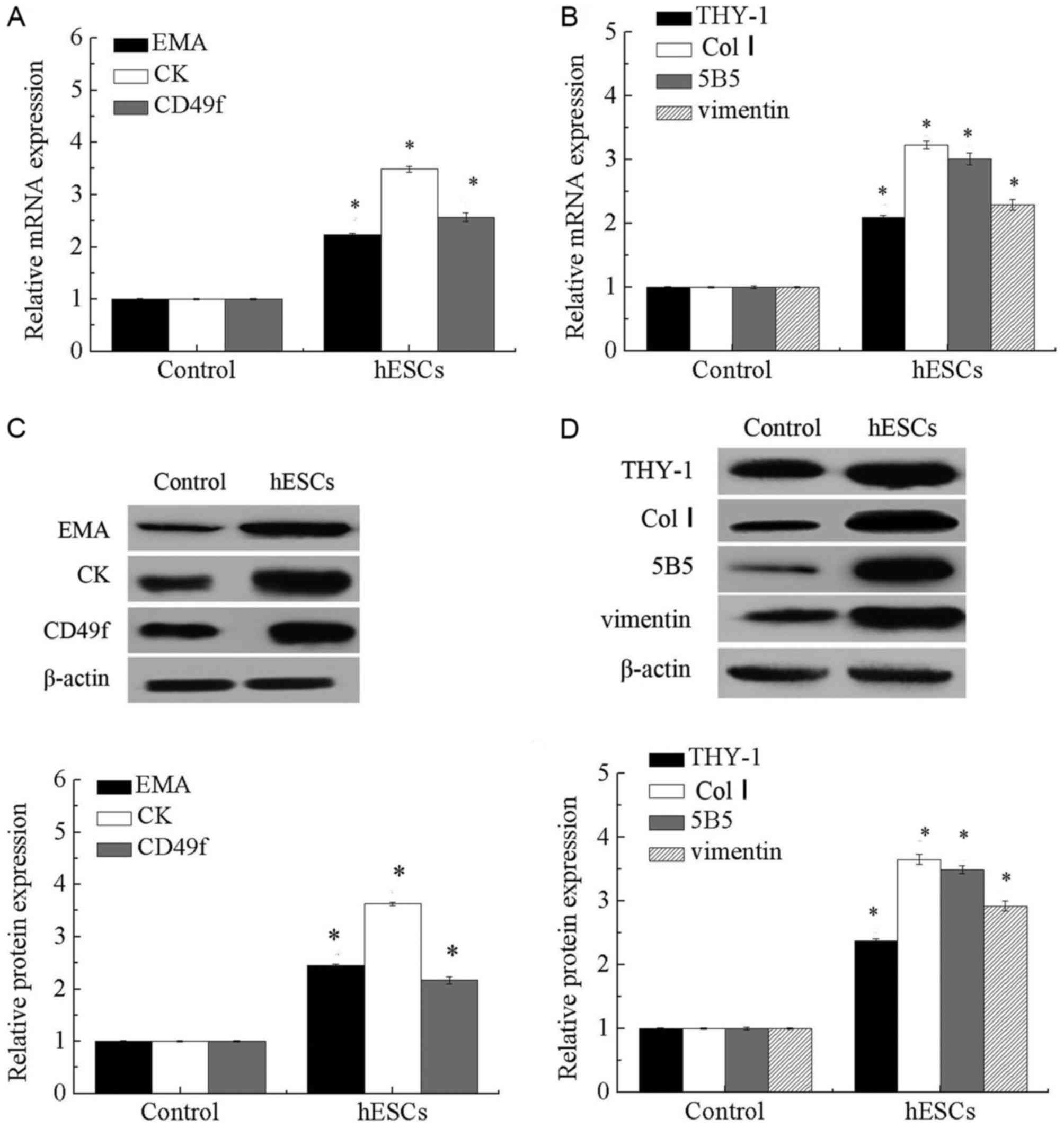 | Figure 2.Expression of EMA, CK, CD49f, THY-1,
Col I. 5B5 and vimentin in EnSCs. (A) mRNA levels of EMA, CK and
CD49f in EnSCs. (B) mRNA levels of THY-1, Col I, 5B5 and vimentin
in EnSCs. (C) Protein expression of EMA, CK and CD49f in EnSCs. (D)
Protein expression of THY-1, Col I, 5B5 and vimentin in EnSCs.
*P<0.05 vs. control. EMA, epithelial membrane antigen; CK,
cytokeratin; Col I, collagen type 1; CD49F, integrin α-6; THY-1,
Thy-1 membrane glycoprotein; EnSCs, endometrial stem cells. |
Characterization of isolated
EnSCs
Isolated EnSCs were positive for CD90, as assessed
using immunocytochemistry (Fig. 3A and
B).
Morphological changes of the
endometrium detected by hematoxylin and eosin staining
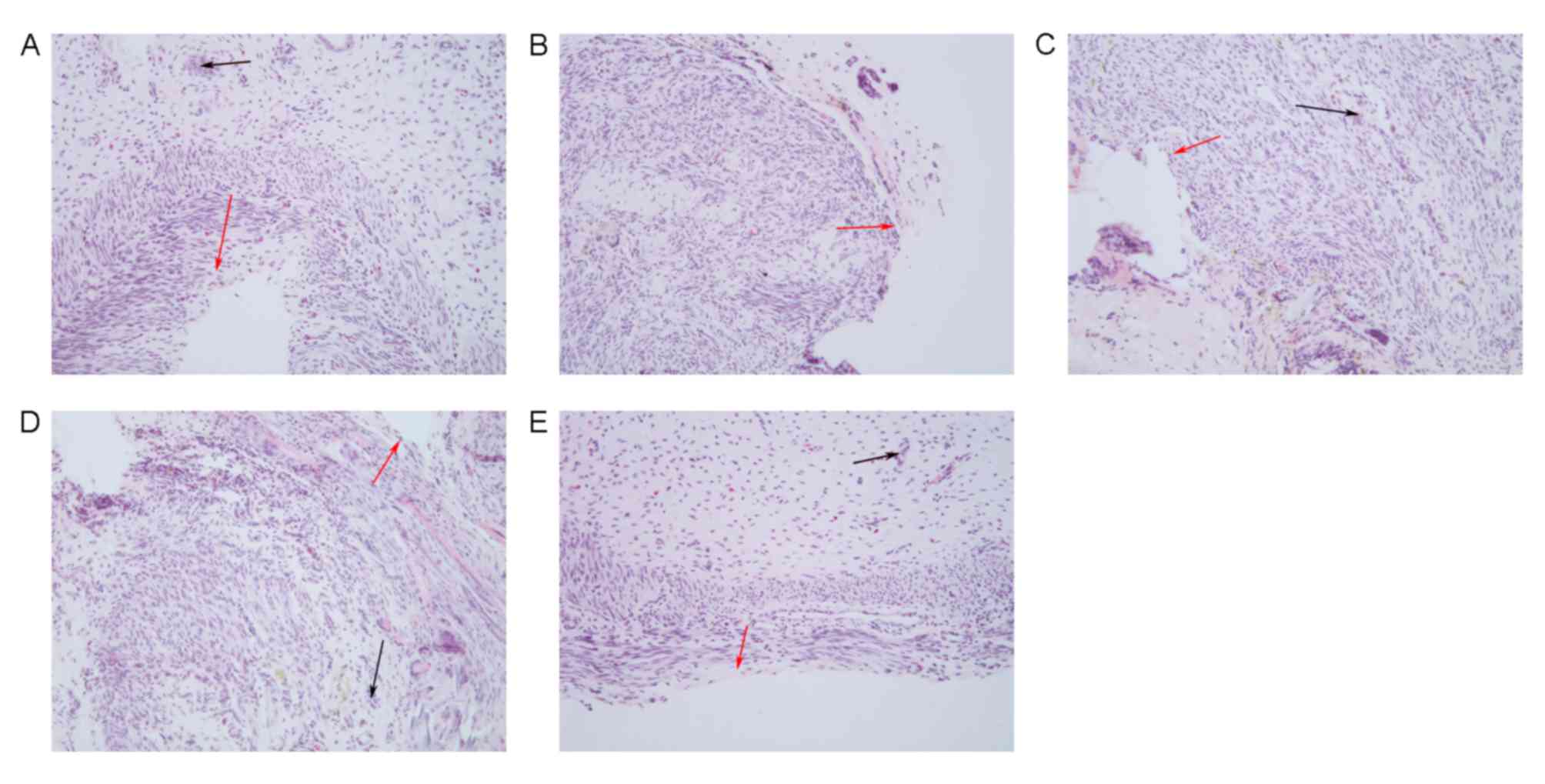
Hematoxylin and eosin staining demonstrated that the
uterine cavity of the control group was covered by columnar
epithelium and oval glands. In the model group, the uterine cavity
was covered with flat columnar epithelial cells or stratified flat
epithelial cells, and glands were rare. The number of endometrial
glands in the estrogen, EnSCs and E+EnSCs groups was increased, and
the newly formed glands were round or oval. No significant
difference in the number of glands was detected between the EnSCs
and estrogen groups. Newly formed glands were detected in the
E+EnSCs group (as indicated by the black arrows; Fig. 4). These results suggest that treatment
efficacy in the E+hESCs group may be improved compared with that in
the remaining groups.
Expression levels of PDGF-BB, E2, EGF
and TGF-β1 in a rat model of IUA
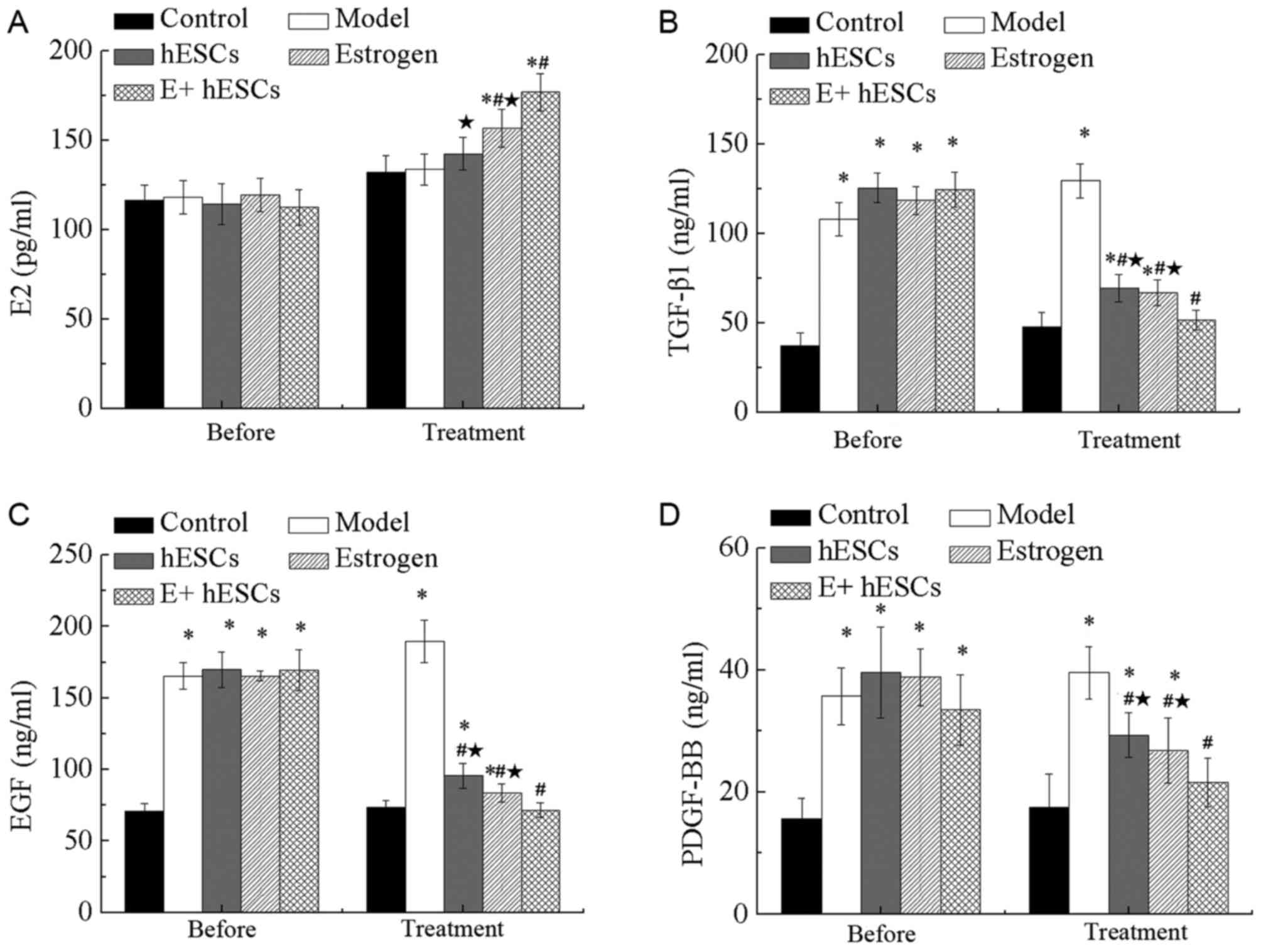
As presented in Fig.
5A, no significant difference in the expression of E2 was
detected 1 week after IUA. The results demonstrated that the levels
of serum E2 in the estrogen, EnSCs and E+EnSCs groups were
significantly higher than that in the control group (P<0.05).
However, no significant differences were detected between the model
and control groups. Additionally, the expression of E2 was
significantly increased in the estrogen and E+EnSCs groups compared
with that in the model group (P<0.05). Additionally, a
significant decrease in the E2 content was detected in the EnSCs
and estrogen groups compared with that in the E+EnSCs group
(P<0.05; Fig. 5A).
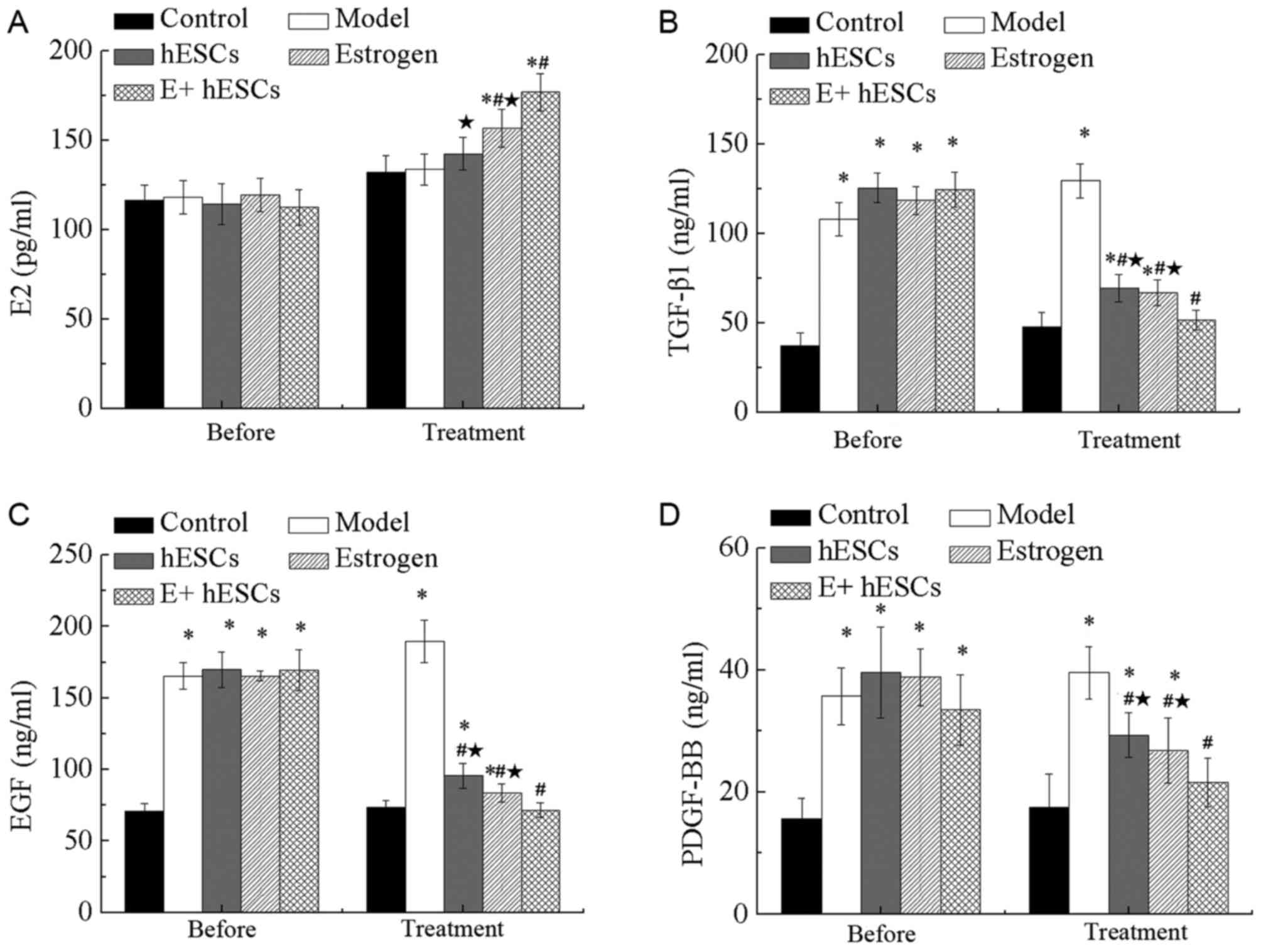 | Figure 5.Serum levels of E2, TGF-β1, EGF and
PDGF-BB in a rat model of intrauterine adhesions. Expression of (A)
E2, (B) TGF-β1, (C) EGF and (D) PDGF-BB in the serum of rats.
*P<0.05 vs. control; #P<0.05 vs. model; *P<0.05
vs. E+EnSCs. E+EnSCs, estrogen plus endometrial stem cells; EGF,
epidermal growth factor; PDGF-BB, platelet-derived growth
factor-BB; TGF-β1, transforming growth factor-β1; E2, β-estradiol.
Before, 1 week after IUA; Treatment, 5 weeks after IUA. |
One week after IUA, the levels of EGF, TGF-β1 and
PDGF-BB were significantly increased in the model, EnSCs, estrogen
and E+EnSCs groups compared with those in the control group
(P<0.05; Fig. 5B-D). The levels of
TGF-β1, EGF and PDGF-BB were significantly decreased in the EnSCs,
estrogen and E+EnSCs groups compared with those in the model group
at 4 weeks post-treatment (P<0.05; Fig. 5B-D). No significant difference in the
expression of EGF, TGF-β1 and PDGF-BB was detected between the
EnSCs and estrogen groups (Fig.
5B-D). Additionally, a significant decrease in the levels of
TGF-β1, EGF and PDGF-BB was detected in the E+EnSCs group compared
with that in the EnSCs and estrogen groups (P<0.05; Fig. 5B-D).
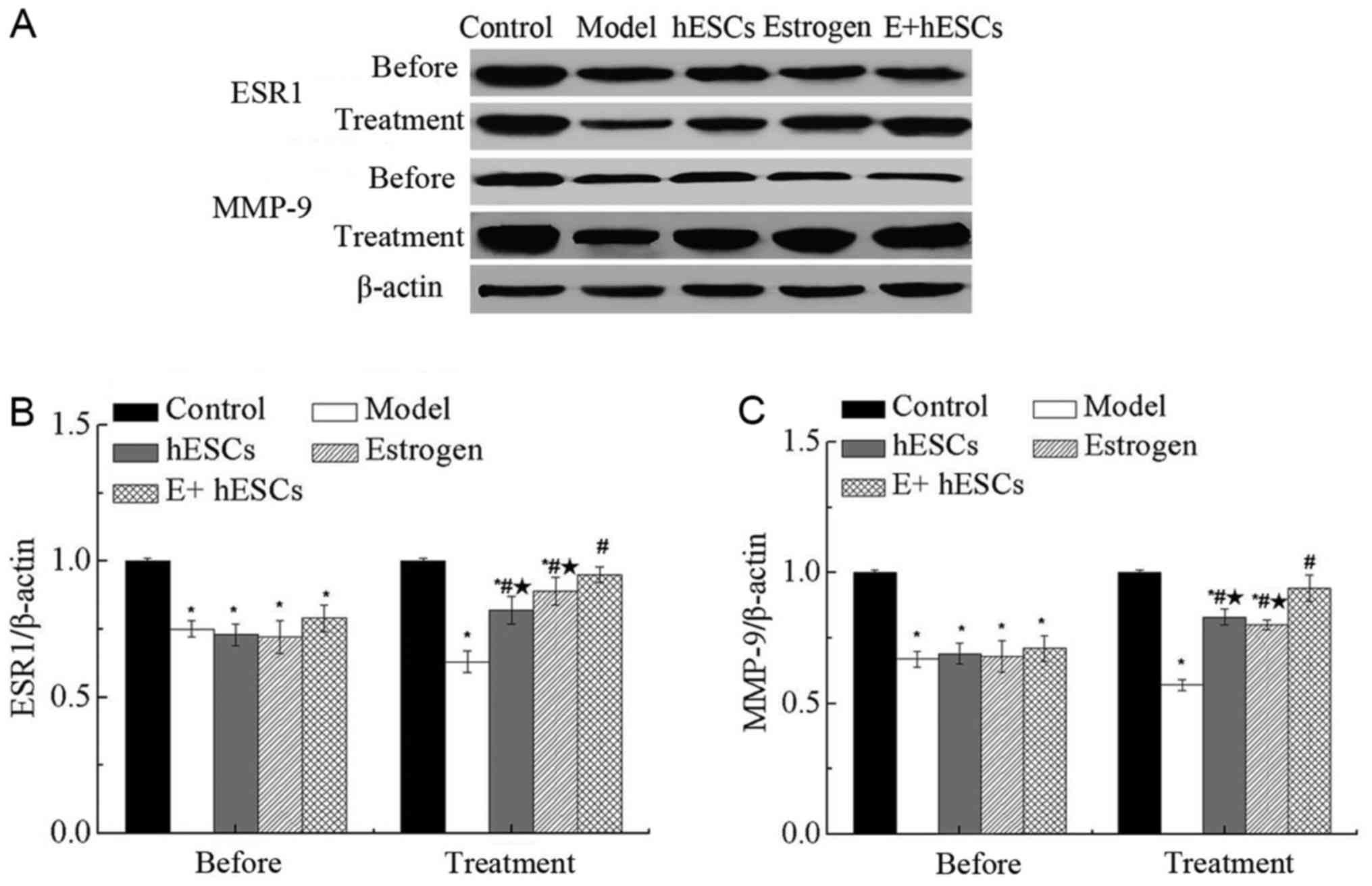
Expression of ESR1 and MMP-9 in
endometrium in a rat model of IUA
One week after IUA, the expression levels of ESR1
and MMP-9 were significantly decreased in the model, EnSCs,
estrogen and E+EnSCs groups compared with those in the control
group (P<0.05; Fig. 6A-C), as
assessed using western blot analysis. The expression levels of ESR1
and MMP-9 were significantly increased in the estrogen, EnSCs and
E+EnSCs groups compared with those in model group at 5 weeks after
IUA (P<0.05; Fig. 6B and C). No
significant difference in expression levels of ESR1 and MMP-9 were
detected between the estrogen and EnSCs groups at 5 weeks after
IUA. However, the expression levels of ESR1 and MMP-9 were
significantly decreased in the estrogen and EnSCs groups compared
with those in the E+EnSCs group (P<0.05; Fig. 6B and C).
Discussion
PDGF-BB has important functions in endometrial
tissue remodeling (19). As a member
of the EGF family, EGF determines cell survival, proliferation,
differentiation and migration through interacting with the EGF
receptor. EGF has also been found to be important for organ repair
and wound healing (20). In the
present study, expression levels of EGF and PDGF-BB in IUA tissues
were significantly increased compared with those in the controls.
Additionally, serum levels of EGF and PDGF-BB in rats with IUA were
significantly increased compared with those of the controls. These
results suggest that EGF and PDGF-BB may be involved in the
development of IUA. Upregulation of TGF-β is associated with the
development of fibrotic diseases (21), and endogenous TGF-β is essential for
hypertrophic remodeling and the pathogenesis of cardiac fibrotic
remodeling (22). In the present
study, it was identified that serum TGF-β level significantly
increased in rats with IUA compared with that in the sham surgery
group. These results suggest that PDGF-BB, EGF and TGF-β may be
involved in the development of IUA.
Estrogen is able to increase the number of cells
during endometrial injury and promote the regeneration of the
uterine endometrium (23–25). In the present study, the level of E2
was significantly increased in the serum of rats with IUA compared
with that in the controls, suggesting an effect of estrogen in the
repair of intrauterine adhesions. Estrogen has been widely used in
the prevention of IUA following operative hysteroscopy. Roy et
al (26) reported that estrogen
treatment reduced the incidence rate of IUA from 6.9 to 0%. In the
present study, estrogen treatment significantly prevented the
IUA-mediated increase in the serum levels of TGF-β1, EGF and
PDGF-BB, indicating that estrogen may inhibit the development of
IUA. Additionally, the serum levels of ESR1 were significantly
decreased in rats with IUA, whereas the level of ESR1 was
significantly increased following estrogen treatment, also
indicating that estrogen may inhibit the development of IUA. MMP-9
serves an important function in the remodeling of the endometrium
(27). In the present study, the
expression level of MMP-9 was significantly decreased in the rats
with IUA compared with that in the controls. Additionally,
morphological changes induced by IUA were partially reversed by
estrogen treatment. These results suggest that estrogen may
regulate the development of IUA.
Several studies (28–30) have reported that EnSCs may
contribute to endometrial repair. Low proliferation and
differentiation rate of EnSCs may lead to a variety of endometrial
diseases, including endometriosis, endometrial polyps or even
endometrial cancer (31). In the
present study, EnSCs were isolated from ovulating women without
endometrial disease, and the results demonstrated that the
expression levels of endometrial epithelial stem cell-associated
genes, including EMA, CK and CD49f, and endometrial stromal
cell-associated genes, including THY-1, Col I, 5B5 and vimentin,
were significantly increased in EnSCs compared with those in the
controls. Additionally, hESC transplantation partially reversed the
biochemical and morphological changes induced by IUA in
vivo. These results indicate the clinical value of EnSCs
transplantation in the treatment of IUA. Additionally, rats with
IUA received EnSCs transplantation and estrogen treatment. The
results demonstrated that EnSCs transplantation combined with
estrogen significantly increased the treatment efficacy of IUA.
These results indicate that EnSCs transplantation combined with
estrogen treatment may achieve improved treatment outcomes compared
with hESC transplantation alone.
Overall, the expression levels of EGF and PDGF-BB
were significantly increased in the endometrium of patients with
IUA compared with those in controls. EnSCs transplantation combined
with estrogen improved the efficacy of treatment in vivo.
The underling molecular mechanism may be associated with the
decreased expression levels of EGF and PDGF-BB, and the increased
expression levels of ESR1 and MMP-9.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant no. 81601276), the
Shandong Natural Science Foundation of China (grant no. ZR2016HL09)
and the Shandong Medical and Health Science and Technology
Development Project (grant no. 2015WS0033).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
XW, HB and CH designed the study. XW, HB, XL, CW and
CH analyzed and interpreted the data. XW and HB wrote and revised
the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
All participants provided written informed consent
and the study was approved by the Ethics Committee of The
Affiliated Yantai Yuhuangding Hospital of Qingdao University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Deans R and Abbott J: Review of
intrauterine adhesions. J Minim Invasive Gynecol. 17:555–569. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schenker JG: Etiology of and therapeutic
approach to synechia uteri. Eur J Obstet Gynecol Reprod Biol.
65:109–113. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Salma U, Xue M, Ali Sheikh MS, Guan X, Xu
B, Zhang A, Huang L and Xu D: Role of transforming growth factor-β1
and smads signaling pathway in intrauterine adhesion. Mediators
Inflamm. 2016:41582872016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen F, Duan H, Zhang Y and Wu YH: Effect
and mechanism of formation of intrauterine adhesion at different
dose of estrogen. Zhonghua Fu Chan Ke Za Zhi. 45:917–920. 2010.(In
Chinese). PubMed/NCBI
|
|
5
|
Di Spiezio Sardo A, Mazzon I, Bramante S,
Bettocchi S, Bifulco G, Guida M and Nappi C: Hysteroscopic
myomectomy: A comprehensive review of surgical techniques. Hum
Reprod Update. 14:101–119. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Johary J, Xue M, Zhu X, Xu D and Velu PP:
Efficacy of estrogen therapy in patients with intrauterine
adhesions: Systematic review. J Minim Invasive Gynecol. 21:44–54.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Capella-Allouc S, Morsad F,
Rongieres-Bertrand C, Taylor S and Fernandez H: Hysteroscopic
treatment of severe Asherman's syndrome and subsequent fertility.
Hum Reprod. 14:1230–1233. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ding L, Li X, Sun H, Su J, Lin N, Péault
B, Song T, Yang J, Dai J and Hu Y: Transplantation of bone marrow
mesenchymal stem cells on collagen scaffolds for the functional
regeneration of injured rat uterus. Biomaterials. 35:4888–4900.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jing Z, Qiong Z, Yonggang W and Yanping L:
Rat bone marrow mesenchymal stem cells improve regeneration of thin
endometrium in rat. Fertil Steril. 101:587–594. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhou BO, Yue R, Murphy MM, Peyer JG and
Morrison SJ: Leptin-receptor-expressing mesenchymal stromal cells
represent the main source of bone formed by adult bone marrow. Cell
Stem Cell. 15:154–168. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang Y, Lin X, Dai Y, Hu X, Zhu H, Jiang
Y and Zhang S: Endometrial stem cells repair injured endometrium
and induce angiogenesis via AKT and ERK pathways. Reproduction.
152:389–402. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yun BH, Jeon YE, Chon SJ, Park JH, Seo SK,
Cho S, Choi YS, Lee JS and Lee BS: The prognostic value of
individual adhesion scores from the revised American fertility
society classification system for recurrent endometriosis. Yonsei
Med J. 56:1079–1086. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ebrahimi-Barough S, Massumi M,
Kouchesfahani Mohseni H and Ai J: Derivation of
pre-oligodendrocytes from human endometrial stromal cells by using
overexpression of MicroRNA 338. J Mol Neurosci. 51:337–343. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ebrahimi-Barough S, Kouchesfahani Mohseni
H, Ai J, Mahmoodiniac M, Tavakole S and Massumic M: Programming of
human endometrial-derived stromal cells (EnSCs) into
pre-oligodendrocyte cells by overexpression of miR-219. Neurosci
Lett. 537:65–70. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tang YQ, Gan L, Xu Q, Wang S, Li JJ and
Duan H: Effects of human umbilical cord mesenchymal stem cells on
intrauterine adhesions in a rat model. Int J Clin Exp Pathol.
9:12119–12129. 2016.
|
|
17
|
You Z, Sun J, Xie F, Chen Z, Zhang S, Chen
H, Liu F, Li L, Chen G, Song Y, et al: Modulatory effect of
fermented papaya extracts on mammary gland hyperplasia induced by
estrogen and progestin in female rats. Oxid Med Cell Longev.
2017:82350692017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhou Y, Kim YS, Chakraborty S, Shi J, Gao
H and Liu S: 99mTc-labeled cyclic RGD peptides for noninvasive
monitoring of tumor integrin αvβ3 expression.
Mol Imaging. 10:386–397. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Matsumoto H, Nasu K, Nishida M, Ito H,
Bing S and Miyakawa I: Regulation of proliferation, motility, and
contractility of human endometrial stromal cells by
platelet-derived growth factor. J Clin Endocrinol Metab.
90:3560–3567. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Martin P and Nunan R: Cellular and
molecular mechanisms of repair in acute and chronic wound healing.
Br J Dermatol. 173:370–378. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Qin W, Chung AC, Huang XR, Meng XM, Hui
DS, Yu CM, Sung JJ and Lan HY: TGF-β/Smad3 signaling promotes renal
fibrosis by inhibiting miR-29. J Am Soc Nephrol. 22:1462–1474.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mascareno E, Galatioto J, Rozenberg I,
Salciccioli L, Kamran H, Lazar JM, Liu F, Pedrazzini T and Siddiqui
MA: Cardiac lineage protein-1 (CLP-1) regulates cardiac remodeling
via transcriptional modulation of diverse hypertrophic and fibrotic
responses and angiotensin II-transforming growth factor β (TGF-β1)
signaling axis. J Biol Chem. 287:13084–13093. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hyodo S, Matsubara K, Kameda K and
Matsubara Y: Endometrial injury increases side population cells in
the uterine endometrium: A decisive role of estrogen. Tohoku J Exp
Med. 224:47–55. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wang Z, Cui Y, Chen Y, Zhang D, Liang Y,
Zhang D, Wu Q, Xie J, Ouyang S, Li D, et al: Comparative genetic
mapping and genomic region collinearity analysis of the powdery
mildew resistance gene Pm41. Theor Appl Genet. 127:1741–1751. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jecker NS: Response to open peer
commentaries on ‘Justice between age groups: An objection to the
prudential lifespan approach’. Am J Bioeth. 14:W10–W12. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Roy KK, Negi N, Subbaiah M, Kumar S,
Sharma JB and Singh N: Effectiveness of estrogen in the prevention
of intrauterine adhesions after hysteroscopic septal resection: A
prospective, randomized study. J Obstet Gynaecol Res. 40:1085–1088.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Skinner JL, Riley SC, Gebbie AE, Glasier
AF and Critchley HO: Regulation of matrix metalloproteinase-9 in
endometrium during the menstrual cycle and following administration
of intrauterine levonorgestrel. Hum Reprod. 14:793–799. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Du H and Taylor HS: Stem cells and female
reproduction. Reprod Sci. 16:126–139. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Gargett CE and Ye L: Endometrial
reconstruction from stem cells. Fertil Steril. 98:11–20. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Gargett CE, Nguyen HP and Ye L:
Endometrial regeneration and endometrial stem/progenitor cells. Rev
Endocr Metab Disord. 13:235–251. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Maruyama T and Yoshimura Y: Stem cell
theory for the pathogenesis of endometriosis. Front Biosci (Elite
Ed). 4:2754–2763. 2012. View
Article : Google Scholar : PubMed/NCBI
|