Introduction
Hypopharyngeal cancer is a malignant tumor with poor
prognosis in head and neck cancer. Its morbidity accounts for 3–5%
of head and neck cancers (1). As the
pathogenic location of hypopharyngeal cancer is concealed, the
lesion tends to infiltrate and spread along the mucosa. The
incidence of cervical lymph node metastasis is high. Cervical lymph
node metastasis has already appeared in patients when they are
diagnosed. Cervical lymph node metastasis is one of the factors
that affect prognosis of patients with hypopharyngeal cancer
(2,3). Therefore, how to accurately diagnose
and evaluate lymph node metastasis in patients with hypopharyngeal
cancer has important clinical significance for patients with
cervical lymph node metastasis of hypopharyngeal cancer (4).
Clinical examination of cervical lymph node
metastasis has been carried out by palpation, but the accuracy of
palpation is easily affected by factors, such as the experience of
the examiner and the location and size of lymph nodes (5). For example, the lymph node has no
obvious swelling and tenderness in patients with cervical lymph
node metastasis of early hypopharyngeal cancer. The texture of the
lymph node is soft and the size is small, so it is difficult to be
found by palpation (6). Ultrasound,
as a non-invasive, economical and convenient method, has been used
to diagnose many diseases in clinic (7). Studies have shown that ultrasound has
diagnostic value for hypopharyngeal cancer and that cervical lymph
node metastasis missed by palpation can be found by ultrasound
(8).
However, research reports on the diagnosis of
regional lymph node metastasis of hypopharyngeal cancer are
generally mentioned in comprehensive reports on head and neck
tumors (9). The studies that
specifically report lymph node metastasis of hypopharyngeal cancer
are rare. Therefore, the results of pathological examination were
used as the standard, the diagnostic value of ultrasonic imaging
was investigated for lymph node metastasis of hypopharyngeal
cancer, in order to provide proper plans for diagnosis of patients
with hypopharyngeal cancer with lymph node metastasis.
Patients and methods
General data
Eighty-nine patients who were diagnosed with
hypopharyngeal cancer in Qilu Hospital of Shandong University
(Qingdao) (Qingdao, China) from January 2014 to June 2016 were
retrospectively analyzed, including 51 male patients and 38 female
patients, with an average age of 54.1±2.5 years. Sixty-eight
patients were diagnosed with hypopharyngeal cancer with cervical
lymph node metastasis by pathological sections. Twenty-one patients
did not have cervical lymph node metastasis (Table I).
 | Table I.General data. |
Table I.
General data.
| Items | Patients with
hypopharyngeal cancer (n=89) |
|---|
| Sex |
|
| Male | 51 (57.30) |
|
Female | 38 (42.70) |
| Age (years) |
|
| ≥54 | 45 (50.56) |
|
<54 | 44 (49.44) |
| BMI |
|
| ≥21 | 37 (41.57) |
|
<21 | 52 (58.43) |
| Educational
level |
|
| ≥ Middle
school | 56 (62.92) |
| <
Middle school | 32 (35.95) |
| Presence and absence
of cervical lymph node metastasis |
|
|
Presence | 68 (76.40) |
|
Absence | 21 (23.60) |
| Liver function
indicators |
|
| Serum
total protein (g/l) | 7142±2.33 |
| Alanine
aminotransferase (µmol/l) | 28.34±4.58 |
| Total
bilirubin (µmol/l) | 11.27±2.10 |
| Renal function
indicators (µmol/l) |
|
|
Creatinine | 59.59±4.11 |
| Serum
urea | 5.19±0.76 |
| Uric
acid | 272.66±11.74 |
Inclusion criteria
Patients who were diagnosed with hypopharyngeal
cancer by pathological examination. Exclusion criteria: Patients
with severe liver dysfunction and kidney dysfunction; patients with
hypopharyngeal cancer and other cancers; patients with severe
infection; patients who did not accept pathological diagnosis;
patients with cognitive disorder or communication disorder;
patients who would not cooperate with the experiment. All the
patients and their family members agreed to participate in the
experiment and signed informed consent forms. This experiment was
approved by the Ethics Committee of Qilu Hospital of Shandong
University (Qingdao).
Detection methods
Palpation
The diagnosis of metastatic lymph node was made by
experienced doctors in a subjective way. At present, only the order
and description can be specified for palpation. All the patients
were diagnosed by palpation, which was carried out by multiple
doctors who had rich clinical experience to reduce bias. When the
doctors carried out palpation, they gently touched the neck of the
patients with their hands in up to down manner. The key area was
the lymph node chain of the internal jugular vein, for lymph nodes
in the II–IV area. The presence and absence of lymphadenopathy and
the size, hardness, and mobility of the lymph nodes were diagnosed
and assessed.
Ultrasound
ATL-HDI 5000 color Doppler ultrasound equipment
(Philips) was used to diagnose the patients. The probe frequency
was 7 MHz, the aliasing speed of the color flow was adjusted to 8
cm/sec, the color gain was adjusted to 80–85%. The patients were in
supine position, with neck exposed and raised with a pillow. When
the patients were examined, the head was turned to the side that
was not examined, the lymph nodes were scanned by seven-point
method (10) of American Joint
Committee on Cancer. The scanning range was from the area behind
the ear to supraclavicular fossa, the longitudinal and transverse
examinations were carried out. The location, shape, size, internal
echo and envelope of the lymph nodes were recorded. The blood flow
of the lymph nodes was observed and the lymph nodes were divided
into several types, including non-blood flow type, central type,
peripheral type and hybrid type. However, the artificial
interpretation of cervical lymph node ultrasound images is
subjective, so the analysis of lymph node ultrasound images was
performed by computer. The diagnostic criteria for malignant lymph
nodes were detailed previously (11,12).
Observation indicators
i) The long/short-diameter ratio of the
characteristic lymph nodes, the maximum systolic velocity and the
blood flow resistance index of the ultrasound images were compared
between the two groups. ii) The sensitivity, specificity,
diagnostic accuracy, positive predictive value and negative
predictive value of palpation and ultrasound were calculated and
compared in the diagnosis of hypopharyngeal cancer with cervical
lymph node metastasis. iii) An association analysis was carried out
between the imaging features of ultrasound and lymph node
metastasis.
Statistical analysis
SPSS 19.0 (IBM) statistical software was used to
analyze the experimental data. Chi-square test was used for the
enumeration data. The association between the imaging features and
lymph node metastasis was analyzed by Logistic regression analysis.
Students t test was used for quantitative parameters of ultrasound
features analysis. P<0.05 was considered to be statistically
significant.
Results
Comparison of ultrasound image
features in patients with and without metastasis
The long/short diameter ratio, maximum systolic
velocity and resistance index of patients with lymph node
metastasis were significantly higher than those without lymph node
metastasis, and the difference was statistically significant
(P<0.05) (Table II).
 | Table II.Quantitative parameters of ultrasound
features. |
Table II.
Quantitative parameters of ultrasound
features.
| Ultrasonic
features | Metastasis
(n=68) | Non-metastasis
(n=21) | t value | P-value |
|---|
| Long/short diameter
ratio | 2.29±0.72 | 1.52±0.63 | 6.637 | <0.001 |
| Maximum systolic
velocity | 34.89±8.31 | 24.33±7.91 | 7.590 | <0.001 |
| Resistance index | 0.72±0.10 | 0.53±0.08 | 12.23 | <0.001 |
Analysis of diagnostic value of
palpation and ultrasound in hypopharyngeal cancer with cervical
lymph node metastasis
Forty-one patients were diagnosed with lymph node
metastasis by palpation, 59 patients were diagnosed for lymph node
metastasis by ultrasound. The sensitivity, specificity, diagnostic
coincidence rate, negative predictive value and positive predictive
value of palpation were 69.29, 61.90, 60.67, 32.5 and 83.67%,
respectively, in the diagnosis of hypopharyngeal cancer with
cervical lymph node metastasis, and those of ultrasound were 86.76,
80.95, 85.39, 65.38 and 93.65%, respectively. The sensitivity and
diagnostic coincidence rate of ultrasound in diagnosis of
hypopharyngeal cancer with cervical lymph node metastasis were
significantly higher than those of palpation. The differences were
statistically significant (P<0.05). The specificity, negative
predictive value and positive predictive value of ultrasound were
higher than those of palpation, but the differences were not
statistically significant (P>0.05) (Tables III–V).
 | Table III.Diagnostic results of hypopharyngeal
cancer with cervical lymph node metastasis diagnosed by
palpation. |
Table III.
Diagnostic results of hypopharyngeal
cancer with cervical lymph node metastasis diagnosed by
palpation.
| Diagnostic
results | Pathology
(metastasis) | Pathology
(non-metastasis) | Summation |
|---|
| Diagnosis
(metastasis) | 41 | 8 | 49 |
| Diagnosis
(non-metastasis) | 27 | 13 | 40 |
| Summation | 68 | 21 | 89 |
 | Table V.Analysis of diagnostic efficacy of
palpation and ultrasound in hypopharyngeal cancer with cervical
lymph node metastasis (%). |
Table V.
Analysis of diagnostic efficacy of
palpation and ultrasound in hypopharyngeal cancer with cervical
lymph node metastasis (%).
| Diagnostic value | Palpation | Ultrasound | χ2 | P-value |
|---|
| Sensitivity | 69.29% | 86.76% | 12.24 | <0.001 |
| Specificity | 61.90% | 80.95% | 1.876 | 0.172 |
| Diagnostic
coincidence rate | 60.67% | 85.39% | 13.81 | <0.001 |
| Negative predictive
value | 32.5% | 65.38% | 0.284 | 0.594 |
| Positive predictive
value | 83.67% | 93.65% | 2.868 | 0.090 |
The relationship between imaging
features of ultrasound and pathological findings
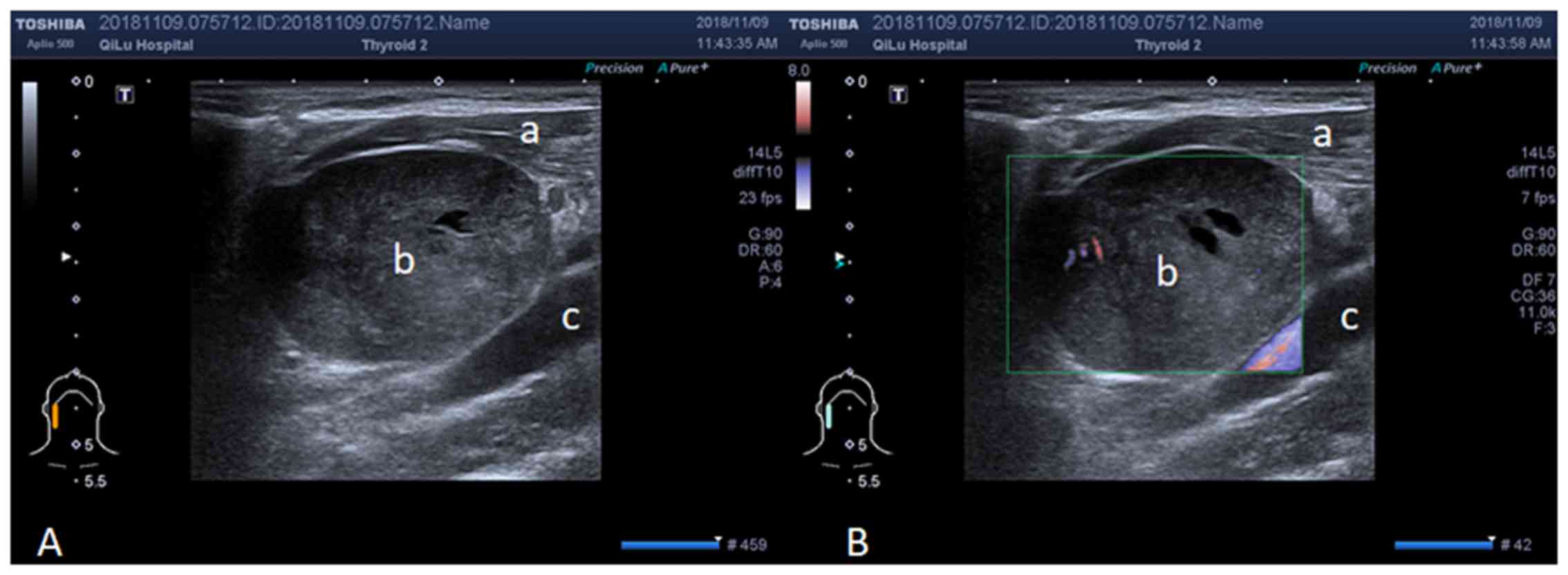
Statistically significant differences were observed
in lymph node internal echo types, medullary echo characteristics,
envelope definition, and blood flow distribution characteristics
between the metastasis group and the non-metastasis group
(P<0.05) (Table VI and Fig. 1).
 | Table VI.The relationship between imaging
features of ultrasound and pathological findings. |
Table VI.
The relationship between imaging
features of ultrasound and pathological findings.
| Imaging
features | Metastasis
(n=68) | Non-metastasis
(n=21) | χ2 | P-value |
|---|
| Internal echo |
|
| 47.04 | <0.001 |
| Homogeneous
hypoecho | 8 (11.76) | 19 (90.48) |
|
|
| Heterogeneous
hypoecho | 60 (88.24) | 2 (9.52) |
|
|
| Medulla |
|
| 75.62 | <0.001 |
| No medulla | 63 (92.65) | 1 (4.76) |
|
|
| Broadening,
centering | 5 (7.35) | 2 (9.52) |
|
|
| Threadiness,
centering | 0 | 18 (85.71) |
|
|
| Envelope |
|
| 36.01 | <0.001 |
| Clear | 15 (22.06) | 20 (95.24) |
|
|
| Not clear | 53 (77.94) | 1 (4.76) |
|
|
| The type of blood
flow |
|
| 48.90 | <0.001 |
| No blood flow | 10 (14.71) | 7
(33.33) |
|
|
| Central regular
blood flow | 4 (5.88) | 14 (66.67) |
|
|
| Central disorderly
blood flow | 27 (39.71) | 0 |
|
|
| Peripheral
disorderly blood flow | 27 (39.71) | 0 |
|
|
Multivariate logistic regression
analysis
Analysis was carried out for the diagnostic results
of ultrasound. The results showed that lymph node internal echo was
heterogeneous. There was no medulla, and the disordered blood flow
in the lymph node predicted lymph node metastasis (P<0.001)
(Table VII).
 | Table VII.Multivariate regression analysis. |
Table VII.
Multivariate regression analysis.
| Ultrasound
findings | Correlation
index | Standard error | P-value | OR |
|---|
| Internal echo | 3.825 | 1.229 | <0.001 | 1.72 |
| Medulla
deformation | 2.492 | 0.671 | <0.001 | 1.41 |
| Blood flow | 1.753 | 0.562 | <0.001 | 1.31 |
Discussion
Hypopharyngeal cancer is a refractory head and neck
tumor, with malignant biological behavior, and it is prone to
infiltration and metastasis in mucosa (13). In recent years, although local
control rate of hypopharyngeal cancer has increased with the
development of medical technology, its 5-year survival rate is
still 25–40% and is difficult to be improved (14). Therefore, how to make an effective
diagnosis for hypopharyngeal cancer with cervical lymph node
metastasis as soon as possible is an urgent problem to be solved.
At present, in addition to palpation, there are other diagnostic
methods for tumors in the throat, such as ultrasound, CT and MRI
(15). However, MRI is expensive and
there is radiation in CT, thus these two methods are currently not
popular (16). Ultrasound has
advantages of being non-invasive, economical and convenient
(17), so the diagnostic value of
ultrasound was analyzed in hypopharyngeal cancer with lymph node
metastasis.
In the present study, according to the results in
the comparison of ultrasound image parameters, the long/short
diameter ratio, the maximum systolic velocity and the resistance
index of patients with lymph node metastasis were significantly
higher than those without lymph node metastasis. The diagnostic
efficacy of palpation and ultrasound was analyzed in hypopharyngeal
cancer with lymph node metastasis. The results showed that the
patients with lymph node metastasis diagnosed by ultrasound was
significantly more than that of palpation (P<0.05). The
sensitivity and diagnostic coincidence rate of ultrasound in
hypopharyngeal cancer with cervical lymph node metastasis were
significantly higher than those of palpation (P<0.05). Although
the specificity, negative predictive value, and positive predictive
value of ultrasound were higher than those of palpation, the
differences were not statistically significant (P>0.05). Studies
have reported that the sensitivity and specificity of ultrasound in
cervical lymph node metastasis were higher than those of palpation,
which confirmed the result of this study (18,19). The
relationship between the image features of ultrasound in lymph
nodes and the pathological findings was analyzed. Statistically
significant differences were observed in lymph node internal echo
types, medullary echo characteristics, envelope definition, and
blood flow distribution characteristics between the metastasis
group and the non-metastasis group (P<0.05). Multivariate
logistic regression analysis also showed that lymph node internal
echo was heterogeneous, there was no medulla, and that the
disordered blood flow in lymph nodes could indicate lymph node
metastasis. It was reported that the diagnostic value of ultrasound
in laryngeal cancer and hypopharyngeal cancer with cervical lymph
node metastasis and demonstrated that lymph node internal echo was
heterogeneous, there was no medulla or medulla decentered, and that
the disordered signal of blood flow in lymph nodes could indicate
lymph node metastasis (20). This
result is consistent with the results of the present study.
Furthermore, it was reported that increased blood flow signals
around lymph nodes indicated the presence of lymph node metastasis,
the reason is that the infiltration of cancer cells injures blood
vessels of medulla, resulting in the residual of blood vessels of
the tunica (21). This explains the
abnormality of the blood flow signal. A report also indicated that
the ultrasound image of cervical lymph node metastasis showed
medullary structural disorders, and that blood flow showed the
increase of peripheral blood flow signal and the increase of
resistance index (22). This result
is also consistent with the findings of this study.
In conclusion, cervical lymph node metastasis is an
important independent prognostic factor for patients with
hypopharyngeal cancer with cervical lymph node metastasis (23,24). The
diagnostic accuracy has important clinical value. This study showed
that the preoperative ultrasound has diagnostic value for
hypopharyngeal cancer with cervical lymph node metastasis and that
the diagnosis result of preoperative ultrasound can be used as an
important reference for the diagnosis and treatment of
hypopharyngeal cancer with lymph node metastasis. However, further
studies are still required.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
GW wrote the manuscript. XL, RS and LL collected and
analyzed the general data of patients. GW, DL and QZ recorded and
analyzed ultrasound results. CG and HG contributed to statistical
analysis. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Qilu Hospital of Shandong University (Qingdao) (Qingdao, China).
Patients who participated in this study, had complete clinical
data. Signed informed consents were obtained from the patients or
the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kim JW, Kim MS, Kim SH, Kim JH, Lee CG,
Kim GE and Keum KC: Definitive chemoradiotherapy versus surgery
followed by adjuvant radiotherapy in resectable stage III/IV
hypopharyngeal cancer. Cancer Res Treat. 48:45–53. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chung EJ, Kim GW, Cho BK, Park HS and Rho
YS: Pattern of lymph node metastasis in hypopharyngeal squamous
cell carcinoma and indications for level VI lymph node dissection.
Head Neck. 38 (Suppl 1):E1969–1973. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Xing Y, Zhang J, Lin H, Gold KA, Sturgis
EM, Garden AS, Lee JJ and William WN Jr: Relation between the level
of lymph node metastasis and survival in locally advanced head and
neck squamous cell carcinoma. Cancer. 122:534–545. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang Z, Ji W, Tang Q and Pan Z:
Relationship among expression of the VEGF gene and MVD with
cervical lymph node metastasis in laryngeal squamous cell
carcinoma. Lin Chuang Er Bi Yan Hou Ke Za Zhi. 18:100–102. 2004.(In
Chinese). PubMed/NCBI
|
|
5
|
Liang H, Li A, Li Y, Cheng H, Zhao Q, Li J
and Wang Q: A retrospective study of dual-energy CT for clinical
detecting of metastatic cervical lymph nodes in laryngeal and
hypopharyngeal squamous cell carcinoma. Acta Otolaryngol.
135:722–728. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ni XG, Cheng RR, Lai SQ, Zhang L, He S,
Zhang YM and Wang GQ: Value of narrow band imaging endoscopy in the
detection of unknown primary site with cervical lymph node
metastasis of squamous cell carcinoma. Zhonghua Zhong Liu Za Zhi.
35:698–702. 2013.(In Chinese). PubMed/NCBI
|
|
7
|
Richardson A, Gallos I, Dobson S, Campbell
BK, Coomarasamy A and Raine-Fenning N: Accuracy of first-trimester
ultrasound in diagnosis of tubal ectopic pregnancy in the absence
of an obvious extrauterine embryo: Systematic review and
meta-analysis. Ultrasound Obstet Gynecol. 47:28–37. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Arens C, Weigt J, Schumacher J and Kraft
M: Ultrasound of the larynx, hypopharynx and upper esophagus. HNO.
59:145–154. 2011.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Buckley JG and MacLennan K: Cervical node
metastases in laryngeal and hypopharyngeal cancer: A prospective
analysis of prevalence and distribution. Head Neck. 22:380–385.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Prativadi R, Dahiya N, Kamaya A and Bhatt
S: Chapter 5 ultrasound characteristics of benign vs. malignant
cervical lymph nodes. Semin Ultrasound CT MR. 38:506–515. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Randolph G, Sacks B and Baskin HJ Sr:
Ultrasound and mapping of neck lymph nodesThyroid Ultrasound and
Ultrasound-Guided FNA. Baskin HJ Sr, Duick DS and Levine RA:
Springer; New York, NY: pp. 149–177. 2018
|
|
12
|
Xia Y: Value of ultrasonography in
differentiating malignant and benign superficial cervical lymph
nodes. Zhongguo Yi Xue Ying Xiang Ji Shu. 27:45–48. 2011.(In
Chinese).
|
|
13
|
Wu Z, Deng XY, Zeng RF, Su Y, Gu MF, Zhang
Y, Xie CM and Zheng L: Analysis of risk factors for retropharyngeal
lymph node metastasis in carcinoma of the hypopharynx. Head Neck.
35:1274–1277. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang J, Cui XB and Sun YH: Significance of
induction chemotherapy in the treatment of locally advanced
laryngeal cancer and hypopharyngeal cancer. Lin Chung Er Bi Yan Hou
Tou Jing Wai Ke Za Zhi. 30:1548–1551. 2016.(In Chinese). PubMed/NCBI
|
|
15
|
Mok G, Gauthier I, Jiang H, Huang SH, Chan
K, Witterick IJ, O'Sullivan B, Waldron JN, Bayley AJ, Cho BC, et
al: Outcomes of intensity-modulated radiotherapy versus
conventional radiotherapy for hypopharyngeal cancer. Head Neck.
37:655–661. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Marioni G, Bertolin A, Giacomelli L,
Marchese-Ragona R, Savastano M, Calgaro N, Marino F, De Filippis C
and Staffieri A: Expression of the apoptosis inhibitor protein
Survivin in primary laryngeal carcinoma and cervical lymph node
metastasis. Anticancer Res. 26:3813–3817. 2006.PubMed/NCBI
|
|
17
|
Leng XF, Zhu Y, Wang GP, Jin J, Xian L and
Zhang YH: Accuracy of ultrasound for the diagnosis of cervical
lymph node metastasis in esophageal cancer: a systematic review and
meta-analysis. J Thorac Dis. 8:2146–2157. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
van den Brekel MW, Stel HV, Castelijns JA,
Nauta JJ, van der Waal I, Valk J, Meyer CJ and Snow GB: Cervical
lymph node metastasis: assessment of radiologic criteria.
Radiology. 177:379–384. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
van den Brekel MW, Castelijns JA, Stel HV,
Luth WJ, Valk J, van der Waal I and Snow GB: Occult metastatic neck
disease: detection with US and US-guided fine-needle aspiration
cytology. Radiology. 180:457–461. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tang QF, Ji WY, Pan ZM, Zheng Y and Guan
C: Expression of the metastasis-associated gene 1 in laryngeal
squamous cell carcinoma: correlation with cervical lymph node
metastasis. Zhonghua Er Bi Yan Hou Ke Za Zhi. 38:213–216. 2003.(In
Chinese). PubMed/NCBI
|
|
21
|
Ahuja A and Ying M: An overview of neck
node sonography. Invest Radiol. 37:333–342. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chikui T, Yonetsu K and Nakamura T:
Multivariate feature analysis of sonographic findings of metastatic
cervical lymph nodes: Contribution of blood flow features revealed
by power Doppler sonography for predicting metastasis. AJNR Am J
Neuroradiol. 21:561–567. 2000.PubMed/NCBI
|
|
23
|
Joo YH, Cho KJ, Kim SY and Kim MS:
Prognostic significance of lymph node density in patients with
hypopharyngeal squamous cell carcinoma. Ann Surg Oncol. 22 (Suppl
3):S1014–S1019. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Roberts TJ, Colevas AD, Hara W, Holsinger
FC, Oakley-Girvan I and Divi V: Number of positive nodes is
superior to the lymph node ratio and American Joint Committee on
Cancer N staging for the prognosis of surgically treated head and
neck squamous cell carcinomas. Cancer. 122:1388–1397. 2016.
View Article : Google Scholar : PubMed/NCBI
|