Introduction
The increase in cervical cancer screening intervals
in the US (1) triggered concerns
about increasing the risk for cancer (2) and the implementation of guidance across
the US (3). Adoption of guidelines
in community-based clinics is lagging and is inefficient (4). Colposcopy with biopsy is a critical
link between screening and diagnosing/treating cancerous or
pre-cancerous lesions; however its sensitivity, accuracy and
reproducibility are limited (5–8), and the
lack of standardization of colposcopic practice in the US is a
recognized contributor to this (9).
The American Society for Colposcopy and Cervical Pathology (ASCCP)
recently published optional standards to improve the performance of
colposcopy (10). Colposcopic biopsy
practice varies widely, ranging from identifying and sampling the
single most suspicious site, to 4-quadrant biopsies including
multiple non-targeted/random biopsies from each patient (11). Based on the findings of the National
Cancer Institute (NCI) Biopsy Study (12), the ASCCP recommends taking multiple
targeted biopsies from patients (typically 2–4), except from
patients with a low-grade referral and nothing observable at
colposcopy (10). This strategy has
not been validated in wider populations, and generalizing a
recommendation based on academic research data to patients with a
potentially low risk of cervical disease may have a negative impact
on patients, such as increasing pain, discharge or bleeding from
additional biopsies, unnecessarily (13). Furthermore, even with multiple
biopsies, a large number of precancers are un/under-detected,
indicating that punch biopsy placement is inaccurate (14). Since studies are often performed by
well-trained and experienced colposcopists and follow specific
protocols, in US community-based clinics, where colposcopists may
be more inexperienced and don't adhere to guidelines fully
(15), the adoption of multiple
biopsy protocols (10) could
introduce a big negative impact on patients. Screening and
management recommendations are generally not fully adopted in
community-based practice (15,16) and
the proposed measures (10) do not
address the fundamentally subjective nature of colposcopy.
Subsequently, standardization of the imaging process during the
colposcopic procedure, and determination of how observations are
assessed and interpreted could be helpful.
Adjunctive Dynamic Spectral Imaging (DSI) mapping is
a standardized way to quantify cervical acetowhitening for
colposcopic assessment and biopsy selection, which increased the
sensitivity of high-grade lesion detection in previous studies
(17–20). Following the aforementioned studies
assessing this technology, IMPROVE-COLPO was the first study to
evaluate colposcopy with DSI on a US population (21,22).
Furthermore, in contrast to the aforementioned previous studies,
the IMPROVE-COLPO study was conducted in community-based clinics,
and included a control group to allow assessment of this technology
in routine practice and its comparison with the prior
standard-of-care for the first time. Previous published analyses of
the IMPROVE-COLPO study reported that detection of high-grade
(grade ≥2) cervical intraepithelial neoplasia (CIN2+) increased
with the use of DSI (21,22). In particular, for patients with an
indication of low grade abnormality in screening, it was reported
that a 21% increase in the number of biopsies, combined with more
efficient biopsy technique, resulted in a 31 and 56% increase in
the detection of women with CIN2+ and CIN3+, respectively (21).
To the best of our knowledge, the present analysis
was the first to present results collected from the recruitment of
7,555 patients in total. The present study evaluated the impact of
digital colposcopy combined with DSI on a well-defined
sub-population, specifically the cohort of women recruited in
IMPROVE-COLPO with cytology of atypical squamous cells of
undetermined significance (ASC-US). The present study may be the
largest conducted on this specific cohort, with this prevalent but
equivocal cytologic indication representing ~1/3 of women having
colposcopy (16) and being
considered as relatively low-risk for high-grade disease (1,23). The
present study may therefore prove valuable in improving the
understanding of colposcopic practice and outcomes, as the
perceived low-risk for the aforementioned patient cohort may be
affecting how colposcopy is being practiced, such as how many
patients are biopsied or how many biopsies are being taken, and
eventually impairing the capacity of colposcopy to efficiently
detect disease in this substantial patient cohort. In order to
ensure a focus on clinically important disease (i.e., disease with
a considerable potential to progress to cancer), and since CIN2
histology results can be ambiguous (24), all primary analyses in the present
study have been performed for histological outcomes of CIN3+.
Materials and methods
Patient recruitment
IMPROVE-COLPO (NCT 02185599) was an observational,
two-arm, cross-sectional study that recruited patients who had been
referred for colposcopy across multiple US community-based clinics
(21,22). The IMPROVE-COLPO study was approved
by a central Institutional Review Board (IRB), E&I Review
Services (Independence, USA), the University of Toledo Biomedical
IRB (Toledo, USA) and the Advocate Health Care IRB (Downers Grove,
USA) and was conducted according to the International Conference on
Harmonization Guideline for Good Clinical Practice.
The DSI method, which is integrated as an adjunct
into a commercially available digital colposcope (DYSIS; DYSIS
Medical Ltd.), standardizes colposcopic imaging, quantifies and
maps the acetowhitening to introduce objectivity, and supports
assessments and biopsy decisions (17,18). US
facilities that adopted the DSI technology participated in the
present study and recruited consecutive patients undergoing
colposcopy with the DSI digital colposcope for inclusion in the
prospective arm. Control cases were collected by chart review from
consecutive historical examinations (retrospective arm) performed
at each facility by the same colposcopists as in the prospective
arm, in the period directly preceding the study device installation
at each facility, but with standard colposcopes and methods to
capture how colposcopy is performed in a real-world setting and to
characterize the standard-of-care performance. To reduce bias from
variabilities among colposcopists, the number of patients recruited
per colposcopist was equal in the two arms. For practical reasons,
the requirement to exactly match the patient numbers per
colposcopist did not include the referral reason of the patients,
and therefore, the number of patients in each referral sub-category
did not exactly match.
The colposcopists that participated in the present
study were those performing colposcopy routinely in each facility,
and comprised gynecologic oncologists, obstetrician-gynecologists,
nurse practitioners and physician assistants. Colposcopists were
all adequately trained for the use of the digital colposcope and
interpretation of the DSI map prior to recruiting prospective
patients. The inclusion criteria for patients across both arms
included age ≥21 years, an abnormal screening result based on
guidelines (1,25) and their ability to provide informed
consent. The present study specifically focused on the sub-group of
women recruited in the IMPROVE-COLPO study with an ASC-US cytologic
result. To be eligible, ASC-US had to either be combined with
positivity to human papillomavirus (HPV+) or be persistent at
repeated screenings (23). The
exclusion criteria for both arms were as follows: Lack of specified
indication; a single ASC-US result without HPV positivity;
pregnancy; human immunodeficiency virus infection and acquired
immune deficiency syndrome positivity; previous hysterectomy; and
patients receiving or having received radiation treatment or
chemotherapy for cervical neoplasia or other concurrent cancer.
There were 1,353 and 1,226 women included in the retrospective and
prospective arms, respectively. Patients from the prospective arm
signed informed consent prior to the study, whereas consent was
waived by the aforementioned IRBs for patients from the
retrospective arm.
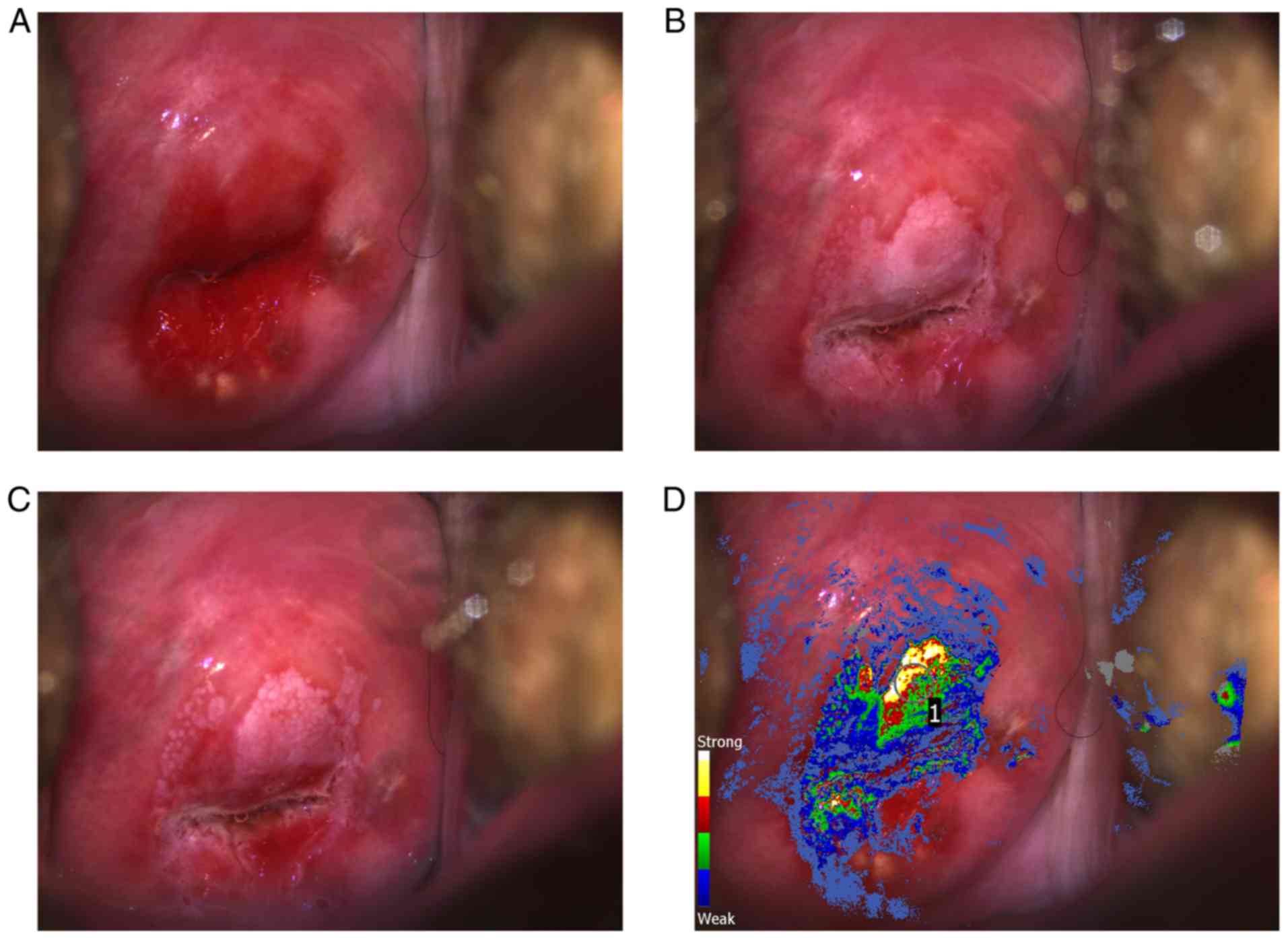
Prospective arm (DSI)
The DSI digital colposcope was used for all
examinations in patients in the prospective arm. This is a
high-resolution digital colposcope offering DSI mapping (17), a method that is based on the analysis
of a baseline image and a series of consecutive images captured for
2–3 min following acetic acid application. Acetowhite changes are
quantified and highlighted for assessment and directed biopsy with
a color scale (Fig. 1). Previous
studies revealed that the upper part of the scale
(red-yellow-white) is associated with high-grade histological
findings (17,18), and may therefore be used for biopsy
selection. Since the DSI map is an aid, the colposcopists could
only see it after completing a thorough visual standard assessment
of acetowhitening and morphology, and after documenting their
biopsy selections based on visualization (standard biopsies). For
patients where the colposcopist did not select any areas to biopsy
based on visualization (i.e., before seeing the DSI map), this was
explicitly documented. Colposcopists could use the DSI map for
selecting additional biopsies at different locations, but standard
biopsies should not be disregarded based on the DSI map result.
Colposcopists were responsible for all clinical
decisions, ensuring that the study would capture the pragmatic,
rather than an investigational, use of DSI. Decisions regarding
which women required a biopsy, and the number and location of the
biopsies, were not protocol-dictated. For each patient, the DSI map
was interpreted and followed or ignored for biopsy selection at the
colposcopists' discretion.
Retrospective arm (standard colposcopy
control)
In order to collect a matched control group
(retrospective arm of the study), appointment and billing
information was used to identify consecutive patients for each
colposcopist. Identified patients were subsequently selected
according to study inclusion/exclusions. Data were extracted from
the patient charts recorded at each clinic.
Data collection
Prospective arm recruitment occurred between
September 2014 and October 2017. Patients in the retrospective arm
(control examinations) were between November 2004 and October 2017,
with >96% of them between January 2012 and October 2017 and 80%
between January 2014 and October 2017. The data collected comprised
basic demographics information, numbers of biopsies taken,
indication whether endocervical sampling (ECS) or treatment was
performed, and histopathology results. Biopsy results are presented
at the single biopsy level, with a few exceptions when multiple
biopsy samples had been processed and reported together, in which
case they were excluded from any biopsy-level analysis. Biopsies
were labeled as ‘standard’, ‘random’ or ‘DYSIS’ (for prospective
patients). Histopathology readings, which are the gold standard for
analyses, were performed by the laboratories used by the
participating facilities, following routine practice.
Although the primary end-point of the IMPROVE-COLPO
study was the detection of women with CIN2+, the current study
presents an analysis primarily for detection of women with CIN3+,
which is a more reliable surrogate for cervical cancer (26) compared with CIN2, which is a more
ambiguous histological finding (24)
and often regresses (27). In order
to better understand the impact of digital colposcopy with DSI, the
number of biopsied women and the number of biopsies were also
analyzed and compared. Performance was compared across the two arms
and, in secondary analyses, within the prospective arm (to evaluate
the contribution of standard-directed vs. DSI-assisted
biopsies).
Data analysis
Given the observational design of the IMPROVE-COLPO
study and the non-investigational colposcopy (in both arms), where
no biopsies or excisional treatments (loop electrosurgical excision
procedure or conization) outside routine care were requested, the
sensitivity of colposcopy and colposcopic biopsy to detect patients
with high-grade cervical disease could not be measured because the
number of subjects with undetected disease was unknown. For
analyses, the ‘disease detection rate’ was used, which was defined
as the number of patients with CIN3+ divided by the total number of
patients. Rates were first calculated for all the detection methods
combined (biopsy/ECS/treatment) as an overview. Subsequently, the
detection rates were calculated, analyzed and compared specifically
for colposcopic (punch) biopsies. In the retrospective arm, the
detection results were also calculated for different time periods.
As an indirect measure of specificity of colposcopic biopsy, the
proportion of women that underwent biopsy without their biopsies
revealing CIN3+ was determined. As indicative measures of biopsy
efficiency in each arm, the total number of biopsies taken (over
the entire population in each arm) per each patient detected with
CIN3+ was calculated, and the positive predictive value (PPV) of
biopsy was determined, which corresponds to the proportion of
biopsies that identified CIN3+.
Statistical analysis
All statistical analyses were pre-planned using
two-sided 5% Type I error. A two-sided Fisher exact test with a
two-sided confidence interval (CI) for the difference was used to
compare detection rates. A two-sided Kruskal-Wallis test was used
to compare the distribution of the number of biopsies and the
number of positive biopsies. An exact binomial test was used to
evaluate the incremental gain in the detection rate attributed to
DSI within the prospective arm.
Results
Patient recruitment
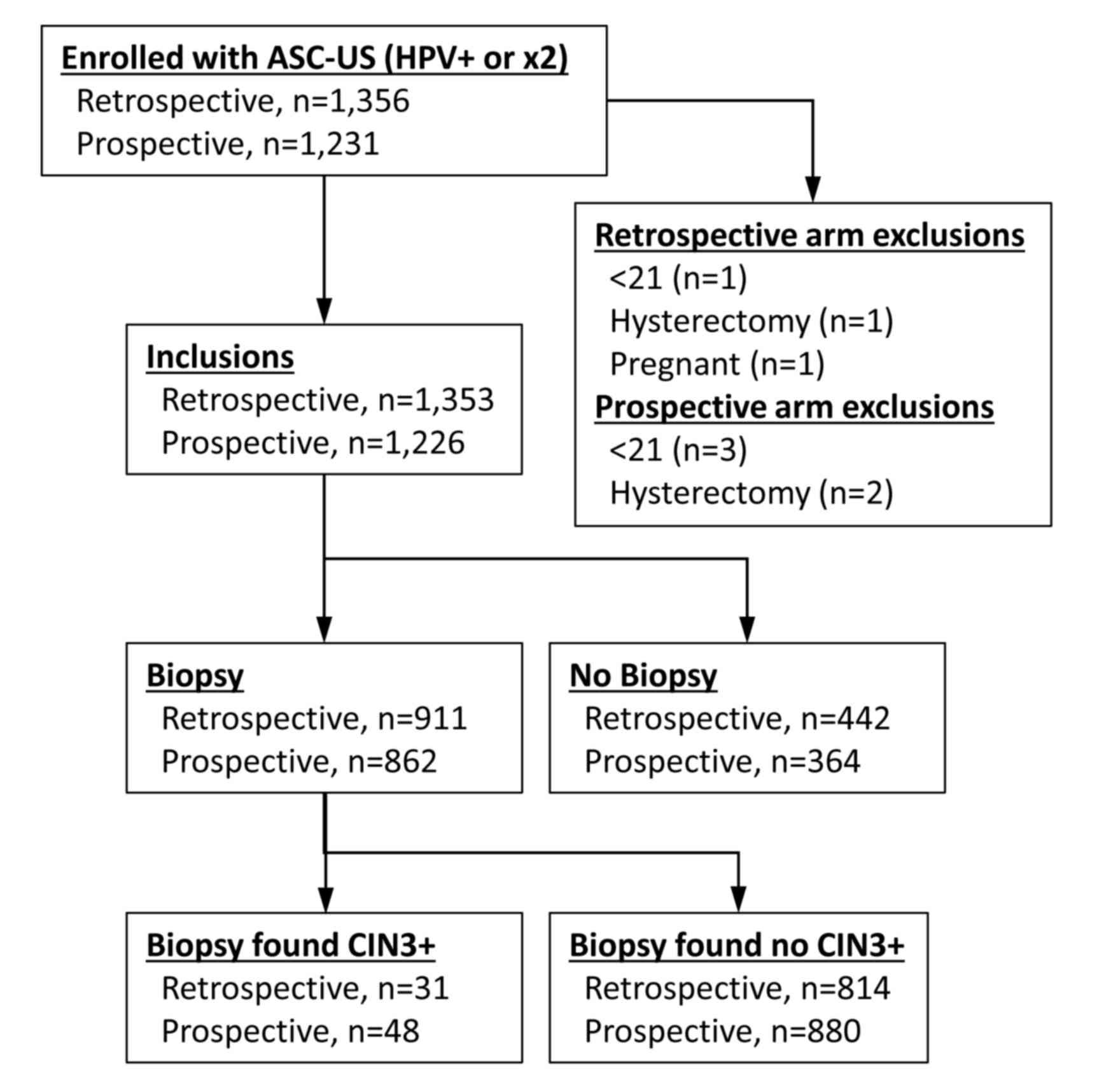
IMPROVE-COLPO recruited a total of 7,555 women
across its two arms. Among these, 2,587 (34.24%) patients had an
ASC-US result and were considered for the present study. These
patients were examined by 146 colposcopists in 42 clinics. Data
were collected separately for each site and colposcopist, so there
was no overlap of recruitment between the two arms at each clinic.
No study/study-device related adverse events were reported. Eight
patients were excluded for the following reasons: Age <21 years
(n=4); history of hysterectomy (n=3); and pregnancy (n=1). A total
of 1,353 and 1,226 women were included in the retrospective and
prospective arms, respectively (Fig.
2). The majority of these patients (~93% in each arm) had an
ASC-US/HPV+ referral rather than persistent ASC-US. These two
sub-groups were therefore analyzed together. Patient baseline
characteristics are presented in Table
I. The median age of patients was 34 years in both arms. There
was no significant difference for each characteristic between the
two groups, apart from Hispanic ethnicity (P=0.037; two-sided
Fisher's exact test).
 | Table I.Baseline characteristics of the study
population. |
Table I.
Baseline characteristics of the study
population.
| Characteristic | Retrospective
control arm | Prospective
arm |
|---|
| Patients, n | 1,353 | 1,226 |
| Age, years |
|
Median | 34.0 | 34.0 |
|
Average | 36.5 | 36.7 |
|
Pre-menopausala, n (%) | 1,167 (86.3) | 1,074 (87.6) |
| Post-menopausal, n
(%) | 185 (13.7) | 185 (12.4) |
| Insurance
statusa, n (%) |
|
Private | 1,212 (89.6) | 1,090 (88.9) |
|
Medicare | 26 (1.9) | 24 (2.0) |
|
Medicaid/Other | 95 (7.0) | 83 (6.8) |
|
Uninsured | 18 (1.3) | 25 (2.0) |
|
Ethnicitya, n (%) |
|
Caucasian | 822 (60.8) | 737 (60.1) |
|
African-American | 311 (23.0) | 269 (21.9) |
|
Asian | 33 (2.4) | 31 (2.5) |
|
Hispanic | 141 (10.4) | 161 (13.1) |
|
Other | 46 (3.4) | 28 (2.3) |
| Referral
pathwaya, n (%) |
|
ASC-US/HPV+ | 1,266 (93.6) | 1,137 (92.7) |
|
Persistent ASC-US | 87 (6.4) | 89 (7.3) |
The clinical characteristics of patients and the
distribution of patients according to their detected disease status
are presented in Tables SI and
SII. The average and median patient
ages in the two arms were comparable for patients in all
histological diagnosis groups (Tables
SI and SII). The percentages of
patients that were biopsied (67.3% in the retrospective and 70.3%
in the prospective arm; Tables SI
and SII, respectively) and of
patients that underwent ECS (74% in the retrospective and 73.2% in
the prospective arm; Tables SI and
SII, respectively) were not
significantly different (P=0.106 and P=0.687, respectively;
two-sided Fisher exact test). More women in the prospective arm
compared with women in the retrospective arm were treated by
excision (11.4 vs. 9.3%, respectively; Tables SII and SI, respectively), although this difference
was not significant (P=0.080; two-sided Fisher exact test). In both
arms, the number of biopsies taken per patient increased with
worsening histology result (Tables
SI and SII), and this was
consistently higher among prospective patients compared with
retrospective patients for all histological grades. Notably, most
often there was no record of a colposcopic impression in the
retrospective patient charts (available for 533/1,353 cases;
Table SI). Conversely, the DSI
software specifically required that a colposcopic impression should
be recorded for each examination, so these data were available for
most patients (1,164/1,226; Table
SII).
In total, 126 patients with CIN3+ were detected: 56
patients in the retrospective arm (4.14%) and 70 patients in the
prospective arm (5.71%) (Tables SI
and SII). These patients included 4
(retrospective) and 7 (prospective) cases of adenocarcinoma in
situ and 1 case of microinvasive squamous carcinoma
(prospective arm).
Punch biopsy detected 31 women with CIN3+ (55.36% of
all women detected with CIN3+) in the retrospective arm vs. 48
women with CIN3+ (68.57% of all women detected with CIN3+) in the
prospective arm. ECS was performed on >73% of the patients in
both arms (Tables SI and SII) and detected an additional 9 (16.07%)
patients with CIN3+ in the retrospective vs. 7 (10%) in the
prospective arm. A further 16 (28.57%) patients in the
retrospective arm vs. 15 (21.43%) in the prospective arm were
detected with CIN3+ in excisions (Tables SI and SII) that were performed on women that had
first been detected with <CIN3 on biopsy/ECS.
Disease detection using biopsy in the
two arms
In the retrospective arm, 911/1,353 women (67.3%)
underwent biopsy vs. 862/1,226 women (70.3%) in the prospective arm
(P=0.1062; two-sided Fisher exact test; Tables SI and SII). The total number of biopsies taken
was 1,308 in the retrospective arm vs. 1,478 in the prospective arm
(average per patient of 0.97 and 1.21, respectively; P<0.001;
two-sided Fisher exact test) (Tables
SI and SII). The number of
biopsies marked as ‘random’ was small (7 in the retrospective arm
and 30 in the prospective arm, Tables
SI and SII).
The average number of biopsies specifically among
the sub-group of patients that underwent biopsy was 1.44
(retrospective) vs. 1.71 (prospective) (Tables SI and SII). This 0.27 difference (P<0.001;
two-sided Fisher exact test) is a relative increase of 18.8% (data
not shown). Hence, ~1 additional biopsy per every 5 biopsied women
was performed in the prospective arm.
Colposcopic biopsy detected 31 women with CIN3+ in
the retrospective arm vs. 48 in the prospective arm. The detection
rates were 2.29% (95% CI, 1.56-3.24) vs. 3.92% (95% CI, 2.90-5.16)
respectively (Table II). The 1.62%
difference (95% CI, 0.30-3.04; P=0.022; two-sided Fisher exact
test) demonstrated that detection was 70.9% higher in the
prospective arm (a 1.71 ratio; 95% CI, 1.1-2.66).
 | Table II.Detection rates of patients with
CIN3+ identified by directed biopsy in the two study arms overall
and by age group. Within the prospective arm, data are also shown
separately for standard and incremental DSI-assisted biopsies. |
Table II.
Detection rates of patients with
CIN3+ identified by directed biopsy in the two study arms overall
and by age group. Within the prospective arm, data are also shown
separately for standard and incremental DSI-assisted biopsies.
|
| Retrospective
control | Prospective
arm |
|
|
|
|---|
|
|
|
|
|
|
|
|---|
| Age, years | Standard
Biopsy |
| Total | Standard
biopsy |
| DSI-assisted
biopsy |
Differencea, % | P-value | Relative gain,
% |
|---|
| Total, n |
| 1,353 |
|
| 1,226 |
|
|
|
|
| Detection rate,
% | 2.29 |
| 3.92b | 2.45 |
| 1.39 | 1.62 | 0.022 | 70.9 |
| 21-24 |
|
Patients, n |
| 165 |
|
| 118 |
|
|
|
|
|
Detection rate, % | 1.21 |
| 5.08 | 3.39 |
| 1.69 | 3.87 | 0.071 | 319.5 |
| 25-29 |
|
Patients, n |
| 299 |
|
| 261 |
|
|
|
|
|
Detection rate, % | 3.01 |
| 4.21 | 3.07 |
| 1.15 | 1.20 | 0.498 | 40.0 |
| >29 |
|
Patients, n |
| 889 |
|
| 847 |
|
|
|
|
|
Detection rate, % | 2.25 |
| 3.66b | 2.13 |
| 1.42 | 1.41 | 0.089 | 62.7 |
The difference in the detection of patients with
CIN3+ in the two arms remained significant (P=0.027; two-sided
Fisher exact test), also when the additional patients with CIN3+
detected by excision (12 in each arm) after biopsy/ies of CIN2 (and
ECS of <CIN2) were taken into account. The detection of patients
with CIN3+ was consistently higher in the prospective arm for
different age sub-groups (Table
II): 3.87% for women 21–24 years old (n=165), 1.20% for women
25–29 years old (n=299) and 1.41% for women >29 years old
(n=889). Random biopsy detected one patient with CIN3+ (in the
prospective arm).
To indirectly assess the specificity of biopsy, the
number of women without CIN3+, specifically among biopsied
patients, was analyzed. Of the 911 biopsied women in the
retrospective arm, 880 (96.6%) had no CIN3+ biopsy vs. 814 of the
862 biopsied women (94.42%) in the prospective arm, a 2.17%
difference (P=0.029; two-sided Fisher exact test; data not
shown).
Detection in the retrospective arm was analyzed for
the different time periods (data not shown), although patient
numbers for the earlier years was too small for a definitive
conclusion. For the 50 women (3.7% of the total) examined between
2004 and 2011, before ASCCP screening guidelines (1) were published and when conventional
cytology may have been the primary approach (compared with
liquid-based cytology), detection rate was 2% (95% CI,
0.05-10.65%). Between 2012 and 2017 (1,303 women, 96.3% of the
total), the detection rate was 2.30% (95% CI, 1.56-3.27%). Between
2014 and 2017 (1,078 women, 79.7% of the total), detection rate was
2.41% (95% CI, 1.58-3.51%). These findings were consistent with the
overall result of 2.29%.
In a secondary analysis, CIN2+ detection was
investigated, and results confirmed a similar trend as with CIN3+,
as there were 91 women in the retrospective and 116 in the
prospective arm (including 1 detected by random biopsy), which
correspond to detection rates of 6.73% (95% CI, 5.45-8.19%) and
9.46% (95% CI, 7.88-11.24%) respectively, a 2.74% difference (95%
CI, 0.55-4.93%; P=0.011; two-sided Fisher exact test) and a 40.7%
increase in the prospective arm compared with the retrospective arm
(data not shown).
Incremental disease detection with
DSI
Among the 1,226 patients from the prospective arm,
the incremental detection of patients with CIN3+ diagnosed by
additional DSI-assisted biopsies selected at different locations on
the cervix after visual assessment biopsies was analyzed (data not
shown). Overall, 659 (53.8%) patients had standard biopsies, and
190 (15.5%) of these patients also had DSI-assisted biopsies. In
addition, 196 patients (16%) underwent DSI-assisted biopsies
without a standard biopsy, whereas an additional 7 patients (0.6%)
underwent random biopsy only and 364 patients (29.7%) had no biopsy
taken (data not shown).
Altogether, there were 966 standard biopsies and 482
DSI-assisted biopsies (Table SII).
Standard visual assessment biopsy in the prospective arm (a biopsy
selected prior to seeing the DSI map) detected 30 patients with
CIN3+ (detection rate 2.45%; 95% CI, 1.66-3.48%), which is
comparable to the 2.29% rate observed in the control group.
DSI-assisted biopsies detected 17 additional patients with CIN3+,
increasing the rate to 3.83% (95% CI, 2.83-5.07%), a 1.38%
difference that is statistically significant (two-sided P=0.006;
exact binomial test relative to a 2.45% null hypothesis) and a
56.3% relative increase in detection for the prospective arm
compared with the retrospective arm (data not shown). One
additional patient with CIN3+ was detected using random biopsy;
however, as there were too few random biopsies, these were not
considered.
The majority of the 17 additional patients with
CIN3+ that were detected by DSI-assisted biopsies selected after
visual assessment, would have been missed without the use of DSI
(data not shown in Tables). For 11 of these patients (64.7%),
before observing the DSI map, the colposcopist had confirmed that
they would not perform a biopsy; 4 patients (23.5%) had standard
visual biopsies that were negative or CIN1 and 2 patients (11.8%)
had CIN2 in a standard visual biopsy preceding the DSI-assisted
biopsy that detected CIN3+.
A similar trend was observed for the detection of
women with CIN2+. Standard visual biopsy detected 75 women, which
corresponds to a detection rate of 6.12% (95% CI, 4.84-7.61%). The
additional DSI-assisted biopsies detected another 40 women with
CIN2+, which increased the detection rate to 9.38% (95% CI,
7.81-11.15%), a 53.3% relative increase over the detection by
standard visual biopsy.
Biopsy efficiency
In a secondary analysis, the biopsy efficiency to
detect CIN3+ was investigated, and the results were compared
between the two arms and within the prospective arm (data not
shown).
Comparing the total number of biopsies taken in each
arm to the number of patients detected with CIN3+, suggests that
biopsy was less efficient in the retrospective arm, i.e., more
biopsies were required to detect a patient with CIN3+ in the
retrospective compared with the prospective arm (42.2 vs. 30.8,
respectively); however, this difference was not statistically
significant (two-sided P=0.164 for the ratio, computed by inverting
the two exact binomial tests).
To compare the PPV of biopsy in the two arms, 1
patient with CIN3 from the retrospective arm was excluded as she
had multiple biopsies taken, but all of them had been processed
together. CIN3+ was detected in 37/1,306 biopsies in the
retrospective arm vs. 58/1,478 in the prospective arm. The PPVs
were 2.83% (95% CI, 2.0-3.88%) and 3.92% (95% CI, 2.99-5.04%) in
the retrospective and prospective arms, respectively. The 1.09%
difference was not statistically significant (95% CI, −0.27-2.46%;
P=0.118; two-sided Fisher exact test).
Within the prospective arm, biopsies were considered
separately as standard/visual and DSI-assisted, in order to analyze
their PPV. Overall, 34/966 standard biopsies and 23/482
DSI-assisted biopsies were CIN3+, with PPVs of 3.52% (95% CI,
2.45-4.88%) and 4.77% (95% CI, 3.05-7.07%), respectively. The 1.25%
difference was not statistically significant (95% CI, −0.83-3.75%;
P=0.254; two-sided Fisher's exact test).
To compare standard/visual biopsy across the two
arms, only the first part of prospective arm examinations (biopsy
selection by standard visualization) was considered. The number of
standard/visual biopsies per patient was higher in the
retrospective arm compared with the prospective arm (0.97 vs. 0.79;
P<0.001; two-sided Kruskal-Wallis test); however, the PPV for
detecting CIN3+ was comparable to prospective arm biopsies (2.83%
vs. 3.52%; P=0.394; two-sided Fisher's exact test), resulting in
the comparable detection rates for CIN3+ (2.29% vs. 2.45%; P=0.797;
two sided Fisher's exact test).
Discussion
ASC-US is an equivocal cytologic state with low-risk
for CIN3+ (6), unless it is combined
with HPV positivity or persistence. In this case, the risk matches
the risk of low-grade squamous intraepithelial lesion (LSIL),
leading to a referral for colposcopy (23). The present analysis of patients with
ASC-US demonstrated that the use of the study's digital colposcope
and the adjunctive DSI aid, resulted in a CIN3+ detection rate
significantly higher compared with retrospective controls, which
was achieved with only 1 more biopsy per 5 patients and without
increasing the number of women undergoing biopsy. The increased
number of biopsies in the prospective arm appears insufficient to
explain the increased detection of patients with CIN3+, as the
18.8% increase in the number of biopsies increased the detection by
as much as 70.9%.
Biopsies selected based on standard visualization
(DSI-assisted biopsies not considered for the prospective arm) had
comparable detection rates (2.29 vs. 2.45%), indicating that
visual/standard colposcopy may be equivalent in the two arms and
that the overall increase in the prospective arm may have been
primarily due to the use of adjunctive DSI for biopsy selection.
The secondary analyses performed on the biopsy-level did not find
significantly different results, which may be due to insufficient
numbers, and should therefore be interpreted with caution. However,
the results from these secondary analyses suggested that
prospective arm biopsies were more efficient than retrospective
control arm biopsies. Proportionally more biopsies detected CIN3+
and it took fewer biopsies to identify a patient with CIN3+ in the
prospective arm. Furthermore, the DSI-assisted biopsies
specifically, exhibited the highest PPV, despite the disadvantage
of being selected after the visual assessment, which should have
identified the majority of obvious lesions, had been completed.
A previous analysis from the IMPROVE-COLPO study
analyzed results from a less specific cohort than in the present
study and used the global threshold for high-grade disease (CIN2)
(21), which however, is less
reproducible than CIN3 and often regresses (27). This previous study analyzed together
all low-grade referrals, i.e., women with LSIL, ASC-US and HPV+. It
had included about half of the women that are also included in the
present analysis (1,461/2,579) and had reported that detection of
women with high-grade disease (CIN2+) was 31% higher in the
prospective arm compared with the controls. The association between
detection of CIN2+ and numbers of biopsies taken was modelled,
suggesting that biopsy efficiency was higher in the prospective arm
(21), which is consistent with the
observations from the present study. Another previous study that
analyzed mixed referrals (low-grade and high-grade) and in
particular the effect of DSI-assisted biopsies, had obtained
similar conclusions (22).
Comparing populations and findings in the present
study of colposcopy in community-based clinics with those of
academic institution-based trials (6,12) or
other large cohorts (28),
highlights some differences. In the HPV triage arm of the ASC-US
LSIL triage study (ALTS), 8.7% of patients with ASC-US had CIN3+
(6), and in the NCI biopsy study,
~7% of ASC-US patients had CIN3+ (12). These numbers are higher compared with
the overall incidences reported in the present study (4.14 and
5.71% in the retrospective and prospective arm, respectively). The
Kaiser Permanente Northern California (KPNC) reported a 5-year
cumulative incidence for CIN3+ among patients with ASC-US/HPV+ of
4.95% (28), which is closer to the
4.14 and 5.71% detected in the present study in a single colposcopy
visit. These disparities may be explained by differences in
population characteristics. For example, in the NCI study, the
median patient age was 26 years (12), whereas it was 34 years in the present
study. In addition, the distribution of referral grades in these
cohorts varied considerably. The ASC-US cases represented 23.8% in
the NCI biopsy study, 20.9% in KPNC and 34.2% in the present study.
Although this is difficult to interpret, it may be hypothesized
that the considerably higher proportion of ASC-US referrals among
patients having colposcopy in community-based clinics in the
present study, combined with the higher age and a mostly privately
insured population, may suggest that this is a lower-risk
population compared with what is typically seen in academic
centers. The present study suggests that the incorporation of the
DSI map to identify and quantify acetowhitening is an aid that
increases disease detection, supporting adherence to ASCCP guidance
by ensuring that acetowhitening is not underestimated and that
biopsy placement is improved.
The present study had some limitations. Firstly,
without additional biopsies, excisional treatments or longitudinal
follow-up, cases of missed disease cannot be confirmed, precluding
the calculation of true sensitivity. However, the relative increase
of detection rate in the prospective arm compared with that of the
retrospective arm corresponds to an equal increase in sensitivity.
Without additional detailed analyses of the histological findings
that were out of scope (e.g., adjudication and lesion size
comparison in treatment specimen), it is hard to confirm the
clinical significance of the present results. However, since the
primary analysis in the present study was for CIN3+ and the
difference in detection was significant, the results from this
study may reflect true impact on patient outcomes. Secondly, a
direct comparison between the use of DSI for additional biopsies
and the collection of additional ‘standard’ biopsies per patient
(10,12) was not addressed in the present
observational setting. Thirdly, the lack of strict guidance by the
study protocol on how to use the DSI map for biopsy could introduce
uncertainty about the generalization of the results from the
present study; however, this may have a minimal impact due to the
large sample size and the large number of participating
colposcopists.
One strength of the present study is that
‘real-world’ data, i.e., data representing routine practice, were
collected both in the control arm and in the active arm with
pragmatic use of DSI, from consecutive patients and with minimal
exclusions. In US community-based colposcopy clinics, in contrast
to recommendations (10,12), biopsy is performed conservatively
(16) as illustrated by the <1
biopsy being taken per patient with ASC-US in the present study,
which may be leading to disease being missed.
In conclusion, the results from the present study
suggest that digital colposcopy combined with DSI mapping may
increase the detection of CIN3+ lesions among women with ASC-US.
The results from the present study also suggest that, in order to
obtain a detection rate for standard visual colposcopy comparable
to that achieved with the use of DSI mapping, colposcopists would
likely have to increase the number of biopsies taken per patient by
more than the 18.8% observed in the present study. These findings
may allow the implementation of changes in clinical practice, and
therefore reduce the negative impact on patients and the cost of
medical care.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was funded by DYSIS Medical,
Edinburgh, UK. The study sponsor was involved in the study design,
the collection, analysis and interpretation of data, the writing of
the report and the decision to submit the paper for
publication.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
KEH, MDA and SD were site principal investigators
for this study and made substantial contributions towards the
acquisition, analysis and interpretation of data. EP and PTL were
involved in the design of the study. PTL performed the statistical
analyses. EP, PTL and KEH drafted the manuscript. MDA and SD
critically revised the manuscript for intellectually important
content. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study did not require a specific
Institutional Review Board approval. The IMPROVE-COLPO study was
approved by the E&I Review Services, Independence, MO (approval
no. 14067), The University of Toledo Biomedical Institutional
Review Board, Toledo, OH (approval no. 200864) and the Advocate
Health Care Institutional Review Board, Downers Grove, IL (approval
no. 6248). All patients in the prospective arm signed informed
consent prior to participation, and consent was waived by the
Institutional Review Boards for patients in the retrospective
arm.
Patient consent for publication
Not applicable.
Competing interests
KEH, PTL, MDA and SD declare that their institutions
received grants from DYSIS Medical for the performance of the
study. EP is an employee of DYSIS Medical. The study sponsor was
involved in the study design, the collection, analysis and
interpretation of data, the writing of the report and the decision
to submit the paper for publication.
Glossary
Abbreviations
Abbreviations:
|
ASCCP
|
American Society for Colposcopy and
Cervical Pathology
|
|
NCI
|
National Cancer Institute
|
|
DSI
|
dynamic spectral imaging
|
|
CIN
|
cervical intraepithelial neoplasia
|
|
ASC-US
|
atypical squamous cells of
underdetermined significance
|
|
IRB
|
Institutional Review Board
|
|
HPV
|
human papillomavirus
|
|
ECS
|
endocervical sampling
|
|
PPV
|
positive predictive value
|
|
CI
|
confidence interval
|
|
LSIL
|
low-grade squamous intraepithelial
lesion
|
|
ALTS
|
ASC-US LSIL triage study
|
|
KPNC
|
Kaiser Permanente Northern
California
|
References
|
1
|
Saslow D, Solomon D, Lawson HW, Killackey
M, Kulasingam SL, Cain J, Garcia FA, Moriarty AT, Waxman AG, Wilbur
DC, et al: American cancer society, American society for colposcopy
and cervical pathology, and American society for clinical pathology
screening guidelines for the prevention and early detection of
cervical cancer. J Low Genit Tract Dis. 16:175–204. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kinney W, Wright TC, Dinkelspiel HE,
DeFrancesco M, Cox TJ and Huh W: Increased cervical cancer risk
associated with screening at longer intervals. Obstet Gynecol.
125:311–315. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schiffman M and Wentzensen N: A suggested
approach to simplify and improve cervical screening in the United
States. J Low Genit Tract Dis. 20:1–7. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kim JJ, Campos NG, Sy S, Burger EA, Cuzick
J, Castle PE, Hunt WC, Waxman A and Wheeler CM; New Mexico HPV Pap
Registry Steering Committee, : Inefficiencies and high-value
improvements in U.S. cervical cancer screening practice: A
cost-effectiveness analysis. Ann Intern Med. 163:589–597. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Massad LS and Collins YC: Strength of
correlations between colposcopic impression and biopsy histology.
Gynecol Oncol. 89:424–428. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
ASCUS-LSIL Traige Study (ALTS) Group, :
Results of a randomized trial on the management of cytology
interpretations of atypical squamous cells of undetermined
significance. Am J Obstet Gynecol. 188:1383–1392. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
ASCUS-LSIL Traige Study (ALTS) Group, : A
randomized trial on the management of low-grade squamous
intraepithelial lesion cytology interpretations. Am J Obstet
Gynecol. 188:1393–1400. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jeronimo J and Schiffman M: Colposcopy at
a crossroads. Am J Obstet Gynecol. 195:349–353. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Khan MJ, Werner CL, Darragh TM, Guido RS,
Mathews C, Moscicki AB, Mitchell MM, Schiffman M, Wentzensen N,
Massad LS, et al: ASCCP colposcopy standards: Role of colposcopy,
benefits, potential harms, and terminology for colposcopic
practice. J Low Genit Tract Dis. 21:223–229. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wentzensen N, Schiffman M, Silver MI, Khan
MJ, Perkins RB, Smith KM, Gage JC, Gold MA, Conageski C, Einstein
MH, et al: ASCCP colposcopy standards: Risk-based colposcopy
practice. J Low Genit Tract Dis. 21:230–234. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Belinson JL and Pretorius RG: A standard
protocol for the colposcopy exam. J Low Genit Tract Dis.
20:e61–e62. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wentzensen N, Walker JL, Gold MA, Smith
KM, Zuna RE, Mathews C, Dunn ST, Zhang R, Moxley K, Bishop E, et
al: Multiple biopsies and detection of cervical cancer precursors
at colposcopy. J Clin Oncol. 33:83–89. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
TOMBOLA (Trial Of Management of Borderline
and Other Low-grade Abnormal smears) Group, . Sharp L, Cotton S,
Cochran C, Gray N, Little J, Neal K and Cruickshank M:
After-effects reported by women following colposcopy, cervical
biopsies and LLETZ: Results from the TOMBOLA trial. BJOG.
116:1506–1514. 2009.
|
|
14
|
Stoler MH, Vichnin MD, Ferenczy A, Ferris
DG, Perez G, Paavonen J, Joura EA, Djursing H, Sigurdsson K,
Jefferson L, et al: The accuracy of colposcopic biopsy: Analyses
from the placebo arm of the Gardasil clinical trials. Int J Cancer.
128:1354–1362. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Huh WK, Papagiannakis E and Gold MA:
Observed colposcopy practice in US community-based clinics: The
retrospective control arm of the IMPROVE-COLPO study. J Low Genit
Tract Dis. 23:110–115. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cooper CP and Saraiya M: Primary HPV
testing recommendations of US providers, 2015. Prev Med.
105:372–377. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Soutter WP, Diakomanolis E, Lyons D,
Ghaem-Maghami S, Ajala T, Haidopoulos D, Doumplis D, Kalpaktsoglou
C, Sakellaropoulos G, Soliman S, et al: Dynamic spectral imaging:
Improving colposcopy. Clin Cancer Res. 15:1814–1820. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Louwers JA, Zaal A, Kocken M, Ter Harmsel
W, Graziosi G, Spruijt J, Berkhof J, Balas C, Papagiannakis E,
Snijders P, et al: Dynamic spectral imaging colposcopy: Higher
sensitivity for detection of premalignant cervical lesions. BJOG.
118:309–318. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Coronado PJ and Fasero M: Colposcopy
combined with dynamic spectral imaging. A prospective clinical
study. Eur J Obstet Gynecol Reprod Biol. 196:11–16. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kaufmann A, Founta C, Papagiannakis E,
Naik R and Fisher A: Standardized digital colposcopy with dynamic
spectral imaging for conservative patient management. Case Rep
Obstet Gynecol. 2017:52692792017.PubMed/NCBI
|
|
21
|
Cholkeri-Singh A, Lavin PT, Olson CG,
Papagiannakis E and Weinberg L: Digital colposcopy with dynamic
spectral imaging for detection of cervical intraepithelial
neoplasia 2+ in low-grade referrals: The IMPROVE-COLPO study. J Low
Genit Tract Dis. 22:21–26. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
DeNardis SA, Lavin PT, Livingston J,
Salter WR, James-Patrick N, Papagiannakis E, Olson CG and Weinberg
L: Increased detection of precancerous cervical lesions with
adjunctive dynamic spectral imaging. Int J Womens Health.
9:717–725. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Massad LS, Einstein MH, Huh WK, Katki HA,
Kinney WK, Schiffman M, Solomon D, Wentzensen N and Lawson HW; 2012
ASCCP Consensus Guidelines Conference, : 2012 updated consensus
guidelines for the management of abnormal cervical cancer screening
tests and cancer precursors. J Low Genit Tract Dis. 17 (5 Suppl
1):S1–S27. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Castle PE, Stoler MH, Solomon D and
Schiffmanx M: The relationship of community biopsy-diagnosed
cervical intraepithelial neoplasia grade 2 to the quality control
pathology-reviewed diagnoses: An ALTS report. Am J Clin Pathol.
127:805–815. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Huh WK, Ault KA, Chelmow D, Davey DD,
Goulart RA, Garcia FA, Kinney WK, Massad LS, Mayeaux EJ, Saslow D,
et al: Use of primary high-risk human papillomavirus testing for
cervical cancer screening: Interim clinical guidance. Gynecol
Oncol. 136:178–182. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Schiffman M and Rodríguez AC:
Heterogeneity in CIN3 diagnosis. Lancet Oncol. 9:404–406. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Tainio K, Athanasiou A, Tikkinen KAO,
Aaltonen R, Cárdenas J, Hernándes, Glazer-Livson S, Jakobsson M,
Joronen K, Kiviharju M, et al: Clinical course of untreated
cervical intraepithelial neoplasia grade 2 under active
surveillance: Systematic review and meta-analysis. BMJ.
360:k4992018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Demarco M, Lorey TS, Fetterman B, Cheung
LC, Guido RS, Wentzensen N, Kinney WK, Poitras NE, Befano B, Castle
PE and Schiffman M: Risks of CIN 2+, CIN 3+, and cancer by cytology
and human papillomavirus status: The foundation of risk-based
cervical screening guidelines. J Low Genit Tract Dis. 21:261–267.
2017. View Article : Google Scholar : PubMed/NCBI
|