Introduction
Cervical cancer is the fourth most common cancer
type among females worldwide, with >500,000 new cases diagnosed
in 2018; 11,000 patients are diagnosed and ~3,000 patients die
annually in Japan (1,2). Although squamous cell carcinoma
continues to be the most frequent pathological type, the incidence
of cervical adenocarcinoma (AC) and adenosquamous carcinoma (ASC)
has increased in several countries (3–5). AC and
ASC of the uterine cervix accounted for 15–25% of all cases of
cervical cancer (3,5) and the affected patients were younger
than those with squamous cell carcinoma (SCC) (5).
The prognosis of patients with AC and ASC has been
evaluated in several studies, but the results remain controversial
(6–18). Certain studies have indicated that
the prognosis of AC and ASC is worse than that of SCC, while others
reported a similar prognosis. In addition, AC and ASC are less
radiosensitive than SCC (16,19).
Hence, it remains elusive whether the treatment strategy used for
SCC may be adopted for patients with AC and ASC. Therefore, the
factors associated with the prognosis of AC and ASC and the
biomarkers targetable with molecular targeted drugs require
investigation.
Erb-b2 receptor tyrosine kinase 3 (HER3) is a member
of the epidermal growth factor receptor (EGFR) family and is a
cell-surface receptor tyrosine kinase (20). HER3 overexpression is associated with
unfavorable prognosis in several cancer types (21). Although the incidence of HER3
overexpression ranged from 55.6 to 74.4% among cases of SCC of the
cervix and HER3 was indicated to be a poor prognostic factor,
information regarding the expression of HER3 in cases of AC and ASC
of the cervix and whether it is a prognostic factor remains limited
(22,23). Therefore, the present study aimed to
evaluate the expression of HER3 and its significance in the
post-operative recurrence in patients with AC and ASC of the
cervix.
Patients and methods
Patients and specimens
The medical records of patients with cervical cancer
who were diagnosed and treated at the National Cancer Center
Hospital (Tokyo, Japan), between January 1997 and December 2017
were retrospectively analyzed. Patients included in the present
study fulfilled the following inclusion criteria: i) Pathological
diagnosis of AC and ASC of the cervix, ii) early-stage disease
[International Federation of Gynecology and Obstetrics (FIGO)
stages I and II] and iii) availability of sufficient formalin-fixed
paraffin-embedded surgical specimens for immunohistochemical
staining and analysis (24).
Specimens of 39 cases of AC (n=27) and ASC (n=12) of
the cervix obtained via surgical resection were retrieved from the
pathology database of the National Cancer Center Hospital (Tokyo,
Japan). The histological type was based on the World Health
Organization classification of tumors of the uterine cervix (4th
edition) (25). The medical records
of all the identified patients were evaluated to obtain the
following information: Age, performance status at diagnosis, FIGO
clinical stage, date of treatment initiation, date of surgery, date
of radiotherapy, the administered chemotherapy regimen, date of
progression, date of the last follow-up and survival status. The
protocol for the human study was reviewed and approved by the
ethics committee of the National Cancer Center Hospital (Tokyo,
Japan; no. 2014-393). Written informed consent was obtained from
all of the participants.
Immunohistochemical staining and
analysis
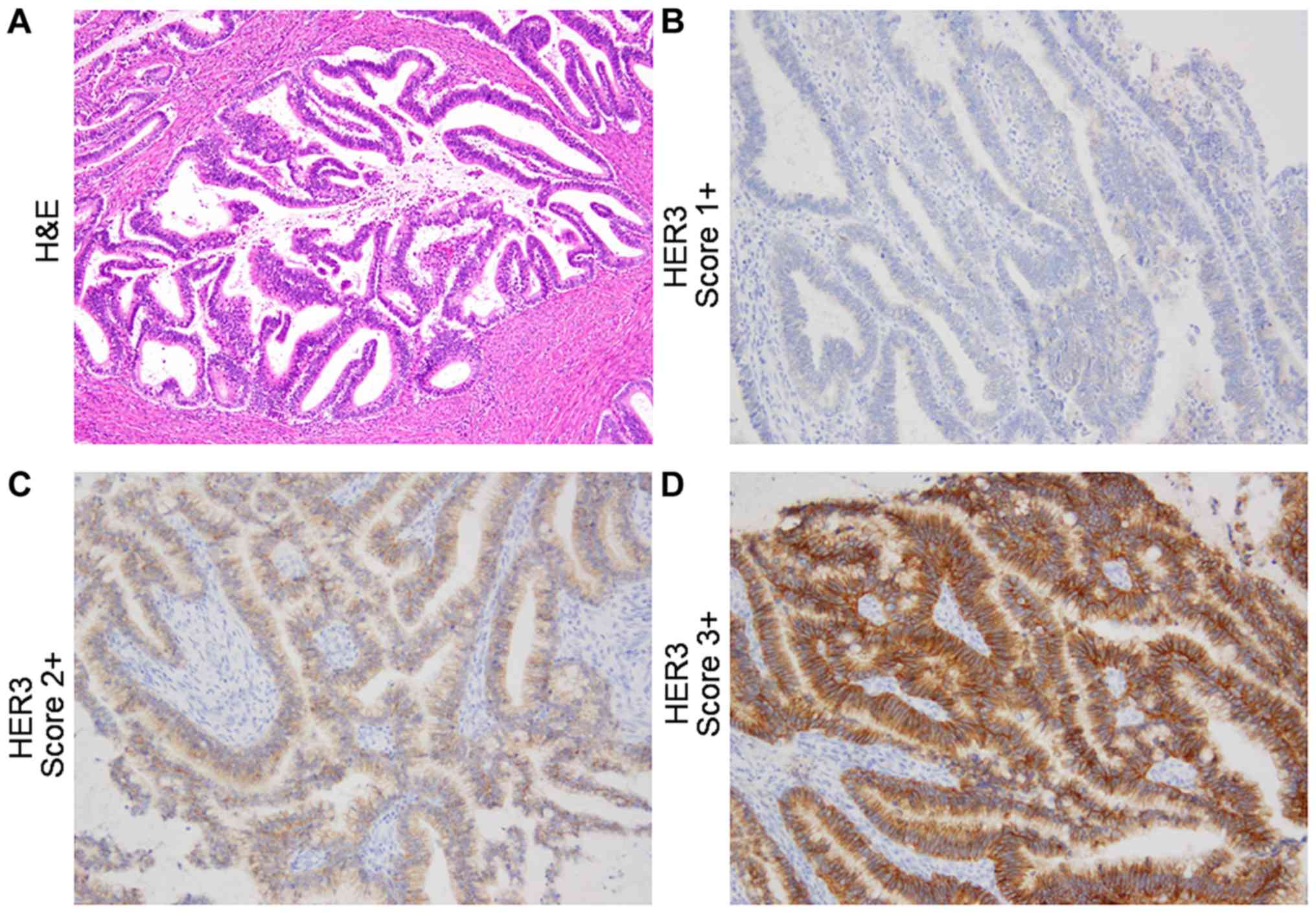
Hematoxylin and eosin (H&E)-stained slides from
each of the cases were reviewed to obtain representative sections.
New 4-µm-thick sections were prepared from formalin-fixed
paraffin-embedded surgical specimens and were immunohistochemically
stained. After deparaffinization, the expression of HER3 was
determined by immunohistochemistry using a rabbit monoclonal
antibody against HER3 (1:59 dilution; clone D22C5; Cell Signaling
Technology, Inc.). Antigen retrieval was achieved by using a PT
Link machine (Dako) at high pH. Immunohistochemistry staining was
performed using the Dako autostainer Link48 (Dako) and EnVision
Flex Mini kit (Dako), according to the manufacturer's protocols.
The slides were counterstained with hematoxylin.
HER3 expression was evaluated by an experienced
pathologist in accordance with the HER2 testing guidelines for
gastroesophageal cancer from the College of American Pathologists,
American Society for Clinical Pathology and American Society of
Clinical Oncology (26). High HER3
expression (HER3-high) was defined as a score of 2+ or 3+ and low
HER3 expression (HER3-low) was defined as a score of 0 or 1+.
Immunohistochemical staining of p16 (clone INK4, 1;10, BD
Bioscience) was also performed for the representative tumor section
of each case. The slides were evaluated by the pathologist with the
cut-off for positivity >70%. The pathologist was blinded to the
clinical data while evaluating the slides.
Statistical analysis
Disease-free survival (DFS) was defined as the time
between the date of initial surgery to the date of documentation of
relapse, including locoregional recurrence and/or distant
metastasis or death from any cause. The absence of relapse or death
was treated as a censored observation. Overall survival (OS) was
defined as the time from the date of initial surgery to the date of
death from any cause. Patients without such events were treated as
censored observations. DFS and OS were estimated using the
Kaplan-Meier method and survival curves were compared using the
log-rank test. A possible influence of HER3 expression on survival
was assessed by using univariate and multivariate Cox regression
analyses with the forced entry method after adjustment for
established risk factors of post-operative recurrence (27–29). A
two-sided P<0.05 was considered to indicate statistical
significance. All statistical analyses were performed with EZR
(Saitama Medical Center, Jichi Medical University) (30), which is a graphical user interface
for R (The R Foundation for Statistical Computing).
Results
Patient characteristics
Of the 39 patients with stages Ib1-IIB included in
the present study, 27 were histologically classified as AC and 12
as ASC. The demographic and clinicopathological characteristics of
the patients are summarized in Table
I. The study population included 39 patients with an age range
of 32 to 67 years. The median age of the patients was 43 years. The
clinical stage of the patients determined according to the FIGO
staging system was stage IB1 in 25 patients, IB2 in 9 and IIB in 4
patients. Lymph node metastasis was present in 38.5% of patients.
Expression of p16 was positive in 79.8% (31/39) of all cases, 70.4%
(19/27) of cases of AC and 100.0% (12/12) of cases of ASC.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
|
| HER3
expression |
|
|---|
|
|
|
|
|---|
| Parameter | High (n=30) | Low (n=9) | P-value |
|---|
| Age (years) | 42.5 (30–67) | 46.0 (40–64) | 0.384 |
| FIGO stage
(2014) |
|
| 0.216 |
|
IB1 | 20 (66.6) | 5 (55.5) |
|
|
IB2 | 8 (26.6) | 2 (22.2) |
|
|
IIB | 2 (6.6) | 2 (22.2) |
|
| Histological
type |
|
| 0.066 |
|
Adenocarcinoma | 23 (76.6) | 4 (44.4) |
|
|
Adenosquamous carcinoma | 7 (23.3) | 5 (55.5) |
|
| Parametrial
invasion |
|
| 0.311 |
|
Present | 8 (26.7) | 4 (44.4) |
|
|
Absent | 22 (73.3) | 5 (55.5) |
|
| Vascular
invasion |
|
| 0.134 |
| 0 | 13 (43.3) | 3 (33.3) |
|
| 1 | 13 (43.3) | 5 (55.5) |
|
| 2 | 3 (10.0) | 1 (11.1) |
|
| 3 | 1 (3.3) | 0 (0.0) |
|
| Tumor size
(cm) |
|
| 0.379 |
| ≤4 | 15 (50.0) | 6 (66.6) |
|
|
>4 | 15 (50.0) | 3 (3.33) |
|
| Lymph node
metastases |
|
| 0.047 |
|
Present | 21 (70.0) | 3 (33.3) |
|
|
Absent | 9 (30.0) | 6 (66.6) |
|
| Treatment |
|
| 0.145 |
| Surgery
alone | 15 (50.0) | 3 (33.3) |
|
| Surgery
+ adjuvant radiation | 13 (43.3) | 5 (55.5) |
|
| Surgery + adjuvant
chemoradiation | 2 (6.6) | 1 (11.1) |
|
Immunohistochemistry staining for HER3
expression in AC and ACC of the cervix
HER3 expression was determined in the surgical
specimens from 39 patients with AC and ASC of the cervix using
immunohistochemistry. Membranous HER3 overexpression was evaluated
according to the criteria described above and representative images
are provided in Fig. 1. High
expression of HER3 (HER3-high) was determined in 85.1% (23/27) of
cases of AC and in 58.3% (7/12) of cases of ASC (Table II).
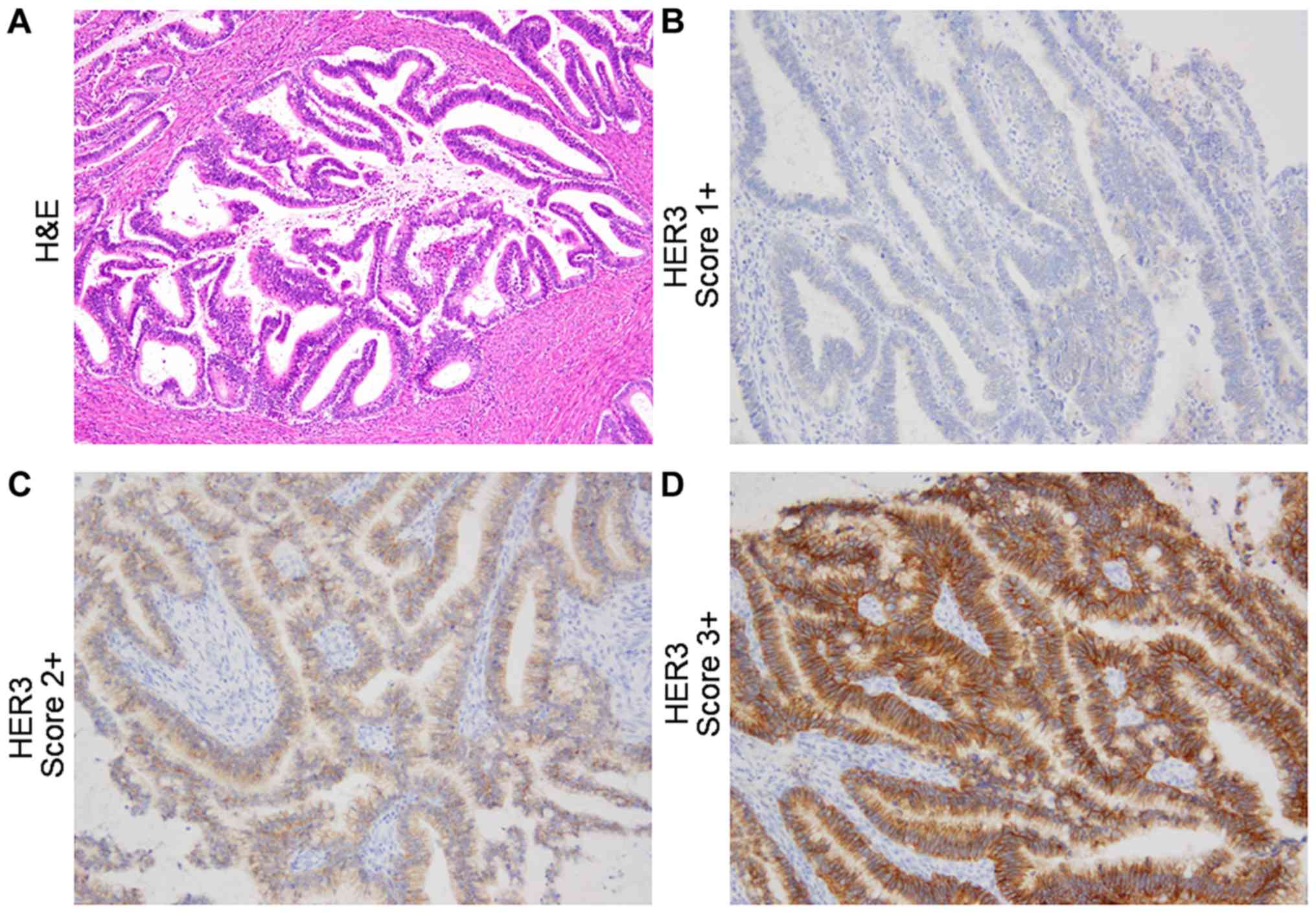 | Figure 1.Representative histology images. (A)
H&E staining. (B-D) Immunohistochemical staining for HER3; (B)
endocervical adenocarcinoma, usual type, pT1bN0, with HER3 score of
1+; (C) endocervical adenocarcinoma, usual type, pT2bN1, HER3 score
of 2+; (D) endocervical adenocarcinoma, usual type, pT2bN1, HER3
score of 3+ (original magnification of all the histological images,
×200). HER3 was predominantly expressed in the cytoplasm and on the
membranes of tumor cells. HER3, Erb-b2 receptor tyrosine kinase 3;
H&E, hematoxylin and eosin. |
 | Table II.Expression score of HER3 in cervical
adenocarcinoma and adenosquamous carcinoma. |
Table II.
Expression score of HER3 in cervical
adenocarcinoma and adenosquamous carcinoma.
| Histological
type | N | 0 | 1+ | 2+ | 3+ | 2+/3+ |
|---|
| Adenocarcinoma | 27 | 0 (0.0) | 4 (14.8) | 12 (44.4) | 11 (40.7) | 23 (85.1) |
| Adenosquamous
carcinoma | 12 | 0 (0.0) | 5 (41.7) | 4 (33.3) | 3 (25.0) | 7 (58.3) |
| Total | 39 | 0 (0.0) | 9 (23.1) | 16 (41.0) | 14 (35.9) | 30 (76.9) |
Association of HER3 expression with
outcomes
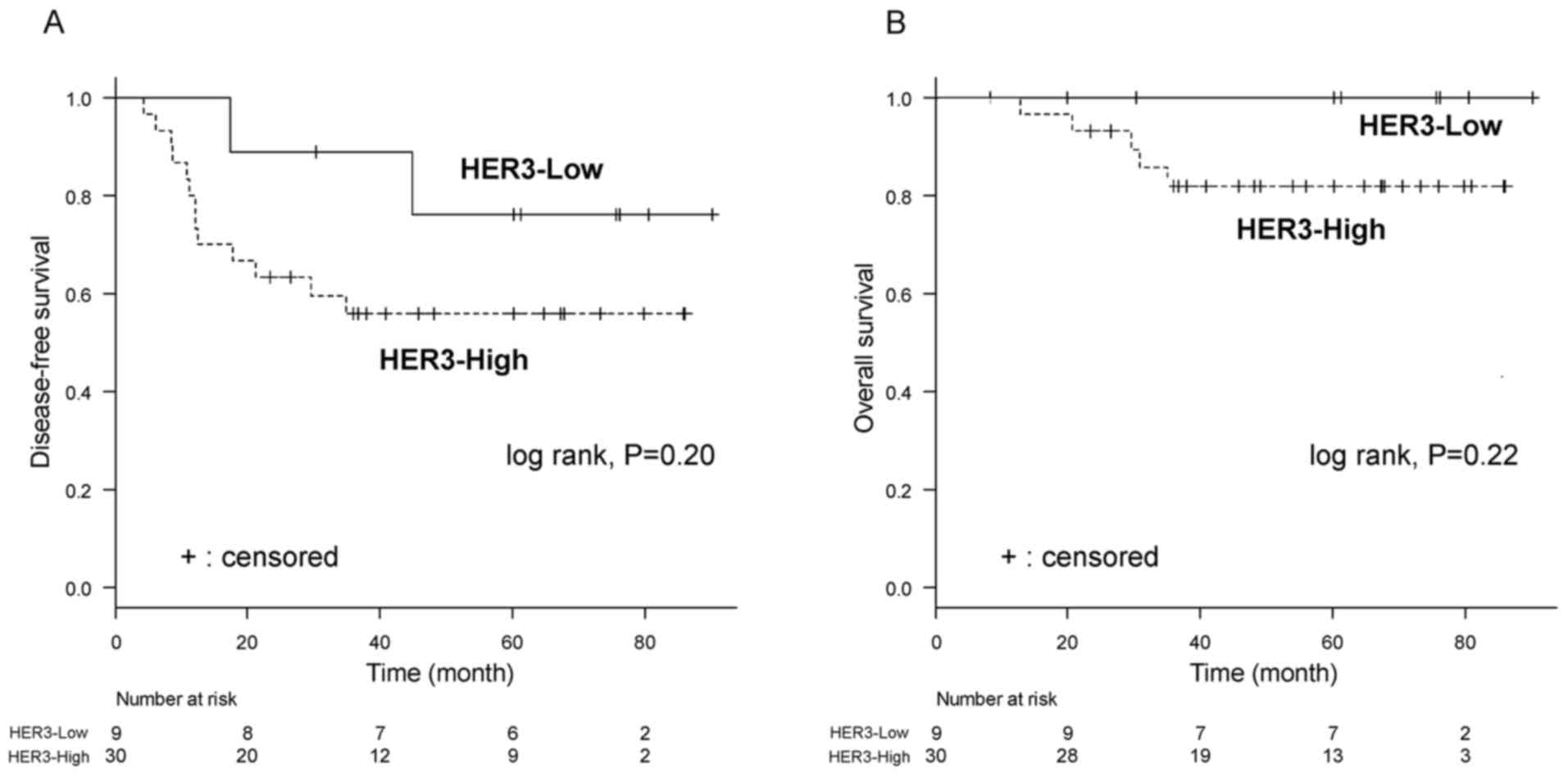
During the median follow-up of 63.1 months, the
5-year DFS rates in patients with AC and ASC of the cervix were
56.7% among patients with HER3-high and 77.8% among patients with
HER3-low (log-rank P=0.20; Fig 2A).
The 5-year OS rates were 83.3% among patients with HER3-high and
100.0% among patients with HER3-low (log-rank P=0.22; Fig 2B). Multivariate logistic regression
analysis with the Cox proportional hazards model revealed that
HER3-high [hazard ratio (HR)=6.32, 95% CI: 1.10–36.26, P=0.039),
pelvic lymph node metastasis (HR=7.61, 95% CI: 2.07–28.00, P=0.002)
and vascular invasion (HR=4.28, 95% CI: 1.12–16.31, P=0.033) were
independent prognostic factors regarding DFS (Table III).
 | Table III.Univariate and multivariate analysis
of prognostic factors for disease-free survival. |
Table III.
Univariate and multivariate analysis
of prognostic factors for disease-free survival.
|
| Univariate |
| Multivariate |
|
|---|
|
|
|
|
|
|
|---|
| Factor | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| HER3 (high vs.
low) | 2.54 | 0.57–11.31 | 0.220 | 6.32 | 1.10–36.26 | 0.039 |
| Pelvic lymph node
metastasis (present vs. absent) | 3.17 | 1.12–8.98 | 0.030 | 7.61 | 2.07–28.00 | 0.002 |
| Tumor size (≥4 vs.
<4 cm) | 1.67 | 0.60–4.63 | 0.322 | 1.05 | 0.30–3.69 | 0.942 |
| Vascular invasion
(present vs. absent) | 3.28 | 1.04–10.39 | 0.043 | 4.28 | 1.12–16.31 | 0.033 |
| Parametrial
invasion (present vs. absent) | 1.62 | 0.58–4.57 | 0.361 | 0.68 | 0.18–2.59 | 0.570 |
Discussion
The results of the present study suggested an
association between the clinical outcomes of early-stage AC and ASC
of the cervix and HER3 expression. Although HER3 expression did not
exhibit any statistical significance on univariate Cox analysis for
DFS, HER3 was a significant predictor on multivariate Cox analysis,
indicating unfavorable DFS and OS prognosis. To the best of our
knowledge, the present study was so far the largest to evaluate the
expression of HER3 and its significance on post-operative
recurrence in patients with early-stage AC and ASC of the
cervix.
HER3 is overexpressed in several cancer types and is
associated with poor prognosis (20,31–38).
HER3 promotes tumor initiation and progression, mainly through
heterodimerization with receptor tyrosine kinases, to activate
oncogenic signaling via the PI3K/AKT pathway. In addition, HER3
expression and downstream PI3K/AKT signaling are major causes of
treatment failure in cancer therapy due to their implication in
therapeutic resistance (39). In the
present study, HER3 expression was not a prognostic factor in the
univariate Cox regression for DFS, on the other hand, HER3
overexpression appeared to be a poor prognostic factor for DFS in
the multivariate Cox regression, along with pelvic lymph node
metastasis and vascular invasion. This discrepancy between
univariate and multivariate results can be attributed to the small
number of cases and the resulting instability of the prognostic
model. These results are still consistent with those of previous
studies on patients with cervical cancer with SCC, in which HER3
was overexpressed in 74.4% (58/78) of patients and was associated
with poor prognosis (22). In a
study by Lee et al (23), 55
patients with FIGO IB-IVA cervical cancer, including 5 patients
with AC and 2 with ASC, were evaluated for the expression of HER
and phosphorylated AKT. However, the incidence of HER3
overexpression and its influence on survival among those
populations were not presented, thereby remaining elusive.
Therefore, the present study was the first to demonstrate the
prognostic value of HER3 overexpression among patients with
cervical AC and ASC. Due to the aforementioned discrepancy between
the univariate and multivariate Cox regression model, the
prognostic value of HER3 should be further verified in future
studies. Combining the results of the present study with those
obtained in previous studies, the incidence of HER3 overexpression
was 55.6–74.4% in patients with SCC, 85.1% in patients with AC and
58.3% in patients with ASC (22,23).
Whole-exome sequencing of primary frozen tumor tissues and the
blood of patients with cervical cancer who did not receive any
prior chemotherapy or radiotherapy indicated that the incidence of
HER3 alterations was higher in patients with AC than in those with
SCC (40). Several targeted
therapies have been developed for HER3 and relevant studies
indicate a possible therapeutic strategy for patients with cervical
cancer expressing HER3 (41,42).
Surgery and/or radiotherapy are highly effective for
early-stage cervical cancer. However, patients with AC and ASC of
the cervix are more resistant to radiotherapy than those with SCC
(16,19); therefore, novel therapies are
required for patients with AC and ASC of the cervix. Recently,
combination therapy with a dual antibody targeting both EGFR and
HER3 and enhanced ionizing radiation was reported to be effective
(43). An additive effect was
observed when the dual antibody, radiation and cisplatin were
combined, leading to improved patient outcomes by increasing tumor
control and by activating the immune response.
The human papillomavirus (HPV) is a carcinogenic
virus in humans and has been implicated in cervical cancer
(44). Among head and neck cancers,
HER3 was overexpressed and highly bound to PI3K in HPV-positive
tumors (45). In addition, a
preclinical study by Brand et al (46) reported an association between HPV
infection and HER3 in head and neck cancers, indicating that
HPV-positive cancers were sensitive to HER3 targeting. By contrast,
no association has been detected between HPV infection and HER in
patients with cervical cancer. In the population included in the
present study, the incidence of both HER3 and p16 expression was
high and the correlation was not significant (data not shown).
Accordingly, further studies are required to evaluate the etiology
of HPV infection and HER3 expression in patients with cervical
cancer.
The present study has several limitations; it was a
retrospective study in a single institution and included a small
number of patients with AC and ASC in the cervix. In addition, as
the enrollement period was long, the treatment strategy varied over
the decades. Hence, further study is required to evaluate the role
of HER3 in the current era of precision medicine, during which
several HER3-targeting drugs are being developed (47–49). In
the present study, the DFS of patients who underwent surgery was
evaluated, which is an important factor for such patients; however,
the influence of HER3 on OS remains undetermined due to the small
number of patients who died. Furthermore, even though most of the
study population was positive for p16, no significant correlation
between p16 and HER3 was determined. Accordingly, future studies
are required to determine the etiology of HPV infection and HER3
expression in patients with cervical cancer.
In conclusion, the results of the present study
indicated that the expression of HER3 was associated with poor DFS
in patients with early-stage AC and ASC of the cervix; therefore,
HER3 expression may be a novel prognostic biomarker. However,
further studies are required to confirm these results and the
prognostic value of HER3.
Acknowledgements
The authors would like to thank Ms. Nao Nakamura and
Ms. Kotone Shoji, Department of Breast and Medical Oncology,
National Cancer Center Hospital (Tokyo, Japan) for their
secretarial assistance.
Funding
The National Cancer Center Biobank is supported by
the National Cancer Center Research and Development Fund,
Japan.
Availability of data and materials
The datasets used during the present study are
available from the corresponding author upon reasonable
request.
Authors' contributions
TM, YK, KY, HY, YS, YoO, HSO, TN, MT, KS, AS, EN,
TK, TS, MU, MI, YF, YuO and KT were responsible for the conception
and design of the present study, drafted the manuscript, were
responsible for the collection and assembly of the data, performed
the data analysis and interpretation, and read, revised and
approved the final manuscript. All authors are in agreement to be
accountable for all aspects of the work in ensuring that questions
related to the accuracy or integrity of any part of the work are
appropriately investigated and resolved.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the National Cancer Center Hospital (Tokyo, Japan;
approval no. 2014-393). Written informed consent was obtained from
all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Center for Cancer Control and Information
Services, National Cancer Center, . Cancer Registry and Statistics.
March
11–2016
|
|
3
|
Castanon A, Landy R and Sasieni PD: Is
cervical screening preventing adenocarcinoma and adenosquamous
carcinoma of the cervix? Int J Cancer. 139:1040–1045. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sasieni P and Adams J: Changing rates of
adenocarcinoma and adenosquamous carcinoma of the cervix in
England. Lancet. 357:1490–1493. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Galic V, Herzog TJ, Lewin SN, Neugut AI,
Burke WM, Lu YS, Hershman DL and Wright JD: Prognostic significance
of adenocarcinoma histology in women with cervical cancer. Gynecol
Oncol. 125:287–291. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Park JY, Kim DY, Kim JH, Kim YM, Kim YT
and Nam JH: Outcomes after radical hysterectomy in patients with
early-stage adenocarcinoma of uterine cervix. Br J Cancer.
102:1692–1698. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lee YY, Choi CH, Kim TJ, Lee JW, Kim BG,
Lee JH and Bae DS: A comparison of pure adenocarcinoma and squamous
cell carcinoma of the cervix after radical hysterectomy in stage
IB-IIA. Gynecol Oncol. 120:439–443. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mabuchi S, Okazawa M, Matsuo K, Kawano M,
Suzuki O, Miyatake T, Enomoto T, Kamiura S, Ogawa K and Kimura T:
Impact of histological subtype on survival of patients with
surgically-treated stage IA2-IIB cervical cancer: Adenocarcinoma
versus squamous cell carcinoma. Gynecol Oncol. 127:114–20. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shingleton HM, Bell MC, Fremgen A, Chmiel
JS, Russell AH, Jones WB, Winchester DP and Clive RE: Is there
really a difference in survival of women with squamous cell
carcinoma, adenocarcinoma, and adenosquamous cell carcinoma of the
cervix? Cancer. 76 (10 Suppl):1948–1955. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Farley JH, Hickey KW, Carlson JW, Rose GS,
Kost ER and Harrison TA: Adenosquamous histology predicts a poor
outcome for patients with advanced-stage, but not early-stage,
cervical carcinoma. Cancer. 97:2196–2202. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lea JS, Coleman RL, Garner EO, Duska LR,
Miller DS and Schorge JO: Adenosquamous histology predicts poor
outcome in low-risk stage IB1 cervical adenocarcinoma. Gynecol
Oncol. 91:558–562. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
dos Reis R, Frumovitz M, Milam MR, Capp E,
Sun CC, Coleman RL and Ramirez PT: Adenosquamous carcinoma versus
adenocarcinoma in early-stage cervical cancer patients undergoing
radical hysterectomy: An outcomes analysis. Gynecol Oncol.
107:458–463. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mabuchi S, Okazawa M, Kinose Y, Matsuo K,
Fujiwara M, Suzuki O, Morii E, Kamiura S, Ogawa K and Kimura T:
Comparison of the prognoses of FIGO stage I to stage II
adenosquamous carcinoma and adenocarcinoma of the uterine cervix
treated with radical hysterectomy. Int J Gynecol Cancer.
22:1389–1397. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Noh JM, Park W, Kim YS, Kim JY, Kim HJ,
Kim J, Kim JH, Yoon MS, Choi JH, Yoon WS, et al: Comparison of
clinical outcomes of adenocarcinoma and adenosquamous carcinoma in
uterine cervical cancer patients receiving surgical resection
followed by radiotherapy: A multicenter retrospective study (KROG
13-10). Gynecol Oncol. 132:618–623. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Huang YT, Wang CC, Tsai CS, Lai CH, Chang
TC, Chou HH, Lee SP and Hong JH: Clinical behaviors and outcomes
for adenocarcinoma or adenosquamous carcinoma of cervix treated by
radical hysterectomy and adjuvant radiotherapy or
chemoradiotherapy. Int J Radiat Oncol Biol Phys. 84:420–427. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rose PG, Java JJ, Whitney CW, Stehman FB,
Lanciano R and Thomas GM: Locally advanced adenocarcinoma and
adenosquamous carcinomas of the cervix compared to squamous cell
carcinomas of the cervix in gynecologic oncology group trials of
cisplatin-based chemoradiation. Gynecol Oncol. 135:208–212. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Winer I, Alvarado-Cabrero I, Hassan O,
Ahmed QF, Alosh B, Bandyopadhyay S, Thomas S, Albayrak S, Talukdar
S, Al-Wahab Z, et al: The prognostic significance of histologic
type in early stage cervical cancer-A multi-institutional study.
Gynecol Oncol. 137:474–478. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cao L, Wen H, Feng Z, Han X and Wu X:
Distinctive clinicopathologic characteristics and prognosis for
different histologic subtypes of early cervical cancer. Int J
Gynecol Cancer. 29:1244–1251. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chen JL, Huang CY, Huang YS, Chen RJ, Wang
CW, Chen YH, Cheng JC, Cheng AL and Kuo SH: Differential clinical
characteristics, treatment response and prognosis of locally
advanced adenocarcinoma/adenosquamous carcinoma and squamous cell
carcinoma of cervix treated with definitive radiotherapy. Acta
Obstet Gynecol Scand. 93:661–668. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Plowman GD, Whitney GS, Neubauer MG, Green
JM, McDonald VL, Todaro GJ and Shoyab M: Molecular cloning and
expression of an additional epidermal growth factor
receptor-related gene. Proc Natl Acad Sci USA. 87:4905–4909. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li Q, Zhang R, Yan H, Zhao P, Wu L, Wang
H, Li T and Cao B: Prognostic significance of HER3 in patients with
malignant solid tumors. Oncotarget. 8:67140–67151. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fuchs I, Vorsteher N, Buhler H, Evers K,
Sehouli J, Schaller G and Kümmel S: The prognostic significance of
human epidermal growth factor receptor correlations in squamous
cell cervical carcinoma. Anticancer Res. 27:959–963.
2007.PubMed/NCBI
|
|
23
|
Lee CM, Shrieve DC, Zempolich KA, Lee RJ,
Hammond E, Handrahan DL and Gaffney DK: Correlation between human
epidermal growth factor receptor family (EGFR, HER2, HER3, HER4),
phosphorylated Akt (P-Akt), and clinical outcomes after radiation
therapy in carcinoma of the cervix. Gynecol Oncol. 99:415–421.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
FIGO Committee on Gynecologic Oncology, .
FIGO staging for carcinoma of the vulva, cervix, and corpus uteri.
Int J Gynaecol Obstet. 125:97–98. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bartley AN, Washington MK, Colasacco C,
Ventura CB, Ismaila N, Benson AB III, Carrato A, Gulley ML, Jain D,
Kakar S, et al: HER2 testing and clinical decision making in
gastroesophageal adenocarcinoma: Guideline From the College of
American Pathologists, American Society for Clinical Pathology, and
American Society of Clinical Oncology. Arch Pathol Lab Med.
140:1345–1363. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kurman RJ, Carcangiu ML and Herrington CS:
World Health Organization classification of tumours of female
reproductive organs. 4th. Geneva: WHO Press; 2014
|
|
27
|
Ryu SY, Kim MH, Nam BH, Lee TS, Song ES,
Park CY, Kim JW, Kim YB, Ryu HS, Park SY, et al: Intermediate-risk
grouping of cervical cancer patients treated with radical
hysterectomy: A Korean gynecologic oncology group study. Br J
Cancer. 110:278–285. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kim MK, Jo H, Kong HJ, Kim HC, Kim JW, Kim
YM, Song YS, Kang SB, Mok JE and Lee HP: Postoperative nomogram
predicting risk of recurrence after radical hysterectomy for
early-stage cervical cancer. Int J Gynecol Cancer. 20:1581–1386.
2010.PubMed/NCBI
|
|
29
|
Wang H, Zhu L, Lu W, Xu H, Yu Y and Yang
Y: Clinicopathological risk factors for recurrence after
neoadjuvant chemotherapy and radical hysterectomy in cervical
cancer. World J Surg Oncol. 11:3012013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kanda Y: Investigation of the freely
available easy-to-use software ‘EZR’ for medical statistics. Bone
Marrow Transplant. 48:452–458. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Tanner B, Hasenclever D, Stern K,
Schormann W, Bezler M, Hermes M, Brulport M, Bauer A, Schiffer IB,
Gebhard S, et al: ErbB-3 predicts survival in ovarian cancer. J
Clin Oncol. 24:4317–4323. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Witton CJ, Reeves JR, Going JJ, Cooke TG
and Bartlett JM: Expression of the HER1-4 family of receptor
tyrosine kinases in breast cancer. J Pathol. 200:290–297. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yi ES, Harclerode D, Gondo M, Stephenson
M, Brown RW, Younes M and Cagle PT: High c-erbB-3 protein
expression is associated with shorter survival in advanced
non-small cell lung carcinomas. Mod Pathol. 10:142–148.
1997.PubMed/NCBI
|
|
34
|
Reschke M, Mihic-Probst D, van der Horst
EH, Knyazev P, Wild PJ, Hutterer M, Meyer S, Dummer R, Moch H and
Ullrich A: HER3 is a determinant for poor prognosis in melanoma.
Clin Cancer Res. 14:5188–5197. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Bae SY, La Choi Y, Kim S, Kim M, Kim J,
Jung SP, Choi MY, Lee SK, Kil WH, Lee JE and Nam SJ: HER3 status by
immunohistochemistry is correlated with poor prognosis in hormone
receptor-negative breast cancer patients. Breast Cancer Res Treat.
139:741–750. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ledel F, Hallstrom M, Ragnhammar P,
Ohrling K and Edler D: HER3 expression in patients with primary
colorectal cancer and corresponding lymph node metastases related
to clinical outcome. Eur J Cancer. 50:656–662. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Qian G, Jiang N, Wang D, Newman S, Kim S,
Chen Z, Garcia G, MacBeath G, Shin DM, Khuri FR, et al: Heregulin
and HER3 are prognostic biomarkers in oropharyngeal squamous cell
carcinoma. Cancer. 121:3600–3611. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ema A, Yamashita K, Ushiku H, Kojo K,
Minatani N, Kikuchi M, Mieno H, Moriya H, Hosoda K, Katada N, et
al: Immunohistochemical analysis of RTKs expression identified HER3
as a prognostic indicator of gastric cancer. Cancer Sci.
105:1591–1600. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Amin DN, Campbell MR and Moasser MM: The
role of HER3, the unpretentious member of the HER family, in cancer
biology and cancer therapeutics. Semin Cell Dev Biol. 21:944–950.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Cancer Genome Atlas Research Network, .
Integrated genomic and molecular characterization of cervical
cancer. Nature. 543:378–384. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Jaiswal BS, Kljavin NM, Stawiski EW, Chan
E, Parikh C, Durinck S, Chaudhuri S, Pujara K, Guillory J, Edgar
KA, et al: Oncogenic ERBB3 mutations in human cancers. Cancer Cell.
23:603–617. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Karachaliou N, Lazzari C, Verlicchi A,
Sosa AE and Rosell R: HER3 as a therapeutic target in cancer.
BioDrugs. 31:63–73. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Bourillon L, Demontoy S, Lenglet A,
Zampieri A, Fraisse J, Jarlier M, Boissière-Michot F, Perrochia H,
Rathat G, Garambois V, et al: Higher anti-tumor efficacy of the
dual HER3-EGFR Antibody MEHD7945a combined with ionizing
irradiation in cervical cancer cells. Int J Radiat Oncol Biol Phys.
106:1039–1051. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Crosbie EJ, Einstein MH, Franceschi S and
Kitchener HC: Human papillomavirus and cervical cancer. Lancet.
382:889–899. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Pollock NI, Wang L, Wallweber G, Gooding
WE, Huang W, Chenna A, Winslow J, Sen M, DeGrave KA, Li H, et al:
Increased expression of HER2, HER3, and HER2:HER3 heterodimers in
HPV-Positive HNSCC using a novel proximity-based assay:
implications for targeted therapies. Clin Cancer Res. 21:4597–4606.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Brand TM, Hartmann S, Bhola NE, Peyser ND,
Li H, Zeng Y, Isaacson Wechsler E, Ranall MV, Bandyopadhyay S,
Duvvuri U, et al: Human papillomavirus regulates HER3 expression in
head and neck cancer: Implications for targeted HER3 therapy in
HPV(+) Patients. Clin Cancer Res. 23:3072–3083. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Liu JF, Ray-Coquard I, Selle F, Poveda AM,
Cibula D, Hirte H, Hilpert F, Raspagliesi F, Gladieff L, Harter P,
et al: Randomized phase II trial of seribantumab in combination
with paclitaxel in patients with advanced platinum-resistant or
-refractory ovarian cancer. J Clin Oncol. 34:4345–4353. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Kogawa T, Yonemori K, Masuda N, Takahashi
S, Takahashi M, Iwase H, Nakayama T, Saeki T, Toyama T, Takano T,
et al: Single agent activity of U3-1402, a HER3-targeting
antibody-drug conjugate, in breast cancer patients: Phase 1 dose
escalation study. J Clin Oncol. 36 (Suppl 15):25122018. View Article : Google Scholar
|
|
49
|
Janne PA, Yu HA, Johnson ML, Steuer CE,
Vigliotti M, Iacobucci C, Chen S, Yu C and Dalila B. Sellami DB;
Dana-Farber Cancer Institute; Memorial Sloan Kettering Cancer
Center; Sarah Cannon Research Institute; Winship Cancer Institute
of Emory University; Daiichi Sankyo Inc., : Safety and preliminary
antitumor activity of U3-1402: A HER3-targeted antibody drug
conjugate in EGFR TKI-resistant, EGFRm NSCLC. J Clin Oncol. 37
(Suppl 15):90102019. View Article : Google Scholar
|