Introduction
Thoracic lesions include diseased tissues in the
lung, mediastinum, pleura and chest wall, and are mostly lung
lesions, which are primarily diagnosed as lung cancer (1). To a large extent, the diagnosis,
treatment and prognosis of thoracic lesions depends on their
pathological classification (2). At
present, ultrasound (US), computed tomography (CT), magnetic
resonance imaging, X-ray, other imaging-guided percutaneous biopsy
and fiberoptic bronchoscopic biopsy are the main investigative
tools for a pathological diagnosis of chest lesions (2). However, there are certain disadvantages
to these investigations. A CT-guided percutaneous biopsy exposes
the patient to a considerable amount of radiation without being
able to dynamically display the puncture process in real time
(3), resulting in possible
complications. Similarly, fiberoptic bronchoscopy is associated
with difficulty in accessing lumps on the pleura, chest wall and
lung-adjacent peripheral pleura (4).
US-guided percutaneous biopsy of thoracic lesions, especially those
close to the chest wall has gradually become one of the
preferential diagnostic methods for chest lesions due to its
advantages of simplicity, being radiation free, providing real-time
dynamic monitoring throughout the entire puncture process as well
as the possibility of lesser complications (5,6).
Despite the high accuracy of conventional US-guided
percutaneous biopsy, there are certain limitations with regard to
the preoperative evaluation and design of the puncture path in
two-dimensional (2D) US and color doppler flow imaging (CDFI); this
poses challenges for the identification of non-perfused areas, such
as intralesional necrotic, unliquified tissues, occult tumors in
atelectatic lung tissue or a poorly defined boundary between the
tumor and the atelectatic lesions in central lung cancer with
atelectasis (7,8). These challenges impact the initial
diagnosis of the lesion as well as the design of the biopsy path,
conferring some difficulties to the procedure and resulting in poor
diagnostic yield of the biopsy specimen (5).
Contrast-enhanced ultrasound (CEUS; acoustic
contrast) involves the use of injectable contrast agents to enhance
backscatter echo, thereby significantly intensifying the
resolution, sensitivity and specificity of US diagnosis and
reflecting the blood perfusion of healthy and diseased tissues
(7). The sensitivity of blood flow
imaging is significantly higher and unaffected by the noise of the
heartbeat in CEUS compared with color doppler US (9,10). In
addition, CEUS can effectively identify both necrotic and viable
tissues within the lesion, as well as provide valuable information
for the accurate design and execution of the preoperative puncture
biopsy (11). However, there is no
established gold standard diagnostic method for the evaluation of
thoracic lesions. Therefore, the present study was conducted to
evaluate the comparative clinical application value of CEUS against
that of conventional US in thoracic lesions with an aim to identify
a novel standard technique for clinical US-guided percutaneous
core-needle biopsy (CNB).
Materials and methods
Patients
This prospective, non-randomized controlled study
included patients who were diagnosed with chest-occupying lesions
between July 14, 2016 and January 31, 2018 at the Affiliated Tumor
Hospital of Guangxi Medical University (Nanning, Guangxi). The
inclusion criteria of the patients were as follows: i) With a
lesion in the chest detected on CT examination that was clearly
visualizable with US; ii) with complete clinical data; iii) who
underwent an US-guided percutaneous biopsy; iv) with biopsy results
or results of surgical or other pathological biopsy contributing to
the final diagnosis; and v) with records of short-term
complications (including hemoptysis, bleeding, pneumothorax and
chest pain) after CNB and after follow up for 4–8 h
postoperatively. Exclusion criteria were as follows: i) Patients
with poor cooperation and unable to perform image-guided biopsies;
ii) patients with contraindications for the use of CEUS, such as
impaired cardiopulmonary function or known allergic reactions; and
iii) patients with a bleeding tendency (prothrombin activity,
<40%; international standardized ratio, >1.7; platelets,
<40,000/ml). Following screening, a total of 120 patients with
first-stage thoracic lesions were included in the present study and
assigned to the US group (n=66) and CEUS group (n=54) based on
their expressed preference. The present study was approved by the
Ethics Committee of the Affiliated Tumor Hospital of Guangxi
Medical University (Nanning, Guangxi; approval no. LW2018055) and
was conducted in accordance with the principles of the Declaration
of Helsinki and its amendments. All the patients provided written
informed consent prior to being enrolled in the study.
Radiological investigations
All patients underwent a chest CT examination to
indicate the location of the lesion prior to their initial US-CNB.
For the US examination, patients were placed in the supine,
lateral, or prone position with the chest surface region of the
probable lesion fully exposed. Following this the thoracic region
was scanned from different angles to ensure the probe was placed as
close to the chest wall as possible. Gaseous and rib obstructions
were avoided and the size, shape and internal structure of the
lesion was carefully observed and recorded. The presence of
liquefaction necrosis and the positional relationship with the
surrounding lung tissue were also observed and recorded using US.
The vascular supply of the lesion was observed using CDFI. All US
images were recorded in the color Doppler Aplio500/Aplio400
(Toshiba Corp.).
In the CEUS group, a color Doppler Aplio500/Aplio400
(Toshiba Corp.) with a frequency of 3.5 MHz and a mechanical index
of 0.12–0.18 was used with sulfur hexafluoride microbubbles
(SonoVue®; Bracco) as the contrast agent. For each set
of images, a 2.4-ml bolus (injected in 3–5 sec) of contrast agent
suspension was injected (prepared by dissolving 24.98 mg dry powder
in 5 ml normal saline) through a peripheral venous catheter
inserted into an antecubital vein followed by a 5 ml saline flush.
A stopwatch was started with the contrast injection and dynamic
images were recorded. These lesions were examined continuously for
at least 180 sec and included part of the normal peripheral
parenchyma in the same ultrasound scan in order to examine the
enhancement of the lesion and the surrounding normal lung in real
time. If normal lung parenchyma could not be included in the same
imaging scan, or the lesion was located at the basis of the lung,
the surrounding chest wall or the liver (lesion in right lung) or
spleen (lesion in left lung) was examined contemporaneously to the
lesion (12). In the case of
unsatisfactory vascular imaging, the contrast injection was
repeated (inter-injection interval >10 min). Following US, 2
experienced sonographers from the Affiliated Tumor Hospital of
Guangxi Medical University played back the video of the CEUS and
recorded the enhancement level, enhancement pattern and vascular
shape of the lesions. Differences, if any, in the evaluation of the
US images were resolved by mutual discussion to arrive at a
consensus.
Fine needle biopsy
Preoperatively, a routine examination of blood and
coagulation function was performed. For the biopsy, patients were
positioned appropriately on the basis of the location of the
lesion. In the US group, the areas with rich blood supply or
hypoechogenicity were selected as the biopsy site (echo-free areas
were avoided). In the CEUS group, the enhanced areas were selected
(unenhanced areas were avoided) and following determination of the
location of the lesion, the most appropriate needle path and
puncture depth were planned.
The CNB procedure was undertaken as follows: Routine
disinfection with Maokang complex iodine skin disinfectant,
draping, local anesthesia with 2% lidocaine, use of a specific
probe for the puncture, reconfirmation of the puncture site, path,
and depth and insertion of the biopsy needle (Bard®
Magnum®; C.R. Bard; BD Biosciences) through the skin
into the deep layers of the chest wall. The patient was asked to
hold his/her breath, the needle was quickly inserted into the
lesion under US guidance and the biopsy gun was triggered
immediately. The puncture needle was pulled out quickly after
cutting the tissue and then the biopsy was completed. In general,
biopsies were obtained using 2–4 core needles, although an
additional 1–2 needles were used if necessary. In case of
unsatisfactory CNBs with inadequate tissue samples, additional
punctures with repositioning of needle direction were performed.
The tissue sampling was considered successful if the biopsy
specimen met the requirements for histopathological diagnosis. The
tissue specimens were fixed using 10% formalin at room temperature
and were sent to the pathology department for a routine
histological examination 30 min following fixing. Following the
removal of the needle, the puncture point was covered with a
sterile gauze bandage and pressure was applied. Patients were
advised bed rest for 4–8 h after the biopsy, their vital signs were
monitored, and complications were noted (such as bleeding,
hemoptysis, chest tightness, chest pain, pneumothorax and air
embolisms).
Final diagnosis
A comprehensive diagnosis of all biopsy specimens
was done by 2 experienced pathologists from The Affiliated Tumor
Hospital of Guangxi Medical University (Nanning, China), and if the
diagnosis of the biopsy specimen was true in the subsequent
analysis, the diagnosis was considered to be true. Malignant tumors
were identified using surgical specimens or subsequent re-biopsies
obtained from other means, such as biopsy under fiberoptic
bronchoscope. The benign diagnosis was considered to be true
positive if the imaging examination confirmed that the lesion
disappeared or shrank following treatment during the 6 month
follow-up period. A false negative diagnosis was given using the
following criteria: i) The diagnosis of the biopsy specimen was
considered to be negative for a malignant tumor and subsequently
confirmed by surgery or re-biopsy as a malignant tumor; ii) the
biopsy specimen was insufficient; ii) or there was no clear
descriptive diagnosis, such as chronic inflammation, necrosis,
muscle tissue, etc. The diagnostic accuracy of the biopsy was
defined as the percentage of lesions with true positive results in
the initial biopsy (13).
Statistical analysis
Data were subjected to statistical analysis using
SPSS version 19.0 J (IBM Corp.). The Shapiro-Wilk method was used
to determine if data was normally distributed or not. Unpaired data
with skewed distribution were analyzed using the Mann-Whitney U
test and the results were expressed as the median (quartile). The
Wilcoxon signed-rank test was used for comparison of paired
continuous data with skewed distribution. Data were expressed as a
rate (%) on analysis with the Pearson's χ2 test, used
for categorical data. P<0.05 was considered to indicate a
statistically significant difference.
Results
Demographic information of
patients
A total of 120 patients were included in the final
analysis of the present study. Of these, 66 cases were assigned to
the US group (males, 46; females, 20; mean age ± SD, 52.9±15.6; and
age range, 17–74 years) and 54 cases to the CEUS group (male, 40;
female, 14; mean age ± SD, 54.6±13.9; age range, 15–81 years).
Subjects were assigned to each study arm on the basis of their
individual preference to undergo either conventional US or
CEUS.
Histopathological diagnosis of CEUS
and US groups
Details of the histopathological diagnosis of both
groups are presented in Table I. In
the CEUS group (n=54), 35 malignant lesions were identified (lung
squamous cell carcinoma, 9; lung adenocarcinoma, 15; adenosquamous
carcinoma, 1; small cell lung carcinoma, 3; lung large cell
carcinoma, 1; lymphoma, 2; malignant mesothelioma, 1; and
metastatic carcinoma, 3) and 19 benign lesions (inflammatory
pseudotumor, 6; pneumonia, 6; schwannoma, 1; and tuberculosis, 6)
(Table I).
 | Table I.Final diagnosis of CEUS group (n=54)
and US group (n=66) after biopsy. |
Table I.
Final diagnosis of CEUS group (n=54)
and US group (n=66) after biopsy.
| Characteristics of
lesions | CEUS group, n | US group, n |
|---|
| Malignant | 35 | 42 |
| Lung
squamous carcinoma | 9 | 10 |
| Lung
adenocarcinoma | 15 | 16 |
|
Adenosquamous carcinoma | 1 | 2 |
| Small
cell carcinoma | 3 | 3 |
| Large
cell carcinoma | 1 | 0 |
|
Lymphoma | 2 | 5 |
| Malignant
mesothelioma | 1 | 0 |
|
Neuroendocrine carcinoma | 0 | 1 |
|
Metastatic carcinoma | 3 | 5 |
| Benign | 19 | 24 |
|
Inflammatory pseudotumor | 6 | 7 |
| Pneumonia
with consolidation | 6 | 8 |
| Solitary
fibrous tumor | 0 | 2 |
|
Schwannoma | 1 | 0 |
|
Tuberculosis | 6 | 7 |
| Total | 54 | 66 |
In the US group, 42 malignant lesions were detected
(lung squamous cell carcinoma, 10; lung adenocarcinoma, 16;
adenosquamous carcinoma, 2; small cell carcinoma, 3; lymphoma, 5;
neuroendocrine carcinoma, 1; and metastatic carcinoma, 5) and 24
benign lesions (inflammatory pseudotumor, 7; pneumonia, 8; solitary
fibrous tumor, 2; and tuberculosis, 7) (Table I).
Comparison of imaging features in the
CEUS and US groups
Shapiro-Wilk test demonstrated that the size of the
lesion and the number of punctures were all skewed (P>0.05).
There were no significant differences among groups in lesion size
and puncture times (P>0.05; Table
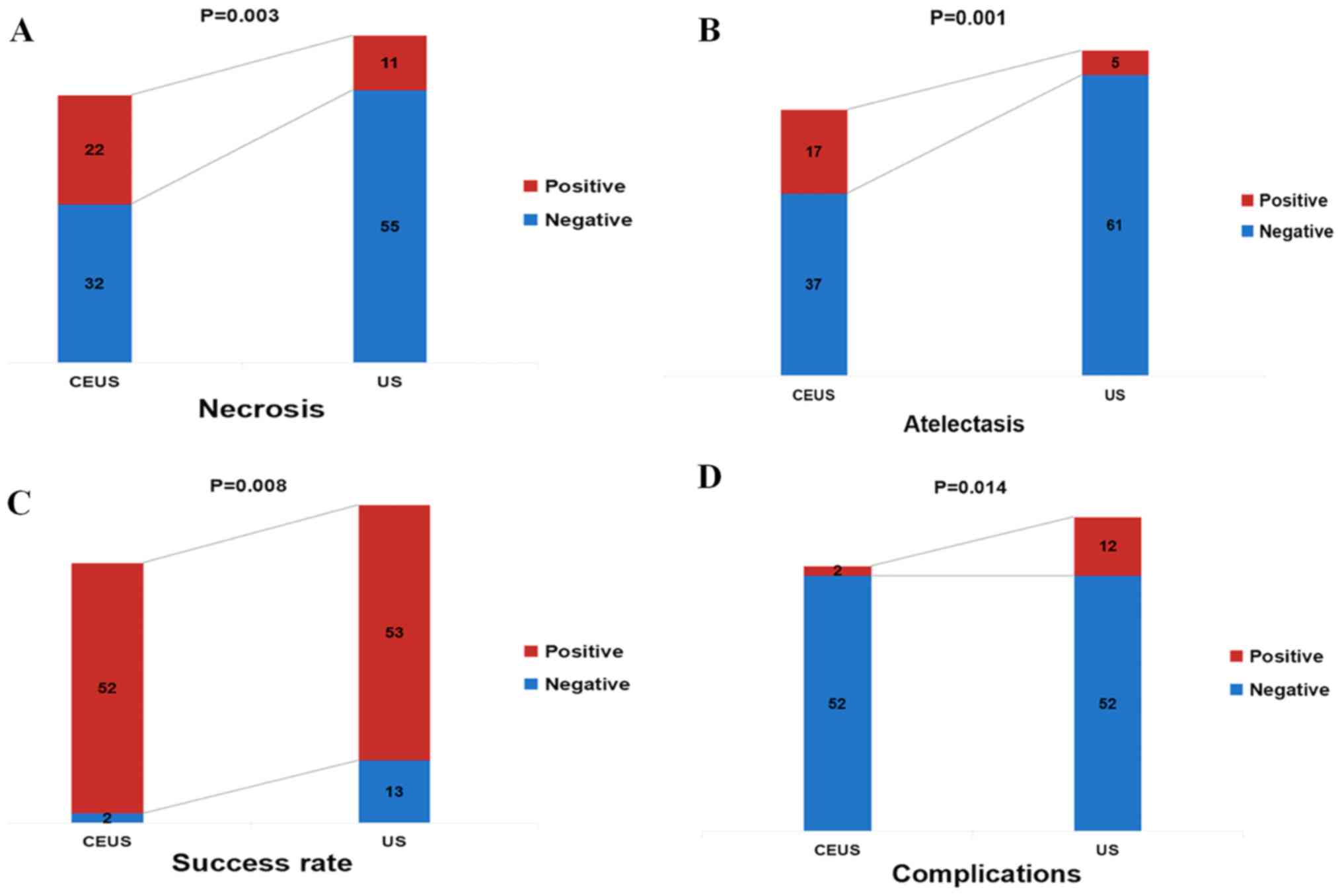
II). The CEUS group had a higher rate of detection of necrotic
tissue compared with the US group (40.7 vs. 16.7%;
χ2=8.633; P=0.003; Table
II; Fig. 1A). In patients with
central lung cancer and atelectasis, the CEUS group exhibited
greater ability to discriminate between the tumor and atelectasis,
compared with the conventional US group (31.5 vs. 7.6%;
χ2=11.336; P=0.001; Table
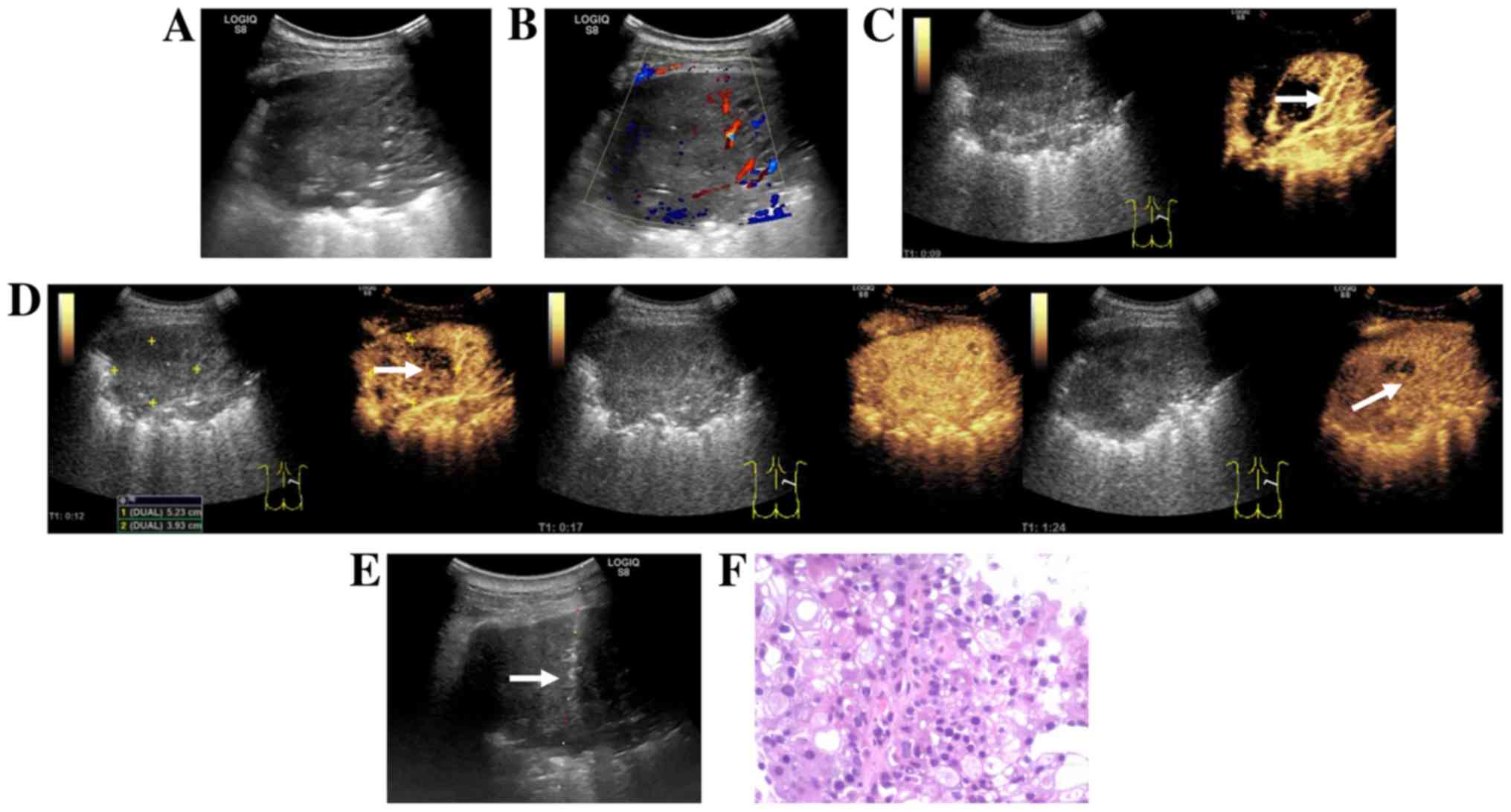
II; Fig. 1B). In addition, in
the CEUS group, the demarcation between the tumor and atelectasis,
as well as the area for puncture biopsy were more clearly defined
compared with the US group (Fig. 2).
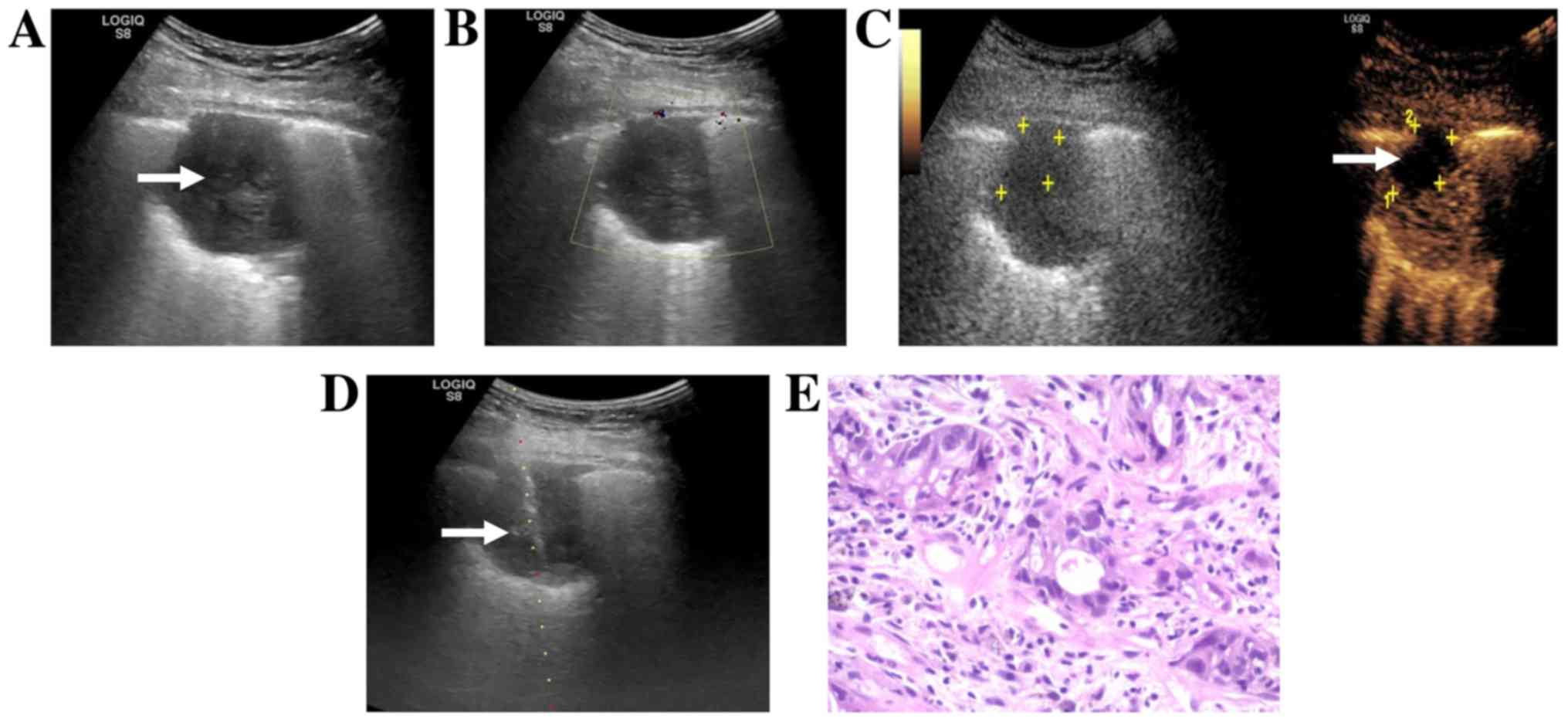
The H&E staining images in Figs.
2 and 3 were obtained by routine
histopathology.
 | Table II.Comparison of imaging features and
biopsy success rate in the CEUS group (n=54) and US group
(n=66). |
Table II.
Comparison of imaging features and
biopsy success rate in the CEUS group (n=54) and US group
(n=66).
| Characteristics | CEUS group | US group | Z
(χ2)-value | P-value |
|---|
| Size, cm | 3.0 (3.0-4.0) | 3.4 (3.0-5.0) | −1.437 | 0.151 |
| Necrosis, %
(n/total) | 40.7 (22/54) | 16.7 (11/66) | 8.633 | 0.003 |
| Atelectasis, %
(n/total) | 31.5 (17/54) | 7.6 (5/66) | 11.336 | 0.001 |
| Punctures times,
n | 3 (3–4) | 3 (3–5) | −1.574 | 0.116 |
| Success rate, %
(n/total) | 96.3 (52/54) | 80.3 (53/66) | 6.946 | 0.008 |
| Complications, %
(n/total) | 3.7 (2/54) | 18.2 (12/66) | 6.041 | 0.014 |
Comparison of biopsy success rate and
complication rate in the CEUS and US groups
In 48.1% (26/54) of the patients in the CEUS group,
the initial puncture path was changed during US-guided
transthoracic biopsy due to the presence of necrotic tissue or
atelectasis tissue in the lesion by CEUS examination, including 17
cases (31.5%) due to necrotic tissue (Fig. 3) and 9 cases (16.6%) due to pulmonary
atelectasis (Table III). The CEUS
group had a higher CNB success rate (96.3 vs. 80.3%;
χ2=6.946; P=0.008; Table
II; Fig. 1C) and a lower
complication rate compared with the US group (3.7 vs. 18.2%;
χ2=6.041; P=0.014; Table
II; Fig. 1D). In the CEUS group,
there was 1 case of hemorrhage and 1 case of chest pain whereas the
US group there were 5 cases of hemoptysis, 2 cases of chest pain, 4
cases of pneumothorax and 1 case of hemorrhage (Table II). All the complications observed
in the present study were reported in previous studies of
conventional ultrasound-guided biopsy (3,8,14) and resolved with conservative
management including hemostasis, oxygen inhalation and bed rest.
There were no reports of serious complications, such as severe
hemopneumothorax requiring closed thoracic drainage.
 | Table III.Initial puncture path was changed
during US-guided transthoracic biopsy after CEUS examination in
CEUS group. |
Table III.
Initial puncture path was changed
during US-guided transthoracic biopsy after CEUS examination in
CEUS group.
|
Characteristics | CEUS group (the
initial puncture path was changed), % (n) |
|---|
| Necrosis | 31.5 (17/54) |
| Atelectasis | 16.6 (9/54) |
| Total | 48.1 (26/54) |
Post hoc analysis of puncture failure
in the CEUS and US groups
A post hoc analysis was performed to evaluate the
cause of puncture failure in the 2 patients in the CEUS group, and
insufficient tissue specimen and poor patient cooperation were
identified as the causes (Table
III). A similar analysis of 13 patients with puncture failure
in the US group revealed that 7 cases had necrotic tissue in biopsy
specimens, 3 had healthy lung and muscle tissues, 2 developed
intraprocedural complications during puncture and 1 had poor
patient cooperation (Table IV).
 | Table IV.Post hoc analysis of the failure of
the puncture in the US and CEUS groups. |
Table IV.
Post hoc analysis of the failure of
the puncture in the US and CEUS groups.
| Cause | CEUS group | US group |
|---|
| Necrotic
tissue | 0 | 7 |
| Lung tissue and
skeletal muscle tissue | 0 | 3 |
| Insufficient
organization | 1 | 0 |
| Complications | 0 | 2 |
| Poor patient
cooperation | 1 | 1 |
| Total | 2 | 13 |
Discussion
In recent years, US-guided percutaneous biopsy has
emerged as one of the main investigative techniques to obtain
histopathological specimens from chest lesions (7). Increasingly, it is becoming the
first-choice investigation in chest lesions because of its
advantages of procedural simplicity, safety and effectiveness,
without the risk of exposure to ionizing radiation (5,6) Despite
its high success rate and fewer complications, conventional US has
certain limitations in the preoperative evaluation of chest lesions
and the design of the puncture path (7). For example, although conventional 2D US
can recognize liquefaction within lesions, it may only poorly
identify necrotic and un-liquified tissues (7). In addition, although CDFI can broadly
observe lesion vascularity, it has low sensitivity and the results
of the observation are easily influenced by numerous factors,
including the angle between the sound wave and the blood vessel,
false negative readings by slow blood flow and noise interference
due to the heartbeat (14).
Conventional US cannot easily distinguish between occult tumors and
atelectatic lung tissue (8,14). These aforementioned factors may
decrease the accuracy of the biopsy results (7,15). A
rebiopsy can improve the diagnostic accuracy, but with an increase
in costs, time to treatment, risk of complications and patient
anxiety, amongst other factors.
CEUS is a vascular imaging method that can
effectively display real-time blood perfusion in healthy and
diseased tissues and provide more diagnostic information compared
with conventional US for a pre-biopsy assessment (4). Sartori et al (11) reported the first case of peripheral
lung tumor with large necrotic tissue successfully guided by CEUS
in 2004. Previous studies have demonstrated that CEUS can
positively identify necrotic areas in lung lesions, despite a lack
of consensus on the ability of CEUS to differentiate between benign
and malignant thoracic lesions (4,16). The
results of the present study demonstrated that the CEUS group had a
higher rate of detection of necrotic tissue (40.7 vs. 16.7%)
compared with the US group. In central lung cancer with
atelectasis, the ability to distinguish between tumor and
atelectasis was higher in the CEUS group compared with that in the
conventional US group (31.5 vs. 7.6%). In addition, in 48.1% of the
patients in the CEUS group, the initial puncture path was changed
during US-guided transthoracic biopsy due to the presence of
necrotic tissue or atelectasis tissue in the tumor by CEUS
examination; the CEUS group had a higher puncture success (96.3 vs.
80.3%) and a lower complication rate (3.7 vs. 18.2%) compared with
those in the US group. The present results are similar to those
reported in previous studies (7,8,11), suggesting that CEUS may identify the
necrotic areas in the lesions, as well as the tumors hidden in the
atelectasis. The inference of a rationale for this is based on a
literature review (17).
Microvessels are present in viable tissues of the lesion, but
absent in necrotic areas. Therefore, regardless of whether CEUS or
super micro-imaging is undertaken in the contrast mode, the
contrast agent will enter viable tissue, but not the necrotic
tissue (4). Therefore, contrast
imaging can effectively distinguish between viable tissue and
necrotic areas within lesions (11).
The vascular supply to malignant tumors of the chest primarily
originates from the bronchial artery, whereas the peritumoral lung
tissue receives dual vasculature from both the pulmonary and
bronchial arteries (4). The injected
contrast agent initially enters the pulmonary artery prior to
entering the bronchial artery; therefore, the viable lung tissue
enhances before the diseased tissue and this is an important basis
to distinguish lung atelectasis from tumor tissue (7). In addition, the findings of the present
study demonstrated earlier initial enhancement of lung tissue
compared with diseased tissue which corresponds to the
histopathological basis of the lesion. The heterogeneity of tumoral
tissue with the associated unevenness of vascularity results in
heterogeneous enhancement, which is an important basis for
distinguishing between tumor tissue and atelectatic lung tissue
(16). In addition, atelectatic
pulmonary tissue has a regular and branched vasculature, whereas
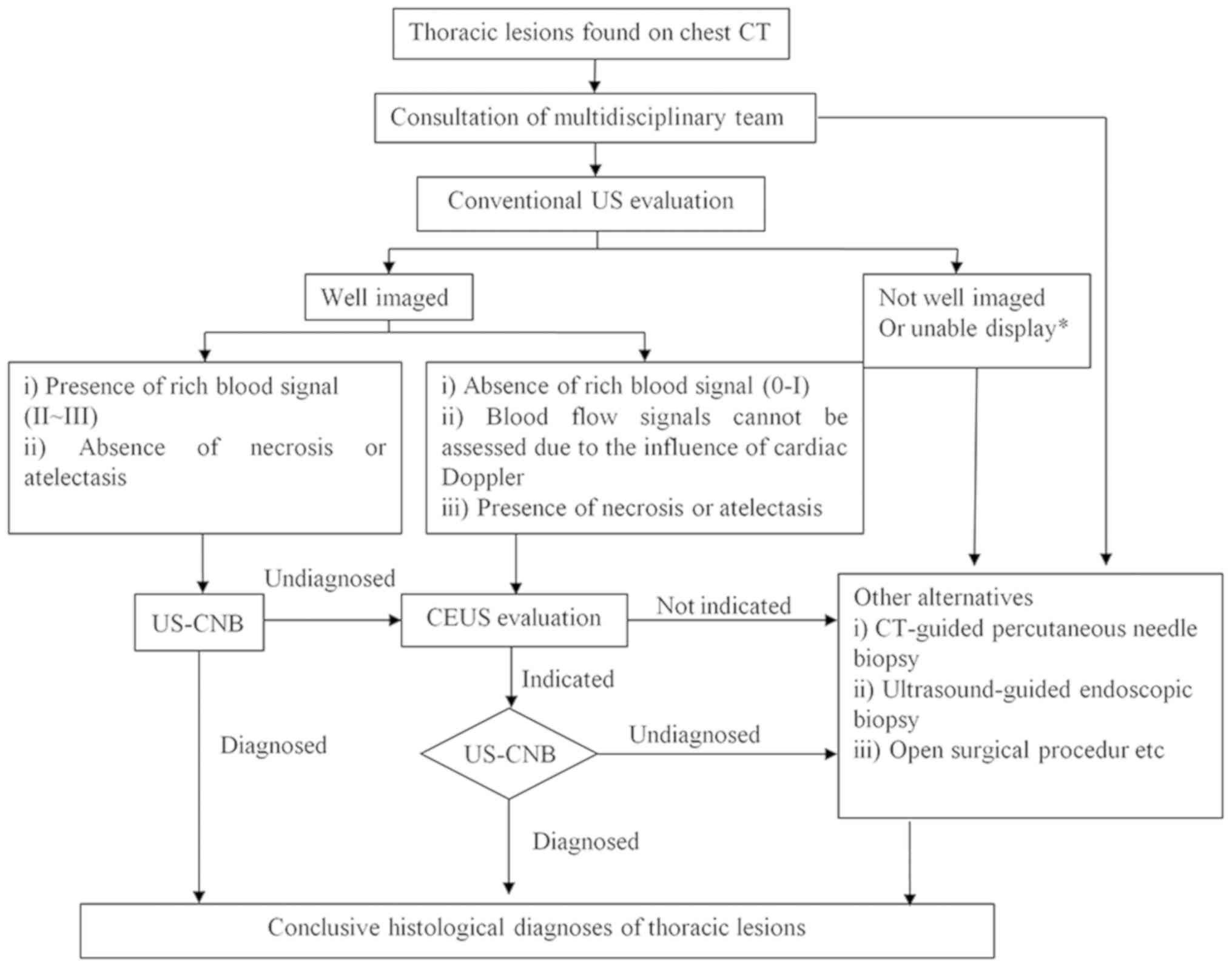
tumor vasculature is distorted and irregular (8). Therefore, CEUS prior to a CNB can
effectively increase the success rate of puncture and minimize the
probability of a repuncture. However, to avoid overdiagnosis and
the associated treatment, CEUS should not be routinely recommended
to all patients. A pre-puncture CEUS is recommended for patients
with chest lesions, with hypovascular lesions (0-I blood flow, on
Adler grading (18) or
indeterminable blood supply (due to cardiac Doppler effects, for
example) in the presence of atelectasis or necrosis who are
scheduled to undergo a repeat US-CNB. This recommendation is
explained in Fig. 4.
The present study has several limitations. Firstly,
the small sample size is insufficient to generate adequate
statistical power to validate the current findings. Secondly, the
study groups were not randomized. Thirdly, potential confounders,
such as the body mass index of patients and poor cooperation were
not accounted for, which likely have an impact on the results of
the study. The findings of the present study need to be validated
in well-designed, randomized, large cohort, multi-center
prospective studies.
In conclusion, the present study demonstrated that
CEUS can identify necrotic areas and occult tumors within
atelectatic lung tissue and can be used for guiding puncture biopsy
of thoracic lesions to improve diagnostic accuracy with greater
clinical utility compared with conventional US. Pre-biopsy CEUS is
particularly useful for patients undergoing repeated US-CNB and
those with hypovascular lesions, atelectasis or necrosis.
Acknowledgements
Not applicable.
Funding
The present study was supported by grants from the
Youth Science Foundation of Guangxi Medical University (grant no.
GXMUYSF201725), Competence Improvement Project of Young and
Middle-aged Teachers in Colleges and Universities in Guangxi (grant
no. 2018KY0118) and National Natural Science Foundation of China
(grant no. 81701721).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
LL and JJL designed the study and revised the
manuscript. DW and ZD participated in designing and conducting the
research. JCL conceived the research and contributed to the writing
of the manuscript. HXL and SZ collected and analyzed the data. MC
and HL analyzed the data and interpreted the results. All authors
have read and approved the manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Affiliated Tumor Hospital of Guangxi Medical
University (Nanning, Guangxi; approval no. LW2018055). All the
patients provided written informed consent prior to being enrolled
in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Pilleron S, Sarfati D, Janssen-Heijnen M,
Vignat J, Ferlay J, Bray F and Soerjomataram I: Global cancer
incidence in older adults, 2012 and 2035: A population-based study.
Int J Cancer. 144:49–58. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Anna ML, David B and Lauren T: Diagnosing
lung cancer: The complexities of obtaining a tissue diagnosis in
the era of minimally invasive and personalised medicine. J Clin
Med. 7:1632018. View Article : Google Scholar
|
|
3
|
Yamamoto N, Watanabe T, Yamada K, Nakai T,
Suzumura T, Sakagami K, Yoshimoto N, Sato K, Tanaka H, Mitsuoka S,
et al: Efficacy and safety of ultrasound (US) guided percutaneous
needle biopsy for peripheral lung or pleural lesion: Comparison
with computed tomography (CT) guided needle biopsy. J Thorac Dis.
11:936–943. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Piscaglia F, Nolsøe C, Dietrich CF,
Cosgrove DO, Gilja OH, Nielsen MB, Albrecht T, Barozzi L,
Bertolotto M, Catalano O, et al: The EFSUMB guidelines and
recommendations on the clinical practice of contrast enhanced
ultrasound (CEUS): Update 2011 on non-hepatic applications.
Ultraschall Med. 33:33–59. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Choi YR, An JY, Kim MK, Han HS, Lee KH,
Kim SW, Lee KM and Choe KH: The diagnostic efficacy and safety of
endobronchial ultrasound-guided transbronchial needle aspiration as
an initial diagnostic tool. Korean J Intern Med. 28:660–667. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jarmakani M, Duguay S, Rust K, Conner K
and Wagner JM: Ultrasound versus computed tomographic guidance for
percutaneous biopsy of chest lesions. J Ultrasound Med.
35:1865–1872. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Song W, Wei Y, Hui Z, Qian X and Yan K:
The role of contrast-enhanced ultrasound in selection indication
and improveing diagnosis for transthoracic biopsy in peripheral
pulmonary and mediastinal lesions. Biomed Res Int.
2015:2317822015.PubMed/NCBI
|
|
8
|
Lei Z, Lou J, Bao L and Lv Z:
Contrast-enhanced ultrasound for needle biopsy of central lung
cancer with atelectasis. J Med Ultrason. 45:461–467. 2018.
View Article : Google Scholar
|
|
9
|
Ramnefjell M, Aamelfot C, Aziz S,
Helgeland L and Akslen LA: Microvascular proliferation is
associated with aggressive tumour features and reduced survival in
lung adenocarcinoma. J Pathol Clin Res. 3:249–257. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lu R, Meng Y, Zhang Y, Zhao W, Wang X, Jin
M and Guo R: Superb microvascular imaging (SMI) compared with
conventional ultrasound for evaluating thyroid nodules. BMC Med
Imaging. 17:652017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sartori S, Nielsen I, Trevisani L, Tombesi
P, Ceccotti P and Abbasciano V: Contrast-enhanced sonography as
guidance for transthoracic biopsy of a peripheral lung lesion with
large necrotic areas. J Ultrasound Med. 23:133–136. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yi D, Feng M, Wang WP, Ji ZB and Fan PL:
Value of contrast-enhanced ultrasound in guidance of percutaneous
biopsy in peripheral pulmonary lesions. Biomed Res Int.
2015:5315072015.PubMed/NCBI
|
|
13
|
Yi D, Feng M, Wen PW, Zheng BJ and Fan PL:
Contrast-enhanced US-guided percutaneous biopsy of anterior
mediastinal lesions. Diagn Interv Radiol. 23:43–48. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Guo YQ, Liao XH, Li ZX, Chen YY, Wang SD,
Wang JH, Liao X and Luo Y: Ultrasound-guided percutaneous needle
biopsy for peripheral pulmonary lesions: Diagnostic accuracy and
influencing factors. Ultrasound Med Biol. 44:1003–1011. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jeon KN, Bae K, Park MJ, Choi HC, Shin HS,
Shin S, Kim HC and Ha CY: US-guided transthoracic biopsy of
peripheral lung lesions: Pleural contact length influences
diagnostic yield. Acta Radiol. 55:295–301. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Görg C, Bert T and Görg K:
Contrast-enhanced sonography for differential diagnosis of pleurisy
and focal pleural lesions of unknown cause. Chest. 128:3894–3899.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Görg C, Bert T and Kring R:
Contrast-enhanced sonography of the lung for differential diagnosis
of atelectasis. J Ultrasound Med. 25:35–39. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Adler DD, Carson PL, Rubin JM and
Quinn-Reid D: Doppler ultrasound color flow imaging in the study of
breast cancer: Preliminary findings. Ultrasound Med Biol.
16:553–559. 1990. View Article : Google Scholar : PubMed/NCBI
|