Introduction
According to statistics, the incidence rate of
ovarian cancer in 2018 was 3.4%, worldwide (1). Ovarian cancer is the eighth most common
cancer in female and the second most common cause of
cancer-associated mortality among gynecological malignancies
worldwide (1). A combination of
antimitotic agents, such as taxanes, and DNA-damaging agents, such
as platinum compounds remains the principle treatment for ovarian
cancer (2), whereby 60–85% of
patients with high-grade ovarian cancer initially respond to this
regimen; however, the majority of these patients eventually relapse
due to chemoresistance (3,4). Furthermore, most patients with
high-grade ovarian cancer are resistant to paclitaxel and
associated microtubule inhibitors (3,4). Thus,
development of novel therapeutic strategies for the treatment of
ovarian cancer remains critical.
Several anticancer drugs exert their effects through
the cell cycle. For example, methotrexate, vinca alkaloids and
bleomycin play function by arresting cells in S phase or G2/M
phase. The cell cycle is a complex multi-step process that is
regulated by different mechanisms, including cyclin-dependent
kinase (CDK) pathways, metabolic adaptations and redox-dependent
signaling. CDK complexes play key regulatory roles in cell cycle
progression (5). In CDK-dependent
pathways, the catalytic activities of CDKs are modulated by the
interactions between cyclins and CDK inhibitors (CKIs) (6). In this progression, cyclins and CKIs
serve as brakes to halt cell cycle progression under unfavorable
conditions, such as when DNA damage is present (7). P21, a member of the cyclin-dependent
kinase inhibition protein/kinase inhibition protein family of CKIs,
is activated following DNA damage and metabolic stress, which
arrests cell cycle progression in the G1/S and G2/M phases by
inhibiting Cyclin D/CDK4 and CDK6, and Cyclin E/CDK2 activities,
respectively (8).
In addition to cyclin-CDK complexes, several other
cell cycle-associated targets exist for antitumor therapies. For
example, taxanes and colchicine can also induce cell cycle arrest
by influencing microtubule (MT) stability (9,10). MTs
are hollow cylindrical tubes consisting of 13 aligned
protofilaments, formed from repeating α-tubulin and β-tubulin
heterodimers (11). MTs undergo
polymerization and de-polymerization, while the dynamic balance
between them plays a central role in cell meiosis. Disruption of
this balance caused by factors, such as low temperature and drugs
halts meiosis. Taxanes are MT regulators that block cell meiosis in
G2/M by binding to tubulin, thus promoting MT polymerization and
eventually inducing apoptosis (12).
In addition to directly affecting tubulin, MT regulators can also
influence the expression of MT-associated proteins. For example,
stathmin is a MT de-polymerizing protein that regulates MT dynamics
and spindle assembly through binding to α/β-tubulin heterodimers
(13). The high expression level of
stathmin decreased the sensitivity of ovarian cancer to paclitaxel
(14). However, taxanes and
anti-stathmin therapy produced a synergistic anticancer effect, and
stathmin knockdown, by transfecting the expression construct
containing full-length stathmin cDNA in the antisense orientation,
increased taxanes sensitivity (15).
A previous study has demonstrated that p53 induces cell arrest at
the G2/M checkpoint by downregulating stathmin, while
its expression is activated following DNA damage (16).
Plant-derived flavones, such as morelloflavone and
ginkgo, have also been reported to play an important role in
preventing cancer progression including prostate and lung cancer
cells (17,18). Amentoflavone (AMF) is a biflavonoid
extracted from the Chinese herb Selaginella tamariscina,
which displays several pharmacological properties, including
antitumor, anti-inflammatory and antiviral effects (19–22). A
previous study demonstrated that AMF inhibits angiogenesis of
endothelial cells and induces apoptosis in hypertrophic scar
fibroblasts (23). Although it has
been demonstrated that AMF inhibits the development of different
types of cancer, its underlying molecular mechanisms in ovarian
cancer remain unclear.
Thus, the present study aimed to investigate the
effect of AMF on ovarian cancer progression and the underlying
mechanisms involved in the observed effects. The results
demonstrated that AMF decreased ovarian cancer cell viability and
induced cell cycle arrest, by disrupting the balance of MT dynamics
and increasing the levels of DNA damage. Taken together, the
results of the present study suggest that AMF may act as a
therapeutic agent in the treatment of ovarian cancer.
Materials and methods
Cell culture, cell line and
reagents
The SKOV3 human ovarian cancer cell line was
purchased from the Cell Bank of Type Culture Collection of the
Chinese Academy of Sciences. Cells were maintained in DMEM
supplemented with 10% FBS, 2 mM glutamine (all from Thermo Fisher
Scientific, Inc.), 100 units of penicillin/ml and 100 µg of
streptomycin/ml (both from Corning Life Sciences) at 37°C in a
humidified atmosphere of 5% CO2 and subcultured every
2–3 days. AMF was purchased from Shanghai Winherb Medical Science
Co. Ltd., with a purity of 99%. A total of 100 mmol/l stock
solution of AMF was prepared in dimethyl sulfoxide (Sigma-Aldrich;
Merck KGaA) and stored at −20°C until further experimentation.
Cell viability assay
SKOV3 cells were seeded in 96-well plates at a
density of 5,000 cells/well (100 µl). After 24 h, cells were
treated with different concentrations of AMF (0, 50, 75, 100, 150
and 200 µmol/l) for 48 h at 37°C. Cell viability was determined via
the CellTiter 96 Aqueous One Solution Proliferation assay (Promega
Corporation) at a wavelength of 490 nm, using a multi-well
spectrophotometer (Agilent Technologies, Inc.). All experiments
were performed in triplicate.
Flow cytometric analysis
A total of 1×105 SKOV3 cells/well were
seeded in 6-well overnight and treated with different
concentrations of AMF (0, 100 and 150 µmol/l) for 48 h at 37°C.
Cells were fixed in 70% ethanol overnight at 4°C, permeabilized
with 0.1% Triton X-100 (Sigma-Aldrich; Merck KGaA), digested with
RNaseA (Thermo Fisher Scientific, Inc.) and subsequently stained
with propidium iodide (BD Biosciences) in the dark for 30 min at
37°C, prior to cell cycle analysis using a FACS Calibur flow
cytometer (BD Biosciences) and analyzed using ModFit LT Windows 3.2
(Verity Software House, Inc.).
Immunofluorescence
A total of 1×104 SKOV3 cells/well were
seeded onto coverslips in a six-well plate. Following incubation
for 24 h at 37°C, cells were treated with different concentrations
of AMF (0, 100 and 150 µmol/l) for 48 h at 37°C. Subsequently,
cells were fixed with 4% paraformaldehyde for 15 min at room
temperature, permeabilized with 0.25% Triton X-100 for 10 min and
blocked with 1% BSA for 30 min at room temperature. Cells were
incubated with primary antibodies against phospho-Histone H2AX
(γ-H2AX; 1:200 v/v; cat. no. 9718), α-tubulin (1:200 v/v; cat. no.
2144) or β-tubulin (1:200 v/v; cat. no. 2146), all from Cell
Signaling Technology Inc., overnight at 4°C. Subsequently, cells
were incubated with Alexa Fluor 488-labeled goat anti-rabbit
secondary antibody (1:500 v/v; cat. no. 4416; Cell Signaling
Technology, Inc.) for 1 h at room temperature. Nuclei were stained
with 0.1 µg/ml DAPI (Santa Cruz Biotechnology Inc.) for 5 min at
room temperature. Cell images were observed under a Nikon Eclipse
E600 fluorescence microscope (magnification, ×400; Nikon
Corporation) and analyzed using NIS-Elements D 4.50 software (Nikon
Corporation).
Western blotting
A total of 1×105 SKOV3 cells/well were
seeded into 100-mm cell culture dishes and treated with different
concentrations of AMF (0, 100 and 150 µmol/l) for 48 h at 37°C.
Total protein was extracted using RIPA lysis buffer (150 mM NaCl,
50 mM Tris with pH 7.4, 1% NP40, 0.1% SDS and 0.5% sodium
deoxycholate; Beyotime Institute of Biotechnology) supplemented
with 10 mM phenylmethanesulphonyl fluoride (Amresco, Inc.) and 10X
phosphatase inhibitor (Roche Applied Science). Total protein
concentration was determined using the bicinchoninic acid protein
assay kit (Thermo Fisher Scientific, Inc.), 20 µg protein samples
per lane were loaded and separated via 10% SDS-PAGE and
electroblotted. The separated proteins were subsequently
transferred onto polyvinylidene difluoride membranes (Merck KGaA)
and blocked with 5% (w/v) non-fat milk powder in TBST [10 mM Tris,
pH 7.5, 150 mM NaCl and 0.1% (v/v) Tween 20] for 2 h at room
temperature. Membranes were incubated with primary antibodies
against GAPDH (1:1,000 v/v; cat. no. 2118; Cell Signaling
Technology Inc.), β-tubulin (1:1,000 v/v; cat. no. 2146; Cell
Signaling Technology Inc.), Cyclin-B1 (1:1,000 v/v; cat. no. 12231;
Cell Signaling Technology Inc.), CDK2 (1:1,000 v/v; cat. no.
ab32147; Abcam), p-CDK1 (1:1,000 v/v; cat. no. 4539; Cell Signaling
Technology Inc.), P21 (1:1,000 v/v; cat. no. 2947; Cell Signaling
Technology Inc.), γ-H2AX (1:1,000 v/v; cat. no. 9718; Cell
Signaling Technology Inc.), stathmin (1:1,000 v/v; cat. no.
ab52630; Abcam), Rad51 (1:1,000 v/v; cat. no. ab133534; Abcam) or
CDK1 (1:1,000 v/v; cat. no. ab18; Abcam) overnight at 4°C. The
membranes were washed three times with TBST and subsequently
incubated with horse radish peroxidase-conjugated secondary
antibodies (1:2,000 v/v; cat. no. 7074 or 7076; Cell Signaling
Technology Inc.) diluted in TBST for 1 h at room temperature.
Membranes were re-washed three times with TBST, and protein bands
were visualized using the electrochemiluminescence detection kit
(Pierce; Thermo Fisher Scientific, Inc.) and imaged using the
ChemiDoc XRS+ Imaging System (Bio-Rad Laboratories, Inc.). Image
Lab 3.0 software (Bio-Rad Laboratories, Inc.) was used for
semi-quantitative analysis of band signals.
Statistical analysis
Statistical analysis was performed using SPSS
software v17.0 (IBM Corp.) and data are presented as the mean +
standard deviation (SD) of at least three independent experiments.
One-way analysis of variance and Student-Newman-Keuls post-hoc test
were used to compare difference between multiple groups. Unpaired
Student's t-test was used to test statistical significance between
two groups. P<0.05 was considered to indicate a statistically
significant difference.
Results
AMF inhibits SKOV3 cell viability
The effect of AMF on SKOV3 cell viability was
assessed via the CellTiter 96 Aqueous One Solution Proliferation
assay. Cells were treated with different concentrations of AMF
(50–200 µmol/l) for 48 h. The results demonstrated that AMF
significantly inhibited SKOV3 cell viability in a dose-dependent
manner, from 75 µmol/l onwards compared with the control cells
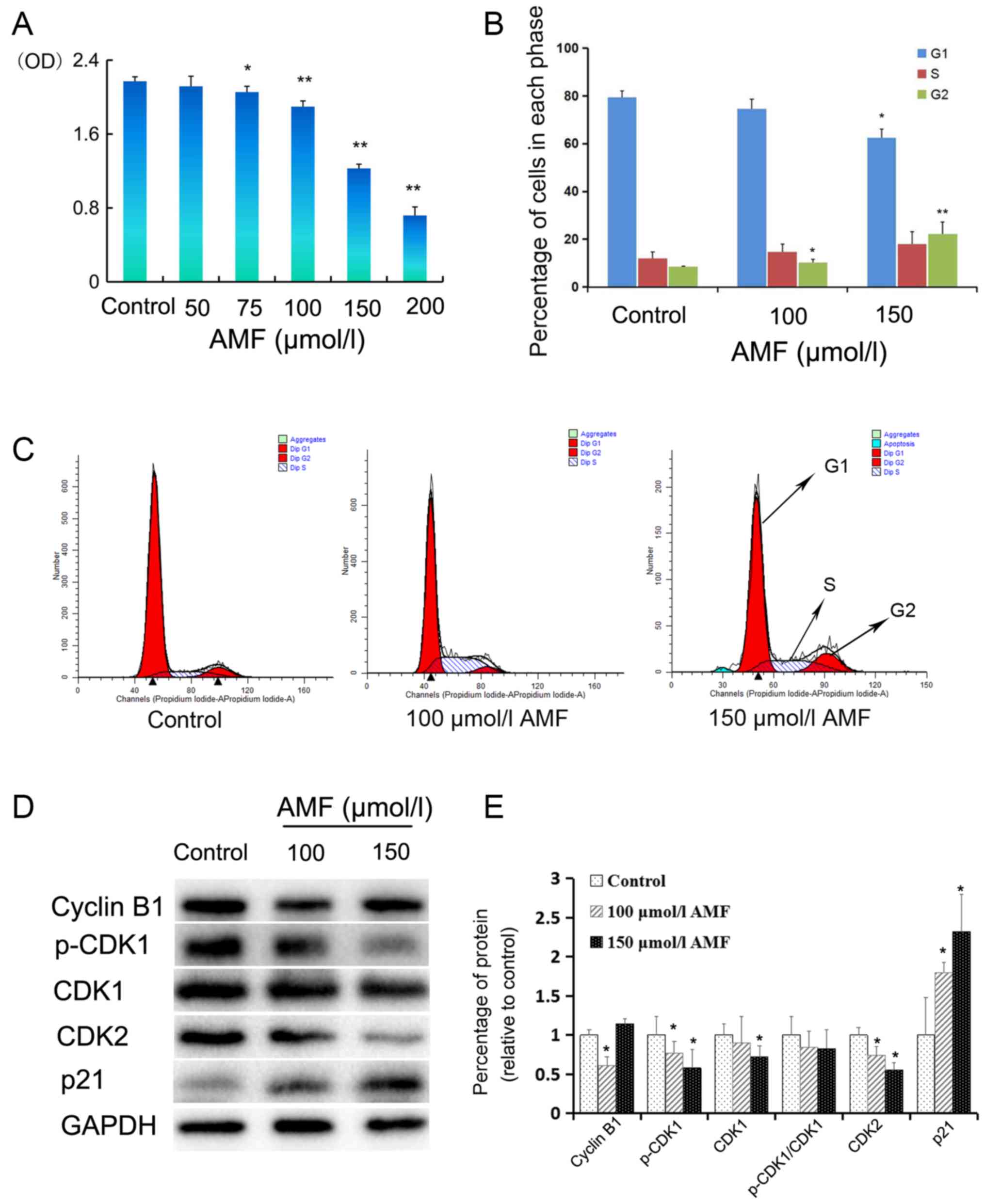
(Fig. 1A).
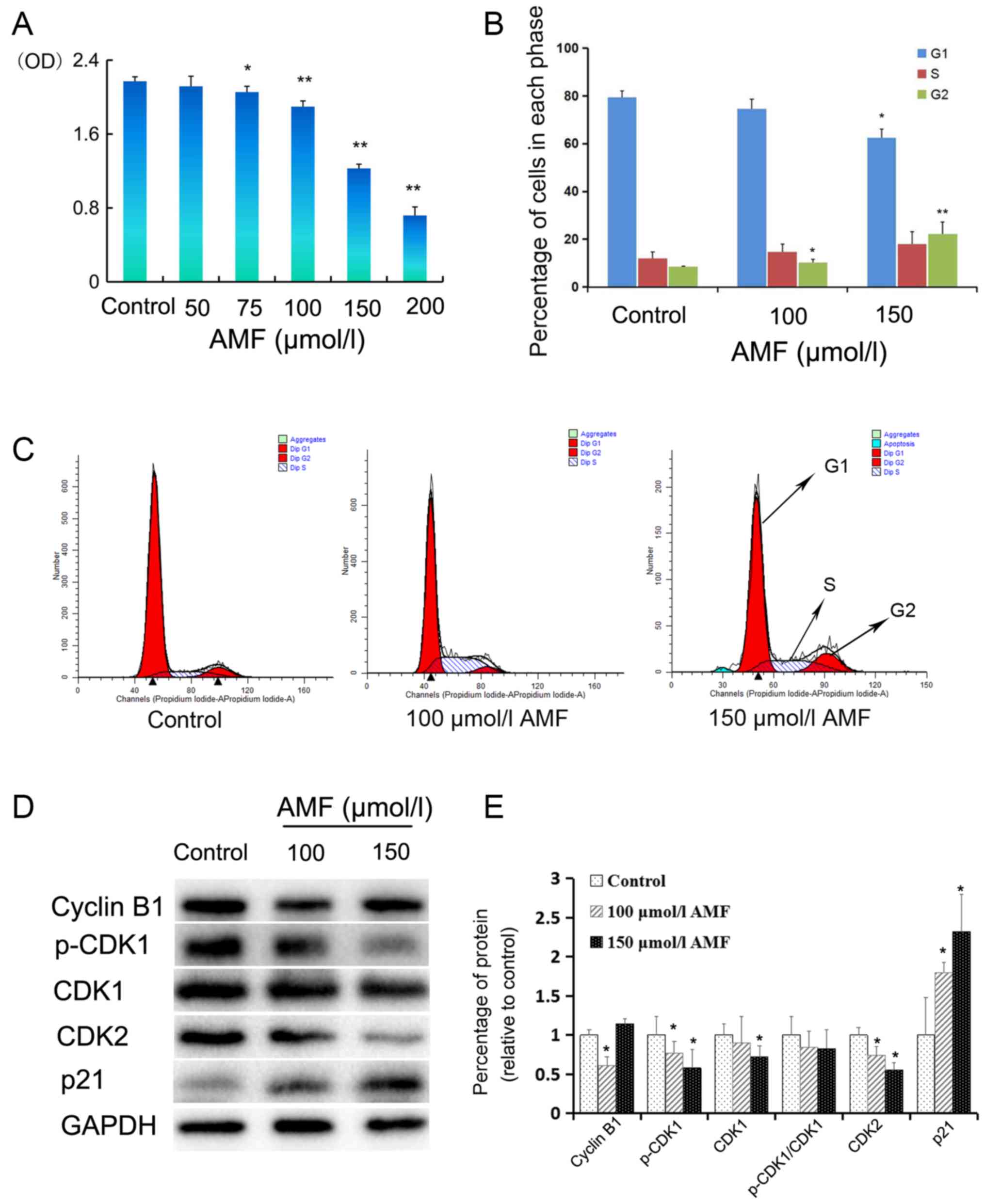 | Figure 1.AMF decreases SKOV3 cell viability
and induces cell cycle arrest. (A) SKOV3 cells were treated with
different concentrations (0, 50 75, 100, 150 and 200 µmol/l) of AMF
for 48 h and cell viability was assessed via the CellTiter 96
Aqueous One Solution Proliferation assay. The results demonstrated
that AMF decreased SKOV3 cell viability in a dose-dependent manner.
(B) Histograms showed the cell cycle distribution at G1, S and G2
phase. Data are presented as the mean ± SD (n=3). SKOV3 cells were
treated with different concentrations of AMF (0, 100 and 150
µmol/l) for 48 h and cell cycle distribution was assessed via flow
cytometric analysis. (C) Cell cycle analysis by flow cytometry.
SKOV3 cells were treated with different concentrations of AMF (0,
100 and 150 µmol/l) for 48 h. (D) The expression levels of cyclin
B, p-CDK1, CDK1, CDK2 and p21 were determined in SKOV3 cells
treated with different concentrations of AMF (0, 100 and 150
µmol/l) for 48 h by western blot. GAPDH was used as the loading
control. (E) Protein expression levels from the western blot in (D)
relative to the GAPDH control. Data are presented as the mean ± SD
(n=3). *P<0.05, **P<0.01 vs. control. AMF, amentoflavone; SD,
standard deviation; CDK, cyclin-dependent kinase. |
AMF induces S phase and G2 cell cycle
arrest of SKOV3 cells
In order to determine the molecular mechanism
underlying the inhibitory effect of AMF on SKOV3 cell viability,
the effect of AMF on the cell cycle was assessed. SKOV3 cells were
treated with 100 or 150 µmol/l AMF for 48 h and flow cytometric
analysis was performed to determine cell cycle distribution. The
results demonstrated that treatment with AMF slightly increased the
percentage of SKOV3 cells in the S or G2 phases, and
decreased the percentage of SKOV3 cells in the G1 phase
(Fig. 1B and C). Comparing with the
percentage of SKOV3 G1 or G2 phase cells in
the control group, the percentage of G1 phase cells in
150 µmol/l AMF group was significantly decreased, while the
percentages of G2 phase cells in 100 and 150 µmol/l AMF
groups were significantly increased. Taken together, these results
suggest that AMF arrests cell cycle at the G2 phase and interferes
with cell meiosis and cell proliferation.
AMF regulates the expression of cell
cycle-associated proteins in SKOV3 cells
In order to further investigate the molecular
mechanisms by which AMF arrests the cell cycle, the effect of AMF
on the expression levels of proteins associated with cell cycle
progression was assessed via western blot analysis. The expression
levels of p-CDK1 and CDK2 decreased in SKOV3 cells treated with 100
or 150 µmol/l AMF for 48 h (Fig. 1D and
E). Furthermore, CDK1 expression decreased in SKOV3 cells
treated with 100 and 150 µmol/l AMF; however, a significant
decrease was only observed in the cells treated with 150 µmol/l of
AMF (Fig. 1D and E). The p-CDK1/CDK1
ratio decreased in cells treated with AMF; however, no significant
differences were observed compared with the control cells (Fig. 1D and E). Notably, cyclin B1
expression was significantly downregulated in SKOV3 cells treated
with 100 µmol/l AMF and upregulated in cells treated with 150
µmol/l AMF. P21, a well-known inhibitor of the cell cycle,
significantly increased in AMF-treated cells compared with
AMF-untreated ovarian cells (Fig.
1E).
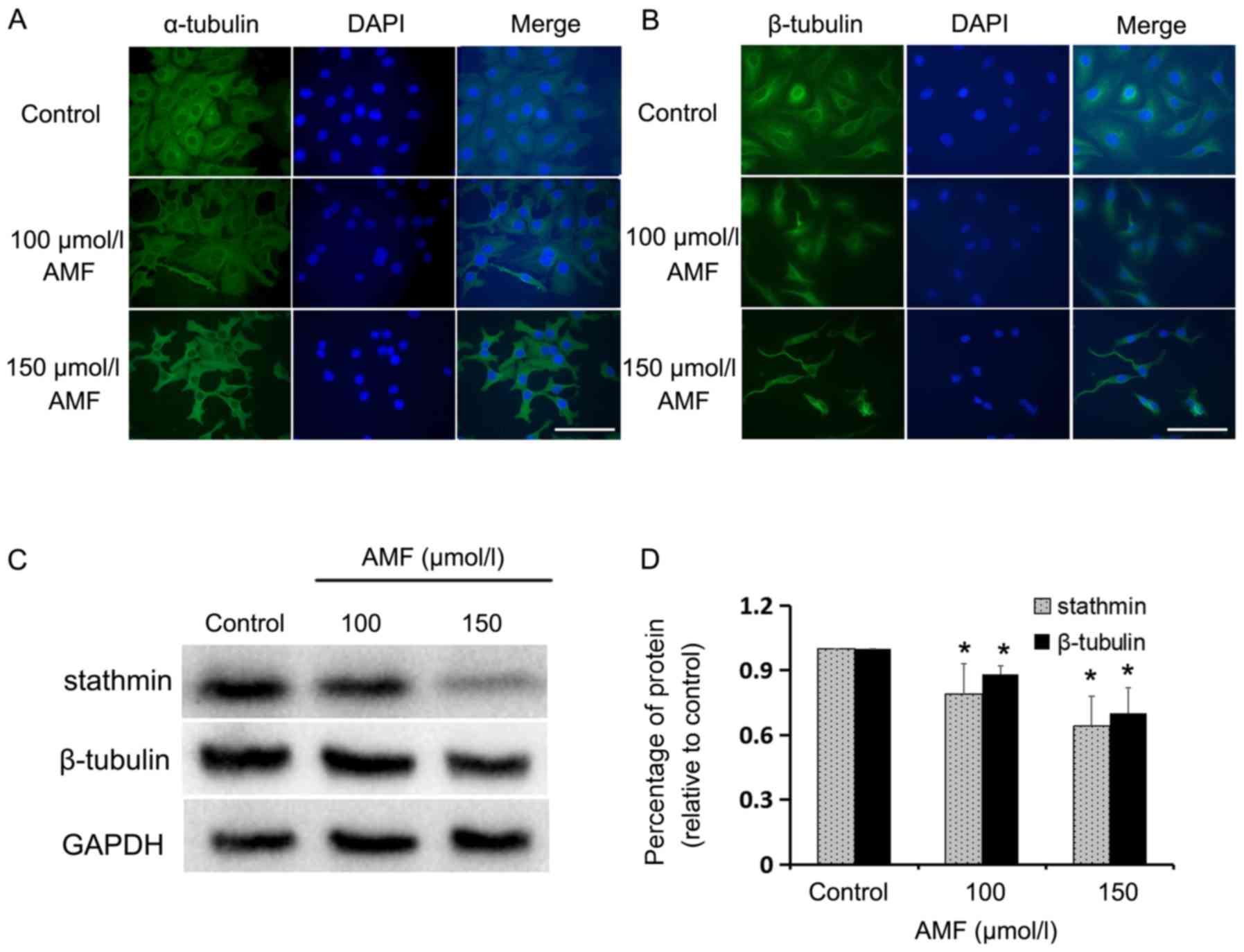
AMF interferes with tubulin expression
and spindle assembly
MTs are made from tubulin heterodimers and are vital
for several cellular processes, such as spindle assembly for cell
meiosis (24). MTs have complex
polymerization characteristics and are stable and long lasting
during interphase (25). Conversely,
MTs become short and dynamic during mitosis. Stathmin regulates
cell cycle progression by influencing the dynamics of MTs (13).
The present study assessed the influence of AMF on
MT structure via immunofluorescent staining of α/β-tubulin in SKOV3
cells, and determined the expression levels of stathmin and
β-tubulin via western blot analysis. Immunofluorescence staining
demonstrated that α/β-tubulin were long and condensed in
AMF-treated cells compared with the control cells (Fig. 2A and B). Furthermore, the expression
levels of β-tubulin and stathmin were significantly downregulated
following treatment with AMF (Fig. 2C
and D). Taken together, these results indicate that spindle
assembly and cell meiosis are altered in AMF-treated SKOV3
cells.
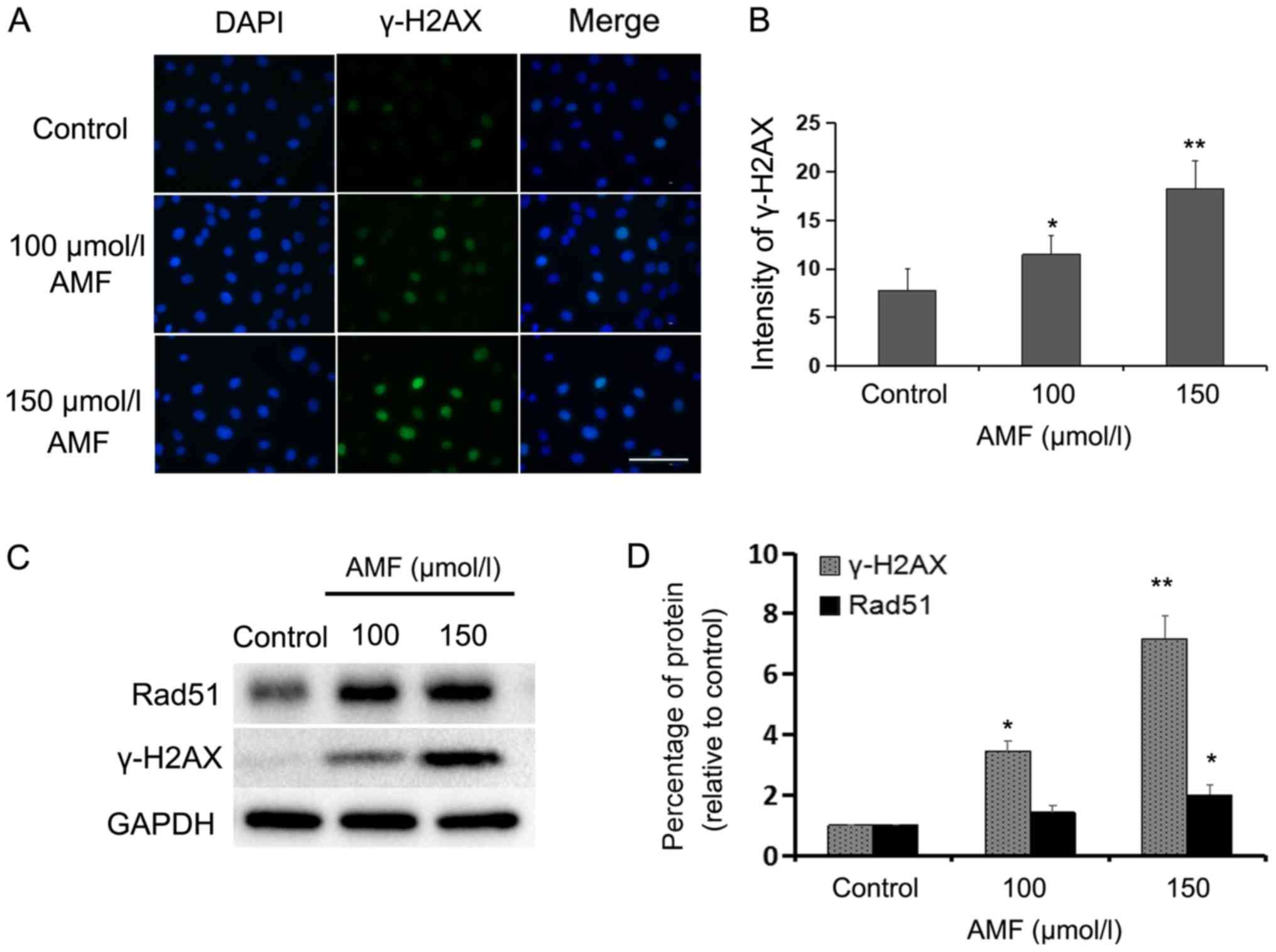
AMF induces DNA damage in SKOV3
cells
In order to determine whether AMF induces DNA damage
in SKOV3 cells, the expression levels of γ-H2AX, a specific marker
of DNA double-strand breaks (DSBs) (26), were assessed via immunofluorescence
and western blot analyses. Immunofluorescence staining demonstrated
that the percentage of γ-H2AX-positive cells significantly
increased in AMF-treated SKOV3 cells compared with the control
cells (Fig. 3A and B). Furthermore,
the number of DNA-damaged cells and fluorescence intensity
increased with AMF in a dose-dependent manner. Compared with in the
control cells, western blot analysis indicated that the protein
expressions were significantly higher in 100 and 150 µmol/l
AMF-treated cells for γ-H2AX and in 150 µmol/l AMF-treated cells
for Rad51 (Fig. 3C and D). Taken
together, these results suggest that AMF induces extensive DNA
damage. Rad51 formation is a hallmark of homologous recombination
repair (HRR), which is often induced by DNA damage (27). The results of the present study
indicated that DSBs were induced by AMF and the cells attempted to
repair DNA damage through the HRR signaling pathway.
Discussion
Previous studies have reported the anticancer
effects of AMF in different types of tumor (28–32). For
example, AMF has been demonstrated to be associated with apoptosis
and the inhibition of metastasis and angiogenesis of tumors.
Furthermore, AMF has exhibited its anticancer effect in SiHa and
CaSki cervical cancer cells by the suppressing expression levels of
the human papilloma virus protein, E7 (33). The present study investigated the
antitumor effect of AMF on ovarian cancer, and the results
demonstrated that AMF decreased SKOV3 cell viability and induced
cell cycle arrest in the S and G2 phases, in a dose-dependent
manner. Furthermore, AMF induced DNA damage and interfered with MT
function and meiosis.
Several antitumor drugs, such as paclitaxel and
cisplatin, decrease cell proliferation by either inducing cell
death or arresting cell cycle progression. Previous studies have
reported that AMF induces cell apoptosis (23,32,33). The
results of the present study demonstrated that treatment with AMF
significantly increased the proportion of G2 phase SKOV3 cells. The
proportion of S phase cells was also upregulated, however, no
significant difference was observed compared with the control
cells. The results of the present study demonstrated that AMF was
able to induce cell cycle arrest of ovarian cancer cells in S and
G2 phases, which is in partly inconsistent with previous findings
that have demonstrated that AMF is able to arrest cells either in S
or G1 phases (34–36). These results suggest that the effect
of AMF on cell cycle is influenced by cell type, AMF concentration
or/and treatment time. There are some AMF-like bioflavonoids, such
as bilobetin, isoginkgetin and morelloflavone, which can also
arrest cell cycle at G2/M phase by inducing cell
apoptosis or inhibiting the activation of Raf/MEK/ERK kinases
(18). It is well known that CDKs,
CKIs and cyclins also play key roles in cell cycle progression
(6,37,38).
CDK1, in combination with cyclin A and B, regulates the transition
from G2 to M phase (39).
P21, a member of the CKIs, can promote cell cycle arrest as a
response to several stimuli such as DNA damage and oxidative stress
by regulating G1/S or G2/M transitions,
respectively (8). P21 is
predominantly induced by p53, which is activated by several
stressors, including DNA damage. P21 is also known to inhibit the
activity of cyclinA/CDK1/2, which results in cell cycle arrest in
the S phase (40,41). In the present study, the expression
levels of p-CDK1 and CDK2 significantly decreased, while P21
expression increased in AMF-treated SKOV3 cells, suggesting that
AMF may induce G2/M cell cycle arrest by upregulating
P21 and downregulating CDK1 and CDK2. A previous study demonstrated
that paclitaxel or eribulin can arrest cell meiosis and lead to the
accumulation of mitotic marker proteins, such as cyclin B1
(42). In the present study, cyclin
B1 was significantly downregulated following treatment with 100
µmol/l AMF, but upregulated following treatment with 150 µmol/l
AMF. A reason for this increase in cyclin B1 expression may be due
to the protein accumulation induced by meiosis arrest.
MT acts as a key drug target in tumor cells due to
its roles in determining and supporting cell shape, cell division,
transport and signal transduction (43). Previous studies have demonstrated
that paclitaxel or eribulin can arrest cell meiosis by regulating
MT polymerization (12,44,45).
Under normal conditions, there is a balance between polymerization
and de-polymerization of MTs, whereby disruption of this balance
destroys the normal MT structures observed (46,47).
Stathmin is a MT destabilizing protein that inhibits tubulin dimer
polymerization and contributes to the formation of cell spindles
(48). Previous studies have
reported that stathmin is upregulated in the highly malignant types
of breast and ovarian cancers (49,50).
Furthermore, downregulation of stathmin inhibits cell viability and
induced apoptosis in several types of cancer cells (51,52).
Paclitaxel is an efficacious MT-stabilizing antitumor drug,
particularly used in the treatments of ovarian, breast and
non-small cell lung cancers (53).
Paclitaxel is considered to shift the assembly equilibrium of MTs
towards the depolymeric state, thus blocking cell entry into
meiosis by suppressing MT dynamics (53). The results of the present study
demonstrated that treatment with AMF decreased the expression
levels of stathmin and β-tubulin in SKOV3 cells. Immunofluorescence
staining was performed to assess MT structures, using antibodies
against α- and β-tubulin. The results indicated that MT structures
were distorted, and the cell spindle-like structures were disturbed
following treatment with AMF. Furthermore, AMF blocked cell cycle
at the G2/M phase, interfered with MT dynamics and downregulated
the expression levels of proteins associated with MT structures.
Taken together, these results indicate that the effects of AMF on
ovarian cancer cells are like those of paclitaxel.
Following cell DNA damage, DNA repair mechanisms are
activated and DNA replication and meiosis are interrupted.
Mammalian cells have evolved a series of DNA repair systems,
including non-homologous end-joining and homologous recombination
(HR) (54). H2AX, a variant of H2A,
is rapidly phosphorylated at Ser 139 and accumulates at DSB sites
with other proteins including Rad51 and BRCA1/2 (55,56).
Among these, Rad51 is a key factor involved in HR (57,58).
Rad51 is recruited to γ-H2AX sites and polymerizes at the
resection-generated single-stranded DNA ends, which leads to
invasion and exchange between homologous DNA sequences (58). The results of the present study
demonstrated that Rad51 expression markedly increased in
AMF-treated SKOV3 cells. Furthermore, the intensity and expression
of γ-H2AX were significantly upregulated in AMF-treated SKOV3
cells. Considering the key roles γ-H2AX and Rad51 play in DNA
damage repair, the results of the present study suggest that AMF
induces DNA damage and activates the HR repair system in
AMF-treated SKOV3 cells. The present study demonstrated that AMF
triggered cell cycle G2/M arrest and induced DNA damage in ovarian
cancer cells, even though it may be better to use several ovarian
cancer cell lines than just to use SKOV3 cell line. We will be
aimed at confirming these findings and prove the antitumor effect
of AMF in ovarian cancer cell line derived xenograft mouse
models.
In conclusion, the results of the present study
demonstrated that AMF inhibited human ovarian cancer cell
proliferation by triggering cell cycle arrest at the
G2/M phase. Furthermore, AMF was demonstrated to
interfere with MT dynamics and induce DNA damage. Thus, AMF may act
as an antitumor drug by exerting its effects on MT dynamics and
inducing DNA damage.
Acknowledgements
Flow cytometry work was supported by Ms. Fang Su and
Ms. Jing Wei (Guangdong Provincial Key Laboratory of Malignant
Tumor Epigenetics and Gene Regulation, Sun Yat-Sen Memorial
Hospital, Sun Yat-Sen University, China).
Funding
The present study was funded by Guangdong Bureau of
Traditional Chinese Medicine (grant nos. 20181206 and 20191260),
the National Natural Science Foundation of China (grant no.
81272222 and 81902802), the General Science and Technology Project
of Guangzhou Municipal Health Commission (grant no. 20181A010017
and 20191A011019), the Medical Science and Technology Research
Foundation of Guangdong (grant nos. B2016018 and A2018063) and the
Guangzhou Science and Technology Program Key Project (grant no.
201704020145).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
ZL, JZ, AL and XL contributed to the initial
conception and design of the experiments. HS, XX, SQ, PW and LD
performed the experiments. ZL and JZ wrote the paper. ZZ revised
the experimental design and analyzed the data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patients consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: Globocan
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bookman MA: Optimal primary therapy of
ovarian cancer. Ann Oncol. 27 (Suppl 1):i58–i62. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang X, Xu B, Sun CY, Wang LM and Miao X:
Knockdown of CIP2A sensitizes ovarian cancer cells to cisplatin: An
in vitro study. Int J Clin Exp Med. 8:16941–16947. 2015.PubMed/NCBI
|
|
4
|
Damia G and Broggini M: Platinum
resistance in ovarian cancer: Role of DNA repair. Cancers (Basel).
11:1192019. View Article : Google Scholar
|
|
5
|
Dia-Moralli S, Tarrado-Castellarnau M,
Miranda A and Cascante M: Targeting cell cycle regulation in cancer
therapy. Pharmacol Ther. 138:255–271. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lim S and Kaldis P: Cdks, cyclins and
CKIs: Roles beyond cell cycle regulation. Development.
140:3079–3093. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Morgan DO: The cell cycle: Principles of
control. Primers in biology, New Science. 2007.
|
|
8
|
Karimian A, Ahmadi Y and Yousefi B:
Multiple functions of p21 in cell cycle, apoptosis and
transcriptional regulation after DNA damage. DNA Repair (Amst).
42:63–71. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liebmann J, Cook JA, Lipschultz C, Teague
D, Fisher J and Mitchell JB: The influence of Cremophor EL on the
cell cycle effects of paclitaxcl (Taxol) in human tumor cell lines.
Cancer Chemother Pharmacol. 33:331–339. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jordan MA, Toso RJ, Thrower D and Wilson
L: Mechanism of milotic block and inhibition of cell proliferation
by taxol at low concentrations. Proc Nati Acad Sci USA.
90:9552–9556. 1993. View Article : Google Scholar
|
|
11
|
Desai A and Mitchison TJ: Microtubule
polymerization dynamics. Annu Rev Cell Dev Biol. 13:83–117. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Schiff PB, Fant J and Horwitz SB:
Promotion of microtubule assembly in vitro by taxol. Nature.
277:665–667. 1979. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Charbaut E, Curmi PA, Ozon S, Lachkar S,
Redeker V and Sobel A: Stathmin family proteins display specific
molecular and tubulin binding properties. J Biol Chem.
276:16146–16154. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Su D, Smith SM, Preti M, Schwartz P,
Rutherford TJ, Menato G, Danese S, Ma S, Yu H and Katsaros D:
Stathmin and tubulin expression and survival of ovarian cancer
patients receiving platinum treatment with and without paclitaxel.
Cancer. 115:2453–2463. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Watanabe A, Suzuki H, Yokobori T,
Tsukagoshi M, Altan B, Kubo N, Suzuki S, Araki K, Wada S,
Kashiwabara K, et al: Stathmin1 regulates p27 expression,
proliferation and drug resistance, resulting in poor clinical
prognosis in cholangiocarcinoma. Cancer Sci. 105:690–696. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Johnsen JI, Aurelio ON, Kwaja Z, Jögensen
GE, Pellegata NS, Plattner R, Stanbridge EJ and Cajot JF:
p53-mediated negative regulation of stathmin/Op18 expression is
associated with G2/M cell-cycle arrest. Int J Cancer. 88:685–691.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Pang X, Yi T, Yi Z, Cho SG, Qu W, Pinkaew
D, Fujise K and Liu M: Morelloflavone, a biflavonoid, inhibits
tumor angiogenesis by targeting rho GTPases and extracellular
signal-regulated kinase signaling pathways. Cancer Res. 69:518–525.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li M, Li B, Xia ZM, Tian Y, Zhang D, Rui
WJ, Dong JX and Xiao FJ: Anticancer Effects of Five Biflavonoids
from Ginkgo Biloba L. Male Flowers In Vitro. Molecules.
24:14962019. View Article : Google Scholar
|
|
19
|
Banerjee T, Valacchi G, Ziboh VA and van
der Vliet A: Inhibition of TNFalpha-induced cyclooxygenase-2
expression by amentoflavone through suppression of NF-kappaB
activation in A549 cells. Mol Cell Biochem. 238:105–110. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhang Z, Sun T, Niu JG, He ZQ, Liu Y and
Wang F: Amentoflavone protects hippocampal neurons:
Anti-inflammatory, antioxidative, and antiapoptotic effects. Neural
Regen Res. 10:1125–1133. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
An J, Li Z, Dong Y, Ren J and Huo J:
Amentoflavone protects against psoriasis-like skin lesion through
suppression of NF-κB-mediated inflammation and keratinocyte
proliferation. Mol Cell Biochem. 413:87–95. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Li F, Song XW, Su GF, Wang YL, Wang ZY,
Jia XY, Qin SR, Huang L and Wang Y, Zheng K and Wang Y:
Amentoflavone inhibits HSV-1 and ACV-resistant strain infection by
suppressing viral early infection. Viruses. 11:4662019. View Article : Google Scholar
|
|
23
|
Zhang J, Liu Z, Cao W, Chen L, Xiong X,
Qin S, Zhang Z, Li X and Hu CA: Amentoflavone inhibits angiogenesis
of endothelial cells and stimulates apoptosis in hypertrophic scar
fifibroblasts. Burns. 40:922–929. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Eshun-Wilson L, Zhang R, Portran D,
Nachury MV, Toso DB, Löhr T, Vendruscolo M, Bonomi M, Fraser JS and
Nogales E: Effects of α-tubulin acetylation on microtubule
structure and stability. Proc Natl Acad Sci USA. 116:10366–10371.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ohkawa N, Fujitani K, Tokunaga E, Furuya S
and Inokuchi K: The microtubule destabilizer stathmin mediates the
development of dendritic arbors in neuronal cells. J Cell Sc.
120:1447–1456. 2007. View Article : Google Scholar
|
|
26
|
Firsanov DV, Solovjeva LV and Svetlova MP:
H2AX phosphorylation at the sites of DNA double-strand breaks in
cultivated mammalian cells and tissues. Clin Epigenetics.
2:283–297. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen JJ, Silver DP, Cantor SB, Cantor S,
Livingston DM and Scully R: BRCA1, BRCA2, and Rad51 operate in a
common DNA damage response pathway. Cancer Res. 59 (7
Suppl):1752S–1756S. 1999.PubMed/NCBI
|
|
28
|
Liu B and Yu S: Amentoflavone suppresses
hepatocellular carcinoma by repressing hexokinase 2 expression
through inhibiting JAK2/STAT3 signaling. Biomed Pharmacother.
107:243–253. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lee KC, Tsai JJ, Tseng CW, Kuo YC, Chuang
YC, Lin SS and Hsu FT: Amentoflavone inhibits ERK-modulated tumor
progression in hepatocellular carcinoma in vitro. In Vivo.
32:549–554. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hsu FT, Chiang IT, Kuo YC, Hsia TC, Lin
CC, Liu YC and Chung JG: Amentoflavone effectively blocked the
tumor progression of glioblastoma via suppression of ERK/NF-κB
signaling pathway. Am J Chin Med. 47:913–931. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Guruvayoorappan C and Kuttan G: Effect of
amentoflavone on the inhibition of pulmonary metastasis induced by
B16F-10 melanoma cells in C57BL/6 mice. Integr Cancer Ther.
6:185–197. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lee JS, Lee MS, Oh WK and Sul JY: Fatty
acid synthase inhibitionby amentoflflavone induces apoptosis and
antiproliferation in human breast cancer cells. Biol Pharm Bull.
32:1427–1432. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lee SJ, Kim HJ, Kang JW, Kim JH, Lee DH,
Kim MS, Yang Y, Woo ER, Kim YM, Hong J and Yoon DY: The biflavonoid
amentoflavone induces apoptosis via suppressing E7 expression, cell
cycle arrest at sub-G1 phase, and mitochondria-emanated intrinsic
pathways in Human Cervical Cancer Cells. J Med Food. 14:808–816.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Pei JS, Liu CC, Hsu YN, Lin LL, Wang SC,
Chung JG, Bau DT and Lin SS: Amentoflavone induces cell-cycle
arrest and apoptosis in MCF-7 human breast cancer cells via
mitochondria-dependent pathway. In Vivo. 26:963–970.
2012.PubMed/NCBI
|
|
35
|
Jung HJ, Park K, Lee IS, Kim HS, Yeo SH,
Woo ER and Lee DG: S-phase accumulation of Candida albicans by
anticandidal effect of amentoflavone isolated from Selaginella
tamariscina. Biol Pharm Bull. 30:1969–1971. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Liu H, Yue Q and He S: Amentoflavone
suppresses tumor growth in ovarian cancer by modulating Skp2. Life
Sci. 189:96–105. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Dehay C and Kennedy H: Cell-cycle control
and cortical development. Nat Rev Neurosci. 8:438–450. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Malumbres M and Barbacid M: Cell cycle,
CDKs and cancer: A changing paradigm. Nat Rev Cancer. 9:153–166.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Marais A, Ji Z, Child ES, Krause E, Mann
DJ and Sharrocks AD: Cell cycle-dependent regulation of the
forkhead transcription factor FOXK2 by CDK-cyclin complexes. J Biol
Chem. 285:35728–35739. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Bertoli C, Skotheim JM and de Bruin RA:
Control of cell cycle transcription during G1 and S phases. Nat Rev
Mol Cell Biol. 14:518–528. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Choi WI, Kim MY, Jeon BN, Koh DI, Yun CO,
Li Y, Lee CE, Oh J, Kim K and Hur MW: Role of promyelocytic
leukemia zinc finger (PLZF) in cell proliferation and
cyclin-dependent kinase inhibitor 1A (p21WAF/CDKN1A) gene
repression. J Biol Chem. 289:18625–18640. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Tsuda Y, Iimori M, Nakashima Y, Nakanishi
R, Ando K, Ohgaki K, Kitao H, Saeki H and Maehara Y: Mitotic
slippage and the subsequent cell fate after inhibition of Aurora B
during tubulin-binding agent-induced mitotic arrest. Sci Rep.
17:167622017. View Article : Google Scholar
|
|
43
|
Burbank KS and Mitchison TJ: Microtubule
dynamic instability. Curr Biol. 16:R516–R517. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Benbow SJ, Wozniak KM, Kulesh B, Savage A,
Slusher BS, Littlefield BA, Jordan MA, Wilson L and Feinstein SC:
Microtubule-targeting agents eribulin and paclitaxel differentially
affect neuronal cell bodies in chemotherapy induced peripheral
neuropathy. Neurotox Res. 32:151–162. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Field JJ, Díaz JF and Miller JH: The
binding sites of microtubule-stabilizing agents. Chem Biol.
20:301–315. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Cao YN, Zheng LL, Wang D, Liang XX, Gao F
and Zhou XL: Recent advances in microtubule-stabilizing agents. Eur
J Med Chem. 143:806–828. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Prota AE, Bargsten K, Zurwerra D, Field
JJ, Diaz JF, Altmann KH and Steinmetz MO: Molecular mechanism of
action of microtubule-stabilizing anticancer agents. Science.
339:587–590. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Cassimeris L: The oncoprotein 18/stathmin
family of microtubule destabilizers. Curr Opin Cell Biol. 14:18–24.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Obayashi S, Horiguchi J, Higuchi T,
Katayama A, Handa T, Altan B, Bai T, Bao P, Bao H, Yokobori T, et
al: Stathmin1 expression is associated with aggressive phenotypes
and cancer stem cell marker expression in breast cancer patients.
Int J Oncol. 51:781–790. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Carney BK and Cassimeris L:
Stathmin/oncoprotein 18, a microtubule regulatory protein, is
required for survival of both normal and cancer cell lines lacking
the tumor suppressor p53. Cancer Biol Ther. 9:699–709. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Alli E, Yang JM and Hait WN: Silencing of
stathmin induces tumor-suppressor function in breast cancer cell
lines harboring mutant p53. Oncogene. 26:1003–1012. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Wang R, Dong K, Lin F, Wang X, Gao P, Wei
SH, Cheng SY and Zhang HZ: Inhibiting proliferation and enhancing
chemosensitivity to taxanes in osteosarcoma cells by RNA
interference-mediated downregulation of stathmin expression. Mol
Med. 13:567–575. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Dumontet C and Jordan MA:
Microtubule-binding agents: A dynamic field of cancer therapeutics.
Nat Rev Drug Discov. 9:790–803. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Velic D, Couturier AM, Ferreira MT,
Rodrigue A, Poirier GG, Fleury G and Masson GY: DNA damage
signalling and repair inhibitors: The long-sought-after Achilles'
heel of cancer. Biomolecules. 5:3204–3259. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Lobrich M, Shibata A, Beucher A, Fisher A,
Ensminger M, Goodarzi AA, Barton O and Jeggo PA: GammaH2AX foci
analysis for monitoring DNA double-strand break repair: Strengths,
limitations and optimization. Cell Cycle. 9:662–669. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Daley JM, Kwon Y, Niu H and Sung P:
Investigations of homologous recombination pathways and their
regulation. Yale J Biol Med. 86:453–461. 2013.PubMed/NCBI
|
|
57
|
Graeser M, McCarthy A, Lord CJ, Savage K,
Hills M, Salter J, Orr N, Parton M, Smith IE, Reis-Filho JS, et al:
A marker of homologous recombination predicts pathologic complete
response to neoadjuvant chemotherapy in primary breast cancer. Clin
Cancer Res. 16:6159–6168. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Baumann P, Benson FE and West SC: Human
Rad51 protein promotes ATP-dependent homologous pairing and strand
transfer reactions in vitro. Cell. 87:757–766. 1996. View Article : Google Scholar : PubMed/NCBI
|