Introduction
Hepatocellular carcinoma (HCC) is a common cause of
cancer-related deaths worldwide, causing approximately 740,000
deaths each year; it is the second most common cause of cancer
related-deaths in the world, second only to lung cancer (1). Although the diagnosis and treatment
techniques of HCC are improving (2,3), the
most widely used treatment is hepatectomy, however approximately
70% of HCC patients experience postoperative recurrence and
metastasis. Postoperative tumor recurrence and metastasis or
chronic liver disease such as hepatitis and/or cirrhosis
complications often lead to poor prognosis, especially when the
tumor progresses to the advanced stage; its 5-year survival rate is
<20% and the currently available drug treatment can only bring
negligible survival benefits, and the cost is high (4–6). China
has a high rate of chronic hepatitis B virus (HBV) infection, and
HCC patients account for nearly 55% of all cases in the world
(7). Recent studies have revealed
that up to 80% of the occurrence of HCC is related to chronic
inflammation caused by chronic liver diseases such as hepatitis,
alcoholic or non-alcoholic steatohepatitis, and may be involved in
the triggering, malignant transformation, invasion and metastasis
of cancer in HCC patients (8,9). Solute
carrier family 17 member 9 (SLC17A9) is also known as vesicular
nucleotide transporter. It is a cell membrane transporter encoded
by the gene located on 20q13.33, and belongs to one of the four
identified new members of the solute carrier family 17 (SLC-17). It
is widely expressed in human organs, tissues and cells, especially
in the brain, adrenal glands and thyroid (10). Its main function is to participate in
vesicle uptake, storage and secretion of adenosine triphosphate
(ATP) as well as other nucleotides, and especially plays an
important role in the ATP transport of airway epithelium and
neutrophils, astrocytes, adrenal chromaffin cells and pancreatic
cells (11). SLC17A9 can mediate ATP
accumulation in lysosomes and is an indispensable factor for
maintaining lysosomal physiology and cell viability (12). Studies have confirmed that SLC17A9
promotes abnormal amplification of chromosome 20q DNA, thereby
driving the transformation from colorectal adenoma to colorectal
cancer (13). SLC17A9 is important
for cell transport and cell vitality, especially for cancer cell
ATP transport (14). However, little
is known about the role of SLC17A9 in HCC. The purpose of the
present study was to detect the expression pattern of SLC17A9 in
HCC and to elucidate its clinical significance.
Materials and methods
Standards for patient selection and
inclusion
Ninety-eight patients with HCC were included in the
present study, including 60 males and 38 females, aged 25 to 90
years old, with a median age of 57.5 years. They were treated at
our hospital from January 2010 to December 2014. There were 10
cases in grade I (Edmondson classification), 50 cases in grade II
and 38 cases in grade III. There were 20 cases with metastasis and
58 cases with cirrhosis. Inclusion criteria were as follows: i) The
patients were diagnosed with primary HCC by pathology; ii) the
patients did not undergo any treatment before surgery, including
radiotherapy, chemotherapy, biotherapy or embolism; iii) the
patients had complete clinical data and follow-up information; iv)
in addition to HCC, the patient did not have tumors at other sites.
Exclusion criteria: Those who did not meet the aforementioned
standards were excluded. The present study was approved by the
Ethics Committee of the Central Hospital of Wuhan (Tongji Medical
College, Huazhong University of Science and Technology). Signed
written informed consents were obtained from the patients and/or
guardians.
Follow-up of patients
The follow-up was carried out through regular
outpatient visits and telephone, and the main end-point events were
recurrence and death. The survival time was from the date of
surgery to the end of follow-up (August 2019) or the date of death.
Tumor-free survival time was the time from the date of the surgery
to the follow-up deadline or to the first recurrence during the
follow-up. During the follow-up period, a total of 3 cases were
lost, which was a cut-off value.
Immunochemistry
The steps for immunochemistry were as follows: The
slices (4-µm-thick) were fixed with 10% formaldehyde and embedded
in paraffin, then they were heated at 60°C for 2 h, dewaxed for 20
min in xylene twice, and rehydrated in gradient ethanol. Antigen
repair was performed in citrate buffer (pH 6.0, 10 mM) by microwave
(95°C, 15 min), and then was blocked with 3%
H2O2 for 15 min (28°C). After washing with
phosphate-buffered saline (PBS), the slices were incubated with 5%
bovine serum (Gene Tech) to block the nonspecific binding, and the
anti-SLC17A9 antibody (dilution 1:100, EMD Millipore, cat. no.
2020-467092) was incubated at 4°C overnight. After washing three
times, the tissue slices were treated with horseradish peroxidase
coupled double antibody (dilution 1:300, Gene Tech, cat. no.
2017-416029) at room temperature for 30 min according to the
manufacturer's instructions. Finally, the slices were immersed in
3,3-o-diamino-benzidine (Gene Tech) for 2 min, stained with
hematoxylin, dehydrated and observed under a microscope (Olympus
BX51, ×400 magnification).
Immunohistochemistry score and patient
grouping
The pathological tissue sections were evaluated by
two pathologists under double-blind method, and the staining score
was multiplied by the staining intensity and the percentage of
positive cells. The staining intensity was assessed (15) as follows: Negative staining (score
0), weak staining (score, 1), moderate staining (score 2), and
strong staining (score, 3). The percentage of positive cells were
scored as follows: 0–10% (score 0), 1125% (score 1), 2650% (score
2), and 51–100% (score 3). According to the results of the
immunohistochemistry score, HCC patients were divided into two
groups: The patients whose immunohistochemistry score was >6
were divided into the SLC17A9-high expression group, and the
patients whose immunohistochemistry score was ≤6 were divided into
the SLC17A9-low expression group.
Statistical analysis
All statistical analysis was carried out using
social science statistical software package (version 19.0; SPSS,
Inc.). The relevance between SLC17A9 expression and
clinicopathological parameters of HCC patients was analyzed by
χ2 or Fisher's accurate test. Kaplan-Meier method and
log-rank test were used to compare the survival rate of patients
with high and low expression of SLC17A9. Cox proportional risk
regression model was used to analyze the risk factors affecting the
prognosis of patients with HCC. A P-value <0.05 indicated a
statistically significant difference.
Results
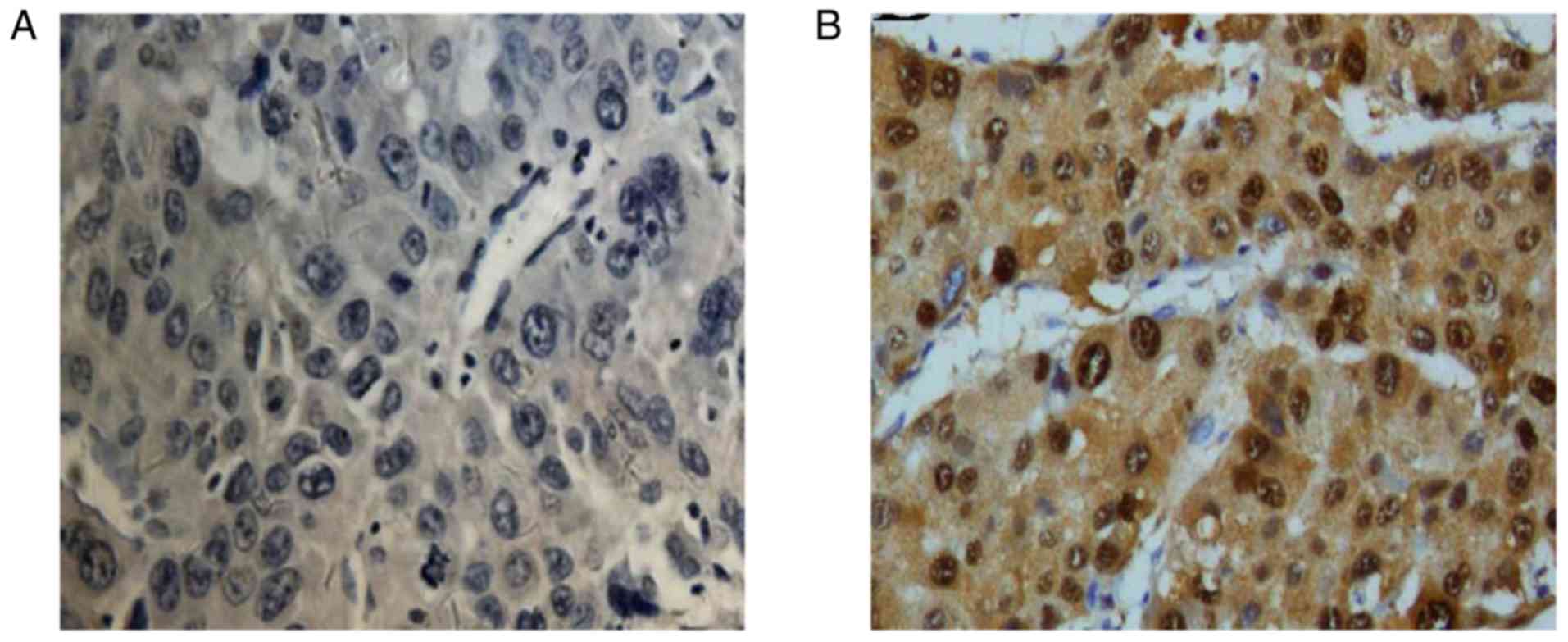
Expression of SLC17A9 in cancer
tissues of patients with HCC
Immunohistochemistry revealed that SLC17A9 was
mainly expressed in the cytoplasm and partially expressed in the
nucleus. Among the 98 patients with HCC, 43 (43/98, 43.88%) had low
expression of SLC17A9 and 55 (55/98, 56.12%) had high expression of
SLC17A9. The typical immunohistochemical images of SLC17A9
expression in cancer tissues of patients with HCC is presented in
Fig. 1.
Relevance between SLC17A9 expression
in cancer tissues of HCC patients and clinicopathological
parameters
According to the histochemical score and the
expression level of SLC17A9, patients were divided into two groups
with high and low expression of SLC17A9. The expression of SLC17A9
was associated with Edmondson grade (P=0.04) and distant metastasis
(P=0.03). The expression of SLC17A9 was not associated with age,
sex, tumor size, tumor number, liver cirrhosis, liver cell surface
antigen (HBs antigen) and AFP concentration (P>0.05; Table I).
 | Table I.Associations between the expression of
SLC17A9 in HCC tissues and clinical parameters. |
Table I.
Associations between the expression of
SLC17A9 in HCC tissues and clinical parameters.
|
|
| Expression of
SLC17A9 |
|
|
|---|
|
|
|
|
|
|
|---|
| Clinical
parameters | No. of cases | Low expression
(%) | High expression
(%) | χ2 | P-value |
|---|
| Age (years) |
| 43 | 55 | 0.32 | 0.57 |
|
<55 | 42 | 21 | 21 |
|
|
| ≥55 | 56 | 22 | 34 |
|
|
| Sex |
|
|
| 0.71 | 0.40 |
| Male | 60 | 30 | 30 |
|
|
|
Female | 38 | 13 | 25 |
|
|
| Tumor size (cm) |
|
|
| 3.28 | 0.07 |
|
<5 | 58 | 18 | 40 |
|
|
| ≥5 | 40 | 25 | 15 |
|
|
| No. of tumors |
|
|
| 0.14 | 0.71 |
| Single
tumor | 70 | 31 | 39 |
|
|
| Multiple
tumors | 28 | 12 | 16 |
|
|
| Edmondson grade |
|
|
| 6.38 | 0.04 |
| I | 10 | 3 | 7 |
|
|
| II | 50 | 17 | 33 |
|
|
| III | 38 | 23 | 15 |
|
|
| Distant
metastasis |
|
|
| 4.14 | 0.03 |
| No | 78 | 33 | 45 |
|
|
|
Yes | 20 | 10 | 10 |
|
|
| Cirrhosis |
|
|
| 0.72 | 0.39 |
| No | 40 | 21 | 19 |
|
|
|
Yes | 58 | 22 | 36 |
|
|
| HBs antigen |
|
|
| 0.77 | 0.29 |
|
Positive | 39 | 20 | 19 |
|
|
|
Negative | 59 | 23 | 36 |
|
|
| AFP
concentration |
|
|
| 0.19 | 0.68 |
| ≤400
µg/l | 29 | 13 | 16 |
|
|
| >400
µg/l | 69 | 30 | 39 |
|
|
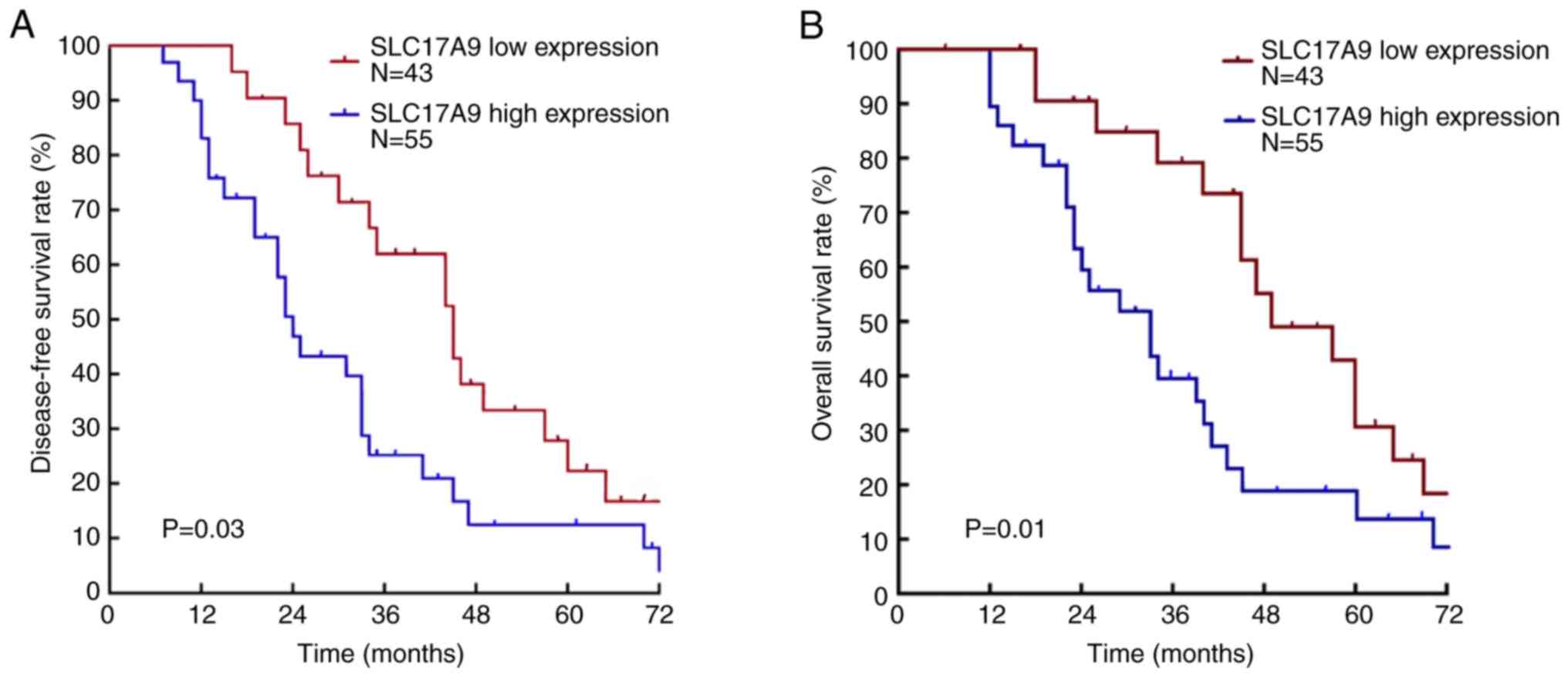
Association between the expression of
SLC17A9 and the prognosis of HCC patients
Kaplan-Meier survival analysis revealed that the
average survival time of patients with low expression of SLC17A9
was 41.12±2.78 months. The average survival time of patients with
high expression of SLC17A9 was 29.18±4.36 months. The 5-year
tumor-free survival rate and total survival rate in patients with
low expression of SLC17A9 were 24.7 and 30.7%, respectively. The
5-year tumor-free survival rate and the overall survival rate in
patients with high expression of SLC17A9 were 14.5 and 22.8%,
respectively. The tumor-free survival rate (P=0.03) and overall
survival rate (P=0.01) of patients in the SLC17A9-high expression
group were significantly lower than those in the SLC17A9-low
expression group (Fig. 2).
Univariate and multivariate analysis
affecting the tumor-free survival of patients with HCC
Univariate analysis revealed that there were several
factors affecting the tumor-free survival rate of HCC patients,
including tumor size (P=0.03), Edmondson grade (P=0.007), distant
metastasis (P=0.006), microvascular invasion (P=0.02), the AFP
level (P=0.003) and SLC17A9 expression (P=0.03). Multivariate
analysis revealed that the expression of SLC17A9 (HR, 0.77; 95% CI,
0.27–2.47; P=0.02) was an independent risk factor for tumor-free
survival in patients with HCC (Table
II).
 | Table II.Univariate and multivariate analysis
of clinical parameters affecting the tumor-free survival of
patients with HCC. |
Table II.
Univariate and multivariate analysis
of clinical parameters affecting the tumor-free survival of
patients with HCC.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Clinical
parameters | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Age | 0.86 | 0.44–1.81 | 0.06 | NA |
|
|
| Sex | 1.79 | 0.87–2.49 | 0.08 | NA |
|
|
| Tumor size | 2.16 | 1.44–3.87 | 0.03a | 1.56 | 0.88–3.90 | 0.79 |
| No. of tumors | 1.45 | 0.67–2.34 | 0.51 | NA |
|
|
| Edmondson
grade | 2.77 | 2.71–4.95 | 0.007a | 2.44 | 1.78–4.93 | 0.02 |
| Distant
metastasis | 5.03 | 2.85–9.41 | 0.006a | 3.99 | 1.27–7.64 | 0.04 |
| Microvascular
infiltration | 2.32 | 1.45–3.99 | 0.02a | 1.35 | 0.95–3.80 | 0.39 |
| HBs antigen | 1.38 | 0.75–2.88 | 0.60 | NA |
|
|
| Cirrhosis | 1.36 | 0.50–1.81 | 0.58 | NA |
|
|
| AFP level | 2.72 | 1.47–4.89 | 0.003a | 1.83 | 0.77–4.89 | 0.19 |
| SLC17A9
expression | 0.80 | 0.26–0.89 | 0.03a | 0.77 | 0.27–2.47 | 0.02 |
Univariate and multivariate analysis
affecting the overall survival rate of patients with HCC
Univariate analysis revealed that the overall
survival rate of patients with HCC was significantly correlated
with tumor size (P=0.01), Edmondson grade (P<0.01), distant
metastasis (P<0.01), AFP level (P<0.01), microvascular
invasion (P=0.01) and SLC17A9 expression (P=0.03). Multivariate
analysis revealed that the expression of SLC17A9 (HR, 1.81; 95% CI,
0.99–3.77; P=0.04), Edmondson grade (P=0.01) and distant metastasis
(P=0.04) were independent risk factors for overall survival rate in
patients with HCC (Table III).
 | Table III.Univariate and multivariate analysis
of clinical parameters affecting the overall survival rate of
patients with HCC. |
Table III.
Univariate and multivariate analysis
of clinical parameters affecting the overall survival rate of
patients with HCC.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Clinical
parameters | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Age | 0.65 | 0.41–1.31 | 0.07 | NA |
|
|
| Sex | 1.58 | 0.92–2.69 | 0.09 | NA |
|
|
| Tumor size | 1.95 | 1.22–3.31 | 0.01 | 1.06 | 0.49–2.28 | 0.89 |
| No. of tumors | 1.24 | 0.68–2.26 | 0.49 | NA |
|
|
| Edmondson
grade | 2.56 | 1.71–3.84 | <0.01 | 2.44 | 1.28–4.63 | 0.01 |
| Distant
metastasis | 4.82 | 2.55–9.11 | <0.01 | 2.99 | 1.07–8.35 | 0.04 |
| Microvascular
infiltration | 2.11 | 1.25–3.56 | 0.01 | 1.35 | 0.65–2.80 | 0.42 |
| HBs antigen | 1.17 | 0.65–2.10 | 0.60 | NA |
|
|
| Cirrhosis | 1.15 | 0.70–1.91 | 0.58 | NA |
|
|
| AFP level | 2.51 | 1.40–4.52 | <0.01 | 1.72 | 0.83–3.56 | 0.14 |
| SLC17A9
expression | 0.59 | 0.36–0.96 | 0.03 | 1.81 | 0.99–3.77 | 0.04 |
Discussion
The incidence of HCC is ranked fifth worldwide and
the mortality rate is ranked third (6). The mortality incidence of HCC in China
is 383,000 people/year, and 70% of new cases originate from Asia
(7). The incidence of HCC is on the
rise and increases steadily at a relative rate of 3% per year
(1,8). Hepatectomy is the main method for the
treatment of HCC, but there are still challenges to overcome such
as improving the rate of radical resection and reducing the
recurrence rate after surgery (8).
It is particularly important to explore the biomarkers related to
the prognosis of patients with HCC.
SLC17A9 is a new member of the transmembrane protein
family involved in the transport of small molecules (16), which is located in the functional
gene coding of human chromosome 20q13.33, in which gene mutations
occur in autosomal dominant disseminated superficial hyperkeratosis
patients (17). SLC17A9 is a
vesicular nucleotide transporter that plays a role in ATP transport
through the secretory vesicles/granule membranes of astrocytes, T
cells and pancreatic cells (18).
Takai et al (19) reported
that knockdown of SLC17A9 could inhibit the exocytosis of ATP and
reduce cell migration of human lung cancer cells. SLC17A9 protein
can also function as a lysosomal ATP transporter and regulate cell
viability (10). A recent study
reported (20) that SLC17A9 was
highly expressed in colorectal cancer. Western blotting and
immunohistochemical examination revealed that the expression of
SLC17A9 in cancer tissue of patients with rectal cancer was
significantly higher than that of adjacent tissues, and was
significantly related to the poor prognosis of patients. To date,
few studies (19–21) have reported the importance of SLC17A9
in HCC.
The present study revealed that SLC17A9 was mainly
located in the cytoplasm. Among the 98 patients with HCC, 43
patients (43/98, 43.88%) had low expression of SLC17A9 and 55
patients (55/98, 56.12%) had high expression of SLC17A9. A previous
study reported that (20) in all 144
patients with colorectal cancer, 61 patients had low expression of
SLC17A9 and 83 patients had high expression of SLC17A9, similar to
the results of the present study, indicating that the low
expression of SLC17A9 exhibits differential expression in different
cancer tissues.
In the present study, it was revealed that the
expression of SLC17A9 was associated with Edmondson grade (P=0.04)
and distant metastasis (P=0.03). Results revealed that patients
with high expression of SLC17A9 had higher Edmondson grade and
higher rate of distant metastasis, which may be related to tumor
invasiveness and metastasis of HCC, however the expression of
SLC17A9 was not related to age, sex, tumor size, tumor number and
liver cirrhosis (P>0.05). At present, it has rarely been
reported that the expression of SLC17A9 is associated with the
clinicopathological parameters of cancer patients (20,21). It
has previously been revealed that the high expression of SLC17A9
was closely related to the TNM stage of cancer patients in oral
squamous cell carcinoma (21).
In the present study, Kaplan-Meier survival analysis
revealed that the tumor-free survival rate (P=0.03) and overall
survival rate (P=0.01) in patients with high expression of SLC17A9
were significantly lower than those in patients with low expression
of SLC17A9. Multivariate analysis of Cox proportional risk model
revealed that SLC17A9 expression was an independent risk factor for
predicting postoperative tumor-free survival rate and overall
survival rate in patients with HCC. These results indicated that
SLC17A9 expression is a new biomarker for potentially predictable
prognosis in patients with HCC. The association between SLC17A9
expression and cancer prognosis was limited to two different types
of tumors (20,21). The high expression of SLC17A9 in
patients with CRC was related to the poor prognosis of patients
with colorectal cancer. After grouping the patients with colorectal
cancer according to different TNM stages, it was also revealed that
the high expression of SLC17A9 remained an independent risk factor
for predicting the poor prognosis of colorectal cancer in stage
IV+III and stage I+II (20), and the
survival rate of patients with high expression of SLC17A9 was
significantly decreased in patients with gastric cancer (21).
The mechanism of how SLC17A9 expression affect the
prognosis of patients with HCC is still not clear. Studies have
reported that SLC17A9 protein is highly enriched in lysosomes and
acts as an ATP transporter. SLC17A9 deficiency has been revealed to
reduce lysosomal ATP accumulation and impair lysosomal function
(22,23). ATP release through lysosomal
exocytosis was revealed to be related to cell migration (24,25). In
animal experiments in mice, it was determined that the high
expression of SLC17A9 could promote the formation of tumor buds in
colorectal cancer (25). A tumor bud
is defined as a cluster of single cells or dedifferentiated tumor
cells at the invasion front, which is highly correlated with
epithelial-stroma transformation in tumor progression (25). In both colorectal cancer (26) and oral squamous cell carcinoma
(25), the formation of tumor buds
was closely related to the occurrence and progression of squamous
cell carcinoma and its EMT process. In the present study, it was
revealed that the high expression of SLC17A9 was related to the
poor prognosis of patients with HCC, and the poor prognosis may be
due to the promotion of the progression of HCC through the
epithelial-mesenchymal transition (EMT) pathway. In future studies,
the molecular mechanism of the function of SLC17A9 in patients with
HCC will be explored. In gastric cancer patients, a previous study
revealed that the expression levels of SLC17A9 mRNA and protein in
cancer tissues of gastric cancer patients were significantly higher
than those in adjacent tissues; the high expression of SLC17A9
protein was positively correlated with the mutation of tumor
protein p53 gene (TP53) in cancer tissues of patients, and was an
independent risk factor for postoperative recurrence and mortality
prediction of the patients and thus it was suggested that SLC17A9
may drive TP53 gene mutations and participate in gastric cancer
progression and poor prognosis (21). A recent genome-wide sequence analysis
of 130 patients with acute lymphoblastic leukemia (including 69
adult patients and 61 pediatric patients) also revealed aberrant
expression of SLC17A9 mRNA; SLC17A9 mRNA overexpression was an
independent risk factor of the poor prognosis for adult patients
with acute lymphoblastic leukemia, and no association between
SLC17A9 mRNA and patient prognosis was found in pediatric patients
(27). The present study revealed
that in patients with HCC, patients with high SLC17A9 protein
expression had a poor prognosis, and its molecular mechanism
remains to be further explored.
The limitations of the present study include: First,
the study was a single-center retrospective study, and the number
of included cases was small; large-scale multicenter prospective
studies are required to further confirm the conclusions of the
present study. Second, the molecular mechanism of SLC17A9 function
in patients with HCC requires further study.
In conclusion, the results of the present study
revealed that the prognosis of patients with high expression of
SLC17A9 in HCC patients was significantly lower than that of
patients with low expression of SLC17A9. The high expression of
SLC17A9 may play an important role in the progression of HCC, which
may be a new prognostic molecular marker and potential therapeutic
target in patients with HCC.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JW and YY conceived and designed the study. JW, YY
and JS were responsible for the collection, analysis and
interpretation of the data. JW drafted the manuscript. YY revised
the manuscript critically for important intellectual content. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of The Central Hospital of Wuhan, Tongji Medical College,
Huazhong University of Science and Technology. Signed written
informed consents were obtained from the patients and/or
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lee S, Kang TW, Cha DI, Song KD, Lee MW,
Rhim H, Lim HK, Sinn DH, Kim JM and Kim K: Radiofrequency ablation
vs. surgery for perivascular hepatocellular carcinoma: Propensity
score analyses of long-term outcomes. J Hepatol. 69:70–78. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Romano A, Angeli P, Piovesan S, Noventa F,
Anastassopoulos G, Chemello L, Cavalletto L, Gambato M, Russo FP,
Burra P, et al: Newly diagnosed hepatocellular carcinoma in
patients with advanced hepatitis C treated with DAAs: A prospective
population study. J Hepatol. 69:345–352. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tokumitsu Y, Sakamoto K, Tokuhisa Y,
Matsui H, Matsukuma S, Maeda Y, Sakata K, Wada H, Eguchi H, Ogihara
H, et al: A new prognostic model for hepatocellular carcinoma
recurrence after curative hepatectomy. Oncol Lett. 15:4411–4422.
2018.PubMed/NCBI
|
|
5
|
Zhu Q, Li N, Zeng X, Han Q, Li F, Yang C,
Lv Y, Zhou Z and Liu Z: Hepatocellular carcinoma in a large medical
center of China over a 10-year period: Evolving therapeutic option
and improving survival. Oncotarget. 6:44402015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Parikh ND, Singal AG and Hutton DW: Cost
effectiveness of regorafenib as second-line therapy for patients
with advanced hepatocellular carcinoma. Cancer. 123:3725–3731.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yang JD, Hainaut P, Gores GJ, Amadou A,
Plymoth A and Roberts LR: A global view of hepatocellular
carcinoma: Trends, risk, prevention and management. Nat Rev
Gastroenterol Hepatol. 22:589–604. 2019. View Article : Google Scholar
|
|
8
|
Zhu RX, Seto WK, Lai CL and Yuen MF:
Epidemiology of hepatocellular carcinoma in the Asia-Pacific
region. Gut Liver. 10:3322016. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Levrero M and Zucman-Rossi J: Mechanisms
of HBV-induced hepatocellular carcinoma. J Hepatol. 64 (Suppl
1):S84–S101. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sreedharan S, Shaik JH, Olszewski PK,
Levine AS, Schiöth HB and Fredriksson R: Glutamate, aspartate and
nucleotide transporters in the SLC17 family form four main
phylogenetic clusters: Evolution and tissue expression. BMC
Genomics. 11:172010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bissa B, Beedle AM and Govindarajan R:
Lysosomal solute carrier transporters gain momentum in research.
Clin Pharmacol Ther. 100:431–436. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Moriyama Y, Hiasa M, Sakamoto S, Omote H
and Nomura M: Vesicular nucleotide transporter (VNUT): Appearance
of an actress on the stage of purinergic signaling. Purinergic
Signal. 13:387–404. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cao Q, Zhao K, Zhong XZ, Zou Y, Yu H,
Huang P, Xu TL and Dong XP: SLC17A9 protein functions as a
lysosomal ATP transporter and regulates cell viability. J Biol
Chem. 289:23189–23199. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sillars-Hardebol AH, Carvalho B, Tijssen
M, Beliën JA, de Wit M, Delis-van Diemen PM, Pontén F, van de Wiel
MA, Fijneman RJ and Meijer GA: TPX2 and AURKA promote 20q
Amplicon-driven colorectal adenoma to carcinoma progression. Gut.
61:1568–1575. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Weinberg SE and Chandel NS: Targeting
mitochondria metabolism for cancer therapy. Nat Chem Biol.
11:92015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhai E, Liang W, Lin Y, Huang L, He X, Cai
S, Chen J, Zhang N, Li J, Zhang Q, et al: HSP70/HSP90-organizing
protein contributes to gastric Cancer progression in an autocrine
fashion and predicts poor survival in gastric Cancer. Cell Physiol
Biochem. 47:879–892. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cui H, Li L, Wang W, Shen J, Yue Z, Zheng
X, Zuo X, Liang B, Gao M, Fan X, et al: Exome sequencing identifies
SLC17A9 pathogenic gene in two Chinese pedigrees with disseminated
superficial actinic porokeratosis. J Med Genet. 51:699–704. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dereure O: Mutation in the SLC17A9 gene in
familial superficial actinic disseminated porokeratosis. Ann
Dermatol Venereol. 142:155–156. 2015.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Takai E, Tsukimoto M, Harada H, Sawada K,
Moriyama Y and Kojima S: Autocrine regulation of TGF-β1-induced
cell migration by exocytosis of ATP and activation of P2 receptors
in human lung cancer cells. J Cell Sci. 125:5051–5060. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yang L, Chen Z, Xiong W, Ren H, Zhai E, Xu
K, Yang H, Zhang Z, Ding L, He Y, et al: High expression of SLC17A9
correlates with poor prognosis in colorectal cancer. Human Pathol.
84:62–70. 2019. View Article : Google Scholar
|
|
21
|
Li J, Su T, Yang L, Deng L, Zhang C and He
Y: High SLC17A9 expression correlates with poor survival in gastric
carcinoma. Future Oncol. 15:4155–4166. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Haanes KA, Kowal JM, Arpino G, Lange SC,
Moriyama Y, Pedersen PA and Novak I: Role of vesicular nucleotide
transporter VNUT (SLC17A9) in release of ATP from AR42J cells and
mouse pancreatic acinar cells. Purinergic Signal. 10:431–440. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Koike M, Nakanishi H, Saftig P, Ezaki J,
Isahara K, Ohsawa Y, Schulz-Schaeffer W, Watanabe T, Waguri S,
Kametaka S, et al: Cathepsin D deficiency induces lysosomal storage
with ceroid lipofuscin in mouse CNS neurons. J Neurosci.
20:6898–6906. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dou Y, Wu HJ, Li HQ, Qin S, Wang YE, Li J,
Lou HF, Chen Z, Li XM, Luo QM and Duan S: Microglial migration
mediated by ATP-induced ATP release from lysosomes. Cell Res.
22:1022–1033. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hong KO, Oh KY, Shin WJ, Yoon HJ, Lee JI
and Hong SD: Tumor budding is associated with poor prognosis of
oral squamous cell carcinoma and histologically represents an
epithelial-mesenchymal transition process. Hum Pathol. 80:123–129.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
De Smedt L, Palmans S, Andel D, Govaere O,
Boeckx B, Smeets D, Galle E, Wouters J, Barras D, Suffiotti M, et
al: Expression profiling of budding cells in colorectal cancer
reveals an EMT-like phenotype and molecular subtype switching. Br J
Cancer. 116:58–65. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen B, Jiang L, Zhong ML, Li JF, Li BS,
Peng LJ, Dai YT, Cui BW, Yan TQ, Zhang WN, et al: Identification of
fusion genes and characterization of transcriptome features in
T-cell acute lymphoblastic leukemia. Proc Natl Acad Sci USA.
115:373–378. 2018. View Article : Google Scholar : PubMed/NCBI
|